Sleep Quality and the Mediating Role of Stress Management on Eating by Nursing Personnel
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Instruments
2.3. Procedure
2.4. Data Analysis
3. Results
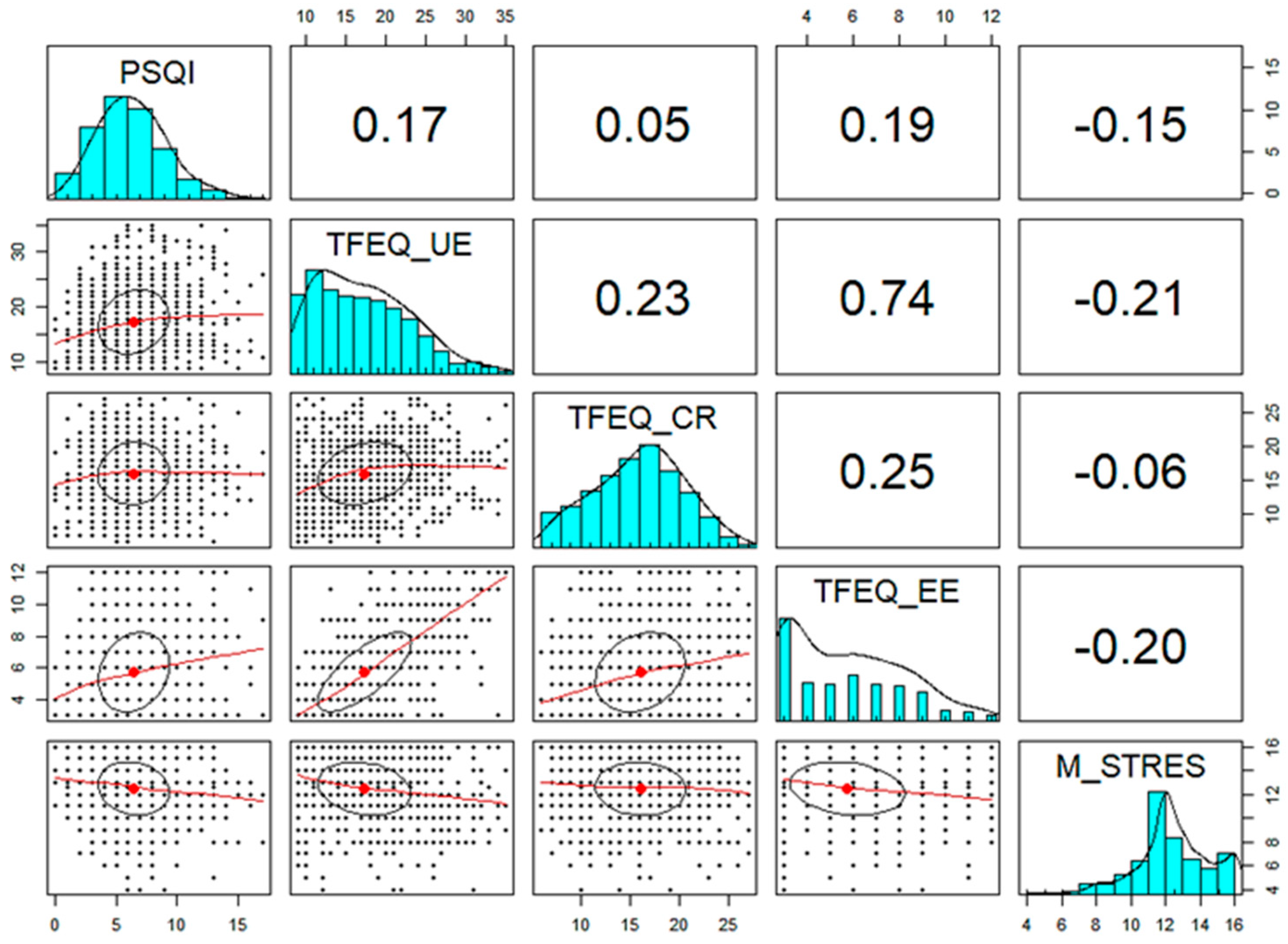
3.1. Descriptive and Correlational Analyses
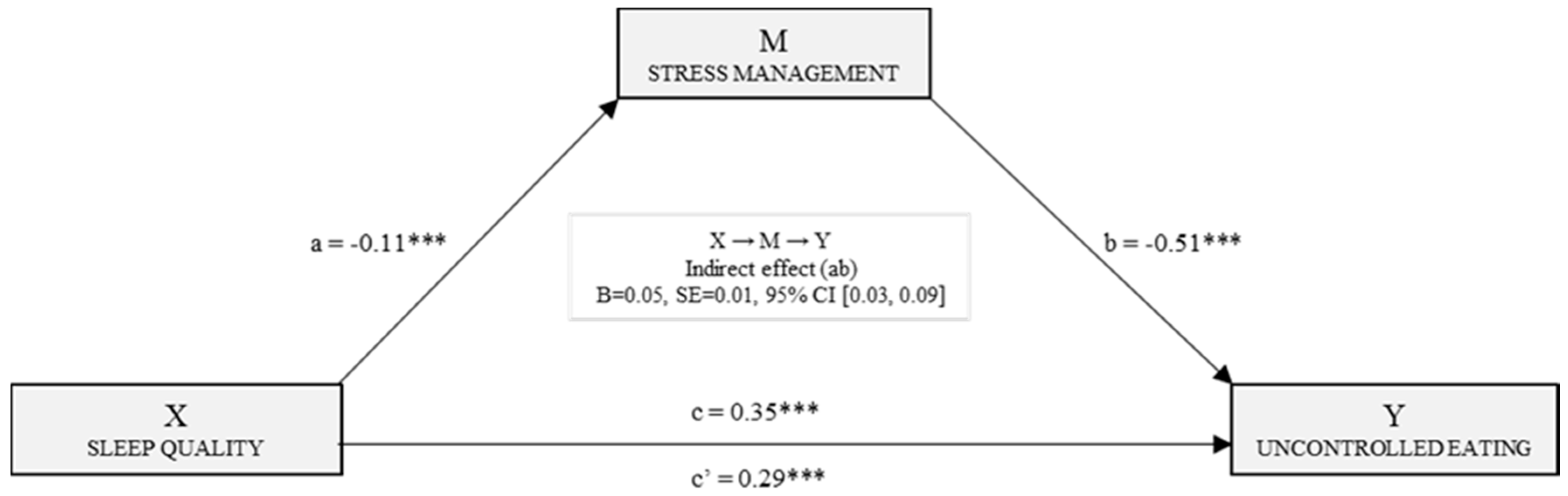
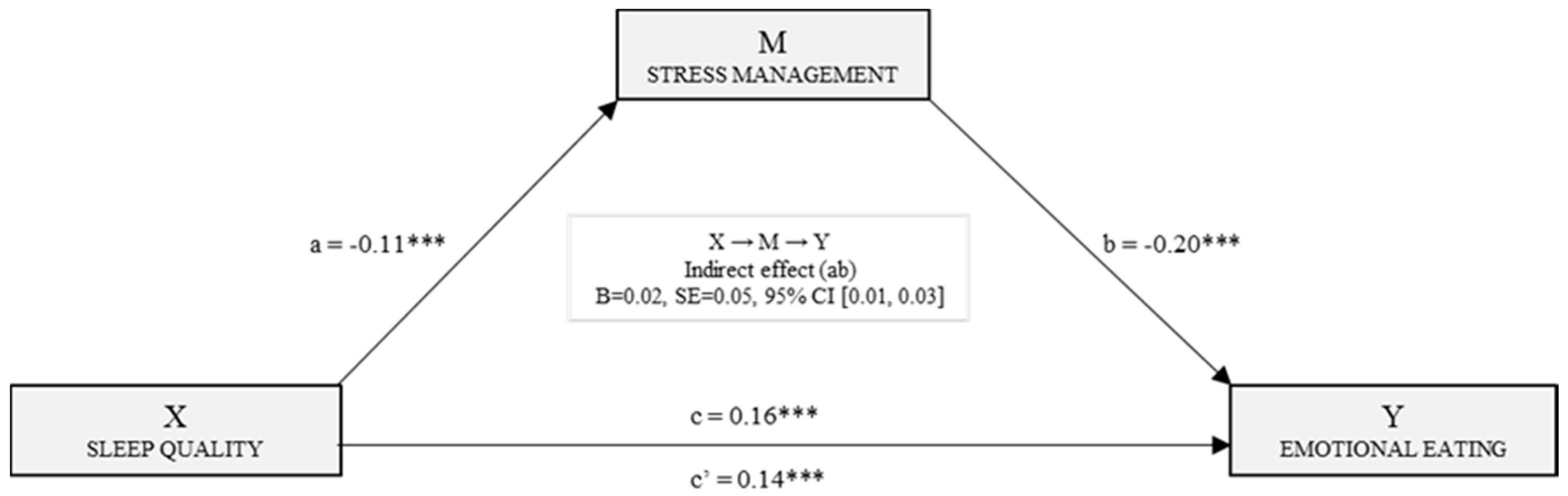
3.2. Mediation Models for Estimating the Effects on Uncontrolled and Emotional Eating
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Jafari-Roodbandi, A.; Choobineh, A.; Daneshvar, S. Relationship between circadian rhythm amplitude and stability with sleep quality and sleepiness among shift nurses and health care workers. Int. J. Occup. Saf. Ergon. 2015, 3, 312–317. [Google Scholar] [CrossRef] [PubMed]
- Dall’Ora, C.; Griffiths, P.; Ball, J.; Simon, M.; Aiken, L.H. Association of 12 h shifts and nurses’ job satisfaction, burnout and intention to leave: Findings from a cross-sectional study of 12 European countries. BMJ Open 2015, 5, e008331. [Google Scholar] [CrossRef] [PubMed]
- Becker, N.B.; de Jesus, S.N.; Viseu, J.N.; Stobäus, C.D.; Guerreiro, M.; Domingues, R.B. Depression and quality of life in older adults: Mediation effect of sleep quality. IJCHP 2018, 18, 8–17. [Google Scholar] [CrossRef]
- Miró, E.; Martínez, P.; Sánchez, A.I.; Marín, J.R. Relación entre el burnout o “síndrome de quemarse por el trabajo”, la tensión laboral y las características del sueño. Psicothema 2007, 19, 388–394. [Google Scholar] [PubMed]
- Blumfield, M.L.; Bei, B.; Zimberg, I.Z.; Cain, S.W. Dietary disinhibition mediates the relationship between poor sleep quality and body weight. Appetite 2018, 120, 602–608. [Google Scholar] [CrossRef] [PubMed]
- Kilkus, J.M.; Booth, J.N.; Bromley, L.E.; Darukhanavala, A.P.; Imperial, J.G.; Penev, P.D. Sleep and eating behavior in adults at risk for type 2 diabetes. Obesity 2012, 20, 112–117. [Google Scholar] [CrossRef] [PubMed]
- Dashti, H.S.; Scheer, F.A.; Jacques, P.F.; Lamon-Fava, S.; Ordovás, J.M. Short sleep duration and dietary intake: Epidemiologic evidence, mechanisms, and health implications. Adv. Nutr. 2015, 6, 648–659. [Google Scholar] [CrossRef]
- Štefan, L.; Radman, I.; Podnar, H.; Vrgoč, G. Sleep duration and sleep quality associated with dietary index in free-living very old adults. Nutrients 2018, 10, 1748. [Google Scholar] [CrossRef]
- Baglioni, C.; Spiegelhalder, K.; Lombardo, C.; Riemann, D. Sleep and emotions: A focus on insomnia. Sleep Med. Rev. 2010, 14, 227–238. [Google Scholar] [CrossRef]
- Amutio, A.; Franco, C.; Sánchez-Sánchez, L.C.; Pérez-Fuentes, M.C.; Gázquez-Linares, J.J.; van Gordon, W.; Molero-Jurado, M.M. Effects of mindfulness training on sleep problems in patients with fibromyalgia. Front. Psychol. 2018, 9, 1–8. [Google Scholar] [CrossRef]
- Sun, Q.; Ji, X.; Zhou, W.; Liu, J.D. Sleep problems in shift nurses: A brief review and recommendations at both individual and institutional levels. J. Nurs. Manag. 2018, 27, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine (IOM). Crossing the Quality Chasm: A New Health System for the 21st Century; National Academy Press: Washington, DC, USA, 2001. [Google Scholar]
- Rathert, C.; Wyrwich, M.D.; Boren, S.A. Patient-centered care and outcomes: A systematic review of the literature. Med Care Res. Rev. 2013, 70, 351–379. [Google Scholar] [CrossRef] [PubMed]
- Sommaruga, M.; Casu, G.; Giaquinto, F.; Gremigni, P. Self-perceived provision of patient centered care by healthcare professionals: The role of emotional intelligence and general self-efficacy. Patient Educ. Couns. 2017, 100, 974–980. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Fuentes, M.M.; Molero, M.M.; Gázquez, J.J.; Oropesa Ruiz, N.F. The role of emotional intelligence in engagement in nurses. Int. J. Environ. Res Public Health 2018, 15, 1915. [Google Scholar] [CrossRef]
- Pérez-Fuentes, M.M.; Molero, M.M.; Gázquez, J.J.; Simón, M.M. Analysis of burnout predictors in nursing: Risk and protective psychological factors. Eur. J. Psychol. Appl. Leg. Context 2019, 11, 33–40. [Google Scholar] [CrossRef]
- Martos, Á.; Pérez-Fuentes, M.C.; Molero, M.M.; Gázquez, J.J.; Simón, M.M.; Barragán, A.B. Burnout y engagement en estudiantes de Ciencias de la Salud. Eur. J. Investig. Health Psycho. Educ. 2018, 8, 23–36. [Google Scholar] [CrossRef]
- Bar-On, R. The Emotional Quotient Inventory (EQ-i): A Test of Emotional Intelligence; Multi-Health Systems: Toronto, ON, Canada, 1997. [Google Scholar]
- Cabanach, R.G.; Souto-Gestal, A.; Cervantes, R.F. Perfiles de regulación emocional y estrés académico en estudiantes de fisioterapia. Eur. J. Educ. Psychol. 2017, 10, 57–67. [Google Scholar] [CrossRef]
- Ridoutt, B.; Baird, D.; Bastiaans, K.; Hendrie, G.; Riley, M.; Sanguansri, P.; Syrette, J.; Noakes, M. Changes in food intake in Australia: Comparing the 1995 and 2011 National Nutrition Survey Results disaggregated into basic foods. Foods 2016, 5, 40. [Google Scholar] [CrossRef]
- Song, F.; Cho, M. Geography of food consumption patterns between south and North China. Foods 2017, 6, 34. [Google Scholar] [CrossRef]
- Gianini, L.M.; White, M.A.; Masheb, R.M. Eating pathology, emotion regulation, and emotional overeating in obese adults with binge eating disorder. Eat. Behav. 2013, 14, 309–313. [Google Scholar] [CrossRef]
- Andrei, F.; Nuccitelli, C.; Mancini, G.; Reggiani, G.M.; Trombini, E. Emotional intelligence, emotion regulation and affectivity in adults seeking treatment for obesity. Psychiatry Res. 2018, 269, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Otsuka, Y.; Kaneita, Y.; Itani, O.; Nakagome, S.; Jike, M.; Ohida, T. Relationship between stress coping and sleep disorders among the general Japanese population: A nationwide representative survey. Sleep Med. 2017, 37, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Bao, X.; Xue, S.; Kong, F. Dispositional mindfulness and perceived stress: The role of emotional intelligence. Pers. Individ. Dif. 2015, 78, 48–52. [Google Scholar] [CrossRef]
- Zhao, J.; Li, X.; Xiao, H.; Cui, N.; Sun, L.; Xu, Y. Mindfulness and burnout among bedside registered nurses: A cross-sectional study. Nurs. Health Sci. 2018, 21, 126–131. [Google Scholar] [CrossRef] [PubMed]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatr. Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Macías, J.A.; Royuela, A. La versión española del índice de calidad de sueño de Pittsburgh. Inf. Psiquiátricas 1996, 146, 465–472. [Google Scholar]
- Royuela, A.; Macías, J.A. Propiedades clinimétricas de la version castellana del Cuestionario de Pittsburgh. Vigilia-Sueño 1997, 9, 81–94. [Google Scholar]
- Stunkard, A.J.; Messick, S. The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J. Psychosom. Res. 1985, 29, 71–83. [Google Scholar] [CrossRef]
- Jáuregui-Lobera, I.; García-Cruz, P.; Carbonero-Carreño, R.; Magallares, A.; Ruiz-Prieto, I. Psychometric properties of Spanish version of the Three-Factor Eating Questionnaire-R18 (TFEQ-SP) and its relationship with some eating and body image-related variables. Nutrients 2014, 6, 5619–5635. [Google Scholar] [CrossRef]
- Pérez-Fuentes, M.C.; Molero, M.M.; Gázquez, J.J.; Oropesa, N.F. Psychometric properties of the Three Factor Eating Questionnaire in healthcare personnel. Nutr. Hosp. 2019, 36, 434–440. [Google Scholar] [CrossRef]
- Pérez-Fuentes, M.C.; Gázquez, J.J.; Mercader, I.; Molero, M.M. Brief Emotional Intelligence Inventory for Senior Citizens (EQ-i-M20). Psicothema 2014, 26, 524–530. [Google Scholar] [CrossRef]
- Bar-On, R.; Parker, J.D.A. Emotional Quotient Inventory: Youth Version (EQ-i:YV): Technical Manual; Multi-Health Systems: Toronto, ON, Canada, 2000. [Google Scholar]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; The Guilford Press: New York, NY, USA, 2013. [Google Scholar]
- Baron, R.M.; Kenny, D.A. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J. Personal. Soc. Psychol. 1986, 51, 1173–1182. [Google Scholar] [CrossRef]
- Hill, C.L.M.; Updegraff, J.A. Mindfulness and its relationship to emotional regulation. Emotion 2012, 12, 81–90. [Google Scholar] [CrossRef]
- Chaput, J.P.; Després, J.P.; Bouchard, C.; Tremblay, A. The Association between Short Sleep Duration and Weight Gain is Dependent on Disinhibited Eating Behavior in Adults. Sleep 2011, 34, 1291–1297. [Google Scholar] [CrossRef]

| Total Sample (n = 1073) | PSQI > 5 (n = 644) Poor Sleepers | PSQI ≤ 5 (n = 429) Good Sleepers | |
|---|---|---|---|
| Sex | |||
| Man | 14.7% (n = 158) | 13.7% (n = 88) | 16.3% (n = 70) |
| Woman | 85.3% (n = 915) | 86.3% (n = 556) | 83.7% (n = 359) |
| Civil status | |||
| Single | 50.6% (n = 543) | 48% (n = 309) | 54.4% (n = 234) |
| Married or stable partner | 47% (n = 504) | 49.2% (n = 317) | 43.6% (n = 187) |
| Separated or divorced | 2.2% (n = 24) | 2.8% (n = 18) | 1.4% (n = 6) |
| Widower | 0.2% (n = 2) | - | 0.5% (n = 2) |
| Age | 32.32 (SD = 6.62) | 32.69 (SD = 6.73) | 31.76 (SD = 6.42) |
| TFEQ-R18 | |||
| Uncontrolled eating | 17.38 (SD = 5.88) | 18.08 (SD = 6.11) | 16.32 (SD = 5.36) |
| Emotional eating | 5.75 (SD = 2.50) | 6.01 (SD = 2.60) | 5.37 (SD = 2.28) |
| Cognitive restriction | 16.08 (SD = 4.55) | 16.28 (SD = 4.55) | 15.77 (SD = 4.53) |
| PSQI Global | 6.44 (SD = 2.90) | 8.27 (SD = 2.16) | 3.70 (SD = 1.25) |
| Perception of health * | 3.40 (SD = 0.59) | 3.32 (SD = 0.59) | 3.52 (SD = 0.57) |
| M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. PSQI Global | 6.44 | 2.90 | - | |||||||
| 2. Uncontrolled eating | 17.38 | 5.88 | 0.17 *** | - | ||||||
| 3. Emotional eating | 5.75 | 2.50 | 0.19 *** | 0.74 *** | - | |||||
| 4. Cognitive restriction | 16.08 | 4.55 | 0.05 | 0.23 *** | 0.25 *** | - | ||||
| 5. Intrapersonal | 9.83 | 2.87 | −0.05 | −0.01 | −0.02 | 0.02 | - | |||
| 6. Interpersonal | 11.65 | 2.04 | −0.00 | 0.02 | −0.00 | 0.04 | 0.37 *** | - | ||
| 7. Stress management | 12.48 | 2.23 | −0.15 *** | −0.21 *** | −0.20 *** | −0.05 | −0.00 | 0.06 * | - | |
| 8. Adaptability | 11.09 | 2.13 | −0.06 * | −0.02 | −0.06 | 0.11 *** | 0.40 *** | 0.57 *** | 0.04 | - |
| 9. Mood | 11.74 | 2.33 | −0.20 *** | −0.18 *** | −0.22 *** | −0.04 | 0.36 *** | 0.35 *** | 0.19 *** | 0.54 *** |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gázquez Linares, J.J.; Pérez-Fuentes, M.d.C.; Molero Jurado, M.d.M.; Oropesa Ruiz, N.F.; Simón Márquez, M.d.M.; Saracostti, M. Sleep Quality and the Mediating Role of Stress Management on Eating by Nursing Personnel. Nutrients 2019, 11, 1731. https://doi.org/10.3390/nu11081731
Gázquez Linares JJ, Pérez-Fuentes MdC, Molero Jurado MdM, Oropesa Ruiz NF, Simón Márquez MdM, Saracostti M. Sleep Quality and the Mediating Role of Stress Management on Eating by Nursing Personnel. Nutrients. 2019; 11(8):1731. https://doi.org/10.3390/nu11081731
Chicago/Turabian StyleGázquez Linares, José Jesús, María del Carmen Pérez-Fuentes, María del Mar Molero Jurado, Nieves Fátima Oropesa Ruiz, María del Mar Simón Márquez, and Mahia Saracostti. 2019. "Sleep Quality and the Mediating Role of Stress Management on Eating by Nursing Personnel" Nutrients 11, no. 8: 1731. https://doi.org/10.3390/nu11081731
APA StyleGázquez Linares, J. J., Pérez-Fuentes, M. d. C., Molero Jurado, M. d. M., Oropesa Ruiz, N. F., Simón Márquez, M. d. M., & Saracostti, M. (2019). Sleep Quality and the Mediating Role of Stress Management on Eating by Nursing Personnel. Nutrients, 11(8), 1731. https://doi.org/10.3390/nu11081731









