Eating Disorders and Gastrointestinal Diseases
Abstract
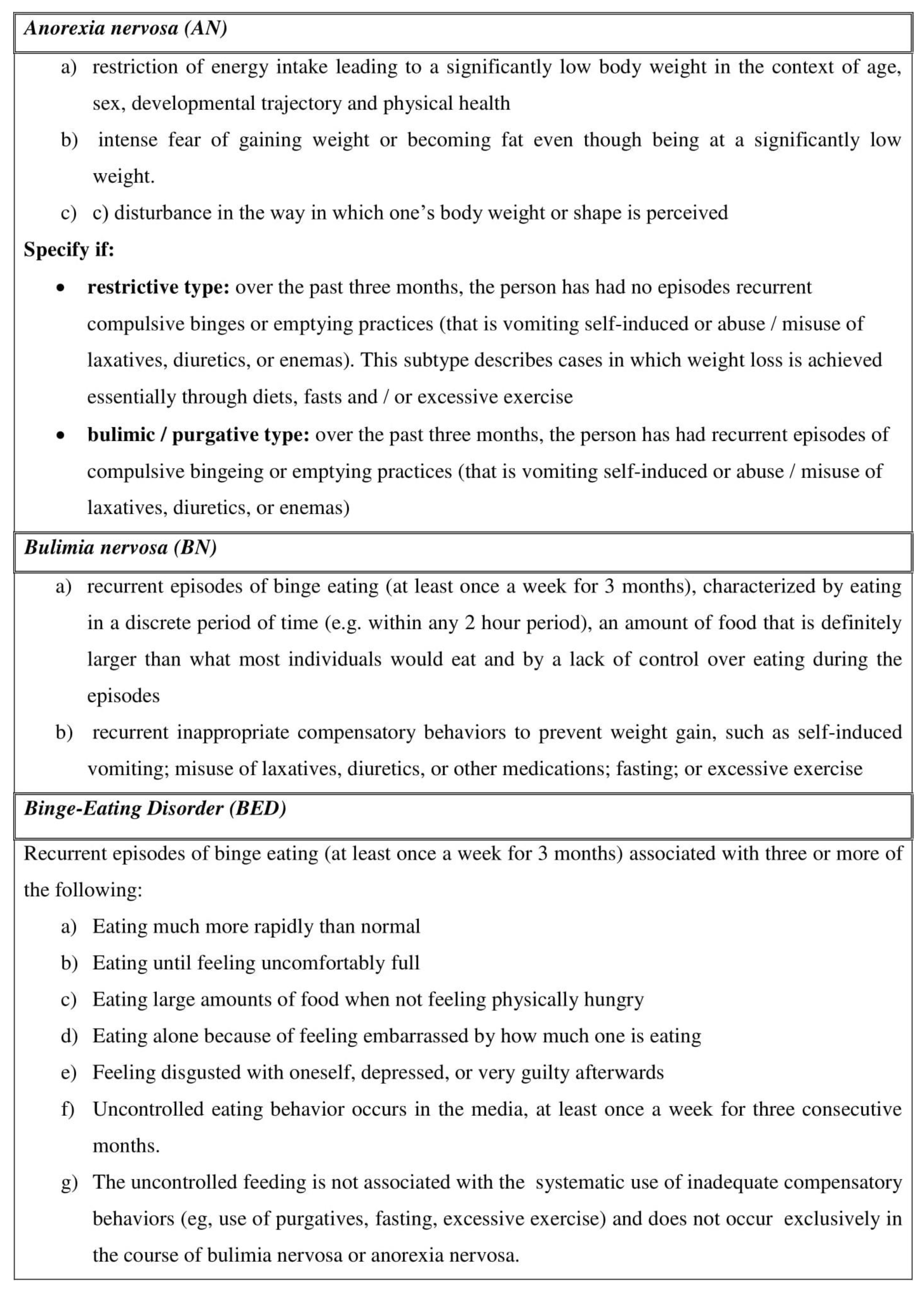
1. Eating Disorders
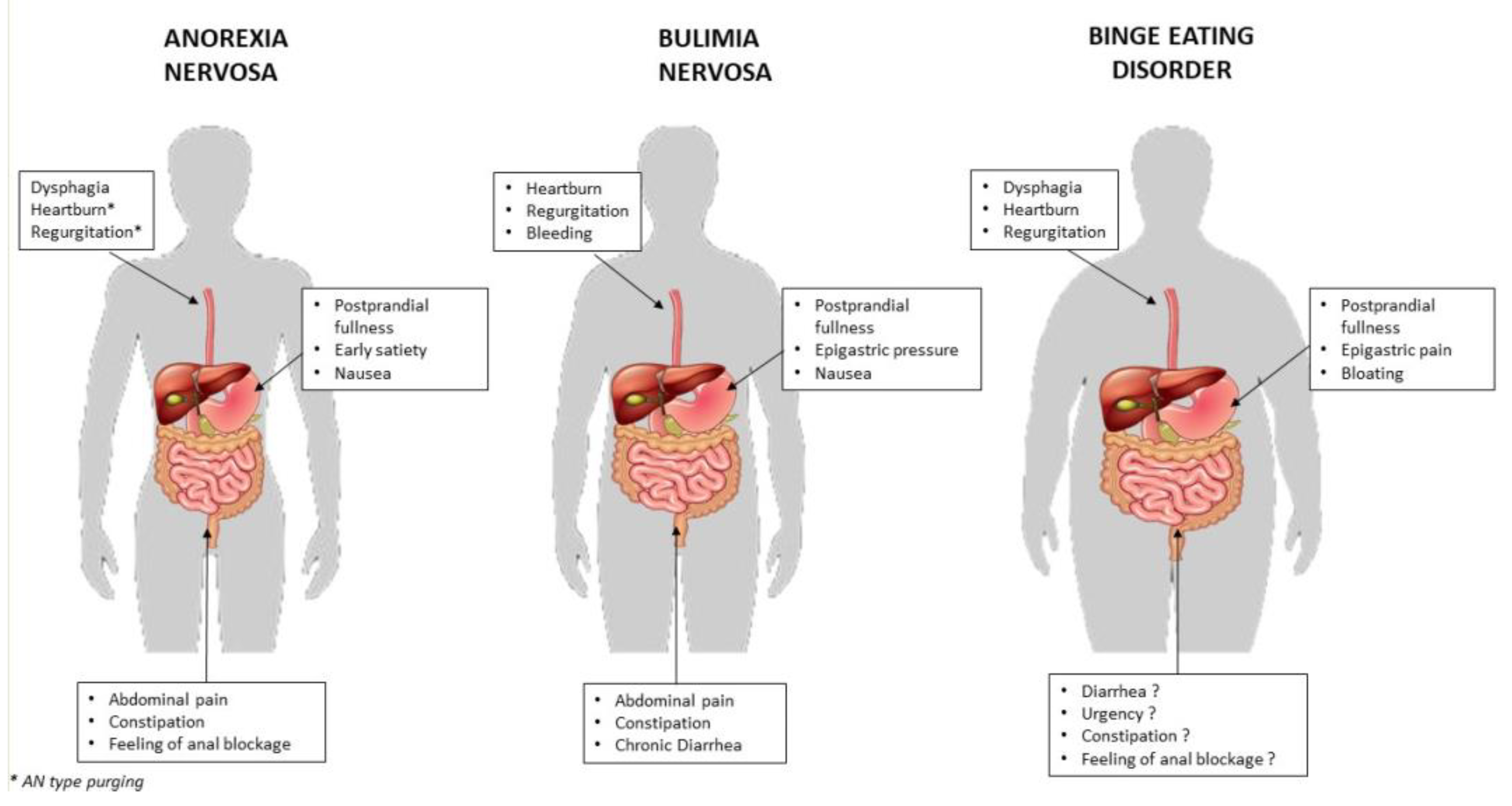
2. ED and GI Tract
3. Esophagus
3.1. Anorexia Nervosa
3.2. Bulimia Nervosa
3.3. Binge Eating Disorder
4. Stomach
4.1. Anorexia Nervosa
4.2. Bulimia Nervosa
4.3. Binge Eating Disorders
5. Intestine
5.1. Anorexia Nervosa
5.2. Bulimia Nervosa
5.3. Binge Eating Disorders
6. Gut Microbiota
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Lewinsohn, P.M.; Hops, H.; Roberts, R.E.; Seeley, J.R.; Andrews, J.A. Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III-R disorders in high school students. J. Abnorm. Psychol. 1993, 102, 133–144. [Google Scholar] [CrossRef] [PubMed]
- Association, A.P. Diagnostic and statistical manual of mental disorders. In DSM—5; American Psychological Association: Washington, DC, USA, 2015. [Google Scholar]
- Hetterich, L.; Mack, I.; Giel, K.E.; Zipfel, S.; Stengel, A. An update on gastrointestinal disturbances in eating disorders. Mol. Cell. Endocrinol. 2018, 497, 110318. [Google Scholar] [CrossRef] [PubMed]
- Udo, T.; Grilo, C.M. Prevalence and Correlates of DSM-5-Defined Eating Disorders in a Nationally Representative Sample of U.S. Adults. Biol. Psychiatry 2018, 84, 345–354. [Google Scholar] [CrossRef] [PubMed]
- Smink, F.R.; van Hoeken, D.; Hoek, H.W. Epidemiology of eating disorders: Incidence, prevalence and mortality rates. Curr. Psychiatry Rep. 2012, 14, 406–414. [Google Scholar] [CrossRef] [PubMed]
- Favaro, A.; Caregaro, L.; Tenconi, E.; Bosello, R.; Santonastaso, P. Time trends in age at onset of anorexia nervosa and bulimia nervosa. J. Clin. Psychiatry 2009, 70, 1715–1721. [Google Scholar] [CrossRef]
- Keski-Rahkonen, A.; Hoek, H.W.; Linna, M.S.; Raevuori, A.; Sihvola, E.; Bulik, C.M.; Rissanen, A.; Kaprio, J. Incidence and outcomes of bulimia nervosa: A nationwide population-based study. Psychol. Med. 2009, 39, 823–831. [Google Scholar] [CrossRef]
- Cossrow, N.; Pawaskar, M.; Witt, E.A.; Ming, E.E.; Victor, T.W.; Herman, B.K.; Wadden, T.A.; Erder, M.H. Estimating the Prevalence of Binge Eating Disorder in a Community Sample From the United States: Comparing DSM-IV-TR and DSM-5 Criteria. J. Clin. Psychiatry 2016, 77, e968–e974. [Google Scholar] [CrossRef]
- Olguin, P.; Fuentes, M.; Gabler, G.; Guerdjikova, A.I.; Keck, P.E., Jr.; McElroy, S.L. Medical comorbidity of binge eating disorder. Eat. Weight Disord. EWD 2017, 22, 13–26. [Google Scholar] [CrossRef]
- Stunkard, A.J. Eating disorders and obesity. Psychiatr. Clin. N. Am. 2011, 34, 765–771. [Google Scholar] [CrossRef]
- Association, A.P. Diagnostic and Statistical Manual of Mental Disorders, 4th ed.; American Psychiatric Association: Washington, DC, USA, 2000. [Google Scholar]
- Silverman, J.A. Louis-Victor Marce, 1828–1864: Anorexia nervosa’s forgotten man. Psychol. Med. 1989, 19, 833–835. [Google Scholar] [CrossRef]
- Perkins, S.J.; Keville, S.; Schmidt, U.; Chalder, T. Eating disorders and irritable bowel syndrome: Is there a link? J. Psychosom. Res. 2005, 59, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Boyd, C.; Abraham, S.; Kellow, J. Psychological features are important predictors of functional gastrointestinal disorders in patients with eating disorders. Scand. J. Gastroenterol. 2005, 40, 929–935. [Google Scholar] [CrossRef] [PubMed]
- Salvioli, B.; Pellicciari, A.; Iero, L.; Di Pietro, E.; Moscano, F.; Gualandi, S.; Stanghellini, V.; De Giorgio, R.; Ruggeri, E.; Franzoni, E. Audit of digestive complaints and psychopathological traits in patients with eating disorders: A prospective study. Dig. Liver Dis. 2013, 45, 639–644. [Google Scholar] [CrossRef] [PubMed]
- Guerdjikova, A.I.; Mori, N.; Casuto, L.S.; McElroy, S.L. Binge Eating Disorder. Psychiatr. Clin. N. Am. 2017, 40, 255–266. [Google Scholar] [CrossRef] [PubMed]
- Ulfvebrand, S.; Birgegard, A.; Norring, C.; Hogdahl, L.; von Hausswolff-Juhlin, Y. Psychiatric comorbidity in women and men with eating disorders results from a large clinical database. Psychiatry Res. 2015, 230, 294–299. [Google Scholar] [CrossRef] [PubMed]
- Bohn, K.; Doll, H.A.; Cooper, Z.; O’Connor, M.; Palmer, R.L.; Fairburn, C.G. The measurement of impairment due to eating disorder psychopathology. Behav. Res. Ther. 2008, 46, 1105–1110. [Google Scholar] [CrossRef]
- Abraham, S.; Kellow, J.E. Do the digestive tract symptoms in eating disorder patients represent functional gastrointestinal disorders? BMC Gastroenterol. 2013, 13, 38. [Google Scholar] [CrossRef]
- Zipfel, S.; Sammet, I.; Rapps, N.; Herzog, W.; Herpertz, S.; Martens, U. Gastrointestinal disturbances in eating disorders: Clinical and neurobiological aspects. Auton. Neurosci. Basic Clin. 2006, 129, 99–106. [Google Scholar] [CrossRef]
- Norris, M.L.; Harrison, M.E.; Isserlin, L.; Robinson, A.; Feder, S.; Sampson, M. Gastrointestinal complications associated with anorexia nervosa: A systematic review. Int. J. Eat. Disord. 2016, 49, 216–237. [Google Scholar] [CrossRef]
- McCallum, R.W.; Grill, B.B.; Lange, R.; Planky, M.; Glass, E.E.; Greenfeld, D.G. Definition of a gastric emptying abnormality in patients with anorexia nervosa. Dig. Dis. Sci. 1985, 30, 713–722. [Google Scholar] [CrossRef]
- Kamal, N.; Chami, T.; Andersen, A.; Rosell, F.A.; Schuster, M.M.; Whitehead, W.E. Delayed gastrointestinal transit times in anorexia nervosa and bulimia nervosa. Gastroenterology 1991, 101, 1320–1324. [Google Scholar] [CrossRef]
- Hutson, W.R.; Wald, A. Gastric emptying in patients with bulimia nervosa and anorexia nervosa. Am. J. Gastroenterol. 1990, 85, 41–46. [Google Scholar] [PubMed]
- Rigaud, D.; Bedig, G.; Merrouche, M.; Vulpillat, M.; Bonfils, S.; Apfelbaum, M. Delayed gastric emptying in anorexia nervosa is improved by completion of a renutrition program. Dig. Dis. Sci. 1988, 33, 919–925. [Google Scholar] [CrossRef] [PubMed]
- Hill, L.D.; Kozarek, R.A.; Kraemer, S.J.; Aye, R.W.; Mercer, C.D.; Low, D.E.; Pope, C.E., 2nd. The gastroesophageal flap valve: In vitro and in vivo observations. Gastrointest. Endosc. 1996, 44, 541–547. [Google Scholar] [CrossRef]
- Abell, T.L.; Malagelada, J.R.; Lucas, A.R.; Brown, M.L.; Camilleri, M.; Go, V.L.; Azpiroz, F.; Callaway, C.W.; Kao, P.C.; Zinsmeister, A.R.; et al. Gastric electromechanical and neurohormonal function in anorexia nervosa. Gastroenterology 1987, 93, 958–965. [Google Scholar] [CrossRef]
- Passananti, V.; Siniscalchi, M.; Zingone, F.; Bucci, C.; Tortora, R.; Iovino, P.; Ciacci, C. Prevalence of eating disorders in adults with celiac disease. Gastroenterol. Res. Pract. 2013, 2013, 491657. [Google Scholar] [CrossRef]
- Vella, A.; Camilleri, M. The Gastrointestinal Tract as an Integrator of Mechanical and Hormonal Response to Nutrient Ingestion. Diabetes 2017, 66, 2729–2737. [Google Scholar] [CrossRef]
- Latorre, R.; Sternini, C.; De Giorgio, R.; Greenwood-Van Meerveld, B. Enteroendocrine cells: A review of their role in brain-gut communication. Neurogastroenterol. Motil. 2016, 28, 620–630. [Google Scholar] [CrossRef]
- Depoortere, I. Taste receptors of the gut: Emerging roles in health and disease. Gut 2014, 63, 179–190. [Google Scholar] [CrossRef]
- Furness, J.B.; Rivera, L.R.; Cho, H.J.; Bravo, D.M.; Callaghan, B. The gut as a sensory organ. Nat. Rev. Gastroenterol. Hepatol. 2013, 10, 729–740. [Google Scholar] [CrossRef]
- Iovino, P.; Azpiroz, F.; Domingo, E.; Malagelada, J.R. The sympathetic nervous system modulates perception and reflex responses to gut distention in humans. Gastroenterology 1995, 108, 680–686. [Google Scholar] [CrossRef]
- Brookes, S.J.; Spencer, N.J.; Costa, M.; Zagorodnyuk, V.P. Extrinsic primary afferent signalling in the gut. Nat. Rev. Gastroenterol. Hepatol. 2013, 10, 286–296. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.J.; Tomasi, D.; Backus, W.; Wang, R.; Telang, F.; Geliebter, A.; Korner, J.; Bauman, A.; Fowler, J.S.; Thanos, P.K.; et al. Gastric distention activates satiety circuitry in the human brain. NeuroImage 2008, 39, 1824–1831. [Google Scholar] [CrossRef] [PubMed]
- Jones, K.L.; Doran, S.M.; Hveem, K.; Bartholomeusz, F.D.; Morley, J.E.; Sun, W.M.; Chatterton, B.E.; Horowitz, M. Relation between postprandial satiation and antral area in normal subjects. Am. J. Clin. Nutr. 1997, 66, 127–132. [Google Scholar] [CrossRef] [PubMed]
- Camilleri, M. Integrated upper gastrointestinal response to food intake. Gastroenterology 2006, 131, 640–658. [Google Scholar] [CrossRef]
- Enck, P.; Azpiroz, F.; Boeckxstaens, G.; Elsenbruch, S.; Feinle-Bisset, C.; Holtmann, G.; Lackner, J.M.; Ronkainen, J.; Schemann, M.; Stengel, A.; et al. Functional dyspepsia. Nat. Rev. Dis. Primers 2017, 3, 17081. [Google Scholar] [CrossRef]
- Iovino, P.; Angrisani, L.; Galloro, G.; Consalvo, D.; Tremolaterra, F.; Pascariello, A.; Ciacci, C. Proximal stomach function in obesity with normal or abnormal oesophageal acid exposure. Neurogastroenterol. Motil. 2006, 18, 425–432. [Google Scholar] [CrossRef]
- Citrome, L. Binge-Eating Disorder and Comorbid Conditions: Differential Diagnosis and Implications for Treatment. J. Clin. Psychiatry 2017, 78 (Suppl. S1), 9–13. [Google Scholar] [CrossRef]
- Guarda, A.S.; Schreyer, C.C.; Boersma, G.J.; Tamashiro, K.L.; Moran, T.H. Anorexia nervosa as a motivated behavior: Relevance of anxiety, stress, fear and learning. Physiol. Behav. 2015, 152, 466–472. [Google Scholar] [CrossRef]
- Drossman, D.A. Functional Gastrointestinal Disorders: History, Pathophysiology, Clinical Features and Rome IV. Gastroenterology 2016. [Google Scholar] [CrossRef]
- Wang, X.; Luscombe, G.M.; Boyd, C.; Kellow, J.; Abraham, S. Functional gastrointestinal disorders in eating disorder patients: Altered distribution and predictors using ROME III compared to ROME II criteria. World J. Gastroenterol. 2014, 20, 16293–16299. [Google Scholar] [CrossRef] [PubMed]
- Stacher, G.; Kiss, A.; Wiesnagrotzki, S.; Bergmann, H.; Hobart, J.; Schneider, C. Oesophageal and gastric motility disorders in patients categorised as having primary anorexia nervosa. Gut 1986, 27, 1120–1126. [Google Scholar] [CrossRef] [PubMed]
- Benini, L.; Todesco, T.; Frulloni, L.; Dalle Grave, R.; Campagnola, P.; Agugiaro, F.; Cusumano, C.D.; Gabbrielli, A.; Vantini, I. Esophageal motility and symptoms in restricting and binge-eating/purging anorexia. Dig. Liver Dis. 2010, 42, 767–772. [Google Scholar] [CrossRef] [PubMed]
- Castell DO, R.J.; Dalton, C.B. Esophageal Motility Testing; Elsevier Science Publishing Co.: New York, NY, USA, 1987. [Google Scholar]
- Conklin, J.L. Evaluation of Esophageal Motor Function With High-resolution Manometry. J. Neurogastroenterol. Motil. 2013, 19, 281–294. [Google Scholar] [CrossRef] [PubMed]
- Pacciardi, B.; Cargioli, C.; Mauri, M. Barrett’s esophagus in anorexia nervosa: A case report. Int. J. Eat. Disord. 2015, 48, 147–150. [Google Scholar] [CrossRef]
- Catala-Lopez, F.; Fores-Martos, J.; Driver, J.A.; Page, M.J.; Hutton, B.; Ridao, M.; Alonso-Arroyo, A.; Macias Saint-Gerons, D.; Genova-Maleras, R.; Valderas, J.M.; et al. Association of Anorexia Nervosa with Risk of Cancer: A Systematic Review and Meta-analysis. JAMA Netw. Open 2019, 2, e195313. [Google Scholar] [CrossRef]
- Denholm, M.; Jankowski, J. Gastroesophageal reflux disease and bulimia nervosa—A review of the literature. Dis. Esophagus 2011, 24, 79–85. [Google Scholar] [CrossRef]
- Kiss, A.; Wiesnagrotzki, S.; Abatzi, T.A.; Meryn, S.; Haubenstock, A.; Base, W. Upper gastrointestinal endoscopy findings in patients with long-standing bulimia nervosa. Gastrointest. Endosc. 1989, 35, 516–518. [Google Scholar] [CrossRef]
- Resano, C.H.; Cabrera, N.; Gonzalez Cueto, D.; Sanchez Basso, A.E.; Rubio, H.H. Double early epidermoid carcinoma of the esophagus in columnar epithelium. Endoscopy 1985, 17, 73–75. [Google Scholar] [CrossRef]
- Dessureault, S.; Coppola, D.; Weitzner, M.; Powers, P.; Karl, R.C. Barrett’s esophagus and squamous cell carcinoma in a patient with psychogenic vomiting. Int. J. Gastrointest. Cancer 2002, 32, 57–61. [Google Scholar] [CrossRef]
- Brewster, D.H.; Nowell, S.L.; Clark, D.N. Risk of oesophageal cancer among patients previously hospitalised with eating disorder. Cancer Epidemiol. 2015, 39, 313–320. [Google Scholar] [CrossRef] [PubMed]
- Kiss, A.; Bergmann, H.; Abatzi, T.A.; Schneider, C.; Wiesnagrotzki, S.; Hobart, J.; Steiner-Mittelbach, G.; Gaupmann, G.; Kugi, A.; Stacher-Janotta, G.; et al. Oesophageal and gastric motor activity in patients with bulimia nervosa. Gut 1990, 31, 259–265. [Google Scholar] [CrossRef] [PubMed]
- Nickl, N.J.; Brazer, S.R.; Rockwell, K.; Smith, J.W. Patterns of esophageal motility in patients with stable bulimia. Am. J. Gastroenterol. 1996, 91, 2544–2547. [Google Scholar] [PubMed]
- Forney, K.J.; Buchman-Schmitt, J.M.; Keel, P.K.; Frank, G.K. The medical complications associated with purging. Int. J. Eat. Disord. 2016, 49, 249–259. [Google Scholar] [CrossRef]
- Cremonini, F.; Camilleri, M.; Clark, M.M.; Beebe, T.J.; Locke, G.R.; Zinsmeister, A.R.; Herrick, L.M.; Talley, N.J. Associations among binge eating behavior patterns and gastrointestinal symptoms: A population-based study. Int. J. Obes. 2009, 33, 342–353. [Google Scholar] [CrossRef]
- Wildi, S.M.; Tutuian, R.; Castell, D.O. The influence of rapid food intake on postprandial reflux: Studies in healthy volunteers. Am. J. Gastroenterol. 2004, 99, 1645–1651. [Google Scholar] [CrossRef]
- Esfandyari, T.; Potter, J.W.; Vaezi, M.F. Dysphagia: A cost analysis of the diagnostic approach. Am. J. Gastroenterol. 2002, 97, 2733–2737. [Google Scholar] [CrossRef]
- Santonicola, A.; Angrisani, L.; Ciacci, C.; Iovino, P. Prevalence of functional gastrointestinal disorders according to Rome III criteria in Italian morbidly obese patients. Sci. World J. 2013, 2013, 532503. [Google Scholar] [CrossRef]
- Chang, P.; Friedenberg, F. Obesity and GERD. Gastroenterol. Clin. North Am. 2014, 43, 161–173. [Google Scholar] [CrossRef]
- Stacher, G. Gut function in anorexia nervosa and bulimia nervosa. Scand. J. Gastroenterol. 2003, 38, 573–587. [Google Scholar] [CrossRef]
- Bluemel, S.; Menne, D.; Milos, G.; Goetze, O.; Fried, M.; Schwizer, W.; Fox, M.; Steingoetter, A. Relationship of body weight with gastrointestinal motor and sensory function: Studies in anorexia nervosa and obesity. BMC Gastroenterol. 2017, 17, 4. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Lee, A.M.; Ngai, E.; Lee, D.T.; Wing, Y.K. Rationales for Food Refusal in Chinese Patients with Anorexia Nervosa. Int. J. Eat. Disord. 2001, 29, 224–229. [Google Scholar] [CrossRef]
- Santonicola, A.; Siniscalchi, M.; Capone, P.; Gallotta, S.; Ciacci, C.; Iovino, P. Prevalence of functional dyspepsia and its subgroups in patients with eating disorders. World J. Gastroenterol. 2012, 18, 4379–4385. [Google Scholar] [CrossRef] [PubMed]
- Holt, S.; Ford, M.J.; Grant, S.; Heading, R.C. Abnormal gastric emptying in primary anorexia nervosa. Br. J. Psychiatry 1981, 139, 550–552. [Google Scholar] [CrossRef] [PubMed]
- Robinson, P.H.; Clarke, M.; Barrett, J. Determinants of delayed gastric emptying in anorexia nervosa and bulimia nervosa. Gut 1988, 29, 458–464. [Google Scholar] [CrossRef]
- Benini, L.; Todesco, T.; Dalle Grave, R.; Deiorio, F.; Salandini, L.; Vantini, I. Gastric emptying in patients with restricting and binge/purging subtypes of anorexia nervosa. Am. J. Gastroenterol. 2004, 99, 1448–1454. [Google Scholar] [CrossRef]
- Robinson, P.H. Perceptivity and paraceptivity during measurement of gastric emptying in anorexia and bulimia nervosa. Br. J. Psychiatry 1989, 154, 400–405. [Google Scholar] [CrossRef]
- Waldholtz, B.D.; Andersen, A.E. Gastrointestinal symptoms in anorexia nervosa. A prospective study. Gastroenterology 1990, 98, 1415–1419. [Google Scholar] [CrossRef]
- Szmukler, G.I.; Young, G.P.; Lichtenstein, M.; Andrews, J.T. A serial study of gastric emptying in anorexia nervosa and bulimia. Aust. N. Z. J. Med. 1990, 20, 220–225. [Google Scholar] [CrossRef]
- Geracioti, T.D., Jr.; Liddle, R.A. Impaired cholecystokinin secretion in bulimia nervosa. New Engl. J. Med. 1988, 319, 683–688. [Google Scholar] [CrossRef]
- Devlin, M.J.; Walsh, B.T.; Guss, J.L.; Kissileff, H.R.; Liddle, R.A.; Petkova, E. Postprandial cholecystokinin release and gastric emptying in patients with bulimia nervosa. Am. J. Clin. Nutr. 1997, 65, 114–120. [Google Scholar] [CrossRef] [PubMed]
- Zimmerli, E.J.; Walsh, B.T.; Guss, J.L.; Devlin, M.J.; Kissileff, H.R. Gastric compliance in bulimia nervosa. Physiol. Behav. 2006, 87, 441–446. [Google Scholar] [CrossRef] [PubMed]
- Geliebter, A.; Hashim, S.A. Gastric capacity in normal, obese, and bulimic women. Physiol. Behav. 2001, 74, 743–746. [Google Scholar] [CrossRef]
- Geliebter, A. Gastric distension, gastric capacity, gastric balloons, and food intake. Physiol. Behav. 2019, 208, 112560. [Google Scholar] [CrossRef] [PubMed]
- Tong, J.; D’Alessio, D. Eating disorders and gastrointestinal peptides. Curr. Opin. Endocrinol. Diabetes Obes. 2011, 18, 42–49. [Google Scholar] [CrossRef] [PubMed]
- Gebhart, T. Superior mesenteric artery syndrome. Gastroenterol. Nurs. Off. J. Soc. Gastroenterol. Nurses Assoc. 2015, 38, 189–193. [Google Scholar] [CrossRef] [PubMed]
- Ikegaya, H.; Nakajima, M.; Shintani-Ishida, K.; Uemura, K.; Yoshida, K. Death due to duodenal obstruction in a patient with an eating disorder: A case report. Int. J. Eat. Disord. 2006, 39, 350–352. [Google Scholar] [CrossRef]
- Crowell, M.D.; Cheskin, L.J.; Musial, F. Prevalence of gastrointestinal symptoms in obese and normal weight binge eaters. Am. J. Gastroenterol. 1994, 89, 387–391. [Google Scholar]
- Geliebter, A.; Yahav, E.K.; Gluck, M.E.; Hashim, S.A. Gastric capacity, test meal intake, and appetitive hormones in binge eating disorder. Physiol. Behav. 2004, 81, 735–740. [Google Scholar] [CrossRef]
- Sysko, R.; Devlin, M.J.; Walsh, B.T.; Zimmerli, E.; Kissileff, H.R. Satiety and test meal intake among women with binge eating disorder. Int. J. Eat. Disord. 2007, 40, 554–561. [Google Scholar] [CrossRef]
- Delgado-Aros, S.; Camilleri, M.; Castillo, E.J.; Cremonini, F.; Stephens, D.; Ferber, I.; Baxter, K.; Burton, D.; Zinsmeister, A.R. Effect of gastric volume or emptying on meal-related symptoms after liquid nutrients in obesity: A pharmacologic study. Clin. Gastroenterol. Hepatol. 2005, 3, 997–1006. [Google Scholar] [CrossRef]
- Gyurkovics, E.; Tihanyi, B.; Szijarto, A.; Kaliszky, P.; Temesi, V.; Hedvig, S.A.; Kupcsulik, P. Fatal outcome from extreme acute gastric dilation after an eating binge. Int. J. Eat. Disord. 2006, 39, 602–605. [Google Scholar] [CrossRef] [PubMed]
- Youm, S.M.; Kim, J.Y.; Lee, J.R. Acute gastric dilatation causing fatal outcome in a young female with eating disorder: A case report. Korean J. Anesthesiol. 2015, 68, 188–192. [Google Scholar] [CrossRef] [PubMed]
- Dincel, O.; Goksu, M. Acute gastric dilatation due to binge eating may be fatal. North Clin. Istanb. 2017, 4, 199–202. [Google Scholar] [CrossRef]
- Kim, B.S.; Kwon, J.W.; Kim, M.J.; Ahn, S.E.; Park, H.C.; Lee, B.H. Abdominal compartment syndrome caused by a bulimic attack in a bulimia nervosa patient. J. Korean Surg. Soc. 2011, 81 (Suppl. S1), S1–S5. [Google Scholar] [CrossRef]
- Kim, H.H.; Park, S.J.; Park, M.I.; Moon, W. Acute gastric dilatation and acute pancreatitis in a patient with an eating disorder: Solving a chicken and egg situation. Intern. Med. 2011, 50, 571–575. [Google Scholar] [CrossRef]
- Carpinelli, L.; Bucci, C.; Santonicola, A.; Zingone, F.; Ciacci, C.; Iovino, P. Anhedonia in irritable bowel syndrome and in inflammatory bowel diseases and its relationship with abdominal pain. Neurogastroenterol. Motil. 2019, 31, e13531. [Google Scholar] [CrossRef]
- Iovino, P.; Tremolaterra, F.; Boccia, G.; Miele, E.; Ruju, F.M.; Staiano, A. Irritable bowel syndrome in childhood: Visceral hypersensitivity and psychosocial aspects. Neurogastroenterol. Motil. 2009, 21, e940–e974. [Google Scholar] [CrossRef]
- Sileri, P.; Franceschilli, L.; De Lorenzo, A.; Mezzani, B.; Todisco, P.; Giorgi, F.; Gaspari, A.L.; Jacoangeli, F. Defecatory disorders in anorexia nervosa: A clinical study. Tech. Coloproctology 2014, 18, 439–444. [Google Scholar] [CrossRef]
- Chiarioni, G.; Bassotti, G.; Monsignori, A.; Menegotti, M.; Salandini, L.; Di Matteo, G.; Vantini, I.; Whitehead, W.E. Anorectal dysfunction in constipated women with anorexia nervosa. Mayo Clin. Proc. 2000, 75, 1015–1019. [Google Scholar] [CrossRef]
- Bellini, M.; Usai-Satta, P.; Bove, A.; Bocchini, R.; Galeazzi, F.; Battaglia, E.; Alduini, P.; Buscarini, E.; Bassotti, G. Chronic constipation diagnosis and treatment evaluation: The “CHRO.CO.DI.T.E.” study. BMC Gastroenterol. 2017, 17, 11. [Google Scholar] [CrossRef] [PubMed]
- Chun, A.B.; Sokol, M.S.; Kaye, W.H.; Hutson, W.R.; Wald, A. Colonic and anorectal function in constipated patients with anorexia nervosa. Am. J. Gastroenterol. 1997, 92, 1879–1883. [Google Scholar] [PubMed]
- Sato, Y.; Fukudo, S. Gastrointestinal symptoms and disorders in patients with eating disorders. Clin. J. Gastroenterol. 2015, 8, 255–263. [Google Scholar] [CrossRef]
- Cortes, E.; Singh, K.; Reid, W.M. Anorexia nervosa and pelvic floor dysfunction. Int. Urogynecol. J. Pelvic Floor Dysfunct. 2003, 14, 254–255. [Google Scholar] [CrossRef] [PubMed]
- Cuellar, R.E.; Van Thiel, D.H. Gastrointestinal consequences of the eating disorders: Anorexia nervosa and bulimia. Am. J. Gastroenterol. 1986, 81, 1113–1124. [Google Scholar] [PubMed]
- Oster, J.R.; Materson, B.J.; Rogers, A.I. Laxative abuse syndrome. Am. J. Gastroenterol. 1980, 74, 451–458. [Google Scholar]
- Malik, M.; Stratton, J.; Sweeney, W.B. Rectal prolapse associated with bulimia nervosa: Report of seven cases. Dis. Colon Rectum 1997, 40, 1382–1385. [Google Scholar] [CrossRef]
- Dejong, H.; Perkins, S.; Grover, M.; Schmidt, U. The prevalence of irritable bowel syndrome in outpatients with bulimia nervosa. Int. J. Eat. Disord. 2011, 44, 661–664. [Google Scholar] [CrossRef]
- Chami, T.N.; Andersen, A.E.; Crowell, M.D.; Schuster, M.M.; Whitehead, W.E. Gastrointestinal symptoms in bulimia nervosa: Effects of treatment. Am. J. Gastroenterol. 1995, 90, 88–92. [Google Scholar]
- Sun, C.; Hull, T.; Ozuner, G. Risk factors and clinical characteristics of rectal prolapse in young patients. J. Visc. Surg. 2014, 151, 425–429. [Google Scholar] [CrossRef]
- WB Saunders. Textbook of Medical Physiology; WB Saunders: Philadelphia, PA, USA, 1991; Volume 707, pp. 701–740. [Google Scholar]
- Guerdjikova, A.I.; O’Melia, A.; Riffe, K.; Palumbo, T.; McElroy, S.L. Bulimia nervosa presenting as rectal purging and rectal prolapse: Case report and literature review. Int. J. Eat. Disord. 2012, 45, 456–459. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, N.; Norris, M.L. Rectal prolapse associated with anorexia nervosa: A case report and review of the literature. J. Eat. Disord. 2013, 1, 39. [Google Scholar] [CrossRef] [PubMed]
- Winstead, N.S.; Willard, S.G. Gastrointestinal complaints in patients with eating disorders. J. Clin. Gastroenterol. 2006, 40, 678–682. [Google Scholar] [CrossRef] [PubMed]
- Lasater, L.M.; Mehler, P.S. Medical complications of bulimia nervosa. Eat. Behav. 2001, 2, 279–292. [Google Scholar] [CrossRef]
- Roerig, J.L.; Steffen, K.J.; Mitchell, J.E.; Zunker, C. Laxative abuse: Epidemiology, diagnosis and management. Drugs 2010, 70, 1487–1503. [Google Scholar] [CrossRef]
- Li, D.; Browne, L.W.; Ladabaum, U. Melanosis coli. Clin. Gastroenterol. Hepatol. 2009, 7, A20. [Google Scholar] [CrossRef]
- Muller-Lissner, S. What has happened to the cathartic colon? Gut 1996, 39, 486–488. [Google Scholar] [CrossRef]
- Neufeld, K.A.; Kang, N.; Bienenstock, J.; Foster, J.A. Effects of intestinal microbiota on anxiety-like behavior. Commun. Integr. Biol. 2011, 4, 492–494. [Google Scholar] [CrossRef]
- Sudo, N.; Chida, Y.; Aiba, Y.; Sonoda, J.; Oyama, N.; Yu, X.N.; Kubo, C.; Koga, Y. Postnatal microbial colonization programs the hypothalamic-pituitary-adrenal system for stress response in mice. J. Physiol. 2004, 558, 263–275. [Google Scholar] [CrossRef]
- Grenham, S.; Clarke, G.; Cryan, J.F.; Dinan, T.G. Brain-gut-microbe communication in health and disease. Front. Physiol. 2011, 2, 94. [Google Scholar] [CrossRef]
- De Palma, G.; Collins, S.M.; Bercik, P.; Verdu, E.F. The microbiota-gut-brain axis in gastrointestinal disorders: Stressed bugs, stressed brain or both? J. Physiol. 2014, 592, 2989–2997. [Google Scholar] [CrossRef] [PubMed]
- Gareau, M.G.; Wine, E.; Rodrigues, D.M.; Cho, J.H.; Whary, M.T.; Philpott, D.J.; Macqueen, G.; Sherman, P.M. Bacterial infection causes stress-induced memory dysfunction in mice. Gut 2011, 60, 307–317. [Google Scholar] [CrossRef] [PubMed]
- Borgo, F.; Riva, A.; Benetti, A.; Casiraghi, M.C.; Bertelli, S.; Garbossa, S.; Anselmetti, S.; Scarone, S.; Pontiroli, A.E.; Morace, G.; et al. Microbiota in anorexia nervosa: The triangle between bacterial species, metabolites and psychological tests. PLoS ONE 2017, 12, e0179739. [Google Scholar] [CrossRef] [PubMed]
- Mack, I.; Cuntz, U.; Gramer, C.; Niedermaier, S.; Pohl, C.; Schwiertz, A.; Zimmermann, K.; Zipfel, S.; Enck, P.; Penders, J. Weight gain in anorexia nervosa does not ameliorate the faecal microbiota, branched chain fatty acid profiles, and gastrointestinal complaints. Sci. Rep. 2016, 6, 26752. [Google Scholar] [CrossRef] [PubMed]
- Schwensen, H.F.; Kan, C.; Treasure, J.; Hoiby, N.; Sjogren, M. A systematic review of studies on the faecal microbiota in anorexia nervosa: Future research may need to include microbiota from the small intestine. Eat. Weight Disord. EWD 2018, 23, 399–418. [Google Scholar] [CrossRef]
- Morita, C.; Tsuji, H.; Hata, T.; Gondo, M.; Takakura, S.; Kawai, K.; Yoshihara, K.; Ogata, K.; Nomoto, K.; Miyazaki, K.; et al. Gut Dysbiosis in Patients with Anorexia Nervosa. PLoS ONE 2015, 10, e0145274. [Google Scholar] [CrossRef]
- Cryan, J.F.; O’Mahony, S.M. The microbiome-gut-brain axis: From bowel to behavior. Neurogastroenterol. Motil. 2011, 23, 187–192. [Google Scholar] [CrossRef]
- Seitz, J.; Trinh, S.; Herpertz-Dahlmann, B. The Microbiome and Eating Disorders. Psychiatr. Clin. N. Am. 2019, 42, 93–103. [Google Scholar] [CrossRef]
- Armougom, F.; Henry, M.; Vialettes, B.; Raccah, D.; Raoult, D. Monitoring bacterial community of human gut microbiota reveals an increase in Lactobacillus in obese patients and Methanogens in anorexic patients. PLoS ONE 2009, 4, e7125. [Google Scholar] [CrossRef]
- Million, M.; Angelakis, E.; Maraninchi, M.; Henry, M.; Giorgi, R.; Valero, R.; Vialettes, B.; Raoult, D. Correlation between body mass index and gut concentrations of Lactobacillus reuteri, Bifidobacterium animalis, Methanobrevibacter smithii and Escherichia coli. Int. J. Obes. 2013, 37, 1460–1466. [Google Scholar] [CrossRef]
- Gottlieb, K.; Wacher, V.; Sliman, J.; Pimentel, M. Review article: Inhibition of methanogenic archaea by statins as a targeted management strategy for constipation and related disorders. Aliment. Pharmacol. Ther. 2016, 43, 197–212. [Google Scholar] [CrossRef] [PubMed]
- Alcock, J.; Maley, C.C.; Aktipis, C.A. Is eating behavior manipulated by the gastrointestinal microbiota? Evolutionary pressures and potential mechanisms. Bioessays News Rev. Mol. Cell. Dev. Biol. 2014, 36, 940–949. [Google Scholar] [CrossRef] [PubMed]
- Fetissov, S.O.; Hokfelt, T. On the origin of eating disorders: Altered signaling between gut microbiota, adaptive immunity and the brain melanocortin system regulating feeding behavior. Curr. Opin. Pharmacol. 2019, 48, 82–91. [Google Scholar] [CrossRef] [PubMed]
- Breton, J.; Legrand, R.; Akkermann, K.; Jarv, A.; Harro, J.; Dechelotte, P.; Fetissov, S.O. Elevated plasma concentrations of bacterial ClpB protein in patients with eating disorders. Int. J. Eat. Disord. 2016, 49, 805–808. [Google Scholar] [CrossRef] [PubMed]
- Breton, J.; Tennoune, N.; Lucas, N.; Francois, M.; Legrand, R.; Jacquemot, J.; Goichon, A.; Guerin, C.; Peltier, J.; Pestel-Caron, M.; et al. Gut Commensal E. coli Proteins Activate Host Satiety Pathways following Nutrient-Induced Bacterial Growth. Cell Metab. 2016, 23, 324–334. [Google Scholar] [CrossRef] [PubMed]
- Grimaldi, R.; Cela, D.; Swann, J.R.; Vulevic, J.; Gibson, G.R.; Tzortzis, G.; Costabile, A. In vitro fermentation of B-GOS: Impact on faecal bacterial populations and metabolic activity in autistic and non-autistic children. FEMS Microbiol. Ecol. 2017, 93. [Google Scholar] [CrossRef]
- Liu, X.; Cao, S.; Zhang, X. Modulation of Gut Microbiota-Brain Axis by Probiotics, Prebiotics, and Diet. J. Agric. Food Chem. 2015, 63, 7885–7895. [Google Scholar] [CrossRef]
- Mallikarjuna, N.; Praveen, K.; Yellamma, K. Role of Lactobacillus plantarum MTCC1325 in membrane-bound transport ATPases system in Alzheimer’s disease-induced rat brain. Bioimpacts 2016, 6, 203–209. [Google Scholar] [CrossRef]
- Wan, M.L.Y.; Ling, K.H.; El-Nezami, H.; Wang, M.F. Influence of functional food components on gut health. Crit. Rev. Food Sci. Nutr. 2019, 59, 1927–1936. [Google Scholar] [CrossRef]
- Wang, H.; Lee, I.S.; Braun, C.; Enck, P. Effect of Probiotics on Central Nervous System Functions in Animals and Humans: A Systematic Review. J. Neurogastroenterol. Motil. 2016, 22, 589–605. [Google Scholar] [CrossRef]
- Bercik, P.; Park, A.J.; Sinclair, D.; Khoshdel, A.; Lu, J.; Huang, X.; Deng, Y.; Blennerhassett, P.A.; Fahnestock, M.; Moine, D.; et al. The anxiolytic effect of Bifidobacterium longum NCC3001 involves vagal pathways for gut-brain communication. Neurogastroenterol. Motil. 2011, 23, 1132–1139. [Google Scholar] [CrossRef] [PubMed]
- Steenbergen, L.; Sellaro, R.; van Hemert, S.; Bosch, J.A.; Colzato, L.S. A randomized controlled trial to test the effect of multispecies probiotics on cognitive reactivity to sad mood. Brain Behav. Immun. 2015, 48, 258–264. [Google Scholar] [CrossRef] [PubMed]
- Mendez-Figueroa, V.; Biscaia, J.M.; Mohedano, R.B.; Blanco-Fernandez, A.; Bailen, M.; Bressa, C.; Larrosa, M.; Gonzalez-Soltero, R. Can Gut Microbiota and Lifestyle Help Us in the Handling of Anorexia Nervosa Patients? Microorganisms 2019, 7. [Google Scholar] [CrossRef] [PubMed]
- Marchesi, J.R.; Adams, D.H.; Fava, F.; Hermes, G.D.; Hirschfield, G.M.; Hold, G.; Quraishi, M.N.; Kinross, J.; Smidt, H.; Tuohy, K.M.; et al. The gut microbiota and host health: A new clinical frontier. Gut 2016, 65, 330–339. [Google Scholar] [CrossRef]
- Saulnier, D.M.; Ringel, Y.; Heyman, M.B.; Foster, J.A.; Bercik, P.; Shulman, R.J.; Versalovic, J.; Verdu, E.F.; Dinan, T.G.; Hecht, G.; et al. The intestinal microbiome, probiotics and prebiotics in neurogastroenterology. Gut Microbes 2013, 4, 17–27. [Google Scholar] [CrossRef]
- Glenny, E.M.; Bulik-Sullivan, E.C.; Tang, Q.; Bulik, C.M.; Carroll, I.M. Eating Disorders and the Intestinal Microbiota: Mechanisms of Energy Homeostasis and Behavioral Influence. Curr. Psychiatry Rep. 2017, 19, 51. [Google Scholar] [CrossRef]
- Huang, R.; Wang, K.; Hu, J. Effect of Probiotics on Depression: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutrients 2016, 8. [Google Scholar] [CrossRef]
- Ng, Q.X.; Peters, C.; Ho, C.Y.X.; Lim, D.Y.; Yeo, W.S. A meta-analysis of the use of probiotics to alleviate depressive symptoms. J. Affect. Disord. 2018, 228, 13–19. [Google Scholar] [CrossRef]
- Kleiman, S.C.; Watson, H.J.; Bulik-Sullivan, E.C.; Huh, E.Y.; Tarantino, L.M.; Bulik, C.M.; Carroll, I.M. The Intestinal Microbiota in Acute Anorexia Nervosa and During Renourishment: Relationship to Depression, Anxiety, and Eating Disorder Psychopathology. Psychosom. Med. 2015, 77, 969–981. [Google Scholar] [CrossRef]

© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Santonicola, A.; Gagliardi, M.; Guarino, M.P.L.; Siniscalchi, M.; Ciacci, C.; Iovino, P. Eating Disorders and Gastrointestinal Diseases. Nutrients 2019, 11, 3038. https://doi.org/10.3390/nu11123038
Santonicola A, Gagliardi M, Guarino MPL, Siniscalchi M, Ciacci C, Iovino P. Eating Disorders and Gastrointestinal Diseases. Nutrients. 2019; 11(12):3038. https://doi.org/10.3390/nu11123038
Chicago/Turabian StyleSantonicola, Antonella, Mario Gagliardi, Michele Pier Luca Guarino, Monica Siniscalchi, Carolina Ciacci, and Paola Iovino. 2019. "Eating Disorders and Gastrointestinal Diseases" Nutrients 11, no. 12: 3038. https://doi.org/10.3390/nu11123038
APA StyleSantonicola, A., Gagliardi, M., Guarino, M. P. L., Siniscalchi, M., Ciacci, C., & Iovino, P. (2019). Eating Disorders and Gastrointestinal Diseases. Nutrients, 11(12), 3038. https://doi.org/10.3390/nu11123038








