Iron Therapy in Inflammatory Bowel Disease
Abstract
1. Introduction
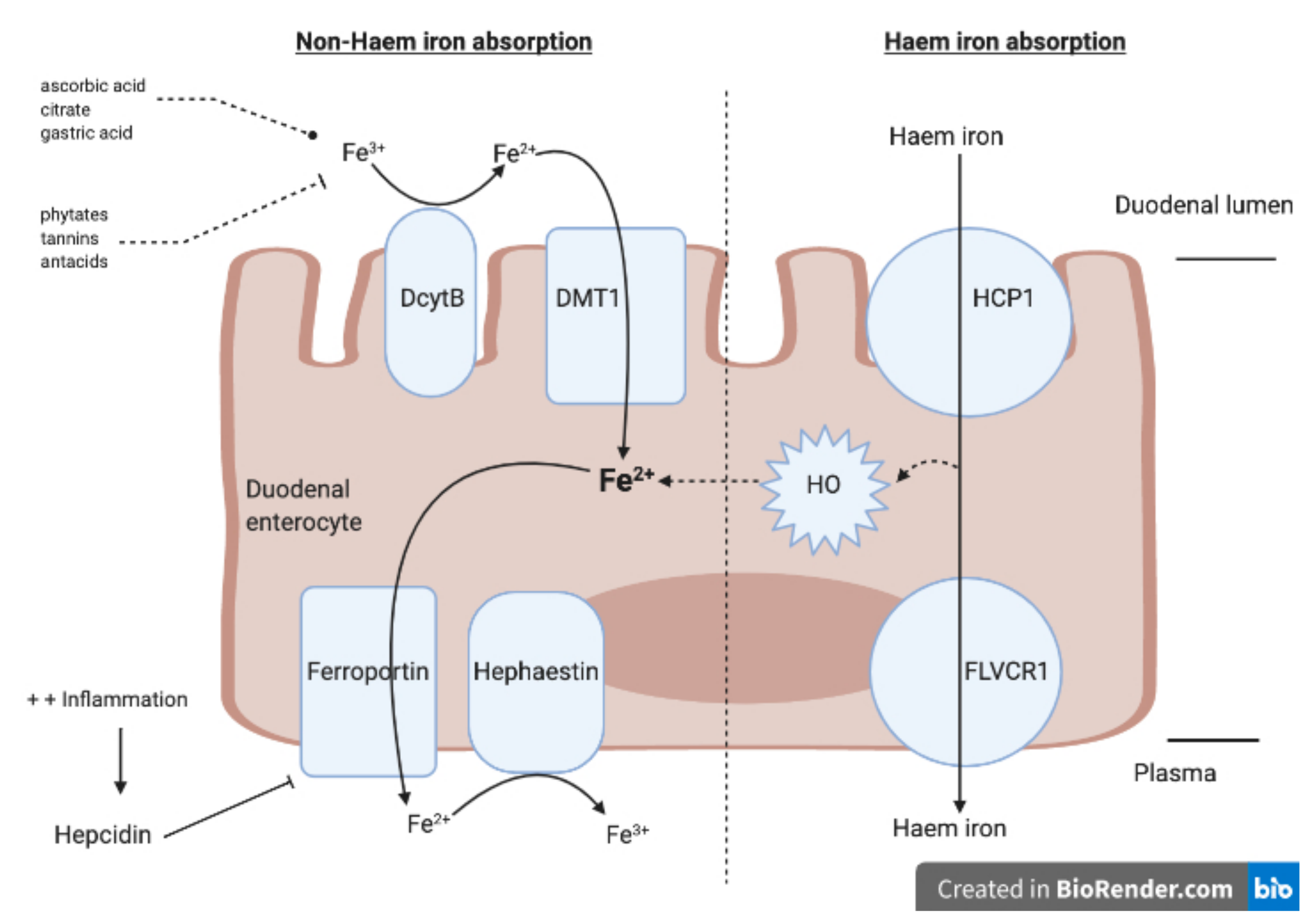
1.1. Iron Absorption, Iron Deficiency and Iron Deficiency Anaemia
1.2. Clinical Manifestations of IDA and Its Effect on Quality of Life
2. Management
2.1. Oral Iron
Types of Preparations
2.2. Ferric Maltol (Ferracru)
2.3. Sucrosomial Iron
2.4. Advantages and Disadvantages of Oral Iron
3. IV Iron
3.1. Parenteral Iron Preparations
3.2. Dextran
3.3. Sucrose (Venofer, Vifor)
3.4. Ferric Carboxymaltose (Ferrinject)
3.5. Ferric Gluconate (Ferrlecit, Sanofi)
3.6. Ferumoxytol
3.7. Ferric Isomaltoside (Monofer)
3.8. Advantages versus Disadvantages of IV Iron
3.9. When to Use IV versus Oral
4. Blood Transfusions
5. Erythropoietin-Stimulating Agents
6. Follow Up and Maintenance
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Jimenez, K.M.; Gasche, C. Management of Iron Deficiency Anaemia in Inflammatory Bowel Disease. Acta Haematol. 2019, 142, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Ng, S.C.; Shi, H.Y.; Hamidi, N.; Underwood, F.E.; Tang, W.; Benchimol, E.I.; Sung, J.J. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: A systematic review of population-based studies. Lancet 2018, 390, 2769–2778. [Google Scholar] [CrossRef]
- D’Amico, F.; Peyrin-Biroulet, L.; Danese, S. Oral Iron for IBD Patients: Lessons Learned at Time of COVID-19 Pandemic. J. Clin. Med. 2020, 9, 1536. [Google Scholar] [CrossRef] [PubMed]
- De Silva, A.D.; Mylonaki, M.; Rampton, D.S. Oral iron therapy in inflammatory bowel disease: Usage, tolerance, and efficacy. Inflamm. Bowel Dis. 2003, 9, 316–320. [Google Scholar] [CrossRef]
- Filmann, N.; Rey, J.; Schneeweiss, S.; Ardizzone, S.; Bager, P.; Bergamaschi, G.; Vavricka, S.R. Prevalence in anemia in inflammatory bowel diseases in European countries: A systematic review and individual patient data meta-analysis. Inflamm. Bowel Dis. 2014, 20, 936–945. [Google Scholar] [CrossRef]
- Høivik, M.L.; Reinisch, W.; Cvancarova, M.; Moum, B.; The IBSEN Study Group. Anaemia in inflammatory bowel disease: A population-based 10-year follow-up. Aliment. Pharmacol. Ther. 2013, 39, 69–76. [Google Scholar] [CrossRef]
- Vegh, Z.; Kürti, Z.; Gonczi, L.; Golovics, P.A.; Lovasz, B.D.; Szita, I.; Balogh, M.; Pandur, T.; Vavricka, S.R.; Rogler, G.; et al. Association of extraintestinal manifestations and anaemia with disease outcomes in patients with inflammatory bowel disease. Scand. J. Gastroenterol. 2016, 51, 848–854. [Google Scholar] [CrossRef]
- Rogler, G.; Evavricka, S. Anemia in Inflammatory Bowel Disease: An Under-Estimated Problem? Front. Med. 2015, 1, 58. [Google Scholar] [CrossRef]
- Evstatiev, R.; Gasche, C. Iron sensing and signalling. Gut 2011, 61, 933–952. [Google Scholar] [CrossRef]
- Gasche, C.; Lomer, M.C.E.; Cavill, I.; Weiss, G. Iron, anaemia, and inflammatory bowel diseases. Gut 2004, 53, 1190–1197. [Google Scholar] [CrossRef]
- Young, I.; Parker, H.M.; Rangan, A.M.; Prvan, T.; Cook, R.L.; Donges, C.E.; Steinbeck, K.; O’Dwyer, N.; Cheng, H.L.; Franklin, J.; et al. Association between Haem and Non-Haem Iron Intake and Serum Ferritin in Healthy Young Women. Nutrients 2018, 10, 81. [Google Scholar] [CrossRef] [PubMed]
- Gulec, S.; Anderson, G.J.; Collins, J.F. Mechanistic and regulatory aspects of intestinal iron absorption. Am. J. Physiol. Liver Physiol. 2014, 307, G397–G409. [Google Scholar] [CrossRef] [PubMed]
- Adrian, R.W.; Oates, P.S. Mechanisms of heme iron absorption: Current questions and controversies. World J. Gastroenterol. 2008, 14, 4101–4110. [Google Scholar] [CrossRef]
- Bhandari, S.; Pereira, D.I.A.; Chappell, H.F.; Drakesmith, A. Intravenous Irons: From Basic Science to Clinical Practice. Pharmaceuticals 2018, 11, 82. [Google Scholar] [CrossRef] [PubMed]
- Ganz, T.; Nemeth, E. Hepcidin and iron homeostasis. Biochim. Biophys. Acta Bioenerg. 2012, 1823, 1434–1443. [Google Scholar] [CrossRef] [PubMed]
- Kaitha, S.; Bashir, M.; Ali, T. Iron deficiency anemia in inflammatory bowel disease. World J. Gastrointest. Pathophysiol. 2015, 6, 62–72. [Google Scholar] [CrossRef]
- Niepel, D.; Klag, T.; Malek, N.P.; Wehkamp, J. Practical guidance for the management of iron deficiency in patients with inflammatory bowel disease. Ther. Adv. Gastroenterol. 2018, 11, 1–16. [Google Scholar] [CrossRef]
- Nielsen, O.H.; Soendergaard, C.; Vikner, M.E.; Weiss, G. Rational Management of Iron-Deficiency Anaemia in Inflammatory Bowel Disease. Nutrients 2018, 10, 82. [Google Scholar] [CrossRef]
- World Health Organisation. Centers for Disease Control and Prevention. Assessing the Iron Status or Populations, 2nd ed.; World Health Organisation: Geneva, Switzerland, 2007. [Google Scholar]
- Dignass, A.; Gasche, C.; Bettenworth, D.; Birgegård, G.; Danese, S.; Gisbert, J.P.; Gomollón, F.; Iqbal, T.; Katsanos, K.; Koutroubakis, I.; et al. European Consensus on the Diagnosis and Management of Iron Deficiency and Anaemia in Inflammatory Bowel Diseases. J. Crohns Colitis 2015, 9, 211–222. [Google Scholar] [CrossRef]
- Reinisch, W.; Staun, M.; Bhandari, S.; Muñoz, M. State of the iron: How to diagnose and efficiently treat iron deficiency anemia in inflammatory bowel disease. J. Crohns Colitis 2013, 7, 429–440. [Google Scholar] [CrossRef]
- Oustamanolakis, P.; Koutroubakis, I.E.; Messaritakis, I.; Kefalogiannis, G.; Niniraki, M.; Kouroumalis, E.A. Measurement of reticulocyte and red blood cell indices in the evaluation of anemia in inflammatory bowel disease. J. Crohns Colitis 2011, 5, 295–300. [Google Scholar] [CrossRef] [PubMed]
- Stein, J.; Dignass, A.U. Management of iron deficiency anemia in inflammatory bowel disease—A practical approach. Ann. Gastroenterol. 2013, 26, 104–113. [Google Scholar] [PubMed]
- Nielsen, O.H.; Ainsworth, M.; Coskun, M.; Weiss, G. Management of Iron-Deficiency Anemia in Inflammatory Bowel Disease. Medicine 2015, 94, e963. [Google Scholar] [CrossRef] [PubMed]
- Gisbert, J.P.; Gomollón, F. Common Misconceptions in the Diagnosis and Management of Anemia in Inflammatory Bowel Disease. Am. J. Gastroenterol. 2008, 103, 1299–1307. [Google Scholar] [CrossRef] [PubMed]
- Lopez, A.; Cacoub, P.; Macdougall, I.C.; Peyrin-Biroulet, L. Iron deficiency anaemia. Lancet 2016, 387, 907–916. [Google Scholar] [CrossRef]
- Stein, J.; Hartmann, F.; Dignass, A. Diagnosis and management of iron deficiency anemia in patients with IBD. Nat. Rev. Gastroenterol. Hepatol. 2010, 7, 599–610. [Google Scholar] [CrossRef]
- World Health Organization. Nutritional Anaemias: Tools for Effective Prevention and Control; World Health Organisation: Geneva, Switzerland, 2017. [Google Scholar]
- Gisbert, J.P.; Bermejo, F.; Pajares, R.; Pérez-Calle, J.-L.; Rodríguez, M.; Algaba, A.; Mancenido, N.; De La Morena, C.S.F.; Carneros, J.A.; McNicholl, A.G.; et al. Oral and intravenous iron treatment in inflammatory bowel disease: Hematological response and quality of life improvement. Inflamm. Bowel Dis. 2009, 15, 1485–1491. [Google Scholar] [CrossRef]
- Kulnigg, S.; Gasche, C. Systematic review: Managing anaemia in Crohn’s disease. Aliment. Pharmacol. Ther. 2006, 24, 1507–1523. [Google Scholar] [CrossRef]
- Gómez-Ramírez, S.; Brilli, E.; Tarantino, G.; Muñoz, M. Sucrosomial® Iron: A New Generation Iron for Improving Oral Supplementation. Pharmaceuticals 2018, 11, 97. [Google Scholar] [CrossRef]
- Fuqua, B.K.; Vulpe, C.D.; Anderson, G.J. Intestinal iron absorption. J. Trace Elem. Med. Biol. 2012, 26, 115–119. [Google Scholar] [CrossRef]
- Stoffel, N.U.; Cercamondi, C.I.; Brittenham, G.; Zeder, C.; Geurts-Moespot, A.J.; Swinkels, D.W.; Zimmermann, M.B. Iron absorption from oral iron supplements given on consecutive versus alternate daus and as single morning doses versus twice-daily split dosing in iron-depleted women: Two open-label, randomised controlled trials. Lancet Haematol. 2017, 4, e524–e533. [Google Scholar] [CrossRef]
- Moretti, D.; Goede, J.S.; Zeder, C.; Jiskra, M.; Chatzinakou, V.; Tjalsma, H.; Melse-Boonstra, A.; Brittenham, G.; Swinkels, D.W.; Zimmermann, M.B. Oral iron supplements increase hepcidin and decrease iron absorption from daily or twice-daily doses in iron-depleted young women. Blood 2015, 126, 1981–1989. [Google Scholar] [CrossRef] [PubMed]
- Khoury, A.P.; Pagan, K.A.; Farland, M.Z. Ferric Maltol: A New Oral Iron Formulation for the Treatment of Iron Deficiency in Adults. Ann. Pharmacother. 2020. [Google Scholar] [CrossRef] [PubMed]
- Asche, C.; Ahmad, T.; Tulassay, Z.; Baumgart, D.C.; Bokemeyer, B.; Büning, C.; Howaldt, S.; Stallmach, A. Ferric maltol is effective in correcting iron deficiency anemia in patients with inflammatory bowel disease: Results from a phase 3 clinical trial program. Inflamm. Bowel Dis. 2015, 21, 579–588. [Google Scholar] [CrossRef]
- Howaldt, S.; Jacob, I.; Sampson, M.; Akriche, F. P567 Impact of oral ferric maltol and IV iron on health-related quality of life in patients with iron deficiency anaemia and inflammatory bowel disease, and relationship with haemoglobin and serum iron. J. Crohns Colitis 2020, 14, S478–S479. [Google Scholar] [CrossRef]
- Accrufer. Package Insert; Shield Therapeutics 2019, UK. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/212320Orig1s000lbl.pdf (accessed on 15 October 2020).
- Riccio, E.; Sabbatini, M.; Capuano, I.; Pellegrino, A.M.; Petruzzelli, L.A.; Pisani, A. Oral Sucrosomial® iron versus intravenous iron for recovering iron deficiency anaemia in ND-CKD patients: A cost-minimization analysis. BMC Nephrol. 2020, 21, 1–8. [Google Scholar] [CrossRef]
- Abbati, G.; Incerti, F.; Boarini, C.; Pileri, F.; Bocchi, D.; Ventura, P.; Buzzetti, E.; Pietrangelo, A. Safety and efficacy of sucrosomial iron in inflammatory bowel disease patients with iron deficiency anemia. Intern. Emerg. Med. 2018, 14, 423–431. [Google Scholar] [CrossRef]
- Howaldt, S.; Jacob, I.; Sampson, M.; Akriche, F. P331 Productivity loss in patients with inflammatory bowel disease receiving treatment for iron deficiency anaemia: A comparison of ferric maltol and IV iron. J. Crohns Coliti 2020, 14, S319–S320. [Google Scholar] [CrossRef]
- Cook, J.D. Diagnosis and management of iron-deficiency anaemia. Best Pr. Res. Clin. Haematol. 2005, 18, 319–332. [Google Scholar] [CrossRef]
- Gasche, C.; Berstad, A.; Befrits, R.; Beglinger, C.; Dignass, A.; Erichsen, K.; Gomollón, F.; Hjortswang, H.; Koutroubakis, I.; Kulnigg, S.; et al. Guidelines on the diagnosis and management of iron deficiency and anemia in inflammatory bowel diseases. Inflamm. Bowel Dis. 2007, 13, 1545–1553. [Google Scholar] [CrossRef]
- Lee, T.; Clavel, T.; Smirnov, K.; Schmidt, A.; Lagkouvardos, I.; Walker, A.; Lucio, M.; Michalke, B.; Schmitt-Kopplin, P.; Fedorak, R.; et al. Oral versus intravenous iron replacement therapy distinctly alters the gut microbiota and metabolome in patients with IBD. Gut 2016, 66, 863–871. [Google Scholar] [CrossRef] [PubMed]
- Koch, T.A.; Myers, J.; Goodnough, L.T. Intravenous Iron Therapy in Patients with Iron Deficiency Anemia: Dosing Considerations. Anemia 2015, 2015, 763576. [Google Scholar] [CrossRef] [PubMed]
- Stein, J.; Connor, S.; Virgin, G.; Ong, D.E.H.; Pereyra, L. Anemia and iron deficiency in gastrointestinal and liver conditions. World J. Gastroenterol. 2016, 22, 7908–7925. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.W.; Kolber, M.R.; Fedorak, R.N.; Van Zanten, S.V. Iron replacement therapy in inflammatory bowel disease patients with iron deficiency anemia: A systematic review and meta-analysis. J. Crohns Colitis 2012, 6, 267–275. [Google Scholar] [CrossRef] [PubMed]
- Auerbach, M.; Ballard, H. Clinical Use of Intravenous Iron: Administration, Efficacy, and Safety. Hematology 2010, 2010, 338–347. [Google Scholar] [CrossRef]
- Chertow, G.M.; Mason, P.D.; Vaage-Nilsen, O.; Ahlmén, J. Update on adverse drug events associated with parenteral iron. Nephrol. Dial. Transplant. 2005, 21, 378–382. [Google Scholar] [CrossRef]
- Muñoz, M.; Gómez-Ramírez, S.; García-Erce, J.A.; Muñoz, S.G.M.; Ramí, M.; Rez, J.; Garciacute, A.; Erce, A. Intravenous iron in inflammatory bowel disease. World J. Gastroenterol. 2009, 15, 4666–4674. [Google Scholar] [CrossRef][Green Version]
- Venofer (Iron Sucrose). Electronic Medicines Compendium. Available online: https://www.medicines.org.uk/emc/product/5911/smpc#gref (accessed on 15 October 2020).
- Schröder, O.; Mickisch, O.; Seidler, U.; De Weerth, A.; Dignass, A.U.; Herfarth, H.; Reinshagen, M.; Schreiber, S.; Junge, U.; Schrott, M.; et al. Intravenous iron sucrose is superior to oral iron supplementation for the treatment of iron deficiency anemia in patients with inflammatory bowel disease—A randomised, controlled, open-label, multicentre study. Am. J. Gastroenterol. 2005, 100, 2503–2509. [Google Scholar] [CrossRef]
- Kooistra, M.P.; Kersting, S.; Gosriwatana, I.; Lu, S.; Nijhoff-Schutte, J.; Hider, R.C.; Marx, J.J. Non-transferrin bound iron in the plasma of haemodialysis patients after intravenous iron saccharate infusion. Eur. J. Clin. Investig. 2002, 32, 36–41. [Google Scholar] [CrossRef]
- Ferrinject (Ferric Carboxymaltose). Electronic Medicines Compendium. Available online: https://www.medicines.org.uk/emc/product/5910/smpc#gref (accessed on 15 October 2020).
- Kulnigg, S.; Stoinov, S.; Simanenkov, V.; Dudar, L.V.; Karnafel, W.; Garcia, L.C.; Sambuelli, A.M.; D’Haens, G.; Gasche, C. A Novel Intravenous Iron Formulation for Treatment of Anemia in Inflammatory Bowel Disease: The Ferric Carboxymaltose (FERINJECT®) Randomized Controlled Trial. Am. J. Gastroenterol. 2008, 103, 1182–1192. [Google Scholar] [CrossRef]
- Evstatiev, R.; Marteau, P.; Iqbal, T.; Khalif, I.L.; Stein, J.; Bokemeyer, B.; Chopey, I.V.; Gutzwiller, F.S.; Riopel, L.; Gasche, C. FERGIcor, a Randomized Controlled Trial on Ferric Carboxymaltose for Iron Deficiency Anemia in Inflammatory Bowel Disease. Gastroenterology 2011, 141, 846–853.e2. [Google Scholar] [CrossRef] [PubMed]
- Wolf, M.; Koch, T.A.; Bregman, D.B. Effects of iron deficiency anemia and its treatment on fibroblast growth factor 23 and phosphate homeostasis in women. J. Bone Miner. Res. 2013, 28, 1793–1803. [Google Scholar] [CrossRef] [PubMed]
- Silverstein, S.B.; Rodgers, G.M. Parenteral iron therapy options. Am. J. Hematol. 2004, 76, 74–78. [Google Scholar] [CrossRef] [PubMed]
- McCormack, P.L. Ferumoxytol: In iron deficiency anaemia in adults with chronic kidney disease. Drugs 2012, 72, 2013–2022. [Google Scholar] [CrossRef]
- Provenzano, R.; Schiller, B.; Rao, M.; Coyne, D.; Brenner, L.; Pereira, B.J. Ferumoxytol as an intravenous iron replacement therapy in hemodialysis patients. Clin. J. Am. Soc. Nephrol. 2009, 4, 386–393. [Google Scholar] [CrossRef]
- Bailie, G.R. Compariuson of rates of reported adverse events associated with i.v. iron products in the United States. Am. J. Health Syst. Pharm. 2012, 69, 310–320. [Google Scholar] [CrossRef]
- Schieda, N. Parenteral ferumoxytol interaction with magnetic resonance imaging: A case report, review of the literature and advisory warning. Insights Imaging 2013, 4, 509–512. [Google Scholar] [CrossRef]
- Kalra, P.A.; Bhandari, S. Efficacy and safety of iron isomaltoside (Monofer®) in the management of patients with iron deficiency anemia. Int. J. Nephrol. Renov. Dis. 2016, 9, 53–64. [Google Scholar] [CrossRef]
- Monofer. Electronic Medicines Compendium. Available online: https://www.medicines.org.uk/EMC/medicine/23669/SPC/Monofer+100%C2%A0mg+ml+solution+for+injection+infusion/#gref (accessed on 15 October 2020).
- Stein, J.; Walper, A.; Klemm, W.; Farrag, K.; Aksan, A.C.; Dignass, A. Safety and efficacy of intravenous iron isomaltoside for correction of anaemia in patients with inflammatory bowel disease in everyday clinical practice. Scand. J. Gastroenterol. 2018, 53, 1059–1065. [Google Scholar] [CrossRef]
- Bonovas, S.; Fiorino, G.; Allocca, M.; Lytras, T.; Tsantes, A.; Peyrin-Biroulet, L.; Danese, S. Intravenous versus oral iron for the treatment of anemia in inflammatory bowel disease: A systematic review and meta-analysis of randomised controlled trials. Medicine 2006, 95, e2308. [Google Scholar] [CrossRef]
- Stein, J.; Haas, J.S.; Ong, S.H.; Borchert, K.; Hardt, T.; Lechat, E.; Nip, K.; Foerster, D.; Braun, S.; Baumgart, D.C. Oral versus intravenous iron therapy in patients with inflammatory bowel disease and iron deficiency with and without anemia in Germany—A real-world evidence analysis. Clin. Outcomes Res. 2018, 10, 93–103. [Google Scholar] [CrossRef] [PubMed]
- Rampton, D.S.; Folkersen, J.; Fishbane, S.; Hedenus, M.; Howaldt, S.; Locatelli, F.; Patni, S.; Szebeni, J.; Weiss, G. Hypersensitivity reactions to intravenous iron: Guidance for risk minimization and management. Haematologica 2014, 99, 1671–1676. [Google Scholar] [CrossRef] [PubMed]
- Rizvi, S.; Schoen, R.E. Supplementation With Oral vs. Intravenous Iron for Anemia With IBD or Gastrointestinal Bleeding: Is Oral Iron Getting a Bad Rap? Am. J. Gastroenterol. 2011, 106, 1872–1879. [Google Scholar] [CrossRef] [PubMed]
- Jimenez, K.; Gasche, C.; Auerbach, M. On both sides of the ocean. Blood Transfus. 2016, 14, 197. [Google Scholar] [PubMed]
- Abhyankar, A.; Moss, A.C. Iron Replacement in Patients with Inflammatory Bowel Disease: A Systematic Review and Meta-analysis. Inflamm. Bowel Dis. 2015, 21, 1976–1981. [Google Scholar] [CrossRef] [PubMed]
- Jairath, V.; Kahan, B.C.; Gray, A.; Doré, C.J.; Mora, A.; Dyer, C.; Stokes, E.A.; Llewelyn, C.; Bailey, A.; Dallal, H.; et al. Restrictive vs. Liberal Blood Transfusion for Acute Upper Gastrointestinal Bleeding: Rationale and Protocol for a Cluster Randomized Feasibility Trial. Transfus. Med. Rev. 2013, 27, 146–153. [Google Scholar] [CrossRef][Green Version]
- Tsiolakidou, G.; Koutroubakis, I.E. Stimulating erythropoiesis in inflammatory bowel disease associated anemia. World J. Gastroenterol. 2007, 13, 4798–4806. [Google Scholar] [CrossRef]
- Unger, E.F.; Thompson, A.M.; Blank, M.J.; Temple, R. Erythropoiesis-Stimulating Agents—Time for a Reevaluation. N. Engl. J. Med. 2010, 362, 189–192. [Google Scholar] [CrossRef]
- Kulnigg, S.; Teischinger, L.; Dejaco, C.; Waldhoer, T.; Gasche, C. W1124 Rapid Recurrence of IBD-Associated Anemia and Iron Deficiency After Intravenous Iron Sucrose and Erythropoietin Treatment. Gastroenterology 2009, 136, 1460–1467. [Google Scholar] [CrossRef]
| Type of Anaemia | Definition of Anaemia | Diagnosis | Microscopic Findings | Management |
|---|---|---|---|---|
| IDA | Women: Hb < 120 g/L Men: Hb < 130 g/L Pregnancy: Hb < 110 g/L | Low serum iron Low ferritin (<30 ug/L) Serum ferritin < 100 ug/L in inflammatory disease Low transferrin saturation (TSAT < 20%) Transferrin levels increased Reduced MCH | Microcytic and hypochromic erythrocytes | Oral or IV replacement Blood transfusion |
| Vitamin B12 deficiency | Low B12 levels Elevated methylmalonic acid Elevated total homocysteine Elevated MCH | Megaloblastic anaemia | High dose IV or oral B12 replacement | |
| ACD | Low reticulocyte count Low iron Low TSAT (<20%) Transferrin levels normal or decreased Normal or raised Ferritin (<100) Low or normal MCH | Normochromic and normocytic erythrocytes | Treatment of underlying condition Blood transfusions Erythropoiesis stimulating agents | |
| IDA and ACD | Normal or raised transferrin saturation Normal or reduced MCH | Hypochromic erythrocytes |
| Molecular Weight | Half-Life | Administration | Disadvantages/Risks | |
|---|---|---|---|---|
| HMW Dextran (DexFerrum) | 100–500 kDa | 3–4 days | Single dose | Anaphylactoid reaction |
| LMW Dextran (CosmoFer) | 73 kDa | 5–20 h | Maximum single infusion of 20 mg/kg over 4–6 h | Immunoglobulin-E mediated anaphylactoid reaction |
| Sucrose (Venofer) | 34–60 kDa | 5–6 h | Single infusion up to 200 mg over 30 min | Multiple sessions needed in severe anaemia |
| Carboxymaltose (Ferrinject) | 150 kDa | 7–12 h | Single dose infusion of 1000 mg over 15 min (max dose of 20 mg/kg) | Hypophosphataemia |
| Isomaltoside (Monofer) | 1000 kDa | 1–4 days | Limited data in IBD | |
| Gluconate (Ferrlecit) | 37 kDa | 1 h | 8 infusions of 125 mg | Not currently for use in IBD |
| Ferumoxytol | 721 kDa | 14–21 h | 510 mg can be given in less than 1 min | High rate of adverse events Interference with MRI |
| Oral Iron | IV Iron | |
|---|---|---|
| Choice of administration | Mild IDA (Hb > 100 g/L) Quiescent IBD | Severe anaemia (Hb < 100 g/L) Intolerant to oral iron Moderate to severe IBD activity |
| Pros | Greater availability Ease of administration Low cost | Bypasses GI tract absorption Less side effects |
| Cons | Side effects with poor patient tolerance Discontinuation in 20% Increases IBD activity Disrupts microbiome | Low bioavailability Inconvenience of IV application Greater cost Risk of hypersensitivity reaction * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kumar, A.; Brookes, M.J. Iron Therapy in Inflammatory Bowel Disease. Nutrients 2020, 12, 3478. https://doi.org/10.3390/nu12113478
Kumar A, Brookes MJ. Iron Therapy in Inflammatory Bowel Disease. Nutrients. 2020; 12(11):3478. https://doi.org/10.3390/nu12113478
Chicago/Turabian StyleKumar, Aditi, and Matthew J. Brookes. 2020. "Iron Therapy in Inflammatory Bowel Disease" Nutrients 12, no. 11: 3478. https://doi.org/10.3390/nu12113478
APA StyleKumar, A., & Brookes, M. J. (2020). Iron Therapy in Inflammatory Bowel Disease. Nutrients, 12(11), 3478. https://doi.org/10.3390/nu12113478





