Child Consumption of Whole Fruit and Fruit Juice Following Six Months of Exposure to a Pediatric Fruit and Vegetable Prescription Program
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Study Design
2.3. Pediatric Fruit and Vegetable Prescription Program
2.4. Participants and Data Collection
2.5. Evaluation Tools
2.5.1. Fruit Consumption
2.5.2. Participation in Food Assistance Programs
2.5.3. Food Security
2.6. Statistical Analyses
3. Results
3.1. Fruit and Vegetable Consumption
3.2. Participation in Food Assistance Programs
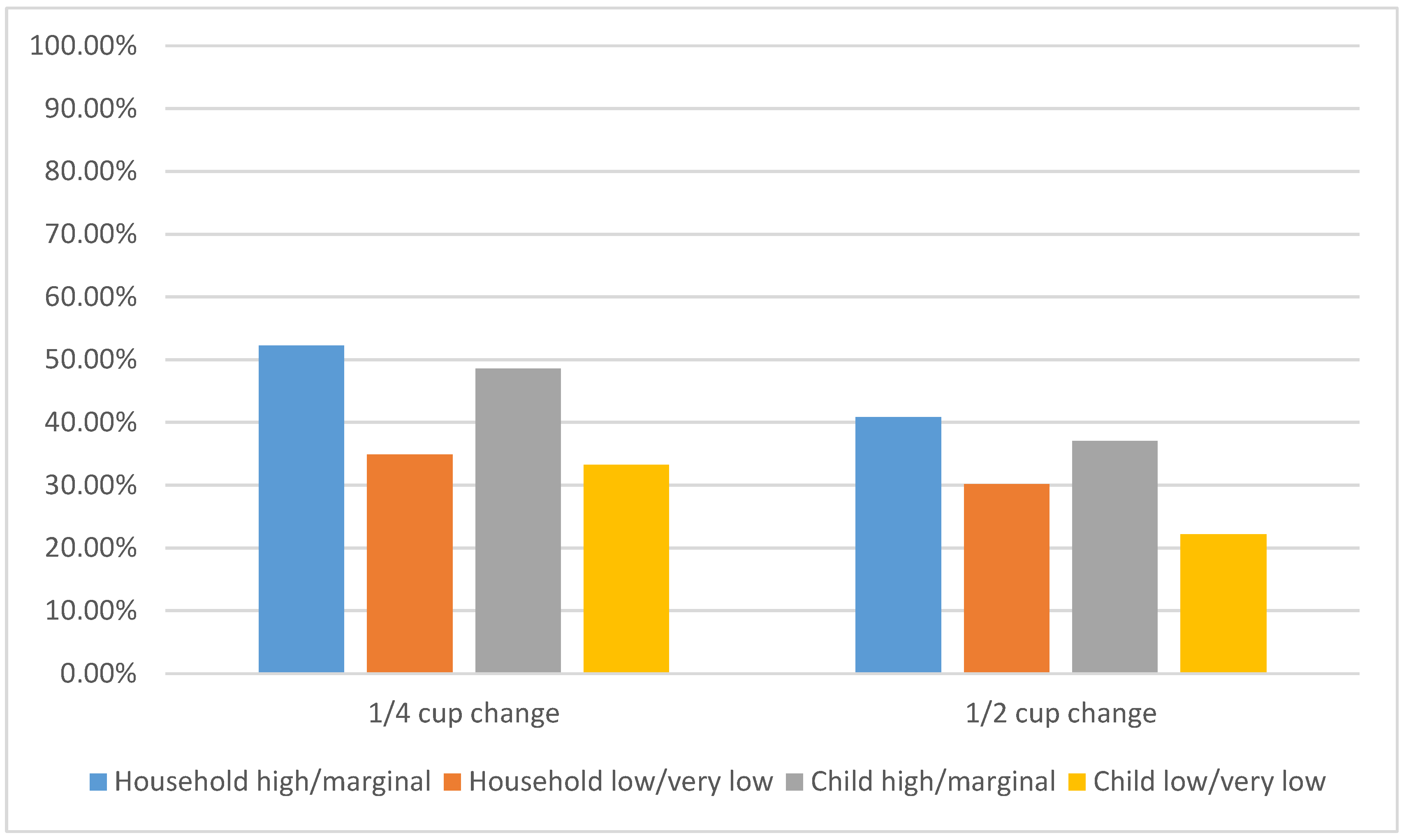
3.3. Food Security
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Dreher, M.L. Whole fruits and fruit fiber emerging health effects. Nutrients 2018, 10, 1833. [Google Scholar] [CrossRef] [PubMed]
- Ho, K.K.K.Y.; Ferruzzi, M.G.; Wightman, J.D. Potential health benefits of (poly)phenols derived from fruit and 100% fruit juice. Nutr. Rev. 2019. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Mateos, A.; Heiss, C.; Borges, G.; Crozier, A. Berry (poly)phenols and cardiovascular health. J. Agric. Food Chem. 2014, 62, 3842–3851. [Google Scholar] [CrossRef] [PubMed]
- Willett, W.C.; Stampfer, M.J. Current evidence on healthy eating. Annu. Rev. Public Health 2013, 34, 77–95. [Google Scholar] [CrossRef] [PubMed]
- Muraki, I.; Imamura, F.; Manson, J.E.; Hu, F.B.; Willett, W.C.; van Dam, R.M.; Sun, Q. Fruit consumption and risk of type 2 diabetes: Results from three prospective longitudinal cohort studies. BMJ 2013, 347, f5001. [Google Scholar] [CrossRef] [PubMed]
- Saxe-Custack, A.; Lofton, H.C.; Hanna-Attisha, M.; Victor, C.; Reyes, G.; Ceja, T.; LaChance, J. Caregiver perceptions of a fruit and vegetable prescription programme for low-income paediatric patients. Public Health Nutr. 2018, 21, 2497–2506. [Google Scholar] [CrossRef]
- Oddy, W.H.; Robinson, M.; Ambrosini, G.L.; O’Sullivan, T.A.; de Klerk, N.H.; Beilin, L.J.; Silburn, S.R.; Zubrick, S.R.; Stanley, F.J. The association between dietary patterns and mental health in early adolescence. Prev. Med. 2009, 49, 39–44. [Google Scholar] [CrossRef]
- Huang, P.; O’Keeffe, M.; Elia, C.; Karamanos, A.; Goff, L.M.; Maynard, M.; Cruickshank, J.K.; Harding, S. Fruit and vegetable consumption and mental health across adolescence: Evidence from a diverse urban British cohort study. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 19. [Google Scholar] [CrossRef]
- Miki, T.; Eguchi, M.; Kurotani, K.; Kochi, T.; Kuwahara, K.; Ito, R.; Kimura, Y.; Tsuruoka, H.; Akter, S.; Kashino, I. Dietary fiber intake and depressive symptoms in Japanese employees: The Furukawa Nutrition and Health Study. Nutrition 2016, 32, 584–589. [Google Scholar] [CrossRef]
- de Vries, J.; Birkett, A.; Hulshof, T.; Verbeke, K.; Gibes, K. Effects of cereal, fruit and vegetable fibers on human fecal weight and transit time: A comprehensive review of intervention trials. Nutrients 2016, 8, 130. [Google Scholar] [CrossRef]
- Lorson, B.A.; Melgar-Quinonez, H.R.; Taylor, C.A. Correlates of fruit and vegetable intakes in US children. J. Am. Diet. Assoc. 2009, 109, 474–478. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.A.; Moore, L.V.; Galuska, D.; Wright, A.P.; Harris, D.; Grummer-Strawn, L.M.; Merlo, C.L.; Nihiser, A.J.; Rhodes, D.G.; Division of nutrition, physical activity, and obesity, national center for chronic disease prevention and health promotion, CDC. Vital signs: Fruit and vegetable intake among children—United States, 2003–2010. MMWR Morb. Mortal. Wkly. Rep. 2014, 63, 671–676. [Google Scholar] [PubMed]
- Hodder, R.K.; Stacey, F.G.; Wyse, R.J.; O’Brien, K.M.; Clinton-McHarg, T.; Tzelepis, F.; Nathan, N.K.; James, E.L.; Bartlem, K.M.; Sutherland, R.; et al. Interventions for increasing fruit and vegetable consumption in children aged five years and under. Cochrane Database Syst. Rev. 2017, 9, CD008552. [Google Scholar] [CrossRef] [PubMed]
- Maynard, M.; Gunnell, D.; Emmett, P.; Frankel, S.; Davey Smith, G. Fruit, vegetables, and antioxidants in childhood and risk of adult cancer: The Boyd Orr cohort. J. Epidemiol. Community Health 2003, 57, 218–225. [Google Scholar] [CrossRef]
- Laitinen, T.T.; Nuotio, J.; Juonala, M.; Niinikoski, H.; Rovio, S.; Viikari, J.S.A.; Rönnemaa, T.; Magnussen, C.G.; Jokinen, E.; Lagström, H.; et al. Success in achieving the targets of the 20-year infancy-onset dietary intervention: Association with insulin sensitivity and serum lipids. Diabetes Care 2018, 41, 2236–2244. [Google Scholar] [CrossRef]
- Saeedi, P.; Shavandi, A.; Skidmore, P.M.L. What do we know about diet and markers of cardiovascular health in children: A review. Int. J. Environ. Res. Public Health 2019, 16, 548. [Google Scholar] [CrossRef]
- Deroover, K.; Bucher, T.; Vandelanotte, C.; de Vries, H.; Duncan, M.J. Practical nutrition knowledge mediates the relationship between sociodemographic characteristics and diet quality in adults: A cross-sectional analysis. Am. J. Health Promot. 2019. [Google Scholar] [CrossRef]
- McKinnon, L.; Giskes, K.; Turrell, G. The contribution of three components of nutrition knowledge to socio-economic differences in food purchasing choices. Public Health Nutr. 2014, 17, 1814–1824. [Google Scholar] [CrossRef]
- Mayfield, K.E.; Carolan, M.; Weatherspoon, L.; Chung, K.R.; Hoerr, S.M. African American women’s perceptions on access to food and water in Flint, Michigan. J. Nutr. Educ. Behav. 2017, 49, 519–524. [Google Scholar] [CrossRef]
- Zenk, S.N.; Odoms-Young, A.M.; Dallas, C.; Hardy, E.; Watkins, A.; Hoskins-Wroten, J.; Holland, L. You have to hunt for the fruits, the vegetables: Environmental barriers and adaptive strategies to acquire food in a low-income African American neighborhood. Health Educ. Behav. 2011, 38, 282–292. [Google Scholar] [CrossRef]
- Baker, E.A.; Schootman, M.; Barnidge, E.; Kelly, C. The role of race and poverty in access to foods that enable individuals to adhere to dietary guidelines. Prev. Chronic Dis. 2006, 3, A76. [Google Scholar] [PubMed]
- Heyman, M.B.; Abrams, S.A.; Section on gastroenterology, hepatology, and nutrition and committee on nutrition. Fruit juice in infants, children, and adolescents: Current recommendations. Pediatrics 2017, 139, e20170967. [Google Scholar] [CrossRef] [PubMed]
- Byrd-Bredbenner, C.; Ferruzzi, M.G.; Fulgoni, V.L., 3rd; Murray, R.; Pivonka, E.; Wallace, T.C. Satisfying America’s fruit gap: Summary of an expert roundtable on the role of 100% fruit juice. J. Food Sci. 2017, 82, 1523–1534. [Google Scholar] [CrossRef] [PubMed]
- Drewnowski, A.; Rehm, C.D. Socioeconomic gradient in consumption of whole fruit and 100% fruit juice among US children and adults. Nutr. J. 2015, 14, 3. [Google Scholar] [CrossRef] [PubMed]
- Auerbach, B.J.; Dibey, S.; Vallila-Buchman, P.; Kratz, M.; Krieger, J. Review of 100% fruit juice and chronic health conditions: Implications for sugar-sweetened beverage policy. Adv. Nutr. 2018, 9, 78–85. [Google Scholar] [CrossRef] [PubMed]
- Abrams, S.A.; Daniels, S.R. Fruit juice and child health. Pediatrics 2017, 139, e20170041. [Google Scholar] [CrossRef]
- Munoz, K.A.; Krebs-Smith, S.M.; Ballard-Barbash, R.; Cleveland, L.E. Food intakes of US children and adolescents compared with recommendations. Pediatrics 1997, 100, 323–329. [Google Scholar] [CrossRef]
- Di Noia, J.; Byrd-Bredbenner, C. Determinants of fruit and vegetable intake in low-income children and adolescents. Nutr. Rev. 2014, 72, 575–590. [Google Scholar] [CrossRef]
- Lee, J.; Kubik, M.Y.; Fulkerson, J.A. Diet quality and fruit, vegetable, and sugar-sweetened beverage consumption by household food insecurity among 8- to 12-year-old children during summer months. J. Acad. Nutr. Diet. 2019, 119, 1695–1702. [Google Scholar] [CrossRef]
- Saxe-Custack, A.; LaChance, J.; Hanna-Attisha, M.; Ceja, T. Fruit and vegetable prescriptions for pediatric patients living in Flint, Michigan: A cross-sectional study of food security and dietary patterns at baseline. Nutrients 2019, 11, 1423. [Google Scholar] [CrossRef]
- Buyuktuncer, Z.; Kearney, M.; Ryan, C.L.; Thurston, M.; Ellahi, B. Fruit and vegetables on prescription: A brief intervention in primary care. J. Hum. Nutr. Diet. 2014, 27, 186–193. [Google Scholar] [CrossRef] [PubMed]
- Trapl, E.S.; Smith, S.; Joshi, K.; Osborne, A.; Benko, M.; Matos, A.T.; Bolen, S. Dietary impact of produce prescriptions for patients with hypertension. Prev. Chronic Dis. 2018, 15, E138. [Google Scholar] [CrossRef] [PubMed]
- Bryce, R.; Guajardo, C.; Ilarraza, D.; Milgrom, N.; Pike, D.; Savoie, K.; Valbuena, F.; Miller-Matero, L.R. Participation in a farmers’ market fruit and vegetable prescription program at a federally qualified health center improves hemoglobin A1C in low income uncontrolled diabetics. Prev. Med. Rep. 2017, 7, 176–179. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, S.; Horner, S.D. Barriers that influence eating behaviors in adolescents. J. Pediatr. Nurs. 2005, 20, 258–267. [Google Scholar] [CrossRef] [PubMed]
- Craigie, A.M.; Lake, A.A.; Kelly, S.A.; Adamson, A.J.; Mathers, J.C. Tracking of obesity-related behaviours from childhood to adulthood: A systematic review. Maturitas 2011, 70, 266–284. [Google Scholar] [CrossRef]
- Cruz, F.; Ramos, E.; Lopes, C.; Araujo, J. Tracking of food and nutrient intake from adolescence into early adulthood. Nutrition 2018, 55, 84–90. [Google Scholar] [CrossRef]
- Appannah, G.; Pot, G.K.; Oddy, W.H.; Jebb, S.A.; Ambrosini, G.L. Determinants of a dietary pattern linked with greater metabolic risk and its tracking during adolescence. J. Hum. Nutr. Diet. 2018, 31, 218–227. [Google Scholar] [CrossRef]
- Landry, M.J.; van den Berg, A.E.; Asigbee, F.M.; Vandyousefi, S.; Ghaddar, R.; Davis, J.N. Child-report of food insecurity is associated with diet quality in children. Nutrients 2019, 11, 1574. [Google Scholar] [CrossRef]
- Casey, P.H.; Simpson, P.M.; Gossett, J.M.; Bogle, M.L.; Champagne, C.M.; Connell, C.; Harsha, D.; McCabe-Sellers, B.; Robbins, J.M.; Stuff, J.E.; et al. The association of child and household food insecurity with childhood overweight status. Pediatrics 2006, 118, e1406–e1413. [Google Scholar] [CrossRef]
- Eisenmann, J.C.; Gundersen, C.; Lohman, B.J.; Garasky, S.; Stewart, S.D. Is food insecurity related to overweight and obesity in children and adolescents? A summary of studies, 1995–2009. Obes. Rev. 2011, 12, e73–e83. [Google Scholar] [CrossRef]
- Metallinos-Katsaras, E.; Must, A.; Gorman, K. A longitudinal study of food insecurity on obesity in preschool children. J. Acad. Nutr. Diet. 2012, 112, 1949–1958. [Google Scholar] [CrossRef] [PubMed]
- Faught, E.L.; Williams, P.L.; Willows, N.D.; Asbridge, M.; Veugelers, P.J. The association between food insecurity and academic achievement in Canadian school-aged children. Public Health Nutr. 2017, 20, 2778–2785. [Google Scholar] [CrossRef] [PubMed]
- Barnidge, E.; LaBarge, G.; Krupsky, K.; Arthur, J. Screening for food insecurity in pediatric clinical settings: Opportunities and barriers. J. Community Health 2017, 42, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Makelarski, J.A.; Abramsohn, E.; Benjamin, J.H.; Du, S.; Lindau, S.T. Diagnostic accuracy of two food insecurity screeners recommended for use in health care settings. Am. J. Public Health 2017, 107, 1812–1817. [Google Scholar] [CrossRef]
- Council on Community Pediatrics; Committee on Nutrition. Promoting food security for all children. Pediatrics 2015, 136, e1431–e1438. [Google Scholar] [CrossRef]
- Saxe-Custack, A.; Lofton, H.C.; Hanna-Attisha, M.; Tata, Z.; Ceja, T.; LaChance, J. Caregiver experiences with an innovative farmers’ market incentive program for children in Flint, Michigan. Glob. Pediatr. Health 2019. [Google Scholar] [CrossRef]
- American FactFinder, United States Census Bureau. Selected Economic Characteristics: 2013–2017 American Community Survey 5-Year Estimates for Flint City, Michigan. Available online: https://factfinder.census.gov/bkmk/table/1.0/en/ACS/17_5YR/DP03/1600000US2629000 (accessed on 26 November 2019).
- Sadler, R.C. Integrating expert knowledge in a GIS to optimize siting decisions for small-scale healthy food retail interventions. Int. J. Health Geogr. 2016, 15, 19. [Google Scholar] [CrossRef][Green Version]
- Hanna-Attisha, M.; LaChance, J.; Sadler, R.C.; Champney Schnepp, A. Elevated blood lead levels in children associated with the Flint drinking water crisis: A spatial analysis of risk and public health response. Am. J. Public Health 2016, 106, 283–290. [Google Scholar] [CrossRef]
- Zahran, S.; McElmurry, S.P.; Sadler, R.C. Four phases of the Flint water crisis: Evidence from blood lead levels in children. Environ. Res. 2017, 157, 160–172. [Google Scholar] [CrossRef]
- Hunsberger, M.; O’Malley, J.; Block, T.; Norris, J.C. Relative validation of Block Kids Food Screener for dietary assessment in children and adolescents. Matern. Child Nutr. 2015, 11, 260–270. [Google Scholar] [CrossRef]
- Nestle, M. The Supplemental Nutrition Assistance Program (SNAP): History, politics, and public health implications. Am. J. Public Health 2019, 109, 1631–1635. [Google Scholar] [CrossRef] [PubMed]
- Blumberg, S.J.; Bialostosky, K.; Hamilton, W.L.; Briefel, R.R. The effectiveness of a short form of the Household Food Security Scale. Am. J. Public Health 1999, 89, 1231–1234. [Google Scholar] [CrossRef] [PubMed]
- Connell, C.L.; Nord, M.; Lofton, K.L.; Yadrick, K. Food security of older children can be assessed using a standardized survey instrument. J. Nutr. 2004, 134, 2566–2572. [Google Scholar] [CrossRef] [PubMed]
- Owen, A.L.; Owen, G.M. Twenty years of WIC: A review of some effects of the program. J. Am. Diet. Assoc. 1997, 97, 777–782. [Google Scholar] [CrossRef]
- Sharpe, P.A.; Liese, A.D.; Bell, B.A.; Wilcox, S.; Hutto, B.E.; Stucker, J. Household food security and use of community food sources and food assistance programs among food shoppers in neighborhoods of low income and low food access. J. Hunger Environ. Nutr. 2018, 13, 482–496. [Google Scholar] [CrossRef]
- Hoophouses for Health. Available online: http://mifma.org/hoophousesforhealth/ (accessed on 16 December 2019).
- Herrick, K.A.; Rossen, L.M.; Nielsen, S.J.; Branum, A.M.; Ogden, C.L. Fruit consumption by youth in the United States. Pediatrics 2015, 136, 664–671. [Google Scholar] [CrossRef]
- Wojcicki, J.M.; Heyman, M.B. Reducing childhood obesity by eliminating 100% fruit juice. Am. J. Public Health 2012, 102, 1630–1633. [Google Scholar] [CrossRef]
- Faith, M.S.; Dennison, B.A.; Edmunds, L.S.; Stratton, H.H. Fruit juice intake predicts increased adiposity gain in children from low-income families: Weight status-by-environment interaction. Pediatrics 2006, 118, 2066–2075. [Google Scholar] [CrossRef]
- Marshall, T.A.; Levy, S.M.; Broffitt, B.; Warren, J.J.; Eichenberger-Gilmore, J.M.; Burns, T.L.; Stumbo, P.J. Dental caries and beverage consumption in young children. Pediatrics 2003, 112, e184–e191. [Google Scholar] [CrossRef]
- Xi, B.; Li, S.; Liu, Z.; Tian, H.; Yin, X.; Huai, P.; Tang, W.; Zhou, D.; Steffen, L.M. Intake of fruit juice and incidence of type 2 diabetes: A systematic review and meta-analysis. PLoS ONE 2014, 9, e93471. [Google Scholar] [CrossRef]
- Cavanagh, M.; Jurkowski, J.; Bozlak, C.; Hastings, J.; Klein, A. Veggie Rx: An outcome evaluation of a healthy food incentive programme. Public Health Nutr. 2017, 20, 2636–2641. [Google Scholar] [CrossRef] [PubMed]
- Friedman, D.B.; Freedman, D.A.; Choi, S.K.; Anadu, E.C.; Brandt, H.M.; Carvalho, N.; Hurley, T.G.; Young, V.M.; Hébert, J.R. Provider communication and role modeling related to patients’ perceptions and use of a federally qualified health center-based farmers’ market. Health Promot. Pract. 2014, 15, 288–297. [Google Scholar] [CrossRef] [PubMed]
- Muhammad, H.; Reeves, S.; Ishaq, S.; Mayberry, J.; Jeanes, Y.M. Adherence to a gluten free diet is associated with receiving gluten free foods on prescription and understanding food labelling. Nutrients 2017, 9, 705. [Google Scholar] [CrossRef] [PubMed]
- Rehm, C.D.; Drewnowski, A. Dietary and economic effects of eliminating shortfall in fruit intake on nutrient intakes and diet cost. BMC Pediatr. 2016, 16, 83. [Google Scholar] [CrossRef] [PubMed]
- Chu, Y.L.; Storey, K.E.; Veugelers, P.J. Involvement in meal preparation at home is associated with better diet quality among Canadian children. J. Nutr. Educ. Behav. 2014, 46, 304–308. [Google Scholar] [CrossRef] [PubMed]
- Berge, J.M.; MacLehose, R.F.; Larson, N.; Laska, M.; Neumark-Sztainer, D. Family food preparation and its effects on adolescent dietary quality and eating patterns. J. Adolesc. Health 2016, 59, 530–536. [Google Scholar] [CrossRef]
- Jarpe-Ratner, E.; Folkens, S.; Sharma, S.; Daro, D.; Edens, N.K. An experiential cooking and nutrition education program increases cooking self-efficacy and vegetable consumption in children in grades 3–8. J. Nutr. Educ. Behav. 2016, 48, 697–705. [Google Scholar] [CrossRef]
- Hersch, D.; Perdue, L.; Ambroz, T.; Boucher, J.L. The impact of cooking classes on food-related preferences, attitudes, and behaviors of school-aged children: A systematic review of the evidence, 2003–2014. Prev. Chronic Dis. 2014, 11, E193. [Google Scholar] [CrossRef]
- Walker, R.E.; Keane, C.R.; Burke, J.G. Disparities and access to healthy food in the United States: A review of food deserts literature. Health Place 2010, 16, 876–884. [Google Scholar] [CrossRef]
- Christoph, M.J.; Larson, N.I.; Winkler, M.R.; Wall, M.M.; Neumark-Sztainer, D. Longitudinal trajectories and prevalence of meeting dietary guidelines during the transition from adolescence to young adulthood. Am. J. Clin. Nutr. 2019, 109, 656–664. [Google Scholar] [CrossRef]
| Characteristics | Mean Change ± SD | p-Value | |
|---|---|---|---|
| Child Gender | Male (n = 51) | 0.18 ± 0.80 | 0.974 |
| Female (n = 57) | 0.19 ± 0.92 | ||
| Child Race | African American (n = 64) | 0.12 ± 0.86 | 0.725 |
| White (n = 20) | 0.19 ± 0.68 | ||
| Child Age | 7–12 years (n = 45) | 0.07 ± 0.91 | 0.288 |
| 13–18 years (n = 50) | 0.25 ± 0.72 | ||
| Caregiver Race | African American (n = 62) | 0.10 ± 0.88 | 0.188 |
| White (n = 26) | 0.37 ± 0.81 | ||
| Caregiver Age | 25–34 years (n = 29) | −0.02 ± 0.94 | 0.149 |
| 35–44 years (n = 43) | 0.38 ± 0.74 | ||
| 45+ years (n = 24) | 0.20 ± 0.86 | ||
| Caregiver Education | High school degree or less (n = 30) | 0.29 ± 0.78 | 0.932 |
| Some college/Technical school/Associate’s degree (n = 41) | 0.21 ± 0.88 | ||
| Bachelor/Graduate degree (n = 20) | 0.21 ± 0.94 |
| Food Assistance Program | Participation | Mean Change | p-Value |
|---|---|---|---|
| SNAP | Yes (n = 44) | 0.18 ± 0.86 | 0.714 |
| No (n = 52) | 0.24 ± 0.83 | ||
| School lunch | Yes (n = 57) | 0.13 ± 0.91 | 0.284 |
| No (n = 39) | 0.33 ± 0.74 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saxe-Custack, A.; LaChance, J.; Hanna-Attisha, M. Child Consumption of Whole Fruit and Fruit Juice Following Six Months of Exposure to a Pediatric Fruit and Vegetable Prescription Program. Nutrients 2020, 12, 25. https://doi.org/10.3390/nu12010025
Saxe-Custack A, LaChance J, Hanna-Attisha M. Child Consumption of Whole Fruit and Fruit Juice Following Six Months of Exposure to a Pediatric Fruit and Vegetable Prescription Program. Nutrients. 2020; 12(1):25. https://doi.org/10.3390/nu12010025
Chicago/Turabian StyleSaxe-Custack, Amy, Jenny LaChance, and Mona Hanna-Attisha. 2020. "Child Consumption of Whole Fruit and Fruit Juice Following Six Months of Exposure to a Pediatric Fruit and Vegetable Prescription Program" Nutrients 12, no. 1: 25. https://doi.org/10.3390/nu12010025
APA StyleSaxe-Custack, A., LaChance, J., & Hanna-Attisha, M. (2020). Child Consumption of Whole Fruit and Fruit Juice Following Six Months of Exposure to a Pediatric Fruit and Vegetable Prescription Program. Nutrients, 12(1), 25. https://doi.org/10.3390/nu12010025





