Iron Status, Anemia, and Iron Interventions and Their Associations with Cognitive and Academic Performance in Adolescents: A Systematic Review
Abstract
1. Introduction
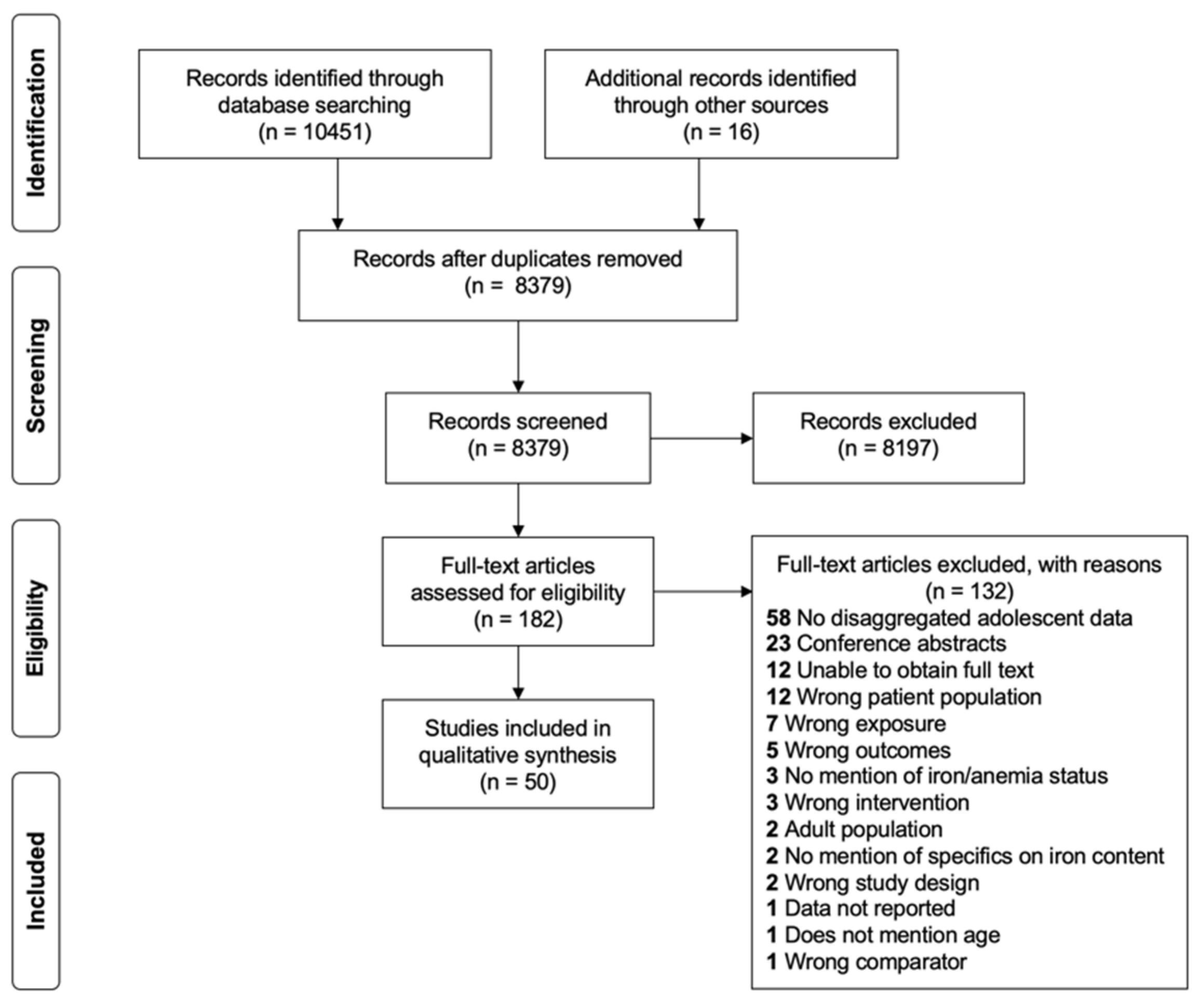
2. Materials and Methods
2.1. Search Strategy
2.2. Selection Criteria and Eligibility
2.3. Quality Assessment
2.4. Data Extraction and Synthesis
3. Results
3.1. Description of Included Studies
3.2. Quality Assessment and Risk of Bias
3.3. Association of Iron Status and/or Anemia with Dimensions of Academic Performance and Cognitive Function
3.3.1. Attention and Concentration
3.3.2. Intelligence
3.3.3. Memory and Recall
3.3.4. School Performance
3.3.5. Other Measures of Cognitive Performance
3.4. The Effects of Dietary Iron Intake on Dimensions of Academic Performance and Cognitive Function
3.4.1. School Performance
3.4.2. Intelligence
3.5. The Effects of Food-Based Interventions on Dimensions of Academic Performance and Cognitive Function
3.5.1. Attention and Concentration
3.5.2. Intelligence
3.5.3. Memory and Recall
3.5.4. School Performance
3.5.5. Other Measures of Cognitive Performance
3.6. The Effects of Iron-Only Supplementation Interventions on Dimensions of Academic Performance and Cognitive Function
3.6.1. Attention and Concentration
3.6.2. Intelligence
3.6.3. Memory and Recall
3.6.4. School Performance
3.6.5. Other Measures of Cognitive Performance
3.7. The Effects of Iron Plus Additional Micronutrients Supplementation Interventions on Dimensions of Academic Performance and Cognitive Function
3.7.1. Intelligence
3.7.2. Other Measures of Cognitive Performance
4. Discussion
4.1. Attention and Concentration
4.2. Intelligence
4.3. Memory and Recall
4.4. School Performance
4.5. Comparison with Other Literature
4.6. Limitations
4.7. Program Implications
4.8. Conclusions and Future Research
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Lynch, S.; Pfeiffer, C.M.; Georgieff, M.K.; Brittenham, G.; Fairweather-Tait, S.; Hurrell, R.F.; McArdle, H.J.; Raiten, D.J. Biomarkers of Nutrition for Development (BOND)-Iron Review. J. Nutr. 2018, 148, 1001S–1067S. [Google Scholar] [CrossRef] [PubMed]
- Gropper, S.; Smith, J. Advanced Human Nutrition and Metabolism, 6th ed.; Wadsworth, Cengage Learning: Belmont, CA, USA, 2013; ISBN 978-1-133-10405-6. [Google Scholar]
- Bothwell, T.; Charlton, R.; Cook, J.; Finch, C. Iron Metabolism in Man; Blackwell Scientific Publications: Oxford, UK, 1979. [Google Scholar]
- World Health Organization. Global Accelerated Action for the Health of Adolescents (AA-HA!) Implementation Guidance, 2016–2030; World Health Organization: Geneva, Switzerland, 2017.
- Burrows, T.; Goldman, S.; Pursey, K.; Lim, R. Is There an Association between Dietary Intake and Academic Achievement: A Systematic Review. J. Hum. Nutr. Diet. 2017, 30, 117–140. [Google Scholar] [CrossRef] [PubMed]
- Falkingham, M.; Abdelhamid, A.; Curtis, P.; Fairweather-Tait, S.; Dye, L.; Hooper, L. The Effects of Oral Iron Supplementation on Cognition in Older Children and Adults: A Systematic Review and Meta-Analysis. Nutr. J. 2010, 9, 4. [Google Scholar] [CrossRef]
- Hermoso, M.; Vucic, V.; Vollhardt, C.; Arsic, A.; Roman-Viñas, B.; Iglesia-Altaba, I.; Gurinovic, M.; Koletzko, B. The Effect of Iron on Cognitive Development and Function in Infants, Children and Adolescents: A Systematic Review. Ann. Nutr. Metab. 2011, 59, 154–165. [Google Scholar] [CrossRef] [PubMed]
- Low, M.; Farrell, A.; Biggs, B.; Pasricha, S. Effects of Daily Iron Supplementation in Primary-School-Aged Children: Systematic Review and Meta-Analysis of Randomized Controlled Trials. CMAJ Can. Med. Assoc. J. = J. L’Assoc. Med. Can. 2013, 185, E791–E802. [Google Scholar] [CrossRef]
- Sterne, J.; Savović, J.; Page, M.; Elbers, R.; Blencowe, N.; Boutron, I.; Cates, C.; Cheng, H.-Y.; Corbett, M.; Eldridge, S.; et al. RoB 2: A Revised Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Sterne, J.; Hernán, M.; Reeves, B.; Savović, J.; Berkman, N.; Viswanathan, M.; Henry, D.; Altman, D.; Ansari, M.; Boutron, I.; et al. ROBINS-I: A Tool for Assessing Risk of Bias in Non-Randomized Studies of Interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef]
- National Institute of Health. Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 5 December 2019).
- Karkada, S.; Upadhya, S.; Upadhya, S.; Bhat, G. Beneficial Effects of Ragi (Finger Millet) on Hematological Parameters, Body Mass Index, and Scholastic Performance among Anemic Adolescent High-School Girls (AHSG). Compr. Child Adolesc. Nurs. 2019, 42, 141–150. [Google Scholar] [CrossRef]
- Sen, A.; Kanani, S.J. Impact of Iron-Folic Acid Supplementation on Cognitive Abilities of School Girls in Vadodara. Indian Pediatr. 2009, 46, 137–143. [Google Scholar]
- Sorensen, L.B.; Damsgaard, C.T.; Dalskov, S.M.; Petersen, R.A.; Egelund, N.; Dyssegaard, C.B.; Stark, K.D.; Andersen, R.; Tetens, I.; Astrup, A.; et al. Diet-Induced Changes in Iron and n-3 Fatty Acid Status and Associations with Cognitive Performance in 8–11-Year-Old Danish Children: Secondary Analyses of the Optimal Well-Being, Development and Health for Danish Children through a Healthy New Nordic Diet. Br. J. Nutr. 2015, 114, 1623–1637. [Google Scholar] [CrossRef]
- Vazir, S.; Nagalla, B.; Thangiah, V.; Kamasamudram, V.; Bhattiprolu, S. Effect of Micronutrient Supplement on Health and Nutritional Status of Schoolchildren: Mental Function. Nutrition 2006, 22, S26–S32. [Google Scholar] [CrossRef] [PubMed]
- Devaki, P.B.; Chandra, R.K.; Geisser, P. Effects of Oral Iron(III) Hydroxide Polymaltose Complex Supplementation on Hemoglobin Increase, Cognitive Function, Affective Behavior and Scholastic Performance of Adolescents with Varying Iron Status: A Single Centre Prospective Placebo Controlled Study. Arzneim.-Forsch./Drug Res. 2009, 59, 303–310. [Google Scholar]
- Halliday, K.E.; Karanja, P.; Turner, E.L.; Okello, G.; Njagi, K.; Dubeck, M.M.; Allen, E.; Jukes, M.C.H.; Brooker, S.J. Plasmodium Falciparum, Anaemia and Cognitive and Educational Performance among School Children in an Area of Moderate Malaria Transmission: Baseline Results of a Cluster Randomized Trial on the Coast of Kenya. Trop. Med. Int. Health 2012, 17, 532–549. [Google Scholar] [CrossRef]
- Abalkhail, B.; Shawky, S. Prevalence of Daily Breakfast Intake, Iron Deficiency Anaemia and Awareness of Being Anaemic among Saudi School Students. Int. J. Food Sci. Nutr. 2002, 53, 519–528. [Google Scholar] [CrossRef]
- Anuar Zaini, M.Z.; Lim, C.T.; Low, W.Y.; Harun, F. Effects of Nutritional Status on Academic Performance of Malaysian Primary School Children. Asia-Pac. J. Public Health 2005, 17, 81–87. [Google Scholar] [CrossRef]
- Aquilani, R.; Maggi, L.; Parisi, U.; Ghioni, G.; Zucchella, M.; Nardi, T.; Lombardi, P.; Covini, C.; Verri, M.; Barbieri, A.; et al. School Performance Is Associated with Dietary Iron and Zinc Intake in Adolescent Girls. Curr. Top. Nutraceutical Res. 2011, 9, 71–76. [Google Scholar]
- Cai, M.Q.; Yan, W.Y. Study on Iron Nutritional Status in Adolescence. Biomedical and environmental sciences. BES 1990, 3, 113–119. [Google Scholar]
- Carruyo-Vizcaíno, C.; Vizcaíno, G.; Diez-Ewald, M.; Arteaga-Vizcaíno, M.; Torres-Guerra, E. Concentration of Haemoglobin and Nutrients in Middle-Class Adolescents. Relationship to Academic Achievement. Investig. Clín. 1995, 36, 117–130. [Google Scholar]
- Dissanayake, D.S.; Kumarasiri, P.V.; Nugegoda, D.B.; Dissanayake, D.M. The Association of Iron Status with Educational Performance and Intelligence among Adolescents. Ceylon Med. J. 2009, 54, 75–79. [Google Scholar] [CrossRef]
- El Hioui, M.; Azzaoui, F.-Z.; Ahami, A.O.T.; Rusinek, S.; Aboussaleh, Y. Iron Deficiency and Cognitive Function among Moroccan School Children. Nutr. Ther. Metab. 2012, 30, 84–89. [Google Scholar]
- Goudarzi, A.; Mehrabi, M.R.; Goudarzi, K. The Effect of Iron Deficiency Anemia on Intelligence Quotient (IQ) in under 17 Years Old Students. Pak. J. Biol. Sci. PJBS 2008, 11, 1398–1400. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Halterman, J.S.; Kaczorowski, J.M.; Aligne, C.A.; Auinger, P.; Szilagyi, P.G. Iron Deficiency and Cognitive Achievement among School-Aged Children and Adolescents in the United States. Pediatrics 2001, 107, 1381–1386. [Google Scholar] [CrossRef]
- Hutchinson, S.E.; Powell, C.A.; Walker, S.P.; Chang, S.M.; Grantham-McGregor, S.M. Nutrition, Anaemia, Geohelminth Infection and School Achievement in Rural Jamaican Primary School Children. Eur. J. Clin. Nutr. 1997, 51, 729–735. [Google Scholar] [CrossRef][Green Version]
- Ivanovic, D.M.; Perez, H.T.; Olivares, M.G.; Diaz, N.S.; Leyton, B.D.; Ivanovic, R.M. Scholastic Achievement: A Multivariate Analysis of Nutritional, Intellectual, Socioeconomic, Sociocultural, Familial, and Demographic Variables in Chilean School-Age Children. Nutrition 2004, 20, 878–889. [Google Scholar] [CrossRef]
- Ji, X.; Cui, N.; Liu, J. Neurocognitive Function Is Associated With Serum Iron Status in Early Adolescents. Biol. Res. Nurs. 2017, 19, 269–277. [Google Scholar] [CrossRef]
- Kharat, P.S.; Waghmare, P.P. Could Anemia Be the Reason for Dysfunctional Cognition? Int. J. Res. Med. Sci. 2015, 3, 663. [Google Scholar] [CrossRef][Green Version]
- Masalha, R.; Afawi, Z.; Mahajnah, M.; Mashal, A.; Hallak, M.; Alsaied, I.; Bolotin, A.; Ifergan, G.; Wirguin, I. The Impact of Nutritional Vitamin B12, Folate and Hemoglobin Deficiency on School Performance of Elementary School Children. J. Pediatr. Neurol. 2008, 6, 243–248. [Google Scholar]
- More, S.; Shivkumar, V.B.; Gangane, N.; Shende, S. Effects of Iron Deficiency on Cognitive Function in School Going Adolescent Females in Rural Area of Central India. Anemia 2013. [Google Scholar] [CrossRef]
- Nagalakshmi, P.; Santhosh, H.; Shobha, C. A Study of Correlation between Hemoglobin Level and Cognitive Function in Children from Rural Area Staying in Residential School. Indian J. Physiol. Pharmacol. 2015, 59, 308–312. [Google Scholar]
- Nemati, A.; Barak, M.; Dehgan, M.H.; Alimohammadi, H.; Ettehad, G.H.; Baghi, N.; Arvin, J.; Mogadam, R.A.; Abbasgholizade, N. Relation between Iron Deficiency and Anemia Whit School Success, Weight and Height in Schoolgirls Aged 12 Year Old in Ardebil Province of Iran, 2005. Res. J. Biol. Sci. 2007, 2, 263–267. [Google Scholar]
- Olson, C.L.; Acosta, L.P.; Hochberg, N.S.; Olveda, R.M.; Jiz, M.; McGarvey, S.T.; Kurtis, J.D.; Bellinger, D.C.; Friedman, J.F. Anemia of Inflammation Is Related to Cognitive Impairment among Children in Leyte, The Philippines. PLoS Negl. Trop. Dis. 2009, 3, e533. [Google Scholar] [CrossRef] [PubMed]
- Ortega, R.M.; Gonzalez Fernandez, M.; Paz, L.; Andres, P.; Jimenez, L.M.; Jimenez, M.J.; Gonzalez Gross, M.; Requejo, A.M.; Gaspar, M.J. Influence of Iron Status on Attention and Intellectual Performance of a Population of Spanish Adolescents. Arch. Lat. Nutr. 1993, 43, 6–11. [Google Scholar]
- Sen, A.; Kanani, S.J. Deleterious Functional Impact of Anemia on Young Adolescent School Girls. Indian Pediatr. 2006, 43, 219–226. [Google Scholar]
- SoonMyung, H.; HyeJin, H.; HyunHee, K. A Study on Iron Nutritional Status and Anemia of Middle School Girls in Ulsan Metropolitan City. J. Community Nutr. 2004, 6, 86–90. [Google Scholar]
- Teni, M.; Shiferaw, S.; Asefa, F. Anemia and Its Relationship with Academic Performance among Adolescent School Girls in Kebena District, Southwest Ethiopia. Biotechnol. Health Sci. 2017, 4, e43458. [Google Scholar] [CrossRef]
- Thalanjeri, P.; Karanth, H.; Vinutha Shankar, M.S.; Kutty, K. Impact of Iron Deficiency Anemia on Cognition of School Children of South India. Indian J. Clin. Anat. Physiol. 2016, 3, 135–138. [Google Scholar] [CrossRef]
- Walker, S.P.; Grantham-Mcgregor, S.M.; Himes, J.H.; Williams, S.; Duff, E.M. School Performance in Adolescent Jamaican Girls: Associations with Health, Social and Behavioural Characteristics, and Risk Factors for Dropout. J. Adolesc. 1998, 21, 109–122. [Google Scholar] [CrossRef][Green Version]
- Webb, T.E.; Oski, F.A. Iron Deficiency Anemia and Scholastic Achievement in Young Adolescents. J. Pediatr. 1973, 82, 827–830. [Google Scholar] [CrossRef]
- Kalaichelvi, D. A Study on Effectiveness of Nutritional Intervention in Treating Iron Deficiency Anemia and Improving Intelligence among Adolescent Girls. Ph.D. Thesis, Vinayaka Missions University, Salem, India, 2016. [Google Scholar]
- Khan, M.A.; Farhana Haseen, F.; Jalal, C.S.B.; Rahman, M.; Akter, S.; Huda, S.N. Effects of a Multiple Micronutrient Beverage Supplement on Haematologic, Iron, Vitamin A and Growth Status and Cognitive Development and School Performance among Adolescent Girls in Bangladesh. BRAC; 2004. Available online: https://idl-bnc-idrc.dspacedirect.org/handle/10625/32143 (accessed on 5 December 2019).
- Muthayya, S.; Thankachan, P.; Hirve, S.; Amalrajan, V.; Thomas, T.; Lubree, H.; Agarwal, D.; Srinivasan, K.; Hurrell, R.F.; Yajnik, C.S.; et al. Iron Fortification of Whole Wheat Flour Reduces Iron Deficiency and Iron Deficiency Anemia and Increases Body Iron Stores in Indian School-Aged Children. J. Nutr. 2012, 142, 1997–2003. [Google Scholar] [CrossRef] [PubMed]
- Scott, S.P.; Murray-Kolb, L.E.; Wenger, M.J.; Udipi, S.A.; Ghugre, P.S.; Boy, E.; Haas, J.D. Cognitive Performance in Indian School-Going Adolescents Is Positively Affected by Consumption of Iron-Biofortified Pearl Millet: A 6-Month Randomized Controlled Efficacy Trial. J. Nutr. 2018, 148, 1462–1471. [Google Scholar] [CrossRef]
- Solon, F.S.; Sarol, J.N., Jr.; Bernardo, A.B.I.; Solon, J.A.A.; Mehansho, H.; Sanchez-Fermin, L.E.; Wambangco, L.S.; Juhlin, K.D. Effect of a Multiple-Micronutrient-Fortified Fruit Powder Beverage on the Nutrition Status, Physical Fitness, and Cognitive Performance of Schoolchildren in the Philippines. Food Nutr. Bull. 2003, 24, S129–S140. [Google Scholar] [CrossRef] [PubMed]
- Vinodkumar, M.; Erhardt, J.G.; Rajagopalan, S. Impact of a Multiple-Micronutrient Fortified Salt on the Nutritional Status and Memory of Schoolchildren. Int. J. Vitam. Nutr. Res. 2009, 79, 348–361. [Google Scholar] [CrossRef]
- Ballin, A.; Berar, M.; Rubinstein, U.; Kleter, Y.; Hershkovitz, A.; Meytes, D. Iron State in Female Adolescents. Am. J. Dis. Child. 1992, 146, 803–805. [Google Scholar] [CrossRef]
- Bruner, A.B.; Joffe, A.; Duggan, A.K.; Casella, J.F.; Brandt, J. Randomised Study of Cognitive Effects of Iron Supplementation in Non-Anaemic Iron-Deficient Adolescent Girls. Lancet 1996, 348, 992–996. [Google Scholar] [CrossRef]
- Chellappa, A.R.; Karunanidhi, S. Effect of Iron and Zinc Supplementation on Cognitive Functions of Female Adolescents in Chennai, India. Int. Proc. Chem. Biol. Environ. Eng. (IPCBEE) 2012, 39, 17–24. [Google Scholar]
- Lambert, A.; Knaggs, K.; Scragg, R.; Schaaf, D. Effects of Iron Treatment on Cognitive Performance and Working Memory in Non-Anaemic, Iron-Deficient Girls. N. Z. J. Psychol. 2002, 31, 19. [Google Scholar]
- Rezaeian, A.; Ghayour-Mobarhan, M.; Mazloum, S.R.; Yavari, M.; Jafari, S.A. Effects of Iron Supplementation Twice a Week on Attention Score and Haematologic Measures in Female High School Students. Singap. Med. J. 2014, 55, 587–592. [Google Scholar] [CrossRef]
- Soemantri, A.G.; Gopaldas, T.; Seshadri, S.; Pollitt, E. Preliminary Findings on Iron Supplementation and Learning Achievement of Rural Indonesian Children. Am. J. Clin. Nutr. 1989, 50, 698–702. [Google Scholar] [CrossRef] [PubMed]
- Soemantri, A.G.; Pollitt, E.; Kim, I. Iron Deficiency Anemia and Educational Achievement. Am. J. Clin. Nutr. 1985, 42, 1221–1228. [Google Scholar] [CrossRef] [PubMed]
- Umamaheswari, K.; Bhaskaran, M.; Krishnamurthy, G.; Kavita, V. Effect of Iron and Zinc Deficiency on Short Term Memory in Children. Indian Pediatr. 2011, 48, 289–293. [Google Scholar] [CrossRef]
- Haskell, C.F.; Scholey, A.B.; Jackson, P.A.; Elliott, J.M.; Defeyter, M.A.; Greer, J.; Robertson, B.C.; Buchanan, T.; Tiplady, B.; Kennedy, D.O. Cognitive and Mood Effects in Healthy Children during 12 Weeks’ Supplementation with Multi-Vitamin/Minerals. Br. J. Nutr. 2008, 100, 1086–1096. [Google Scholar] [CrossRef] [PubMed]
- Lynn, R.; Harland, E.P. A Positive Effect of Iron Supplementation on the IQs of Iron Deficient Children. Personal. Individ. Differ. 1998, 24, 883–885. [Google Scholar] [CrossRef]
- Nelson, M.; Naismith, D.J.; Burley, V.; Gatenby, S.; Geddes, N. Nutrient Intakes, Vitamin-Mineral Supplementation, and Intelligence in British Schoolchildren. Br. J. Nutr. 1990, 64, 13–22. [Google Scholar] [CrossRef]
- Schoenthaler, S.J.; Amos, S.P.; Eysenck, H.J.; Peritz, E.; Yudkin, J. Controlled Trial of Vitamin-Mineral Supplementation: Effects of Intelligence and Performance. Personal. Individ. Differ. 1991, 12, 351–362. [Google Scholar] [CrossRef]
- Southon, S.; Wright, A.J.A.; Finglas, P.M.; Bailey, A.L.; Loughridge, J.M.; Walker, A.D. Dietary Intake and Micronutrient Status of Adolescents: Effect of Vitamin and Trace Element Supplementation on Indices of Status and Performance in Tests of Verbal and Non-Verbal Intelligence. Br. J. Nutr. 1994, 71, 897–918. [Google Scholar] [CrossRef] [PubMed]
- Vinodkumar, M.; Rajagopalan, S.; Vinodkumar, M.; Rajagopalan, S. Efficacy of Fortification of School Meals with Ferrous Glycine Phosphate and Riboflavin against Anemia and Angular Stomatitis in Schoolchildren. Food Nutr. Bull. 2009, 30, 260–264. [Google Scholar] [CrossRef]
- The World Bank. World Bank Country and Lending Groups. Available online: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (accessed on 24 February 2020).
- Deary, I.J.; Pattie, A.; Starr, J.M. The Stability of Intelligence from Age 11 to Age 90 Years: The Lothian Birth Cohort of 1921. Psychol. Sci. 2013, 24, 2361–2368. [Google Scholar] [CrossRef]
- Plomin, R.; von Stumm, S. The New Genetics of Intelligence. Nature reviews. Genetics 2018, 19, 148–159. [Google Scholar]
- Walker, S.; Grantham-McGregor, S.; Powell, C.; Chang, S. Effects of Growth Restriction in Early Childhood on Growth, IQ, and Cognition at Age 11 to 12 Years and the Benefits of Nutritional Supplementation and Psychosocial Stimulation. J. Pediatr. 2000, 137, 36–41. [Google Scholar] [CrossRef]
- Khor, G.L.; Misra, S. Micronutrient Interventions on Cognitive Performance of Children Aged 5-15 Years in Developing Countries. Asia Pac. J. Clin. Nutr. 2012, 21, 476–486. [Google Scholar]
- Lam, L.F.; Lawlis, T.R. Feeding the Brain—The Effects of Micronutrient Interventions on Cognitive Performance among School-Aged Children: A Systematic Review of Randomized Controlled Trials. Clin. Nutr. 2017, 36, 1007–1014. [Google Scholar] [CrossRef]
- Finkelstein, J.L.; Fothergill, A.; Hackl, L.S.; Haas, J.D.; Mehta, S. Iron Biofortification Interventions to Improve Iron Status and Functional Outcomes. Proc. Nutr. Soc. 2019, 78, 197–207. [Google Scholar] [CrossRef]
- Grantham-McGregor, S.; Ani, C. A Review of Studies on the Effect of Iron Deficiency on Cognitive Development in Children. J. Nutr. 2001, 131, 649S–668S. [Google Scholar] [CrossRef]
- Pasricha, S.; Gheorghe, A.; Sakr-Ashour, F.; Arcot, A.; Neufeld, L.; Murray-Kolb, L.; Suchdev, P.; Bode, M. Net Benefit and Cost-Effectiveness of Universal Iron-Containing Multiple Micronutrient Powders for Young Children in 78 Countries: A Microsimulation Study. Lancet Glob. Health 2020, 8, e1071–e1080. [Google Scholar] [CrossRef]
- UNESCO. Institute of Statistics Data for the Sustainable Development Goals. Available online: http://uis.unesco.org/ (accessed on 21 February 2021).
- UNESCO. Institute of Statistics Learning Outcomes. Available online: http://uis.unesco.org/en/topic/learning-outcomes (accessed on 21 February 2021).
- Nutrition International. Helping Adolescent Girls in Indonesia Reach Their Full Potential. Available online: https://www.nutritionintl.org/project/mitra-youth/ (accessed on 21 February 2021).
- United Nations. Children’s Fund (UNICEF) Programming Guidance: Nutrition in Middle Childhood and Adolescence; United Nations: New York, NY, USA, 2021. [Google Scholar]
- Bhardwaj, A.; Murage, L.; Sharma, S.; Dipo, D.; Makena, C.; Roche, M.; Arabi, M. Weekly Iron and Folic Acid Supplementation and Nutrition Education for Adolescent Girls in Africa and Asia. Field Exch. 2021, 66, 40. [Google Scholar]
- Roche, M.L.; Bury, L.; Yusadiredja, I.N.; Asri, E.K.; Purwanti, T.S.; Kusyuniati, S.; Bhardwaj, A.; Izwardy, D. Adolescent Girls’ Nutrition and Prevention of Anaemia: A School Based Multisectoral Collaboration in Indonesia. BMJ 2018, 363, k4541. [Google Scholar] [CrossRef] [PubMed]
- McCulloch, A.; Joshi, H. Neighbourhood and Family Influences on the Cognitive Ability of Children in the British National Child Development Study. Soc. Sci. Med. 2001, 53, 579–591. [Google Scholar] [CrossRef]
- Edefonti, V.; Rosato, V.; Parpinel, M.; Nebbia, G.; Fiorica, L.; Fossali, E.; Ferraroni, M.; Decarli, A.; Agostoni, C. The Effect of Breakfast Composition and Energy Contribution on Cognitive and Academic Performance: A Systematic Review. Am. J. Clin. Nutr. 2014, 100, 626–656. [Google Scholar] [CrossRef] [PubMed]
- Wachs, T.D. The Nature and Nurture of Child Development. Food Nutr Bull. 1999, 20, 7–22. [Google Scholar] [CrossRef]
- World Health Organization. Guideline: Daily Iron Supplementation in Adult Women and Adolescent Girls; World Health Organization: Geneva, Switzerland, 2016.
- World Health Organization. Guideline: Daily Iron Supplementation in Infants and Children; World Health Organization: Geneva, Switzerland, 2016.
- World Health Organization. Guideline: Intermittent Iron and Folic Acid Supplementation in Menstruating Women; World Health Organization: Geneva, Switzerland, 2011.
- Samson, K.L.I.; Loh, S.P.; Lee, S.S.; Sulistyoningrum, D.C.; Khor, G.L.; Mohd Shariff, Z.; Ismai, I.Z.; Yelland, L.N.; Leemaqz, S.; Makrides, M.; et al. Weekly Iron-Folic Acid Supplements Containing 2.8 Mg Folic Acid Are Associated with a Lower Risk of Neural Tube Defects than the Current Practice of 0.4 Mg: A Randomised Controlled Trial in Malaysia. BMJ Glob. Health 2020, 5, e003897. [Google Scholar] [CrossRef] [PubMed]
- Roche, M.L.; Samson, K.L.I.; Karakochuk, C.D.; Green, T.J.; Martínez, H. Perspective: Weekly Iron and Folic Acid Supplementation (WIFAS): A Critical Review and Rationale for Inclusion in the Essential Medicines List to Accelerate Anemia and Neural Tube Defects Reduction. Adv. Nutr. 2021, 12, 334–342. [Google Scholar] [CrossRef]
- Nutrition International. Women and Girls’ Nutrition. Available online: https://www.nutritionintl.org/what-we-do/by-programs/women-girls-nutrition/ (accessed on 17 April 2020).
- De-Regil, L.M.; Jefferds, M.E.D.; Sylvetsky, A.C.; Dowswell, T. Intermittent Iron Supplementation for Improving Nutrition and Development in Children under 12 Years of Age. Cochrane Database Syst. Rev. 2011, 12, CD009085. [Google Scholar] [CrossRef] [PubMed]
- Low, M.S.Y.; Speedy, J.; Styles, C.E.; De-Regil, L.M.; Pasricha, S.-R. Daily Iron Supplementation for Improving Anaemia, Iron Status and Health in Menstruating Women. Cochrane Database Syst. Rev. 2016, 4, CD009747. [Google Scholar] [CrossRef]
- Fernandez-Gaxiola, A.; De-Regil, L. Intermittent Iron Supplementation for Reducing Anaemia and Its Associated Impairments in Adolescent and Adult Menstruating Women. Cochrane Database Syst. Rev. 2019, 1, CD009218. [Google Scholar] [PubMed]
- De-Regil, L.M.; Jefferds, M.E.D.; Peña-Rosas, J.P. Point-of-Use Fortification of Foods with Micronutrient Powders Containing Iron in Children of Preschool and School-Age. Cochrane Database Syst. Rev. 2017, 11, CD009666. [Google Scholar] [CrossRef] [PubMed]
- Das, J.K.; Salam, R.A.; Mahmood, S.B.; Moin, A.; Kumar, R.; Mukhtar, K.; Lassi, Z.S.; Bhutta, Z.A. Food Fortification with Multiple Micronutrients: Impact on Health Outcomes in General Population. Cochrane Database Syst. Rev. 2019, 12, CD011400. [Google Scholar] [CrossRef] [PubMed]
- de Jager, C.A.; Dye, L.; de Bruin, E.A.; Butler, L.; Fletcher, J.; Lamport, D.J.; Latulippe, M.E.; Spencer, J.P.; Wesnes, K. Criteria for Validation and Selection of Cognitive Tests for Investigating the Effects of Foods and Nutrients. Nutr. Rev. 2014, 72, 162–179. [Google Scholar] [CrossRef]
- World Health Organization. Haemoglobin Concentrations for the Diagnosis of Anaemia and Assessment of Severity; World Health Organization: Geneva, Switzerland, 2011.
| Author (Year, Country) | Study Design | Study Population 1 | Exposure or Nutrition/Anemia Status | Learning/Cognition Outcome Assessed and Measure | Key Results 2 |
|---|---|---|---|---|---|
| Abalkhail et al. (2002, Saudi Arabia) [18] | Cross-sectional study | n = 800 school children aged 9–21 y Age: 14 ± 2.6 y | Prevalence of anemia was assessed using Hb estimated by Refletron (Boehringer Mannheim). | School grades were classified according to the national school grading classification. | Higher percentage of anemia among students with marks < 70% (fail/pass) than students with good, very good or excellent grades (no statistical analyses). |
| Anuar Zaini et al. (2005, Malaysia) [19] | Cross-sectional study | n = 1405 standard four primary students, aged 9–10 y Age: 9.7 ± 0.5 y (68% were 10 y) | Prevalence of anemia from finger-prick blood samples with a HemoCue®. | School grades in Malay language (comprehension and written), math, English, and science. RCPM for intelligence. | Severe anemics had higher scores in Malay language comprehension and writing, math, and English; lower science scores and RCPM. Moderate anemics had lower science scores and RCPM (no statistical analyses). |
| Aquilani et al. (2011, Italy) [20] | Cross-sectional study | n = 48 high school girls aged 14–15 y Age: 14.6 ± 0.7 y | Daily iron intake (mg) was assessed by a student-kept weighted 7 day food record and analysis was conducted using a computer system designed by the research group. | School achievement was assessed by mid-year curriculum performance in written math, oral math, and written Italian. | Students with satisfactory school performance had higher iron intakes than those with unsatisfactory scores **. Iron intake was significantly positively correlated with written math (r = 0.43 ***), oral math (r = 0.40 **) and written Italian (r = 0.37 *). |
| Cai and Yan (1990, China) [21] | Cross-sectional study | n = 58/478 middle school students aged 13–15 y | Prevalence of IDA was assessed using a 5 mL venous blood sample for Hb, ferritin, and free erythrocyte porphyrin. | IQ was tested using the Bourden–Wisconsin test. School marks in Chinese, math, and English class were taken from school records. | No significant difference in scores for verbal IQ, performance IQ, total IQ, or school marks by subject for students with IDA compared with those without IDA. |
| Carruyo-Vizcaíno et al. (1995, Venezuela) [22] | Cross-sectional study | n = 213 middle-class adolescents ages 12–17 y Age: 13.8 ± 1.3 y | Prevalence of ID and anemia was determined using a CBC, SI, TIBC, TS, and ferritin. | IRA was the ratio between the number of subjects approved over the total number of subjects taken. The final GPA from grades of each subject from three periods of the school year | IRA scores positively correlated with ferritin levels < 20 ug/L (r = 0.411 **); negatively correlated with Hb, iron, and ferritin in the total population (not shown); anemic males scored worse than non-anemic males * and all non-anemic adolescents **; no differences in average scores for any other blood parameters. Hb in females was negatively correlated with GPA; no differences in final GPA were found for any blood parameters. |
| Dissanayake et al. (2009, Sri Lanka) [23] | Cross-sectional study | n = 188 Sinhalese students age 13–15 y | Prevalence of ID and IDA was assessed by Hb, determined by the indirect cyanmethemoglobin method, and ferritin. | RPM for intelligence. School marks in science, math, social science, and Sinhala language, and total marks. | No significant relationship was observed between IQ or school performance and iron status or severity of ID. |
| El Hioui et al. (2012, Morocco) [24] | Cross-sectional study | n = 259 primary school children aged 6–16 y Age: 10.2 ± 2.48 y | Prevalence of IDA and anemia was assessed by CBC and ferritin. | RPM for intelligence. School achievement was assessed by the students’ scores in math GPA, cumulative GPA, and rank. | More anemic children had an intellectual deficit *; RPM performance related to Hb level ***. Ferritin was correlated with math (r = 0.5 *) and cumulative GPA (r = 0.37 *); math GPA was related to Hb level *; iron status related to school achievement ****. |
| Goudarzi et al. (2008, Iran) [25] | Cross-sectional study | n = 540 students aged 11–17 y Age: 14.9 ± 1.2 y | Prevalence of ID was assessed by SI, TIBC, and ferritin. | RPM for intelligence. | No significant difference in IQ scores or IQ classification among students with ID, IDA or normal iron status. |
| Halliday et al. (2012, Kenya) [17] | Cross-sectional RCT baseline analyses | n = 2400 students aged 5–18 y Age: 10.3 y | Prevalence of anemia was assessed using a portable hemoglobinometer. | Attention was assessed by pencil-tap test and the code transmission test. RPM for non-verbal reasoning. | Anemia status was not associated with attention, literacy, non-verbal reasoning, comprehension, or numeracy skills. |
| Halterman et al. (2001, USA) [26] | Cross-sectional study | n = 5398 children aged 6–16 y (61.3% were 6–11 y, 38.7% were 12–16 y) | Prevalence of ID and IDA was determined by TS, ferritin, erythrocyte protoporphyrin, and Hb. | WISCR: verbal component (digit span) and performance examination (block design). WRAT: math and reading components. | For all categories, scores lowered with diminishing iron status. IDA and ID did not score differently than normal status for reading and digit span (ns). For reading, block design, and digit span the % scoring below average did not differ by iron status. ID was not at increased odds of scoring below average for reading, block design, or digit span (ns) but IDA scored lower than children with normal status *. IDA and ID had lower math scores * and had higher risk of scoring below average (OR 2.3; 95% CI: 1.1,4.4). |
| Hutchinson et al. (1997, Jamaica) [27] | Cross-sectional study | n = 800 rural students in grade 5 aged 9–13 y Age: 10.8 ± 0.6 y | Prevalence of anemia was assessed by portable hemoglobinometer. Samples were obtained from 769 children. | WRAT: reading, spelling and math subtests. | Hb was significantly positively correlated with reading and spelling scores but not correlated with math scores. |
| Ivanovic et al. (2004, Chile) [28] | Cross-sectional study | n = 4509 students ages 5–22 y Age: 10.4 ± 3.5 y | Daily iron intake (% of adequacy) from 24 h dietary recall data by individual interviews. | School achievement was evaluated through standard Spanish-language and math achievement tests designed for the study. | Iron intake (% daily value) was correlated with scholastic achievement for the whole sample (r = 0.065 ***). By grade, this positive correlation was only significant in grade 4 high school students (r = 0.142 *). NS for grade 1 high school, grade 6 or 8. |
| Ji et al. (2017, China) [29] | Cross-sectional study | n = 428 elementary school students aged 11–14 y Age: 12.0 ± 0.4 y | Prevalence of ID from Hb and SI. | CNB was used for performance accuracy and speed in four neurobehavioral domains. Chinese version of the WISCR was used to measure intelligence. | Only one difference in mean raw CNB scores was found * which was ns after adjustment. ID had longer reaction times on tests of mental flexibility and capacity for abstraction and the test of special processing ability *. High SI had slower speed on tests of spatial processing ability * and had decreased abstraction ability and mental flexibility *. Iron status was associated with the full-scale IQ score (ns). |
| Kharat and Waghmare (2015, India) [30] | Cross-sectional study | n = 74 adolescent girls aged 18–19 y | Prevalence of anemia was assessed by Hb concentration, tested by the cyanmethemoglobin method. | Cognitive performance was assessed with P300 using an odd ball paradigm with an RMSEMG EP II machine. | Anemic group had delayed P300 latencies as compared with the control group ****. The P300 amplitudes were larger in the girls in the control group than the anemic group *. |
| Masalha et al. (2008, Israel) [31] | Cross-sectional study | n = 67 fourth, fifth, and sixth graders ages 9–11 y. | Prevalence of anemia was assessed using venous blood was used. | Academic Achievement Index was calculated as the ratio of all marks achieved of all approved courses over the total. Low achievement was classified as scores < 80%. | Of the 14 children with anemia, 6 had low academic achievement scores (42.9%). (no statistical analyses reported.) |
| More et al. (2013, India) [32] | Cross-sectional study | n = 87 girl aged 12−15 y studying in sixth to ninth standard | Screening for anemia and ID was performed by CBC and ferritin. | School achievement was assessed by math score from the final term exam on report cards. Multicomponent Test for verbal learning, memory, and attention; PGI test; and Bhatia battery performance test. | Scholastic performance, IQ, and scores of mental balance, attention and concentration, verbal memory, and recognition were decreased in iron-deficient girls, both anemic and non-anemic, as compared with the non-iron-deficient girls *. |
| Nagalakshmi et al. (2015, India) [33] | Cross-sectional study | n = 60 rural school children aged 9–12 y Age: 10.4 ± 1.1 y | Hb level was assessed using Sahli’s acid hematin method. | Visual reaction time; whole-body reaction time, and MMSE. | Whole-body reaction time was negatively correlated with Hb ***. Visual reaction time and MMSE were negatively correlated with Hb (ns). |
| Nemati et al. (2005, Iran) [34] | Cross-sectional study | n = 170 adolescent girls Age: 12 y | Prevalence of IDA and anemia from venous blood samples. Measured Hb, hematocrit, MCV, TIBC, and ferritin. | “Educational progression including average test score of base class primary school for schoolgirls”. Test scores (/20) were classified as low (10–15) and high (15.1–20). | Anemics had lower test scores than those without anemia *. IDA had significantly lower test scores than those without IDA *. ID did not have significantly lower test scores than those without ID. Hb was correlated with average test score (r = 0.171 *). Ferritin was not significantly correlated. |
| Olson et al. (2009, Philippines) [35] | Cross-sectional study | n = 322 rural school students aged 7–18 y Age: 12.1 (95% CI: 11.7,12.4) y | Prevalence of IDA and anemia from a CBC by hematology analyzer on venous blood samples. Ferritin, sTfR were also measured for iron status. | WRAML, verbal fluency, and PNIT. | Students with IDA and NIDA had lower non-verbal intelligence scores than students with no anemia **. After adjustment, anemia status showed no effect on WRAML learning index, but children with NIDA scored worse than children without anemia on the verbal memory component *. Anemia status, regardless of type, had no significant effect after adjustment on verbal fluency. |
| Ortega et al. (1993, Spain) [36] | Cross-sectional study | n = 64 middle-class adolescents aged 15–18 y Age: 15.9 ± 0.8 y | Iron intake was quantified using the 5 day “food consumption registration” technique. Fasting venous blood samples were used for a CBC measured using a Coulter S analyzer Plus. SI was also measured. | Spanish TEA for verbal, reasoning, and calculus. IQ percentile (IQ < or > 100) is calculated from total scores. The attention test consisted of clearly crossing out all the letters that were accompanied by two apostrophes and the hits, errors, omissions, and speed were recorded. School grades for Latin, Spanish language, foreign language, geography, religion-ethics, math, physics-chemistry, physical education, and technical-professional activities were obtained. | In girls, ID was associated with lower scores for verbal, calculus, school aptitude, and IQ *; higher IQ had higher Hb *; iron status was not associated with school grades. In boys, ID was associated with lower factor scores for verbal, reasoning, school aptitude, attention speed, grades in physics and chemistry *; ferritin was positively associated with IQ percentile *. Overall, Hb was associated with calculus score (r = 0.2905 *), but not attention, verbal scores, reasoning scores, or overall TEA global scores. Ferritin was associated with attention hits (r = 0.3434 *) and speed (r = 0.3989 *). Iron intake was negatively associated with attention hits (r = −0.2874 *) but not IQ percentile. SI was associated with none of the above scores. |
| Sen and Kanani (2006, India) [37] | Cross-sectional study | n = 350 low-income adolescent girls aged 9–14 y | Prevalence of anemia was measured with Hb by the cyanmethemoglobin method. | Gujarati version of WISC: digit span test for short-term memory, maze test for visual–motor coordination, Clerical task for concentration and ability to discriminate, and visual memory test for short-term memory. | Girls with anemia performed worse on the digit span test and visual memory tests in both 9–11 and 12–14 age ranges *. No difference in performance on the maze test or clerical task by anemia statuses. |
| SoonMyung et al. (2004, Korea) [38] | Cross-sectional study | n = 193 adolescent girls aged 11–14 y Age: 12.6 ± 0.6 y | Prevalence of anemia through Hb was measured using an Automatic Blood Cell Counter. SI, TIBC, and ferritin were also measured. | Questionnaire regarding clinical symptoms of anemia was administered. Decreased ability to concentrate and poor memory were measured using Likert-type scales. | Hb and ferritin were not significantly correlated with decreased ability to concentrate and poor memory. |
| Teni et al. (2017, Ethiopia) [39] | Cross-sectional study | n = 442 adolescent girls aged 10–19 y Age: 14.2 ±1.7 y | Prevalence of anemia measured by the HemoCue (Hb 301) system. | Average scores in the school were obtained from the school records. | Anemic girls were more likely to show low academic performance, compared with non-anemic girls (AOR = 1.7; 95% CI: 1.2, 2.7 *). More anemic girls had academic performance below the mean compared with non-anemic girls (71.1 vs. 64.5%) (no statistics analyses). |
| Thalanjeri et al. (2016, India) [40] | Cross-sectional study | n = 30 school going children both males and females between the ages of 9 and 13 y | Prevalence of anemia was assessed through venous blood was collected for a CBC using a semi-auto hematology analyzer. | Visual memory test and RPM. | RPM scores were lower in anemic children as compared with non-anemic children ***. No significant correlation between Hb and the visual memory test. |
| Walker et al. (1998, Jamaica) [41] | Cross-sectional study | n = 452 adolescent girls aged 13–14 y in grade 8 | Prevalence of anemia using Hb measured by an automated method on a Cell Dyn 700 cell counter. | School achievement using the WRAT for spelling, reading, and arithmetic. Scores on the test were converted to grade levels. | Anemia was associated with lower achievement levels in reading and spelling **. |
| Webb and Oski (1973, USA) [42] | Cross-sectional study | n = 193 students ages 12–14 y in a junior high school low SES black community | Prevalence of anemia assessed by CBC using the Coulter Counter, Model S. | School achievement using the composite score of the Iowa Tests of Basic Skills. | Anemic subjects differed from non-anemic subjects in composite scores achieved *. Anemic girls aged 12 y scored better than non-anemic girls. All other anemic subjects scored worse than non-anemic subjects. |
| Author (Year, Country) | Study Design | Population 1 | Exposure | Learning and Cognition Outcome Assessment Method | Key Results 2 |
|---|---|---|---|---|---|
| Food-based interventions | |||||
| Kalaichelvi (2016, India) [43] | Randomized, controlled trial (Dissertation) | n = 240 adolescent girls with anemia in the age group of 12–15 y | 8 weeks; intervention given 5 days a week (Monday to Friday):
| Malin’s intelligence scale for Indian children for verbal response, general information, arithmetic, similarities and digit span and in performance, picture completion, object assembly, coding, and maze. | Intelligence scores increased in the treatment group *, no change in control group; post-test scores were higher in anemic girls in treatment group than anemic controls ***; positive correlation between Hb level and intelligence score (r = 0.84 **). |
| Karkada et al. (2019, India) [12] | Quasi-experimental trial | n = 60 semi-rural adolescent girls aged 11–17 y | 90 days; twice-daily intervention:
| The scholastic performance was determined by exam percentage scores before data collection. | No statistically significant changes in school performance were found following the intervention. |
| Khan et al. (2004, Bangladesh) [44] | Randomized, double-blind, placebo-controlled trial | n = 317/1268 adolescent girls aged 11–14 y selected for cognitive testing and n = 697/1268 for school achievement test Age: 12.0 y | 12 months; each subject received one 200 mL serving of the constituted beverage for six days a week (Saturday to Thursday).
| RCPM and tests of verbal fluency, visual search, and free recall. WRAT containing sections of spelling and arithmetic. | After 12 mo., intervention group scored higher in spelling ** and math ** than placebo. In non-anemic girls, a negative trend in visual search test scores was seen in the intervention compared with placebo *; no difference in anemic. No difference in between groups for free recall, RCPM and verbal fluency; anemic supplemented girls trended better than anemic placebo girls in RCPM and verbal fluency (ns). |
| Muthayya et al. (2012, India) [45] | Randomized, double-blind, controlled, school feeding trial | n = 401 urban and rural primary school children aged 6–15 y Age: 10.4 y | 7 months; daily lunch 6 days/week:
| Cognitive tests used were the Atlantis, Kohs block design, word order, pattern reasoning, verbal fluency, and coding WISC-III. | No effect of treatment on cognitive performance after adjusting for baseline scores. No significant interaction effect of treatment for gender, grouping, ferritin, or body iron store. |
| Scott et al. (2018, India) [46] | Double-blind, randomized, intervention study | n = 140 rural students (aged 12–16 y) Age: 13.7 y | 6 months; 200–300 g (dry) pearl millet/d in the form of bhakri during lunch and dinner:
| Five cognitive/behavioral tasks (3 attention tasks and 2 memory tasks) were administered on laptop computers: SRT, GNG for sustained attention and speed of simple attentional capture, ANT, CFE, and CRT. | The consumption of biofortified pearl millet resulted in greater improvement in attention (SRT, GNG, and ANT) and memory (CFE and CRT **). Reaction time decreased twice as much from 0 to 6 mo. in those consuming biofortified on attention tasks **. |
| Solon et al. (2003, Philippines) [47] | Randomized, double-blind, placebo-controlled field efficacy trial | n = 808 children in grades 1–6 Age: 9.95 y | 16 weeks; 200 mL serving of either fortified or non-fortified beverage twice each school day:
| Primary Mental Abilities Test for Filipino Children for three basic mental abilities: verbal, non-verbal, and quantitative. | Fortified beverage showed no significant effect on change in total cognitive scores for all subjects. Among moderate to severe anemics at baseline, children receiving the fortified beverage showed improvement in changes in non-verbal ability score *. |
| Sorensen et al. (2015, Denmark) [14] | Cluster-randomized trial with cross-over design (baseline analysis only) | n = 726 Danish third- and fourth-grade children ages 8–11 y Age: 10.0 ± 0.6 y | 3 months cross-over (6 months total) on school days:
| At baseline and at the end of each study period (3 mo and 6 mo.), three tests related to concentration and school performance were administered: d2 Test of attention, the Sentence Reading Test 2, and a math test. | Low iron was associated with poor school performance in girls but not boys *. Children with low iron scored worse for attention and concentration ***. Iron stores were not associated with math scores. Girls with low iron had a worse reading speed and lower number of correct sentences ***. Boys with low iron had higher reading speed and correct number of sentences ***. Low iron was associated with a higher % correct in reading and was associated with reading comprehension in both sexes *. |
| Vazir et al. (2006, India) [15] | Double-blind, placebo-controlled, matched-pair, cluster, randomized feeding trial | n = 608 middle-income semi-urban children ages 6–15 y Age: 10.7 y | 14 months; beverage was served twice daily:
| Knox Cube Imitation Test and Letter Cancellation Test for attention, Malin’s Intelligence Scale for Indian Children, and PGI Memory Scale. School marks in science, math, and social studies and aggregate marks of quarterly and final annual examinations were used. | Supplementation significantly improved attention and concentration **. Supplementation made no significant improvements on IQ scores, memory scores, or school achievement. |
| Vinodkumar et al. (2009, India) [48] | Randomized controlled trial | n = 162/323 children aged 5–18 y Age: 12.3 y | 9 months of school meals fortified with:
| Memory tests were given to children aged 11–18 years. | Memory scores of the experimental group were significantly higher than those of the control group, repeated-measures ANOVA showed a group x time interaction *. Treatment group showed significant improvement in memory scores compared with control group. |
| Iron-only supplementation interventions | |||||
| Ballin et al. (1992, Israel) [49] | Double-blind, placebo-controlled prospective study (trial) | n = 59 urban, middle-class high school girls aged 16–17 y | 2 months; once-daily intervention:
| Questionnaires were given for information about lassitude, fatigue, the ability to concentrate in school, mood, appetite, and quality of sleep. | Girls who received the iron intervention reported significant improvement in lassitude *, the ability to concentrate in school *, and mood *. |
| Bruner et al. (1996, USA) [50] | Double-blind, placebo-controlled randomized clinical trial | n = 81 high school girls aged 13–18 y | 8 weeks; twice-daily intervention:
| Brief Test of Attention for auditory attention; Symbol Digit Modalities Test for visual attention, motor speed, and rapid coding; Visual Search and Attention Test for visual scanning, target detection, and cancellation; HVLT for recall and recognition | Iron treatment had no significant effect on post-intervention Brief Test of Attention, Symbol Digit Modalities Test, Visual Search and Attention Test, or Hopkins Verbal Learning Test scores. |
| Chellappa and Karunanidhi (2012, India) [51] | Randomized, double-blind, placebo-controlled, intervention trial | n = 109 low and middle income 17–19 y adolescent girls Age: 18.4 y | 16 weeks; once-daily intervention:
| Digit Symbol Substitution Test for mental speed, Digit Vigilance test for sustained attention, Standard Progressive Matrices for abstract reasoning, the Rey Auditory Verbal Learning Test for verbal memory and recognition; Rey Complex Figure Test and PGI Memory Scale for visual memory and recognition. | Iron and FeZn supplementation produced significantly higher adjusted post-test scores for mental speed error component **; visual memory immediate ** and delayed recall * compared with placebo. No intervention improved sustained attention, abstract reasoning, immediate and delayed recall of verbal material, and verbal and visual recognition compared with placebo. |
| Devaki et al. (2009, India) [16] | Single-center prospective placebo-controlled study | n = 120 healthy adolescent girls and boys aged 15–18 y Divided into groups based on iron and anemia status | 8 months; once-daily intervention, 6 days a week:
| Cognitive performance was measured using: STM, LTM, RPM, WAIS. Scholastic performance was assessed by a math test. | All groups that received iron supplements had significantly improved test scores for STM, LTM, RPM, WAIS, and scholastic performance compared with the placebo group **. |
| Lambert et al. (2002, New Zealand) [52] | Randomized, double-blind intervention study | n = 116 female high school students aged 12.5–17.9 y with ID Age: 15.2 y | 8 weeks; once-daily intervention:
| HVLT, Stroop task, Visual Search task, and reading span task. | Reading span was positively correlated with ferritin (r = 0.250 **). Relationship between ferritin change scores and post-treatment reading span (B = 0.22 **) controlled for pre-treatment reading span. No significant relationship was found for delayed recall and recognition scores on the HVLT, Stroop task, or visual search task and iron treatment. |
| Rezaeian et al. (2014, Iran) [53] | Blind, controlled, clinical trial study | n = 200 female students aged 14–18 y Age: 16.2 ± 1.3 y | 16 weeks; twice-weekly supplementation:
| The Toulouse–Piéron test for attention score. | Iron supplementation was associated with a positive increase in attention scores ***. |
| Soemantri et al. (1989, Indonesia) [54] | Double-blind, randomized clinical trial | n = 130 primary school children aged 8.1–11.6 y Age: 10.5 y | 3 months of intervention followed by 3 months of no intervention:
| RCPM for general intelligence. An educational achievement test in math, biology, social science, and language. | Iron supplementation produced no significant effects on IQ at any time point. Iron treatment had a positive effect on learning in the anemic children in the four subject areas; scores improved in the non-anemic children for math and biology (no statistical analyses). |
| Soemantri et al. (1985, Indonesia) [55] | Randomized, placebo-controlled trial | n = 119 anemic and non-anemic school children. Age: 10.9 y | 3 months of intervention:
| Educational achievement test in math, biology, social science, and language. The Bourden–Wisconsin test for concentration. | Iron significantly improved adjusted school achievement scores. In anemics, the adjusted score of the iron group was significantly higher than the placebo group; no significant differences in non-anemics. Iron group had a significantly higher increase in concentration scores than placebo. |
| Umamaheswari et al. (2011, India) [56] | Intervention study | n = 100 upper-low SES randomly selected children ages 6–11 y (60% aged 9–11 y) | 3 months:
| Intelligence was assessed using the Binet–Kamath scale. Memory was tested using: digit forward, sentence repetition, story recall, picture recall, Benton visual retention test, and Cattell’s retentivity test. | ID children had lower verbal memory, non-verbal memory, and IQ scores than normal controls. After supplementation, ID children showed larger improvement scores for all fields compared with normal controls (no statistical analyses). |
| Iron plus additional micronutrients supplementation interventions | |||||
| Haskell et al. (2008, England) [57] | Randomized, double-blind, placebo-controlled, parallel groups trial | n = 81 children aged 8–14 y Age: 11.1 y | 12 weeks; daily intervention at breakfast:
| Cognitive battery for the speed and accuracy of attention and aspects of memory (secondary, semantic, and spatial working). | No significant differences were found for any unadjusted mean scores at 12 weeks between the treatment and placebo group following micronutrient supplementation. |
| Lynn and Harland (1998, England) [58] | Placebo-controlled trial | n = 413 comprehensive school students aged 12–16 y Age: 13.1 y | 16 weeks; once-daily intervention:
| RPM were used, raw scores on the matrices were transformed to age-standardized percentiles from the test manual and percentiles were transformed to IQs. | Overall, there were no significant changes in IQ following the treatment period for either group. For participants with low and high ferritin levels, following treatment, the gain in IQ points was higher in the treatment group than placebo *. |
| Nelson et al. (1990, England) [59] | Randomized, double-blind, placebo-controlled trial | n = 227 school children aged 7–12 y | 4 weeks; once-daily intervention:
| Children 7–10 y completed the Heim AHlX test of non-verbal intelligence, and children 11–12 y completed the Heim AH4 test of verbal and non-verbal intelligence. All children completed the WISCR digit span and coding tests. | The supplement did not affect intelligence. |
| Schoenthaler et al. (1991, USA) [60] | Randomized, triple-blind placebo-controlled trial | n = 615 8th graders (aged 12–13 y) and 10th graders (aged 15–16 y) | 13 weeks; each student took one dose Tues to Thurs with a double dose on Mon and Fri:
| WISCR, MAT, RT/IT, and CTBS. RPM after one month of supplementation, no retest. | For WISCR, gains in the 100% RDA group vs. the placebo in non-verbal intelligence *, primarily due to gains in object assembly, coding, and picture arrangement. No difference in the 50% nor 200% group and supplementation did not affect verbal intelligence. Treatment only produced an effect over the placebo group for 3/13 components in CTBS: comprehension, battery, and reading *. Treatment did not affect MAT and RPM. |
| Sen and Kanani (2009, India) [13] | Cluster randomized, control trial | n = 161 girls in Standards V–VI aged 9–13 y | One year of interventions:
| Gujarati version of WISC: digit span for short-term memory; maze test for visual–motor coordination and speed, and fine motor coordination; visual memory test for short-term memory; and Clerical task for concentration and discrimination. | Experimental subjects showed a higher increase in test scores than controls. Overall, IFA-Daily and IFA-2Wkly showed improvements in most tests, while IFA-1Wkly consistently showed less improvement. Cognitive function scores were higher among those who gained more than 1 g/dL Hb (ns). |
| Southon et al. (1994, England) [61] | Placebo-controlled intervention trial | n = 51 adolescents aged 13–14 y Age: 13.8 y | 16 weeks, two capsules per day:
| WISC—Anglicized Revised Edition. | No treatment effect was observed on either total verbal or total non-verbal test scores in the subjects. |
| Study | Randomization | Intervention Deviations | Missing Data | Outcome Measurement | Selection of Reported Results | Overall |
|---|---|---|---|---|---|---|
| Food-based interventions | ||||||
| Kalaichelvi (2016) [43] | L | H | L | H | L | H |
| Karkada et al. (2019) [12] | L | H | L | U | H | H |
| Khan et al. (2004) [44] | L | L | L | L | U | S |
| Muthayya et al. (2012) [45] | L | L | L | L | L | L |
| Scott et al. (2018) [46] | L | L | L | L | L | L |
| Solon et al. (2003) [47] | L | L | L | L | L | L |
| Sorensen et al. (2015) [14] | L | L | L | L | L | L |
| Vazir et al. (2006) [15] | L | L | L | L | L | L |
| Vinodkumar et al. (2009) [48] | L | L | L | L | L | L |
| Iron-only supplementation interventions | ||||||
| Ballin et al. (1992) [49] | H | H | H | H | U | H |
| Bruner et al. (1996) [50] | L | L | L | U | U | S |
| Chellappa and Karunanidhi (2012) [51] | L | L | U | L | U | S |
| Lambert et al. (2002) [52] | L | U | L | L | U | S |
| Rezaeian et al. (2014) [53] | L | U | L | L | U | S |
| Soemantri et al. (1989) [54] | L | H | L | H | U | H |
| Soemantri et al. (1985) [55] | U | U | U | H | U | H |
| Umamaheswari et al. (2011) [56] | H | H | U | L | H | H |
| Iron plus additional micronutrients supplementation interventions | ||||||
| Haskell et al. (2008) [57] | L | L | L | L | L | L |
| Lynn and Harland (1998) [58] | L | L | L | U | H | H |
| Nelson et al. (1990) [59] | L | U | L | L | U | S |
| Schoenthaler et al. (1991) [60] | L | U | H | L | U | H |
| Sen and Kanani (2009) [13] | L | U | U | L | U | S |
| Southon et al. (1994) [61] | H | U | L | L | L | H |
| Study | Confounding | Participant Selection | Intervention Classification | Intervention Deviations | Missing Data | Measurement of Outcomes | Selection of Reported Results | Overall |
|---|---|---|---|---|---|---|---|---|
| Iron Supplementation Intervention | ||||||||
| Devaki et al. (2009) [16] | M | L | L | L | L | L | L | M |
| Observational Cross-Sectional Studies | 1. Clear Research Question | 2. Clear Study Population | 3. 50% Participation Rate | 4. Groups Recruited from the Same Population | 5. Sample Size Justification | 6. Exposure Assessed Prior to Outcome Measure | 7. Sufficient Timeframe to See Effect | 8. Different Levels of the Exposure of Interest | 9. Exposure Measures and Assessment | 10. Repeated Exposure Assessment | 11. Outcome Measures | 12. Blinding of Outcome Assessors | 13. Follow-Up Rate | 14. Statistical Analysis | Overall Quality Rating |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Abalkhail et al. (2002) [18] | Y | Y | Y | Y | N | N | N | N | Y | N | N | U | Y | N | Poor |
| Anuar Zaini et al. (2005) [19] | Y | Y | Y | Y | N | N | N | Y | U | N | N | U | U | N | Poor |
| Aquilani et al. (2011) [20] | Y | Y | U | Y | N | U | U | N | N | N | N | U | Y | N | Poor |
| Cai et al. (1990) [21] | Y | Y | U | Y | N | N | N | N | U | N | U | Y | U | U | Poor |
| Carruyo-Vizcaíno et al. (1995) [22] | Y | N | N | Y | N | N | N | Y | Y | N | U | U | U | N | Poor |
| Dissanayake et al. (2009) [23] | Y | U | Y | Y | N | N | N | Y | Y | N | Y | U | U | N | Poor |
| El Hioui et al. (2012) [24] | Y | Y | U | U | N | N | N | N | Y | N | Y | U | U | N | Poor |
| Goudarzi et al. (2008) [25] | Y | Y | U | U | N | N | N | N | U | N | Y | N | U | N | Poor |
| Halliday et al. (2012) [17] | Y | Y | Y | Y | Y | N | N | N | Y | N | Y | U | U | Y | Unclear |
| Halterman et al. (2001) [26] | Y | Y | Y | N | N | N | N | N | Y | N | Y | Y | U | Y | Poor |
| Hutchinson et al. (1997) [27] | Y | Y | Y | Y | Y | N | N | Y | Y | N | Y | N | U | Y | Unclear |
| Ivanovic et al. (2004) [28] | Y | Y | U | Y | Y | N | N | Y | N | N | Y | U | U | N | Poor |
| Ji et al. (2017) [29] | Y | Y | N | Y | N | N | N | Y | Y | N | Y | U | U | Y | Poor |
| Kharat et al. (2015) [30] | Y | N | U | Y | N | N | N | N | Y | N | Y | U | U | N | Poor |
| Masalha et al. (2008) [31] | Y | N | Y | Y | N | N | N | N | N | N | N | U | U | N | Poor |
| More et al. (2013) [32] | Y | Y | Y | Y | N | N | N | N | Y | N | Y | Y | U | N | Poor |
| Nagalakshmi et al. (2015) [33] | Y | N | U | Y | N | N | N | Y | N | N | Y | U | U | N | Poor |
| Nemati et al. (2007) [34] | Y | N | U | Y | N | N | N | Y | Y | N | N | U | U | N | Poor |
| Olson et al. (2009) [35] | Y | Y | Y | Y | N | N | N | Y | Y | N | Y | U | U | Y | Poor |
| Ortega et al. (1993) [36] | Y | N | U | U | N | N | N | Y | Y | N | U | U | U | N | Poor |
| Sen et al. (2006) [37] | Y | N | U | Y | N | N | N | Y | Y | N | Y | U | U | Y | Unclear |
| SoonMyung et al. (2004) [38] | N | N | U | Y | N | N | N | Y | Y | N | N | U | U | N | Poor |
| Teni et al. (2017) [39] | Y | Y | U | Y | Y | N | N | N | Y | N | N | U | U | N | Poor |
| Thalanjeri et al. (2016) [40] | N | N | U | Y | U | N | N | Y | Y | N | Y | U | U | N | Poor |
| Walker et al. (1998) [41] | Y | Y | N | Y | N | N | N | N | Y | N | Y | U | U | N | Poor |
| Webb et al. (1973) [42] | Y | N | N | Y | N | N | N | N | Y | N | Y | U | U | N | Poor |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Samson, K.L.I.; Fischer, J.A.J.; Roche, M.L. Iron Status, Anemia, and Iron Interventions and Their Associations with Cognitive and Academic Performance in Adolescents: A Systematic Review. Nutrients 2022, 14, 224. https://doi.org/10.3390/nu14010224
Samson KLI, Fischer JAJ, Roche ML. Iron Status, Anemia, and Iron Interventions and Their Associations with Cognitive and Academic Performance in Adolescents: A Systematic Review. Nutrients. 2022; 14(1):224. https://doi.org/10.3390/nu14010224
Chicago/Turabian StyleSamson, Kaitlyn L. I., Jordie A. J. Fischer, and Marion L. Roche. 2022. "Iron Status, Anemia, and Iron Interventions and Their Associations with Cognitive and Academic Performance in Adolescents: A Systematic Review" Nutrients 14, no. 1: 224. https://doi.org/10.3390/nu14010224
APA StyleSamson, K. L. I., Fischer, J. A. J., & Roche, M. L. (2022). Iron Status, Anemia, and Iron Interventions and Their Associations with Cognitive and Academic Performance in Adolescents: A Systematic Review. Nutrients, 14(1), 224. https://doi.org/10.3390/nu14010224






