Social and Economic Factors and Malnutrition or the Risk of Malnutrition in the Elderly: A Systematic Review and Meta-Analysis of Observational Studies
Abstract
1. Introduction
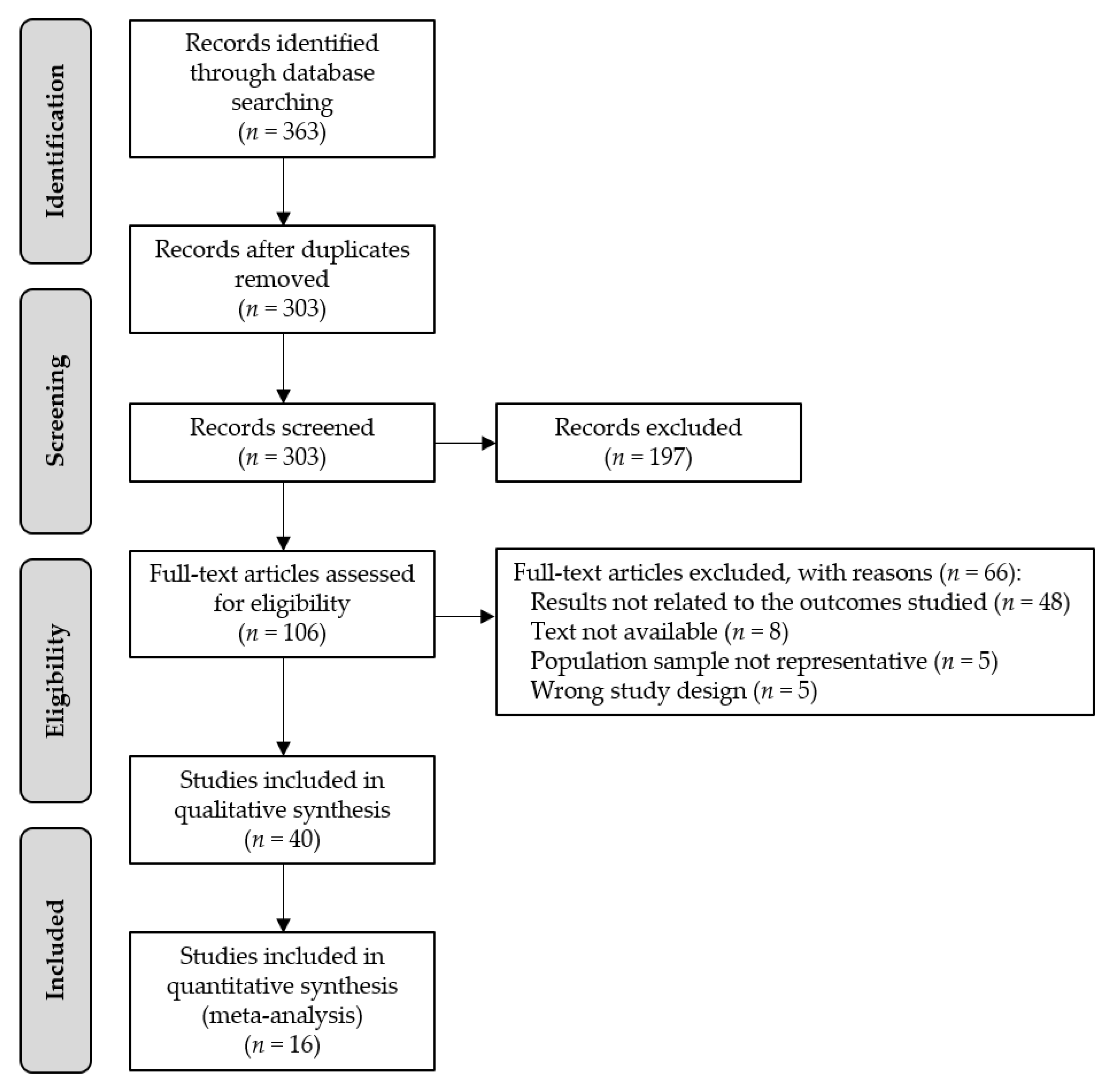
2. Materials and Methods
2.1. Search Strategy
2.2. Study Selection
2.3. Article Review and Data Extraction
2.4. Risk of Bias in Individual Studies
2.5. Statistical Analysis: Meta-Analysis
3. Results
3.1. Characteristics of the Included Studies in the Systematic Review
3.2. Educational Level and Malnutrition/Malnutrition Risk
3.3. Living Alone or Cohabiting and Malnutrition/Malnutrition Risk
3.4. Marital Status and Malnutrition/Malnutrition Risk
3.5. Income Level and Malnutrition/Malnutrition Risk
3.6. Occupational Level and Malnutrition/Malnutrition Risk
3.7. Feeling of Loneliness and Malnutrition/Malnutrition Risk
3.8. Place of Residence and Malnutrition/Malnutrition Risk
3.9. Food Expenditure and Malnutrition/Malnutrition Risk
3.10. Quality of the Articles Included in the Systematic Review
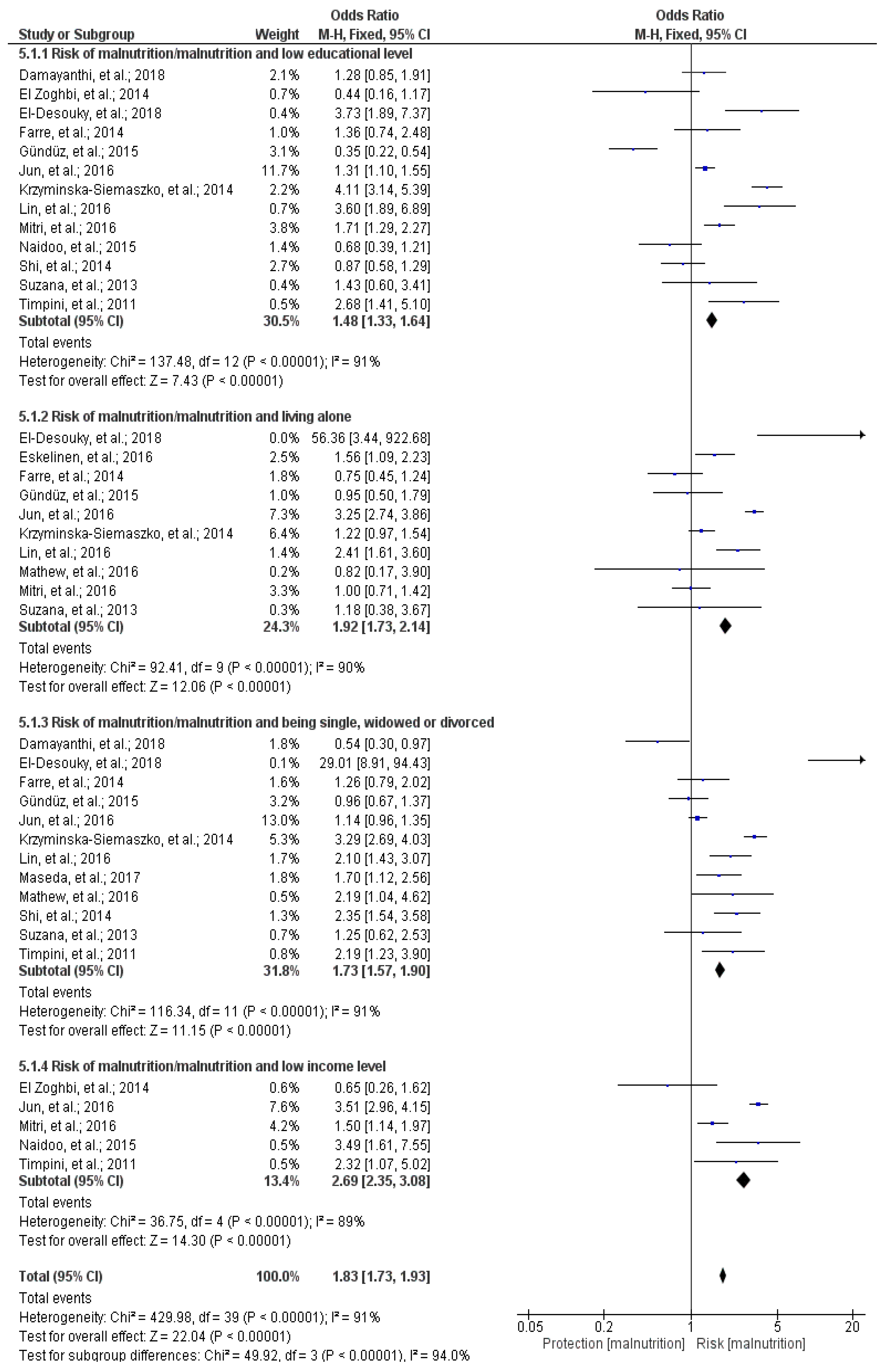
3.11. Meta-Analysis
3.11.1. Educational Level and Malnutrition/Malnutrition Risk
3.11.2. Living Alone or Cohabiting and Malnutrition/Malnutrition Risk
3.11.3. Marital Status and Malnutrition/Malnutrition Risk
3.11.4. Income Level and Malnutrition/Malnutrition Risk
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- European Commission Population Structure and Ageing. Available online: https://ec.europa.eu/eurostat/stati-sticsexplained/index.php/Population_structure_and_ageing#Past_and_future_population_ageing_trends_in_the_EU (accessed on 9 December 2019).
- World Health Organization Ageing and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 8 January 2020).
- Streicher, M.; Zwienen-Pot, J.; Bardon, L.; Nagel, G.; Teh, R.; Meisinger, C.; Colombo, M.; Torbahn, G.; Kiesswetter, E.; Flechtner-Mors, M.; et al. Determinants of incident malnutrition in community-dwelling older adults: A MaNuEL multicohort meta-analysis. J. Am. Geriatr. Soc. 2018, 66, 2335–2343. [Google Scholar] [CrossRef] [PubMed]
- Van der Pols-Vijlbrief, R.; Wijnhoven, H.A.H.; Schaap, L.A.; Terwee, C.B.; Visser, M. Determinants of protein–energy malnutrition in community-dwelling older adults: A systematic review of observational studies. Ageing Res. Rev. 2014, 18, 112–131. [Google Scholar] [CrossRef] [PubMed]
- Hickson, M. Malnutrition and ageing. Postgrad. Med. J. 2006, 82, 2–8. [Google Scholar] [CrossRef] [PubMed]
- Corish, C.A.; Bardon, L.A. Malnutrition in older adults: Screening and determinants. Proc. Nutr. Soc. 2018, 78, 372–379. [Google Scholar] [CrossRef] [PubMed]
- Cederholm, T.; Bosaeus, I.; Barazzoni, R.; Bauer, J.; Van Gossum, A.; Klek, S.; Muscaritoli, M.; Nyulasi, I.; Ockenga, J.; Schneider, S.M.; et al. Diagnostic criteria for malnutrition—An ESPEN Consensus Statement. Clin. Nutr. 2015, 34, 335–340. [Google Scholar] [CrossRef]
- Crichton, M.; Craven, D.; Mackay, H.; Marx, W.; de van der Schueren, M.; Marshall, S. A systematic review, meta-analysis and meta-regression of the prevalence of protein-energy malnutrition: Associations with geographical region and sex. Age Ageing 2018, 48, 38–48. [Google Scholar] [CrossRef]
- Kaiser, M.J.; Bauer, J.M.; Rämsch, C.; Uter, W.; Guigoz, Y.; Cederholm, T.; Thomas, D.R.; Anthony, P.S.; Charlton, K.E.; Maggio, M.; et al. Frequency of malnutrition in older adults: A multinational perspective using the mini nutritional assessment. J. Am. Geriatr. Soc. 2010, 58, 1734–1738. [Google Scholar] [CrossRef]
- Donini, L.M.; Poggiogalle, E.; Molfino, A.; Rosano, A.; Lenzi, A.; Rossi Fanelli, F.; Muscaritoli, M. Mini-nutritional assessment, malnutrition universal screening tool, and nutrition risk screening tool for the nutritional evaluation of older nursing home residents. J. Am. Med. Dir. Assoc. 2016, 17, 959.e11–959.e18. [Google Scholar] [CrossRef]
- Kondrup, J.; Allison, S.P.; Elia, M.; Vellas, B.; Plauth, M. ESPEN guidelines for nutrition screening. Clin. Nutr. 2003, 22, 415–421. [Google Scholar] [CrossRef]
- Correia, M.I.T.D.; Waitzberg, D.L. The impact of malnutrition on morbidity, mortality, length of hospital stay and costs evaluated through a multivariate model analysis. Clin. Nutr. 2003, 22, 235–239. [Google Scholar] [CrossRef]
- Maseda, A.; Diego-Diez, C.; Lorenzo-López, L.; López-López, R.; Regueiro-Folgueira, L.; Millán-Calenti, J.C. Quality of life, functional impairment and social factors as determinants of nutritional status in older adults: The VERISAÚDE study. Clin. Nutr. 2018, 37, 993–999. [Google Scholar] [CrossRef] [PubMed]
- Donini, L.M.; Scardella, P.; Piombo, L.; Neri, B.; Asprino, R.; Proietti, A.R.; Carcaterra, S.; Cava, E.; Cataldi, S.; Cucinotta, D.; et al. Malnutrition in elderly: Social and economic determinants. J. Nutr. Health Aging 2013, 17, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 17 April 2019).
- Chen, C.C.-H.; Bai, Y.-Y.; Huang, G.-H.; Tang, S.T. Revisiting the concept of malnutrition in older people. J. Clin. Nurs. 2007, 16, 2015–2026. [Google Scholar] [CrossRef]
- Boulos, C.; Salameh, P.; Barberger-Gateau, P. Social isolation and risk for malnutrition among older people. Geriatr. Gerontol. Int. 2017, 17, 286–294. [Google Scholar] [CrossRef]
- Cabrera, M.A.S.; Mesas, A.E.; Garcia, A.R.L.; de Andrade, S.M. Malnutrition and depression among community-dwelling elderly people. J. Am. Med. Dir. Assoc. 2007, 8, 582–584. [Google Scholar] [CrossRef]
- Bardon, L.A.; Streicher, M.; Corish, C.A.; Clarke, M.; Power, L.C.; Kenny, R.A.; O’Connor, D.M.; Laird, E.; O’Connor, E.M.; Visser, M.; et al. Predictors of incident malnutrition in older Irish adults from the Irish longitudinal study on ageing cohort—A MaNuEL study. J. Gerontol. Ser. A 2020, 75, 249–256. [Google Scholar] [CrossRef]
- El Zoghbi, M.; Boulos, C.; Awada, S.; Rachidi, S.; Al-Hajje, A.; Bawab, W.; Saleh, N.; Salameh, P. Prevalence of malnutrition and its correlates in older adults living in long stay institutions situated in Beirut, Lebanon. J. Res. Health Sci. 2014, 14, 11–17. [Google Scholar]
- Eskelinen, K.; Hartikainen, S.; Nykänen, I. Is loneliness associated with malnutrition in older people? Int. J. Gerontol. 2016, 10, 43–45. [Google Scholar] [CrossRef]
- Ferra, A.; Del Mar Bibiloni, M.; Zapata, M.E.; Pich, J.; Pons, A.; Tur, J.A. Body mass index, life-style, and healthy status in free living elderly people in menorca island. J. Nutr. Health Aging 2012, 16, 298–305. [Google Scholar] [CrossRef]
- Fjell, A.; Cronfalk, B.S.; Carstens, N.; Rongve, A.; Kvinge, L.M.R.; Seiger, Å.; Skaug, K.; Boström, A.-M. Risk assessment during preventive home visits among older people. J. Multidiscip. Healthc. 2018, 11, 609–620. [Google Scholar] [CrossRef]
- Madeira, T.; Peixoto-Plácido, C.; Sousa-Santos, N.; Santos, O.; Alarcão, V.; Goulão, B.; Mendonça, N.; Nicola, P.J.; Yngve, A.; Bye, A.; et al. Malnutrition among older adults living in Portuguese nursing homes: The PEN-3S study. Public Health Nutr. 2019, 22, 486–497. [Google Scholar] [CrossRef]
- Mitri, R.; Boulos, C.; Adib, S.M. Determinants of the nutritional status of older adults in urban Lebanon. Geriatr. Gerontol. Int. 2017, 17, 424–432. [Google Scholar] [CrossRef] [PubMed]
- Farre, T.B.; Formiga, F.; Ferrer, A.; Plana-Ripoll, O.; Almeda, J.; Pujol, R. Risk of being undernourished in a cohort of community-dwelling 85-year-olds: The Octabaix study. Geriatr. Gerontol. Int. 2014, 14, 702–709. [Google Scholar] [CrossRef] [PubMed]
- Park, M.; Kim, H.; Kim, S.K. Knowledge discovery in a community data set: Malnutrition among the elderly. Healthc. Inform. Res. 2014, 20, 30–38. [Google Scholar] [CrossRef] [PubMed]
- Mokhber, N.; Majdi, M.; Ali-Abadi, M.; Shakeri, M.; Kimiagar, M.; Salek, R.; Moghaddam, P.A.; Sakhdari, A.; Azimi-Nezhad, M.; Ghayour-Mobarhan, M.; et al. Association between malnutrition and depression in elderly people in Razavi Khorasan: A population based-study in Iran. Iran. J. Public Health 2011, 40, 67–74. [Google Scholar] [PubMed]
- Damayanthi, H.D.W.T.; Moy, F.M.; Abdullah, K.L.; Dharmaratne, S.D. Prevalence of malnutrition and associated factors among community-dwelling older persons in Sri Lanka: A cross-sectional study. BMC Geriatr. 2018, 18, 199. [Google Scholar] [CrossRef]
- Shi, R.; Duan, J.; Deng, Y.; Tu, Q.; Cao, Y.; Zhang, M.; Zhu, Q.; Lü, Y. Nutritional status of an elderly population in Southwest China: A cross-sectional study based on comprehensive geriatric assessment. J. Nutr. Health Aging 2015, 19, 26–32. [Google Scholar] [CrossRef]
- Romero-Ortuno, R.; Casey, A.-M.; Cunningham, C.U.; Squires, S.; Prendergast, D.; Kenny, R.A.; Lawlor, B.A. Psychosocial and functional correlates of nutrition among community-dwelling older adults in Ireland. J. Nutr. Health Aging 2011, 15, 527–531. [Google Scholar] [CrossRef]
- Rodríguez-Tadeo, A.; Wall-Medrano, A.; Gaytan-Vidaña, M.E.; Campos, A.; Ornelas-Contreras, M.; Novelo-Huerta, H.I. Malnutrition risk factors among the elderly from the US-Mexico border: The “one thousand” study. J. Nutr. Health Aging 2012, 16, 426–431. [Google Scholar] [CrossRef]
- Schilp, J.; Wijnhoven, H.A.H.; Deeg, D.J.H.; Visser, M. Early determinants for the development of undernutrition in an older general population: Longitudinal aging study Amsterdam. Br. J. Nutr. 2011, 106, 708–717. [Google Scholar] [CrossRef]
- Söderhamn, U.; Dale, B.; Sundsli, K.; Söderhamn, O. Nutritional screening of older home-dwelling Norwegians: A comparison between two instruments. Clin. Interv. Aging 2012, 7, 383–391. [Google Scholar] [CrossRef][Green Version]
- Timpini, A.; Facchi, E.; Cossi, S.; Ghisla, M.K.; Romanelli, G.; Marengoni, A. Self-reported socio-economic status, social, physical and leisure activities and risk for malnutrition in late life: A cross-sectional population-based study. J. Nutr. Health Aging 2011, 15, 233–238. [Google Scholar] [CrossRef]
- Suzana, S.; Boon, P.C.; Chan, P.P.; Normah, C.D. Malnutrition risk and its association with appetite, functional and psychosocial status among elderly Malays in an agricultural settlement. Malays. J. Nutr. 2013, 19, 65–75. [Google Scholar]
- Ji, L.; Meng, H.; Dong, B. Factors associated with poor nutritional status among the oldest-old. Clin. Nutr. 2012, 31, 922–926. [Google Scholar] [CrossRef]
- Westergren, A.; Hagell, P.; Sjödahl Hammarlund, C. Malnutrition and risk of falling among elderly without home-help service-A cross sectional study. J. Nutr. Health Aging 2014, 18, 905–911. [Google Scholar] [CrossRef]
- Krzymińska-Siemaszko, R.; Mossakowska, M.; Skalska, A.; Klich-Rączka, A.; Tobis, S.; Szybalska, A.; Cylkowska-Nowak, M.; Olszanecka-Glinianowicz, M.; Chudek, J.; Wieczorowska-Tobis, K. Social and economic correlates of malnutrition in Polish elderly population: The results of PolSenior study. J. Nutr. Health Aging 2015, 19, 397–402. [Google Scholar] [CrossRef]
- Johansson, L.; Sidenvall, B.; Malmberg, B.; Christensson, L. Who will become malnourished? A prospective study of factors associated with malnutrition in older persons living at home. J. Nutr. Health Aging 2009, 13, 855–861. [Google Scholar] [CrossRef]
- Ferdous, T.; Kabir, Z.N.; Wahlin, Å.; Streatfield, K.; Cederholm, T. The multidimensional background of malnutrition among rural older individuals in Bangladesh—A challenge for the millennium development goal. Public Health Nutr. 2009, 12, 2270–2278. [Google Scholar] [CrossRef]
- Mathew, A.C.; Das, D.; Sampath, S.; Vijayakumar, M.; Ramakrishnan, N.; Ravishankar, S. Prevalence and correlates of malnutrition among elderly in an urban area in Coimbatore. Indian J. Public Health 2016, 60, 112–117. [Google Scholar] [CrossRef]
- Naidoo, I.; Charlton, K.E.; Esterhuizen, T.M.; Cassim, B. High risk of malnutrition associated with depressive symptoms in older South Africans living in KwaZulu-Natal, South Africa: A cross-sectional survey. J. Health. Popul. Nutr. 2015, 33, 19. [Google Scholar] [CrossRef]
- Debnath, S.C. Relationship of socio-economic status with nutritional status among the elderly in a rural community of Bangladesh. Fam. Med. Prim. Care Rev. 2017, 2, 104–109. [Google Scholar] [CrossRef]
- El-Desouky, R.; Abed, H. Screening of malnutrition and its correlates among a sample of rural elderly in Qalyobeya Governorate, Egypt. J. Egypt. Public Health Assoc. 2017, 92, 156–166. [Google Scholar] [CrossRef]
- Jésus, P.; Guerchet, M.; Pilleron, S.; Fayemendy, P.; Maxime Mouanga, A.; Mbelesso, P.; Preux, P.M.; Desport, J.C. Undernutrition and obesity among elderly people living in two cities of developing countries: Prevalence and associated factors in the EDAC study. Clin. Nutr. ESPEN 2017, 21, 40–50. [Google Scholar] [CrossRef] [PubMed]
- Olayiwola, I.O.; Ketiku, A.O. Socio-demographic and nutritional assessment of the elderly Yorubas in Nigeria. Asia Pac. J. Clin. Nutr. 2006, 15, 95–101. [Google Scholar] [PubMed]
- Wham, C.; Maxted, E.; Teh, R.; Kerse, N. Factors associated with nutrition risk in older Māori: A cross sectional study. N. Z. Med. J. 2015, 128, 45–54. [Google Scholar]
- Ramage-Morin, P.L.; Garriguet, D. Nutritional risk among older Canadians. Heal. Rep. 2013, 24, 3–13. [Google Scholar]
- Lengyel, C.O.; Jiang, D.; Tate, R.B. Trajectories of nutritional risk: The Manitoba follow-up study. J. Nutr. Health Aging 2017, 21, 604–609. [Google Scholar] [CrossRef]
- Jun, T.; Yuan, Z. Cross sectional study of nutritional status in older han women. Southeast Asian J. Trop. Med. Public Health 2016, 47, 92–100. [Google Scholar]
- Gündüz, E.; Eskin, F.; Gündüz, M.; Bentli, R.; Zengin, Y.; Dursun, R.; İçer, M.; Durgun, H.M.; Gürbüz, H.; Ekinci, M.; et al. Malnutrition in community-dwelling elderly in Turkey: A multicenter, cross-sectional study. Med. Sci. Monit. 2015, 21, 2750–2756. [Google Scholar] [CrossRef]
- Lin, W.-Q.; Wang, H.H.X.; Yuan, L.-X.; Li, B.; Jing, M.-J.; Luo, J.-L.; Tang, J.; Ye, B.-K.; Wang, P.-X. The unhealthy lifestyle factors associated with an increased risk of poor nutrition among the elderly population in China. J. Nutr. Health Aging 2017, 21, 943–953. [Google Scholar] [CrossRef]
- Programa de las Naciones Unidas para el Desarrollo Índices e Indicadores de Desarrollo Humano. Available online: http://hdr.undp.org/sites/default/files/2018_human_development_statistical_update_es.pdf (accessed on 17 May 2019).
- Damião, R.; Santos, Á.d.S.; Matijasevich, A.; Menezes, P.R. Factors associated with risk of malnutrition in the elderly in south-eastern Brazil. Rev. Bras. Epidemiol. 2017, 20, 598–610. [Google Scholar]
- García-Lorda, P.; Foz, M.; Salas-Salvadó, J. Nutritional status of the elderly population of Catalonia, Spain. Med. Clin. 2002, 118, 707–715. [Google Scholar] [CrossRef]
- De Groot, C.P.; van Staveren, W.A.; de Graaf, C. Determinants of macronutrient intake in elderly people. Eur. J. Clin. Nutr. 2000, 54, S70–S76. [Google Scholar] [CrossRef] [PubMed]
- Sampson, G. Weight loss and malnutrition in the elderly--the shared role of GPs and APDs. Aust. Fam. Physician 2009, 38, 507–510. [Google Scholar]
- McCormack, P. Undernutrition in the elderly population living at home in the community: A review of the literature. J. Adv. Nurs. 1997, 26, 856–863. [Google Scholar] [CrossRef]
- Locher, J.L.; Robinson, C.O.; Roth, D.L.; Ritchie, C.S.; Burgio, K.L. The effect of the presence of others on caloric intake in homebound older adults. J. Gerontol. A Biol. Sci. Med. Sci. 2005, 60, 1475–1478. [Google Scholar] [CrossRef]
- O’Keeffe, M.; Kelly, M.; O’Herlihy, E.; O’Toole, P.W.; Kearney, P.M.; Timmons, S.; O’Shea, E.; Stanton, C.; Hickson, M.; Rolland, Y.; et al. Potentially modifiable determinants of malnutrition in older adults: A systematic review. Clin. Nutr. 2018, 38, 2477–2498. [Google Scholar] [CrossRef]
- Brownie, S. Why are elderly individuals at risk of nutritional deficiency? Int. J. Nurs. Pract. 2006, 12, 110–118. [Google Scholar] [CrossRef]
- Shahar, D.R.; Schultz, R.; Shahar, A.; Wing, R.R. The effect of widowhood on weight change, dietary intake, and eating behavior in the elderly population. J. Aging Health 2001, 13, 186–199. [Google Scholar] [CrossRef]
- Koo, Y.X.; Kang, M.L.; Auyong, A.; Liau, G.Z.; Hoe, J.; Long, M.; Koh, A.; Koh, F.; Liu, R.; Koh, G. Malnutrition in older adults on financial assistance in an urban Asian country: A mixed methods study. Public Health Nutr. 2014, 17, 2834–2843. [Google Scholar] [CrossRef]
- Guyonnet, S.; Rolland, Y. Screening for malnutrition in older people. Clin. Geriatr. Med. 2015, 31, 429–437. [Google Scholar] [CrossRef] [PubMed]
- Payette, H.; Shatenstein, B. Determinants of healthy eating in community-dwelling elderly people. Can. J. Public Health 2005, 96, S27–S31. [Google Scholar] [PubMed]
- Chen, S.-H.; Cheng, H.-Y.; Chuang, Y.-H.; Shao, J.-H. Nutritional status and its health-related factors among older adults in rural and urban areas. J. Adv. Nurs. 2015, 71, 42–53. [Google Scholar] [CrossRef] [PubMed]
- Grammatikopoulou, M.G.; Gkiouras, K.; Theodoridis, X.; Tsisimiri, M.; Markaki, A.G.; Chourdakis, M.; Goulis, D.G. Food insecurity increases the risk of malnutrition among community-dwelling older adults. Maturitas 2019, 119, 8–13. [Google Scholar] [CrossRef] [PubMed]
- Mueller, M.; D’Addario, M.; Egger, M.; Cevallos, M.; Dekkers, O.; Mugglin, C.; Scott, P. Methods to systematically review and meta-analyse observational studies: A systematic scoping review of recommendations. BMC Med. Res. Methodol. 2018, 18, 44. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Antentas, J.M.; Vivas, E. Impacto de la crisis en el derecho a una alimentación sana y saludable. Informe SESPAS 2014. Gac. Sanit. 2014, 28, 58–61. [Google Scholar] [CrossRef]
- Volkert, D.; Beck, A.M.; Cederholm, T.; Cruz-Jentoft, A.; Goisser, S.; Hooper, L.; Kiesswetter, E.; Maggio, M.; Raynaud-Simon, A.; Sieber, C.C.; et al. ESPEN guideline on clinical nutrition and hydration in geriatrics. Clin. Nutr. 2019, 38, 10–47. [Google Scholar] [CrossRef]
| Quality | Socioeconomic Variables Analyzed | |
|---|---|---|
| Bardon et al., 2018 [19] | Medium | Educational level, living alone, marital status |
| Boulos et al., 2016 [17] | High | Feeling of loneliness |
| Cabrera et al., 2007 [18] | Medium | Educational level |
| Chen et al., 2007 [16] | Medium | Educational level, marital status, income level |
| Damayanthi et al., 2018 [29] | High | Educational level, living alone, marital status, income level |
| Debnath et al., 2017 [44] | Medium | Educational level, living alone, marital status, income level, occupational level |
| Donini et al., 2013 [14] | Medium | Educational level, living alone, marital status, income level, occupational level |
| El Zoghbi et al., 2014 [20] | Medium | Educational level, income level |
| El-Desouky et al., 2018 [45] | High | Educational level, living alone, marital status, income level, occupational level |
| Eskelinen et al., 2016 [21] | Medium | Living alone, feeling of loneliness |
| Farre et al., 2014 [26] | High | Educational level, living alone, marital status |
| Ferdous et al., 2009 [41] | High | Educational level, marital status, income level, food expenditure |
| Ferra et al., 2012 [22] | High | Educational level, living alone, income level |
| Fjell et al., 2018 [23] | Medium | Marital status |
| Gündüz et al., 2015 [52] | Medium | Educational level, living alone, marital status |
| Jésus et al., 2017 [46] | High | Educational level, marital status, occupational level |
| Ji et al., 2012 [37] | Medium | Educational level, living alone, income level, occupational level |
| Johansson et al., 2009 [40] | Medium | Living alone |
| Jun et al., 2016 [51] | High | Educational level, living alone, marital status, income level, occupational level, place of residence |
| Krzymińska-Siemaszko et al., 2014 [39] | Medium | Educational level, living alone, marital status, income level, place of residence |
| Lengyel et al., 2017 [50] | Medium | Living alone |
| Lin et al., 2016 [53] | High | Educational level, living alone, marital status, occupational level |
| Madeira et al., 2018 [24] | High | Educational level, marital status, income level |
| Maseda et al., 2017 [13] | Medium | Educational level, living alone, marital status, feeling of loneliness |
| Mathew et al., 2017 [42] | Medium | Educational level, living alone, marital status, income level |
| Mitri et al., 2016 [25] | High | Educational level, living alone, income level |
| Mokhber et al., 2011 [28] | Low | Educational level, living alone, occupational level, place of residence |
| Naidoo et al., 2015 [43] | High | Educational level, living alone, income level |
| Olayiwola et al., 2006 [47] | Medium | Educational level, income level |
| Park et al., 2014 [27] | Medium | Educational level, living alone, marital status, income level |
| Ramage-Morin et al., 2013 [49] | Medium | Educational level, living alone |
| Rodriguez-Tadeo et al., 2011 [32] | Medium | Living alone |
| Romero-Ortuno et al., 2010 [31] | Medium | Living alone |
| Schilp et al., 2011 [33] | High | Educational level, marital status, income level, loneliness feeling |
| Shi et al., 2014 [30] | High | Educational level, marital status, income level, occupational level |
| Söderhamn et al., 2012 [34] | Medium | Marital status, occupational level, feeling of loneliness |
| Suzana et al., 2013 [36] | Medium | Educational level, living alone, marital status, occupational level, feeling of loneliness |
| Timpini et al., 2011 [35] | Medium | Educational level, marital status, income level, occupational level |
| Westergren et al., 2014 [38] | High | Living alone |
| Wham et al., 2015 [48] | High | Educational level, living alone, marital status |
| Socioeconomic Factors | Nutritional Interventions |
|---|---|
| Low educational level | Create promotion and education campaigns for healthy eating [71] |
| Form information meetings on nutrition for patients and their families [72] | |
| Living alone Feeling of loneliness Single, widowed, divorced | Socialize during meals, avoid eating alone; go to the relative’s home [72] |
| Do group activities and share meals [72] | |
| Cook a greater quantity of food and keep it in the fridge for another day of the week | |
| Low income level Low occupational level Low food expenditure | Buy healthy white label products |
| Buy seasonal products | |
| Make a shopping list to avoid buying unnecessary things | |
| Make a weekly menu and adjust the grocery shop to that menu | |
| Buy basic necessities, avoid superfluous products | |
| Resort to social organizations or social programs when it is necessary [71,72] | |
| Rural place of residence | Buy local and proximity products |
| Cook traditional local recipes | |
| Inform the elderly about healthy eating in local shops |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Besora-Moreno, M.; Llauradó, E.; Tarro, L.; Solà, R. Social and Economic Factors and Malnutrition or the Risk of Malnutrition in the Elderly: A Systematic Review and Meta-Analysis of Observational Studies. Nutrients 2020, 12, 737. https://doi.org/10.3390/nu12030737
Besora-Moreno M, Llauradó E, Tarro L, Solà R. Social and Economic Factors and Malnutrition or the Risk of Malnutrition in the Elderly: A Systematic Review and Meta-Analysis of Observational Studies. Nutrients. 2020; 12(3):737. https://doi.org/10.3390/nu12030737
Chicago/Turabian StyleBesora-Moreno, Maria, Elisabet Llauradó, Lucia Tarro, and Rosa Solà. 2020. "Social and Economic Factors and Malnutrition or the Risk of Malnutrition in the Elderly: A Systematic Review and Meta-Analysis of Observational Studies" Nutrients 12, no. 3: 737. https://doi.org/10.3390/nu12030737
APA StyleBesora-Moreno, M., Llauradó, E., Tarro, L., & Solà, R. (2020). Social and Economic Factors and Malnutrition or the Risk of Malnutrition in the Elderly: A Systematic Review and Meta-Analysis of Observational Studies. Nutrients, 12(3), 737. https://doi.org/10.3390/nu12030737





