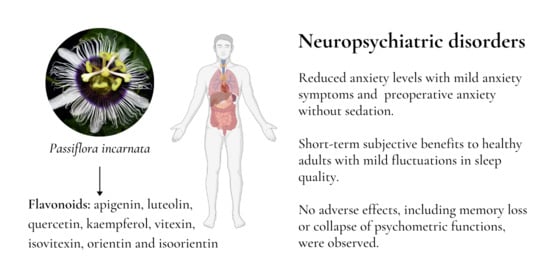
Passiflora incarnata in Neuropsychiatric Disorders—A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy, Inclusion Criteria
2.2. Data Abstraction
2.3. Outcomes
3. Results
3.1. Search Results
3.2. Study Characteristics
3.3. Effect of Passiflora Treatments on Neuropsychiatric Parameters
3.4. Risk of Bias Assessment
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Patel, S. Passiflora Incarnata Linn: A phytopharmacological review. Int. J. Green Pharm. 2009, 3, 277–280. [Google Scholar] [CrossRef]
- Da Fonseca, L.R.; de Rodrigues, R.A.; de Ramos, A.S.; da Cruz, J.D.; Ferreira, J.L.P.; de Silva, J.R.A.; Amaral, A.C.F. Herbal Medicinal Products from Passiflora for Anxiety: An Unexploited Potential. Available online: https://www.hindawi.com/journals/tswj/2020/6598434/ (accessed on 17 November 2020).
- Dhawan, K.; Dhawan, S.; Sharma, A. Passiflora: A review update. J. Ethnopharmacol. 2004, 94, 1–23. [Google Scholar] [CrossRef] [PubMed]
- European Medicines Agency. Assessment Report on Passiflora Incarnata L. herba; European Medicines Agency: Amsterdam, The Netherlands, 2014; Volume 22. [Google Scholar]
- Miyasaka, L.S.; Atallah, A.N.; Soares, B.G.O. Passiflora for anxiety disorder. Cochrane Database Syst. Rev. 2007, CD004518. [Google Scholar] [CrossRef] [PubMed]
- Movafegh, A.; Alizadeh, R.; Hajimohamadi, F.; Esfehani, F.; Nejatfar, M. Preoperative oral Passiflora Incarnata reduces anxiety in ambulatory surgery patients: A double-blind, placebo-controlled study. Anesth. Analg. 2008, 106, 1728–1732. [Google Scholar] [CrossRef]
- Lupien, S.J.; McEwen, B.S.; Gunnar, M.R.; Heim, C. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat. Rev. Neurosci. 2009, 10, 434–445. [Google Scholar] [CrossRef] [PubMed]
- Jawna-Zboińska, K.; Blecharz-Klin, K.; Joniec-Maciejak, I.; Wawer, A.; Pyrzanowska, J.; Piechal, A.; Mirowska-Guzel, D.; Widy-Tyszkiewicz, E. Passiflora Incarnata L. Improves Spatial Memory, Reduces Stress, and Affects Neurotransmission in Rats. Phytother. Res. 2016, 30, 781–789. [Google Scholar] [CrossRef]
- Kim, G.-H.; Lim, K.; Yang, H.S.; Lee, J.-K.; Kim, Y.; Park, S.-K.; Kim, S.-H.; Park, S.; Kim, T.-H.; Moon, J.-S.; et al. Improvement in neurogenesis and memory function by administration of Passiflora Incarnata L. extract applied to sleep disorder in rodent models. J. Chem. Neuroanat. 2019, 98, 27–40. [Google Scholar] [CrossRef]
- Miroddi, M.; Calapai, G.; Navarra, M.; Minciullo, P.L.; Gangemi, S. Passiflora Incarnata L.: Ethnopharmacology, clinical application, safety and evaluation of clinical trials. J. Ethnopharmacol. 2013, 150, 791–804. [Google Scholar] [CrossRef]
- Kim, M.; Lim, H.-S.; Lee, H.-H.; Kim, T.-H. Role Identification of Passiflora Incarnata Linnaeus: A Mini Review. J. Menopausal. Med. 2017, 23, 156–159. [Google Scholar] [CrossRef] [Green Version]
- Makara-Studzińska, M.; Pyłypczuk, A.; Madej, A. Nasilenie objawów depresji i lęku wśród osób uzależnionych od alkoholu i hazardu. EJMT 2015, 2, 7. [Google Scholar]
- Sohn, H.-M.; Ryu, J.-H. Monitored anesthesia care in and outside the operating room. Korean J. Anesthesiol. 2016, 69, 319–326. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Freeman, R.; Clarke, H.M.M.; Humphris, G.M. Conversion tables for the Corah and Modified Dental Anxiety Scales. Community Dent. Health 2007, 24, 49–54. [Google Scholar] [PubMed]
- Corah, N.L.; Gale, E.N.; Illig, S.J. Assessment of a dental anxiety scale. J. Am. Dent. Assoc. 1978, 97, 816–819. [Google Scholar] [CrossRef]
- Murray, P.; Liddell, A.; Donohue, J. A longitudinal study of the contribution of dental experience to dental anxiety in children between 9 and 12 years of age. J. Behav. Med. 1989, 12, 309–320. [Google Scholar] [CrossRef]
- Cravero, J.P.; Kaplan, R.F.; Landrigan-Ossar, M.; Coté, C.J. 48—Sedation for Diagnostic and Therapeutic Procedures outside the Operating Room. In A Practice of Anesthesia for Infants and Children, 6th ed.; Coté, C.J., Lerman, J., Anderson, B.J., Eds.; Elsevier: Philadelphia, PA, USA, 2019; pp. 1109–1128.e7. ISBN 978-0-323-42974-0. [Google Scholar]
- Jaeger, J. Digit Symbol Substitution Test: The Case for Sensitivity over Specificity in Neuropsychological Testing. J. Clin. Psychopharmacol. 2018, 38, 513–519. [Google Scholar] [CrossRef] [PubMed]
- Bates, M.E.; Lemay, E.P. The d2 Test of attention: Construct validity and extensions in scoring techniques. J. Int. Neuropsychol. Soc. 2004, 10, 392–400. [Google Scholar] [CrossRef]
- Gualtieri, C.T.; Johnson, L.G. ADHD: Is Objective Diagnosis Possible? Psychiatry (Edgmont) 2005, 2, 44–53. [Google Scholar]
- Rodríguez, C.; Areces, D.; García, T.; Cueli, M.; González-Castro, P. Comparison between two continuous performance tests for identifying ADHD: Traditional vs. virtual reality. Int. J. Clin. Health Psychol. 2018, 18, 254–263. [Google Scholar] [CrossRef]
- Tsai, S.K.; Lee, C.; Kwan, W.F.; Chen, B.J. Recovery of cognitive functions after anaesthesia with desflurane or isoflurane and nitrous oxide. Br. J. Anaesth. 1992, 69, 255–258. [Google Scholar] [CrossRef]
- Gupta, A.; Lind, S.; Eklund, A.; Lennmarken, C. The effects of midazolam and flumazenil on psychomotor function. J. Clin. Anesth. 1997, 9, 21–25. [Google Scholar] [CrossRef]
- Hentzen, S.; Haret, D.; Ward, C.; Peterson, A.R. King Devick Test as a Monitor of Anesthetic Recovery. A validation study. Pediatr. Anesth. Crit. Care J. PACCJ 2019, 31–36. [Google Scholar] [CrossRef]
- Axelrod, B.N.; Meyers, J.E.; Davis, J.J. Finger Tapping Test performance as a measure of performance validity. Clin. Neuropsychol. 2014, 28, 876–888. [Google Scholar] [CrossRef] [PubMed]
- Dantas, L.-P.; de Oliveira-Ribeiro, A.; de Almeida-Souza, L.-M.; Groppo, F.-C. Effects of Passiflora Incarnata and midazolam for control of anxiety in patients undergoing dental extraction. Med. Oral Patol. Oral Cir. Bucal 2017, 22, e95–e101. [Google Scholar] [CrossRef] [Green Version]
- Aslanargun, P.; Cuvas, O.; Dikmen, B.; Aslan, E.; Yuksel, M.U. Passiflora Incarnata Linneaus as an anxiolytic before spinal anesthesia. J. Anesth. 2012, 26, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Dimpfel, W.; Koch, K.; Weiss, G. Early effect of NEURAPAS®balance on current source density (CSD) of human EEG. BMC Psychiatry 2011, 11, 123. [Google Scholar] [CrossRef] [Green Version]
- Kaviani, N.; Tavakoli, M.; Tabanmehr, M.; Havaei, R. The efficacy of Passiflora Incarnata linnaeus in reducing dental anxiety in patients undergoing periodontal treatment. J. Dent. (Shiraz) 2013, 14, 68–72. [Google Scholar]
- Akhondzadeh, S.; Naghavi, H.R.; Vazirian, M.; Shayeganpour, A.; Rashidi, H.; Khani, M. Passionflower in the treatment of generalized anxiety: A pilot double-blind randomized controlled trial with oxazepam. J. Clin. Pharm. Ther. 2001, 26, 363–367. [Google Scholar] [CrossRef]
- Azimaraghi, O.; Yousefshahi, F.; Khatavi, F.; Zamani, M.M.; Movafegh, A. Both Oral Passiflora Incarnata and Oxazepam Can Reduce Pre-Operative Anxiety in Ambulatory Surgery Patients: A Double-Blind, Placebo-Controlled Study. Asian J. Pharm. Clin. Res. 2017, 10, 331–334. [Google Scholar] [CrossRef] [Green Version]
- Ngan, A.; Conduit, R. A double-blind, placebo-controlled investigation of the effects of Passiflora Incarnata (passionflower) herbal tea on subjective sleep quality. Phytother. Res. 2011, 25, 1153–1159. [Google Scholar] [CrossRef]
- Rokhtabnak, F.; Ghodraty, M.R.; Kholdebarin, A.; Khatibi, A.; Seyed Alizadeh, S.S.; Koleini, Z.S.; Zamani, M.M.; Pournajafian, A. Comparing the Effect of Preoperative Administration of Melatonin and Passiflora Incarnata on Postoperative Cognitive Disorders in Adult Patients Undergoing Elective Surgery. Anesth. Pain Med. 2017, 7, e41238. [Google Scholar] [CrossRef] [Green Version]
- WHO. Depression and other Common Mental Disorders. Available online: http://www.who.int/mental_health/management/depression/prevalence_global_health_estimates/en/ (accessed on 17 November 2020).
- Cuijpers, P.; Stringaris, A.; Wolpert, M. Treatment outcomes for depression: Challenges and opportunities. Lancet Psychiatry 2020, 7, 925–927. [Google Scholar] [CrossRef] [Green Version]
- Rogers, J.P.; Chesney, E.; Oliver, D.; Pollak, T.A.; McGuire, P.; Fusar-Poli, P.; Zandi, M.S.; Lewis, G.; David, A.S. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: A systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry 2020, 7, 611–627. [Google Scholar] [CrossRef]
- Vasileva, L.V.; Ivanovska, M.V.; Murdjeva, M.A.; Saracheva, K.E.; Georgiev, M.I. Immunoregulatory natural compounds in stress-induced depression: An alternative or an adjunct to conventional antidepressant therapy? Food Chem. Toxicol. 2019, 127, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Liu, C.; Wang, Y.; Wang, P.; Li, Y.; Li, B. Herbal Medicine for Anxiety, Depression and Insomnia. Curr. Neuropharmacol. 2015, 13. [Google Scholar] [CrossRef] [Green Version]
- Al-kuraishy, H.; Alwindy, S.; Al-Gareeb, A. Beneficial Neuro-Pharmacological Effect of Passionflower (Passiflora Incarnate L). Online J. Neurol. Brain Disord. 2020, 3, 285–289. [Google Scholar] [CrossRef]
- Appel, K.; Rose, T.; Fiebich, B.; Kammler, T.; Hoffmann, C.; Weiss, G. Modulation of the γ-aminobutric acid (GABA) system by Passiflora Incarnata L. Phytother. Res. PTR 2011, 25, 838–843. [Google Scholar] [CrossRef]
- Aman, U.; Subhan, F.; Shahid, M.; Akbar, S.; Ahmad, N.; Ali, G.; Fawad, K.; Sewell, R.D.E. Passiflora Incarnata attenuation of neuropathic allodynia and vulvodynia apropos GABA-ergic and opioidergic antinociceptive and behavioural mechanisms. BMC Complement. Altern. Med. 2016, 16, 77. [Google Scholar] [CrossRef] [Green Version]
- Grundmann, O.; Wang, J.; McGregor, G.P.; Butterweck, V. Anxiolytic activity of a phytochemically characterized Passiflora Incarnata extract is mediated via the GABAergic system. Planta Med. 2008, 74, 1769–1773. [Google Scholar] [CrossRef]
- Nassiri-Asl, M.; Zamansoltani, F.; Shariatirad, S. Possible role of GABAA—Benzodiazepine receptor in anticonvulsant effects of Pasipay in rats. J. Chin. Integr. Med. 2008, 6, 1170–1173. [Google Scholar] [CrossRef]
- Elsas, S.-M.; Rossi, D.J.; Raber, J.; White, G.; Seeley, C.-A.; Gregory, W.L.; Mohr, C.; Pfankuch, T.; Soumyanath, A. Passiflora incarnata L. (Passionflower) extracts elicit GABA currents in hippocampal neurons in vitro, and show anxiogenic and anticonvulsant effects in vivo, varying with extraction method. Phytomedicine 2010, 17, 940–949. [Google Scholar] [CrossRef] [Green Version]

| Reference/Year/Country | Description of Treatment | Characteristics of The Intervention and of the Study Group | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Study Objective | Blinding | Duration of Administration (Days) | ROB * | Commercial Name of Product Containing P. Incarnata | Passiflora Dose | Comparator | n Total Randomized/Analyzed | Age Years (Mean) | Males (%) | |
| Akhondzadeh et al., 2001 (Iran) [12] | Comparative efficacy of Passiflora incarnata extract with oxazepam in the treatment of systemic anxiety disorder | DB | 28 | 5 | Passipay (Iran, Darouk) | 45 drops/day | Placebo + oxazepam (30 mg/day) | 36/32 | 19–47 # | 44.4 |
| Aslanargun et al., 2012 (Turkey) [13] | Effects of preoperative oral administration of Passiflora incarnata on anxiety, psychomotor functions, sedation and hemodynamics in patients undergoing spinal anesthesia | DB | 1 | 4 | Passiflora Syrup (Sandoz, Kocaeli, Turkey) | 700 mg/5 mL | Placebo | 60/60 | 25–55 # | 86.6 |
| Azimaraghi et al., 2017 (Iran) [14] | The efficacy of Passiflora incarnata to reduce preoperative anxiety in comparison to oxazepam | DB | NA | 7 | Passipy™ (Iran Darouk) | 500 mg | Oxazepam (10 mg) | 128/128 | 36.77 | 57.8 |
| Dantas et al., 2017 (Brazil) [15] | The influence of Passiflora incarnata and midazolam on the control of anxiety in patients exposed to the extraction of the third mandibular molar tooth | DB, CO | 15-30 | 7 | Passiflora incarnata | 260 mg | Midazolam (15 mg) | 40/40 | 23.94 | 32.5 |
| Dimpfel et al., 2011 (Germany) [16] | Explanation of the effectiveness of the preparation by analysis of current density (CFD) of brain activity in the presence of various mental challenges | SB, CO | 1 | 4 | NEURAPAS® | 192 mg of P. incarnata extract | Placebo | 16/16 | 47.85 | 50 |
| Kaviani et al., 2013 (Iran) [17] | Determining the effectiveness of passion flower application in reducing anxiety during dental procedures | SB | 2 | 4 | Passipay (Iran, Darouk) | 40 drops/day | Placebo | 63/63 | 34.07 | 38.1 |
| Kaviani et al., 2013 (Iran) [17] | Determining the effectiveness of passion flower application in reducing anxiety during dental procedures | SB | 2 | 4 | Passipay (Iran, Darouk) | 40 drops/day | Negative group | 63/63 | 34.07 | 38.1 |
| Movafegh et al., 2008 (Iran) [6] | Effectiveness of Passiflora in reducing preoperative anxiety | DB | 1 | 7 | Passipy™ (Iran Darouk) | 500 mg | Placebo | 60/60 | 31.85 | 50 |
| Ngan and Conduit, 2011 (Australia) [18] | To test the effectiveness of the Passiflora infusion on human sleep, measured by means of sleep logs approved by polysomnography | DB | 22 | 6 | Tea bags (Hilde Hemmes’ HerbalSupplies Pty Ltd.; SA, Australia) | infusion (2 g in 250 mL water; concentration 0.8%) | Placebo | 41/41 | 22.73 | 34.1 |
| Rokhtabnak et al., 2017 (Iran) [19] | Effects of Passiflora incarnata and melatonin on cognitive functions and sedative effect without causing cognitive disturbance | DB | 1 | 7 | Passiflora incarnata | 1000 mg (prepared and packed by Department of Pharmacy, Shahid Beheshti University of Medical Sciences, Iran) | Melatonin (6 mg) | 64/52 | 20–60 # | 44.2 |
| Reference/Year/Country | Comparator | Control Group | Tested Group | Conclusions | ||
|---|---|---|---|---|---|---|
| Baseline Data | Endpoint Data | Baseline Data | Endpoint Data | |||
| Akhondzadeh et al., 2001 (Iran) [12] | Placebo + oxazepam (30 mg/day) | Hamilton scale: 19.74 ± 0.83 | Hamilton scale: 5.1 ± 1.28 | Hamilton scale: 19.74 ± 0.83 | Hamilton scale: 5.5 ± 0.75 | Passiflora extract is effective in the treatment of systemic anxiety; additionally, there is a low incidence of impairment of work efficiency with Passiflora extract, as compared to oxazepam. There is a need for further research on the use of Passiflora in the treatment of systemic anxiety. |
| Aslanargun et al., 2012 (Turkey) [13] | Placebo | STAI-S: 34.8 ± 8.4; STAI-T: 35.3 ± 8.3; PAT: 95.2 ± 16.4; FTT: 72.3 ± 14.1; OAA/S: 5 ± 0; NRS: 6.6 ± 1; TDTmm: 0.8 ± 0.2; TDTnr: 0.9 ± 0.7; DSST: 30.8 ± 5; | STAI-S: 36.6 ± 7.6; STAI-T: 38.1 ± 9.2; PAT: 99.1 ± 1.4; FTT: 72.3 ± 13.1; OAA/S: 5 ± 0.15; NRS: 6.1 ± 1.3; TDTmm:1.1 ± 0.3; TDTnr: 1.2 ± 1; DSST: 29.1± 4.8; | STAI-S: 36.4 ± 10.9; STAI-T: 32.5 ± 9.5; PAT: 98.0 ± 2.6; FTT:67.4 ± 18.9; OAA/S: 5 ± 0; NRS:7.6 ± 0.9; TDTmm: 0.9 ± 0.2; TDTnr: 0.8 ± 0.8; DSST: 31.1 ± 5.1; | STAI-S: 35.7 ± 10.8; STAI-T: 33.4 ± 8.7; PAT: 99.1 ± 1.7; FTT: 67.6 ± 19.8; OAA/S: 5 ± 0.15; NRS: 4.4 ± 1.2; TDTmm: 1.2 ± 0.4; TDTnr: 1 ± 0.9; DSST: 28.6 ± 5; | Preoperative oral administration of 700 mg/5 mL of Passiflora water extract reduces the level of anxiety in patients before spinal anesthesia without changing their sedation level, psychomotor function test results, or hemodynamics. |
| Azimaraghi et al., 2017 (Iran) [14] | Oxazepam (10 mg) | NRS: 6.6 ± 1; TDTmm: 0.8 ± 0.2; TDTnr: 0.9 ± 0.7; DSST: 30.8 ± 5; | NRS: 6.1 ± 1.3; TDTmm: 1.1 ± 0.3; TDTnr: 1.2 ± 1; DSST: 29.1 ± 4.8; | NRS: 7.6 ± 0.9; TDTmm: 0.9 ± 0.2; TDTnr: 0.8 ± 0.8; DSST: 31.1 ± 5.1; | NRS: 4.4 ± 1.2; TDTmm: 1.2 ± 0.4; TDTnr: 1 ± 0.9; DSST: 28.6 ± 5; | In outpatient surgery, oral administration of Passiflora as a premedication reduces preoperative anxiety with comparable dysfunction of psychomotor functions, as compared to preoperative oral intake of oxazepam. |
| Dimpfel et al., 2011 (Germany) [16] | Midazolam (15 mg) | d2 test: 12.32 ± 4.02; memory test: 10.77 ± 3.98; ccCPT: 6.57 ± 6.17; | d2 test: 13.59 ± 3.77; memory test: 11.51 ± 3.74; CPT: 6.87 ± 7.3; | d2 test: 12.14 ± 3.06; memory test: 11.37 ± 3.64; CPT: 5.59 ± 5.85; | d2 test: 13.53 ± 3.13; memory test: 11.95 ± 3.65; CPT: 7.86 ± 5.76; | Analysis of neurophysiological changes after NEURAPAS® intake showed similarity of changes compared to sedatives and antidepressants, in EEG, without cognitive function impairment. |
| Kaviani et al., 2013 (Iran) [17] | Placebo | Corah DAS-R: 12 ± 2.66; | Corah DAS-R: 10.52 ± 2.11; | Corah DAS-R: 13.09 ± 2.42; | Corah DAS-R: 8.47 ± 2.08; | The serving of the passion flower as a premeditation is effective in reducing anxiety. Further trials with more people are needed to confirm the results. |
| Placebo | Corah DAS-R: 11.66 ± 2.39 | Corah DAS-R: 11.23 ± 2.34 | Corah DAS-R: 13.09 ± 2.42; | Corah DAS-R: 8.47 ± 2.08; | ||
| Movafegh et al., 2008 (Iran) [6] | Negative group | NRS: 5.1 ± 2; TDTmm: 0.6 ± 1; TDTnr: 0.8 ± 0.9; DSST: 24.3 ± 6.2; | NRS: 3.88 ± 0.81; TDTmm: 0.6 ± 0.3; TDTnr: 0.9 ± 0.8; DSST: 21.5 ± 7.1; | NRS: 4.6 ± 1.7; TDTmm: 0.7 ± 1.1; TDTnr: 0.7 ± 0.62; DSST: 23.6 ± 7.2; | NRS: 0.97 ± 0.72; TDTmm: 0.7 ± 0.2; TDTnr: 8 ± 0.5; DSST: 22.4 ± 6.5; | In outpatient surgery, oral administration of Passiflora as premeditation reduces anxiety without sedation. |
| Ngan and Conduit, 2011 (Australia) [18] | Placebo | NA | NA | NA | NA | Consumption of a small dose of Passiflora infusion brings short-term subjective benefits to healthy adults with mild fluctuations in sleep quality. |
| Rokhtabnak et al., 2017 (Iran) [19] | Placebo | DSST: 30.67 ± nd; Ramsy scale: 1.81 ± nd; VAS: 26.5 ± nd; | DSST: 27.5 ± nd; Ramsey scale: 1.95 ± nd; VAS: 26.5 ± nd; | DSST: 22.33 ± nd; Ramsey scale: 1.85 ± nd; VAS: 26.5 ± nd; | DSST: 25.5 ± nd; Ramsey scale: 1.95 ± nd; VAS: 26.5 ± nd; | Passiflora premedication reduces anxiety, as does melatonin, but melatonin causes less cognitive disorders compared to Passiflora. |
| What Did You Feel during the Surgery? | Protocol 1 (Midazolam) | Protocol 2 (Passiflora) | Results | ||
| Midazolam (1) | Passiflora (2) | Passiflora (2) | Midazolam (1) | Passiflora showed an anti-anxiety effect similar to midazolam; it was safe and effective in the case of conscious sedation in adult patients having their third mandibular molar tooth extracted | |
| Calm | 5 (33.3%) | 17 (68%) | 13 (52%) | 3 (20%) | |
| Slight anxiety | 6 (40%) | 7 (28%) | 10 (40%) | 8 (55.3%) | |
| Serious anxiety or fear | 3 (20%) | 1 (4%) | 2 (8%) | 3 (20%) | |
| Bad feeling caused by anxiety | 1 (6.7%) | 0 | 0 | 1 (6.7%) | |
| Total | 15 | 25 | 25 | 15 | |
| Reference/Country | Publication Year | Random Generation of The Error Sequence (Selection Error) | Hiding the Allocation (Selection Variation) | Blinding of Participants and Staff (Biased Evaluation) | Performance Evaluation Blindness (Detection Error) | Incomplete Result Data | Selective Reporting (Reporting Error) | Other Biases | Number of Indications with Low Risk of Bias |
|---|---|---|---|---|---|---|---|---|---|
| Akhondzadeh et al. (Iran) [12] | 2001 | L | ? | L | ? | L | L | L | 5 |
| Aslanargun et al. (Turkey) [13] | 2012 | ? | ? | L | ? | L | L | L | 4 |
| Azimaraghi et al. (Iran) [14] | 2017 | L | L | L | L | L | L | L | 7 |
| Dantas et al. (Brazil) [15] | 2017 | L | L | L | L | L | L | L | 7 |
| Dimpfel et al. (Germany) [16] | 2011 | L | ? | ? | ? | L | L | L | 4 |
| Kaviani et al. (Iran) [17] | 2013 | L | ? | H | ? | L | L | L | 4 |
| Movafegh et al. (Iran) [6] | 2008 | L | L | L | L | L | L | L | 7 |
| Ngan and Conduit (Australia) [18] | 2011 | ? | L | L | L | L | L | L | 6 |
| Rokhtabnaket al. (Iran) [19] | 2017 | L | L | L | L | L | L | L | 7 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Janda, K.; Wojtkowska, K.; Jakubczyk, K.; Antoniewicz, J.; Skonieczna-Żydecka, K. Passiflora incarnata in Neuropsychiatric Disorders—A Systematic Review. Nutrients 2020, 12, 3894. https://doi.org/10.3390/nu12123894
Janda K, Wojtkowska K, Jakubczyk K, Antoniewicz J, Skonieczna-Żydecka K. Passiflora incarnata in Neuropsychiatric Disorders—A Systematic Review. Nutrients. 2020; 12(12):3894. https://doi.org/10.3390/nu12123894
Chicago/Turabian StyleJanda, Katarzyna, Karolina Wojtkowska, Karolina Jakubczyk, Justyna Antoniewicz, and Karolina Skonieczna-Żydecka. 2020. "Passiflora incarnata in Neuropsychiatric Disorders—A Systematic Review" Nutrients 12, no. 12: 3894. https://doi.org/10.3390/nu12123894
APA StyleJanda, K., Wojtkowska, K., Jakubczyk, K., Antoniewicz, J., & Skonieczna-Żydecka, K. (2020). Passiflora incarnata in Neuropsychiatric Disorders—A Systematic Review. Nutrients, 12(12), 3894. https://doi.org/10.3390/nu12123894