Evidence Use in the Development of the Australian Dietary Guidelines: A Qualitative Study
Abstract
:1. Introduction
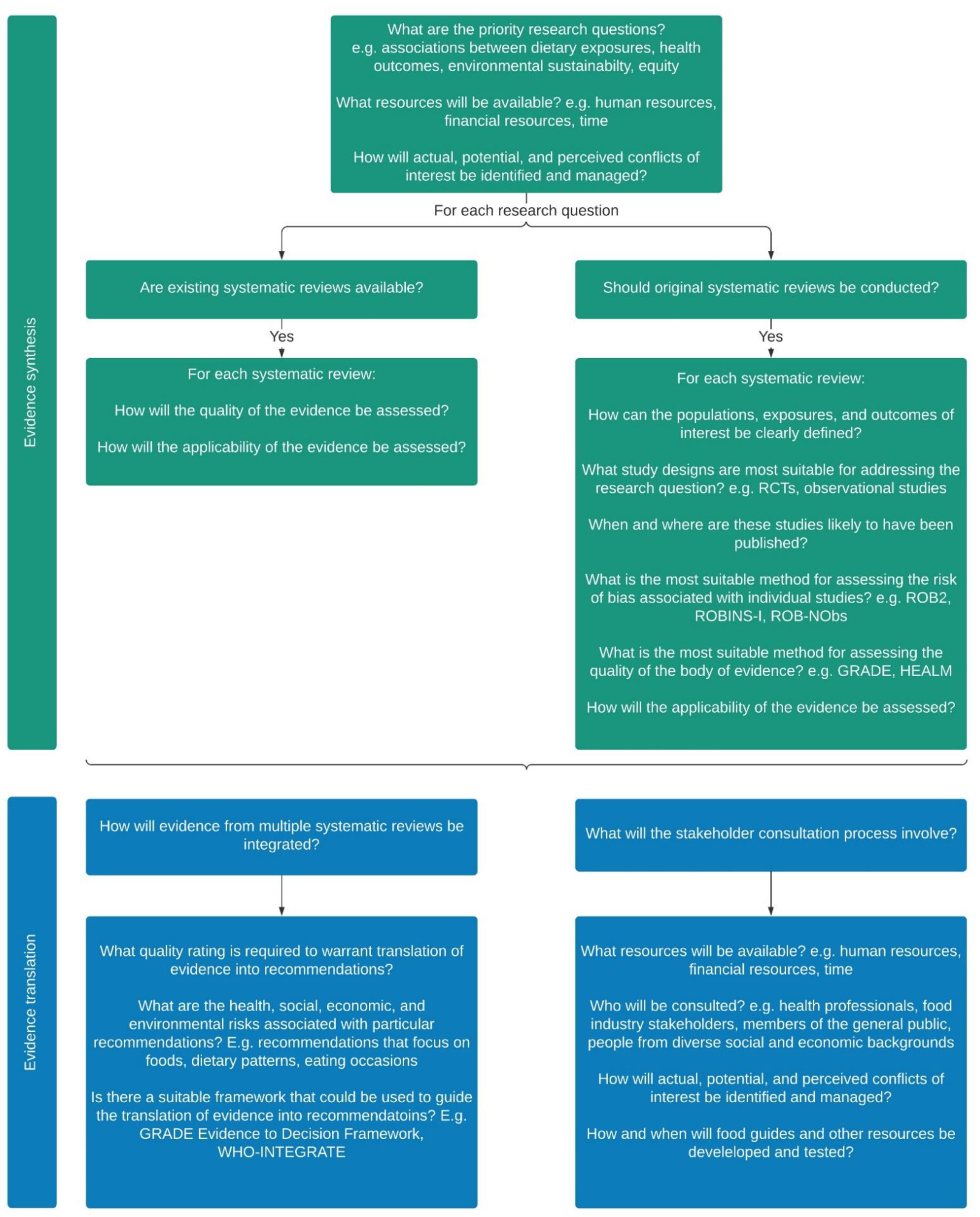
2. Materials and Methods
3. Results
3.1. Exposures and Outcomes of Interest
3.1.1. Dietary Exposures
“… if we’re defining health in terms of maximising functionality and preventing chronic disease, which is a public health goal, then we need to accept that it’s not a single food, it’s not a single nutrient, it’s actually a package, which we are now calling dietary patterns, which influences those outcomes, and it doesn’t happen quickly.”[Participant 3, Working Committee].
“… I guess if you’ve got a dietary pattern, it might not include all the different foods. Whereas if you’ve got food studies, for example, we know that fatty fish is high in omega-3. Those studies are still important, because that’s a strong source of that particular nutrient”[Participant 20, Review Team].
“… since we’re talking about the biological aspects, we do need to have a good understanding of the molecular basis for how food components influence health, and that’s actually the nutrient side of it. But it’s not just nutrients, it’s the things we don’t call nutrients, like phytocomponents, and it’s also the interaction between nutrients that occur within the food delivery system”[Participant 3, Working Committee].
3.1.2. Health Outcomes
3.1.3. Environmental Sustainability
“So the first thing I’d say is that you don’t even have to put those two things together. You don’t even have to say health and environmental sustainability, because anything that degrades environmental sustainability eventually degrades human health, and that’s becoming more and more accepted”[Participant 12, Review Team].
“We now have much more evidence than we had back then. And not just of modelling studies of actual observational data. So in terms of environment and food related health, so we’ve got much more data”[Participant 4, Working Committee].
3.1.4. Equity
“So if there’s anything I think we should be looking at, it’s the relationship between socioeconomic status and dietary intake. I’m not a food security expert by any means, I’ve just been an interested observer during the pandemic, and how people’s food skills, so utilisation has been poor, worse than that, we’ve got people economically doing it tough, not having enough to eat. So I think if there’s any time to be asking questions, that’s an important one to be asking of the literature”[Participant 22, Review Team].
3.2. Practicalities Associated with Evidence Synthesis
3.2.1. Planning the Evidence Review
“So rather than say, ‘go and do some dietary guidelines again’, it’s ‘we thought about how this needs to be done, now here’s the methodology’. And then it’s like the rules of the game have been stipulated before everyone goes on the field; it’s much more functional”[Participant 3, Working Committee].
3.2.2. Conducting Original Systematic Reviews
“… I remember specific points of discussion around, how is [meat] dealt with? You know, what’s red meat? What’s white meat? What’s processed meat? What’s not?”[Participant 17, Review Team].
“So we have to be prepared to stand back and look at the way in which evidence is constructed in different disciplines, because what you don’t want is to say we’re going to have to have a whole lot of systematic reviews [on environmental sustainability], find there’s two studies, and then find we can’t say anything, because there isn’t any research, but there’s probably a lot of research, it’s just not constructed in that way”[Participant 3, Working Committee].
“I think it’s always useful to have tools that are appropriate for the study designs and the questions being asked. Most of the risk of bias, certainly the Cochrane Risk of Bias tools, downgrade many nutrition studies, because of the problems with blinding, [but] blinding is quite difficult, so that needs to be managed in some way”[Participant 15, Review Team].
“I think on reflection, it would be good to have a system which is specific to dietary type studies, because you’re hardly ever going to get RCTs in this kind of field. They’re more likely to be cohort studies or large population studies. And that doesn’t make them bad. But when you rate them in traditional systems, they always look like low quality evidence. So I think whatever system that is used going forward, there needs to be a process for rating the evidence provided by those kinds of studies more appropriately”[Participant 20, Review Team].
“… my assumption would be that a lot of the [dietary pattern] studies would not be necessarily conducted in Australia, but they may be European or US studies that could be applied to our Australian context. Again, same thing in reverse, there may be some that may not be relevant at all. And we need to have a process in place where we start to work out, how do we deem them as relevant and what would then be appropriate to be considered for the Australian context”[Participant 9, Review Team].
“I think something that we’ve recognised is that the scientific literature has conflicts of interest within it. And we did include sources of funding. When we did the literature review, we extracted data on the sources of funding. But I think that this time, we would pay more careful attention to that, and perhaps highlight that”[Participant 21, Review Team].
“So I think it’s really important in the future that there’s a lot of oversight to make sure that we don’t have reviewers who have vested interests, [or] funding for other work”[Participant 2, Working Committee].
“I think you do need people who understand nutrition to do it. There’s lots of professional, systematic reviewing people, but honestly, if they don’t understand nutrition, it can lead to erroneous conclusions”[Participant 21, Review Team].
3.3. Practicalities Associated with Evidence Translation
3.3.1. Integrating the Evidence
“So theoretically, we might be getting reasonably close to saying, these are the combinations of foods that we think will give the best outcomes in terms of population health. But then you have to ask yourself, if the population is to consume this way, how good are we at providing it? And what is the impact on the environment of us producing it? What is the economic cost? Is this something that we trade in? How important is it from the point of view of the country’s GDP? And then the social side of it, which groups in our society actually eat like this? And what are the consequences of us saying they have to eat this other way?”[Participant 3, Working Committee].
“I guess one challenge with the dietary patterns approach is that any unhealthy food can be part of a healthy diet pattern, as far as our food industry friends would be concerned. So that’s a bit of a downside, in that we play into this rhetoric of, ‘it’s all about the total diet’ when really we do want to be highlighting some foods, all the discretionary foods basically, and having clear messages about those. I think that’s where it gets a bit difficult”[Participant 10, Working Committee].
“…I do wonder if as nutrition scientists, we actually should just get to the point where we call out what’s not a very healthy food and should be consumed in small amounts. And we all agree on that. If we just keep inventing classification after classification, and spending all our time on that, then it actually may play into the hands of interests that are not so interested in people having a healthy diet”[Participant 21, Review Team].
“… the more that we sort of broaden it out with other messages, the more the food industry can say ‘Well, it’s all about enjoyment. We have a dietary guideline about enjoying meals with families and family and friends. And here is our McDonald’s meal on a Friday’…”[Participant 10, Working Committee].
“I think we all have a bit of a short-term view of things, and we all feel a little bit invincible. So making it closer in terms of timeframes. So feeling well, not getting sick, being able to do the things that you want to do, so being able to enjoy life, particularly as people get older”[Participant 15, Review Team].
“So there’s two layers of evidence, first of all, which foods and which compounds in foods and which combinations of foods are best for health. And there could be a number of different ways you could eat, we know that. But then the second layer is, which of these combinations are achievable in terms of our cuisine, in terms of people’s food preferences, in terms of accessibility and sustainability for ensuring equitable food access?”[Participant 16, Review Team].
“… the food guide is essential in taking all of those technical reviews and all of the actual guidelines and translating that for the public. So if people with all of that skill and expertise are not involved in that really important next step, it sort of negates the process. Because if you can’t get the message across properly, then there’s no point in having dietary guidelines...”[Participant 16, Review Team].
3.3.2. Consulting Stakeholders
“… we always think that we know best, and we actually don’t know best, we don’t know what the consumer and what the person out there on the street, what message they receive. And we need to just be investing much more time in trying to understand that. But we’re not, we’re going to go through the whole process of doing a million [systematic reviews], synthesising the evidence, which is all good and well, but then we fail at the most important step, which is understanding how consumers understand”[Participant 16, Review Team].
“When you can say, look, we’re basing it on proper systematic reviews. And that was the good thing about the last one […] we could say, well, this was the evidence that we were using and this was why…”[Participant 1, Review Team].
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- FAO; WHO. Preparation and Use of Food-Based Dietary Guidelines. Report of a Joint FAO/WHO Consultation; World Health Organization: Geneva, Switzerland, 1998; Available online: http://www.who.int/iris/handle/10665/42051 (accessed on 7 June 2021).
- FAO. Developing Food Based Dietary Guidelines. A Manual from the English-Speaking Caribbean; Food and Agriculture Organization of the United Nations: Rome, Italy, 2007; Available online: http://www.fao.org/3/ai800e/ai800e00.htm (accessed on 7 June 2021).
- FAO. Food-Based Dietary Guidelines. Available online: http://www.fao.org/nutrition/education/food-dietary-guidelines/home/en/ (accessed on 7 April 2021).
- Wijesinha-Bettoni, R.; Khosravi, A.; Ramos, A.I.; Sherman, J.; Hernandez-Garbanzo, Y.; Molina, V.; Vargas, M.; Hachem, F. A snapshot of food-based dietary guidelines implementation in selected countries. Glob. Food Sec. 2021, 29. [Google Scholar] [CrossRef]
- Blake, P.; Durao, S.; Naude, C.E.; Bero, L. An analysis of methods used to synthesize evidence and grade recommendations in food-based dietary guidelines. Nutr. Rev. 2018, 76, 290–300. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zeraatkar, D.; Johnston, B.C.; Guyatt, G. Evidence collection and evaluation for the development of dietary guidelines and public policy on nutrition. Annu. Rev. Nutr. 2019, 39, 227–247. [Google Scholar] [CrossRef]
- Tapsell, L.C.; Neale, E.P.; Satija, A.; Hu, F.B. Foods, nutrients, and dietary patterns: Interconnections and implications for dietary guidelines. Adv. Nutr. 2016, 7, 445–454. [Google Scholar] [CrossRef]
- Bero, L.A.; Norris, S.L.; Lawrence, M.A. Making nutrition guidelines fit for purpose. BMJ 2019, 365, 1579. [Google Scholar] [CrossRef]
- Mozaffarian, D.; Forouhi, N.G. Dietary guidelines and health—Is nutrition science up to the task? BMJ 2018, 360, 822. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mozaffarian, D.; Rosenberg, I.; Uauy, R. History of modern nutrition science—Implications for current research, dietary guidelines, and food policy. BMJ 2018, 361, 1–6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dietary Guidelines Advisory Committee. Scientific Report of the 2020 Dietary Guidelines Advisory Committee: Advisory Report to the Secretary of Agriculture and the Secretary of Health and Human Services; United States Department of Agriculture: Washington, DC, USA, 2020. Available online: https://www.dietaryguidelines.gov/2020-advisory-committee-report (accessed on 14 June 2021).
- Kumanyika, S.; Afshin, A.; Arimond, M.; Lawrence, M.; McNaughton, S.A.; Nishida, C. Approaches to Defining Healthy Diets: A Background Paper for the International Expert Consultation on Sustainable Healthy Diets. Food Nutr. Bull. 2020, 41, 7S–30S. [Google Scholar] [CrossRef]
- McNaughton, S.A. Dietary Patterns; International Life Sciences Institute (ILSI): Washington, DC, USA, 2020; Volume 2, pp. 235–248. [Google Scholar]
- Schulze, M.B.; Martínez-González, M.A.; Fung, T.T.; Lichtenstein, A.H.; Forouhi, N.G. Food based dietary patterns and chronic disease prevention. BMJ 2018, 361, 2396. [Google Scholar] [CrossRef] [Green Version]
- WCRF; AICR. Continuous Update Project Expert Report 2018. Judging the Evidence; World Cancer Research Fund and American Institute for Cancer Research: London, UK, 2018; Available online: https://www.wcrf.org/wp-content/uploads/2021/02/judging-the-evidence.pdf (accessed on 14 June 2021).
- Jacobs, D.R.; Tapsell, L.C.; Temple, N.J. Food synergy: The key to balancing the nutrition research effort. Public Health Rev. 2012, 33, 507–529. [Google Scholar] [CrossRef] [Green Version]
- Reedy, J.; Subar, A.F.; George, S.M.; Krebs-Smith, S.M. Extending methods in dietary patterns research. Nutrients 2018, 10, 571. [Google Scholar] [CrossRef] [Green Version]
- Jacobs, D.R.; Tapsell, L.C. Food synergy: The key to a healthy diet. Proc. Nutr. Soc. 2013, 72, 200–206. [Google Scholar] [CrossRef] [Green Version]
- Cespedes, E.M.; Hu, F.B. Dietary patterns: From nutritional epidemiologic analysis to national guidelines. Am. J. Clin. Nutr. 2015, 101, 899–900. [Google Scholar] [CrossRef] [Green Version]
- WHO. Handbook for Guideline Development; World Health Organization: Geneva, Switzerland, 2014; Available online: http://apps.who.int/medicinedocs/documents/s22083en/s22083en.pdf (accessed on 20 August 2021).
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (Updated February 2021); Cochrane: 2021. Available online: www.training.cochrane.org/handbook (accessed on 11 October 2021).
- Tobias, D.K.; Wittenbecher, C.; Hu, F.B. Grading nutrition evidence: Where to go from here? Am. J. Clin. Nutr. 2021. [Google Scholar] [CrossRef] [PubMed]
- Schunemann, H.J.; Cuello, C.; Akl, E.A.; Mustafa, R.A.; Meerpohl, J.J.; Thayer, K.; Morgan, R.L.; Gartlehner, G.; Kunz, R.; Katikireddi, S.V.; et al. GRADE guidelines: 18. How ROBINS-I and other tools to assess risk of bias in nonrandomized studies should be used to rate the certainty of a body of evidence. J. Clin. Epidemiol. 2018. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Katz, D.L.; Karlsen, M.C.; Chung, M.; Shams-White, M.M.; Green, L.W.; Fielding, J.; Saito, A.; Willett, W. Hierarchies of evidence applied to lifestyle Medicine (HEALM): Introduction of a strength-of-evidence approach based on a methodological systematic review. BMC Med. Res. Methodol. 2019, 19, 178. [Google Scholar] [CrossRef]
- Truswell, A.S. Dietary guidelines: Theory and practice. Proc. Nutr. Soc. Aust. 1995, 19, 1–10. [Google Scholar]
- NHMRC. Dietary Guidelines for Australians; National Health and Medical Research Council: Canberra, Australia, 1992.
- NHMRC. Dietary Guidelines for Children and Adolescents; National Health and Medical Research Council: Canberra, Australia, 1995.
- NHMRC. Dietary Guidelines for Older Australians; National Health and Medical Research Council: Canberra, Australia, 1999.
- NHMRC. Dietary Guidelines for Children and Adolescents in Australia; National Health and Medical Research Council: Canberra, Australia, 2003.
- NHMRC. Dietary Guidelines for Australian Adults; National Health and Medical Research Council: Canberra, Australia, 2003.
- NHMRC. Australian Dietary Guidelines; National Health and Medical Research Council: Canberra, Australia, 2013. Available online: https://www.nhmrc.gov.au/guidelines/publications/n55 (accessed on 10 June 2021).
- NHMRC. A Modelling System to Inform the Revision of the Australian Guide to Healthy Eating; Commonwealth of Australia: Canberra, Australia, 2011. Available online: https://www.eatforhealth.gov.au/sites/default/files/files/public_consultation/n55a_dietary_guidelines_food_modelling_111216.pdf (accessed on 10 June 2021).
- Wingrove, K.; Lawrence, M.A.; McNaughton, S.A. Dietary patterns, foods and nutrients: A descriptive analysis of the systematic reviews conducted to inform the Australian Dietary Guidelines. Nutr. Res. Rev. 2020, 1–8. [Google Scholar] [CrossRef]
- NHMRC. Review of the Australian Dietary Guidelines: Living Well for Longer; National Health and Medical Research Council: Canberra, Australia, 2020. Available online: https://www.health.gov.au/ministers/the-hon-greg-hunt-mp/media/review-of-the-australian-dietary-guidelines-living-well-for-longer (accessed on 10 June 2021).
- Mann, J.I. Evidence-based nutrition: Does it differ from evidence-based medicine? Ann. Med. 2010, 42, 475–486. [Google Scholar] [CrossRef] [PubMed]
- Allman-Farinelli, M.; Byron, A.; Collins, C.; Gifford, J.; Williams, P. Challenges and lessons from systematic literature reviews for the Australian dietary guidelines. Aust. J. Prim. Health 2014, 20, 236–240. [Google Scholar] [CrossRef] [Green Version]
- Sandelowski, M. Whatever happened to qualitative description? Res. Nurse Health 2000, 23, 334–340. [Google Scholar] [CrossRef]
- Sandelowski, M. What’s in a name? Qualitative description revisited. Res. Nurs. Health 2010, 33, 77–84. [Google Scholar] [CrossRef]
- Hansen, E.C. Successful Qualitative Health Research: A Practical Introduction; Allen & Unwin: Crows Nest, Australia, 2006. [Google Scholar]
- Swift, J.A.; Tischler, V. Qualitative research in nutrition and dietetics: Getting started. J. Hum. Nutr. Diet. 2010, 23, 559–566. [Google Scholar] [CrossRef]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 16, 349–357. [Google Scholar] [CrossRef] [Green Version]
- Draper, A.; Swift, J.A. Qualitative research in nutrition and dietetics: Data collection issues. J. Hum. Nutr. Diet. 2011, 24, 3–12. [Google Scholar] [CrossRef] [PubMed]
- FAO. Food-based dietary guidelines—Australia. Available online: http://www.fao.org/nutrition/education/food-based-dietary-guidelines/regions/countries/australia/es/ (accessed on 11 October 2021).
- NHMRC. A Review of the Evidence to Address Targeted Questions to Inform the Revision of the Australian Dietary Guidelines; National Health and Medical Research Council: Canberra, Australia, 2011. Available online: https://www.eatforhealth.gov.au/sites/default/files/files/the_guidelines/n55d_dietary_guidelines_evidence_report.pdf (accessed on 20 August 2021).
- Malterud, K.; Siersma, V.D.; Guassora, A.D. Sample size in qualitative interview studies: Guided by information power. Qual. Health Res. 2016, 26, 1753–1760. [Google Scholar] [CrossRef] [PubMed]
- Braun, V.; Clarke, V. To saturate or not to saturate? Questioning data saturation as a useful concept for thematic analysis and sample-size rationales. Qual. Res. Sport Exerc. Health 2019, 1–16. [Google Scholar] [CrossRef]
- Jacob, S.A.; Furgerson, S.P. Writing interview protocols and conducting interviews: Tips for students new to the field of qualitative research. Qual. Rep. 2012, 17, 1–10. [Google Scholar]
- Orb, A.; Eisenhauer, L.; Wynaden, D. Ethics in qualitative research. J. Nurs. Scholarsh. 2001, 33, 93–96. [Google Scholar] [CrossRef]
- Burnard, P.; Gill, P.; Stewart, K.; Treasure, E.; Chadwick, B. Analysing and presenting qualitative data. Br. Dent. J. 2008, 204, 429–432. [Google Scholar] [CrossRef]
- Green, J.; Willis, K.; Hughes, E.; Small, R.; Welch, N.; Gibbs, L.; Daly, J. Generating best evidence from qualitative research: The role of data analysis. Aust, N Z J. Public Health 2007, 31, 545–550. [Google Scholar] [CrossRef]
- QSR International Pty Ltd. NVivo (Version 12 Plus). 2018. Available online: https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home/ (accessed on 10 October 2021).
- Stok, F.M.; Renner, B.; Allan, J.; Boeing, H.; Ensenauer, R.; Issanchou, S.; Kiesswetter, E.; Lien, N.; Mazzocchi, M.; Monsivais, P.; et al. Dietary behavior: An interdisciplinary conceptual analysis and taxonomy. Front. Psychol. 2018, 9, 1689. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- USDA. A Series of Systematic Reviews on the Relationship Between Dietary Patterns and Health Outcomes; United States Department of Agriculture: Washington, DC, USA, 2014. Available online: https://nesr.usda.gov/sites/default/files/2019-06/DietaryPatternsReport-FullFinal2.pdf (accessed on 20 August 2021).
- Louzada, M.L.d.C.; Canella, D.S.; Jaime, P.C.; Monteiro, C.A. Food and Health: The Scientific Evidence Informing the Dietary Guidelines for the Brazilian Population; Faculdade de Saúde Pública and Universidade de São Paulo: Sao Paulo, Brazil, 2019; Available online: http://www.livrosabertos.sibi.usp.br/portaldelivrosUSP/catalog/view/402/355/1436-1 (accessed on 20 August 2021).
- Satija, A.; Yu, E.; Willett, W.C.; Hu, F.B. Understanding nutritional epidemiology and its role in policy. Adv. Nutr. 2015, 6, 5–18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- NHMRC. Guidelines for Guidelines: Assessing Risk of Bias; National Health and Medical Research Council: Canberra, Australia, 2019. Available online: https://www.nhmrc.gov.au/guidelinesforguidelines/develop/assessing-risk-bias (accessed on 1 September 2021).
- Sterne, J.A.C.; Savovic, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [Green Version]
- Sterne, J.A.; Hernan, M.A.; Reeves, B.C.; Savovic, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [Green Version]
- NHMRC. Guidelines for Guidelines: Assessing Certainty of Evidence; National Health and Medical Research Council: Canberra, Australia, 2019. Available online: https://www.nhmrc.gov.au/guidelinesforguidelines/develop/assessing-certainty-evidence (accessed on 1 September 2021).
- Bero, L. Developing reliable dietary guidelines. BMJ 2017, 359, 4845. [Google Scholar] [CrossRef] [PubMed]
- Nestle, M. Perspective: Challenges and controversial issues in the Dietary Guidelines for Americans, 1980–2015. Adv Nutr. 2018, 9, 148–150. [Google Scholar] [CrossRef] [PubMed]
- Alonso-Coello, P.; Schunemann, H.J.; Moberg, J.; Brignardello-Petersen, R.; Akl, E.A.; Davoli, M.; Treweek, S.; Mustafa, R.A.; Rada, G.; Rosenbaum, S.; et al. GRADE Evidence to Decision (EtD) frameworks: A systematic and transparent approach to making well informed healthcare choices. 1: Introduction. BMJ 2016, 353, 2016. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rehfuess, E.A.; Stratil, J.M.; Scheel, I.B.; Portela, A.; Norris, S.L.; Baltussen, R. The WHO-INTEGRATE evidence to decision framework version 1.0: Integrating WHO norms and values and a complexity perspective. BMJ Glob. Health 2019, 4, e000844. [Google Scholar] [CrossRef]

| Categories | Themes |
|---|---|
| Exposures and outcomes of interest |
|
| Practicalities associated with evidence synthesis |
|
| Practicalities associated with evidence translation |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wingrove, K.; Lawrence, M.A.; Russell, C.; McNaughton, S.A. Evidence Use in the Development of the Australian Dietary Guidelines: A Qualitative Study. Nutrients 2021, 13, 3748. https://doi.org/10.3390/nu13113748
Wingrove K, Lawrence MA, Russell C, McNaughton SA. Evidence Use in the Development of the Australian Dietary Guidelines: A Qualitative Study. Nutrients. 2021; 13(11):3748. https://doi.org/10.3390/nu13113748
Chicago/Turabian StyleWingrove, Kate, Mark A. Lawrence, Cherie Russell, and Sarah A. McNaughton. 2021. "Evidence Use in the Development of the Australian Dietary Guidelines: A Qualitative Study" Nutrients 13, no. 11: 3748. https://doi.org/10.3390/nu13113748
APA StyleWingrove, K., Lawrence, M. A., Russell, C., & McNaughton, S. A. (2021). Evidence Use in the Development of the Australian Dietary Guidelines: A Qualitative Study. Nutrients, 13(11), 3748. https://doi.org/10.3390/nu13113748







