Isoflavone Supplements for Menopausal Women: A Systematic Review
Abstract
1. Introduction
2. Terminology
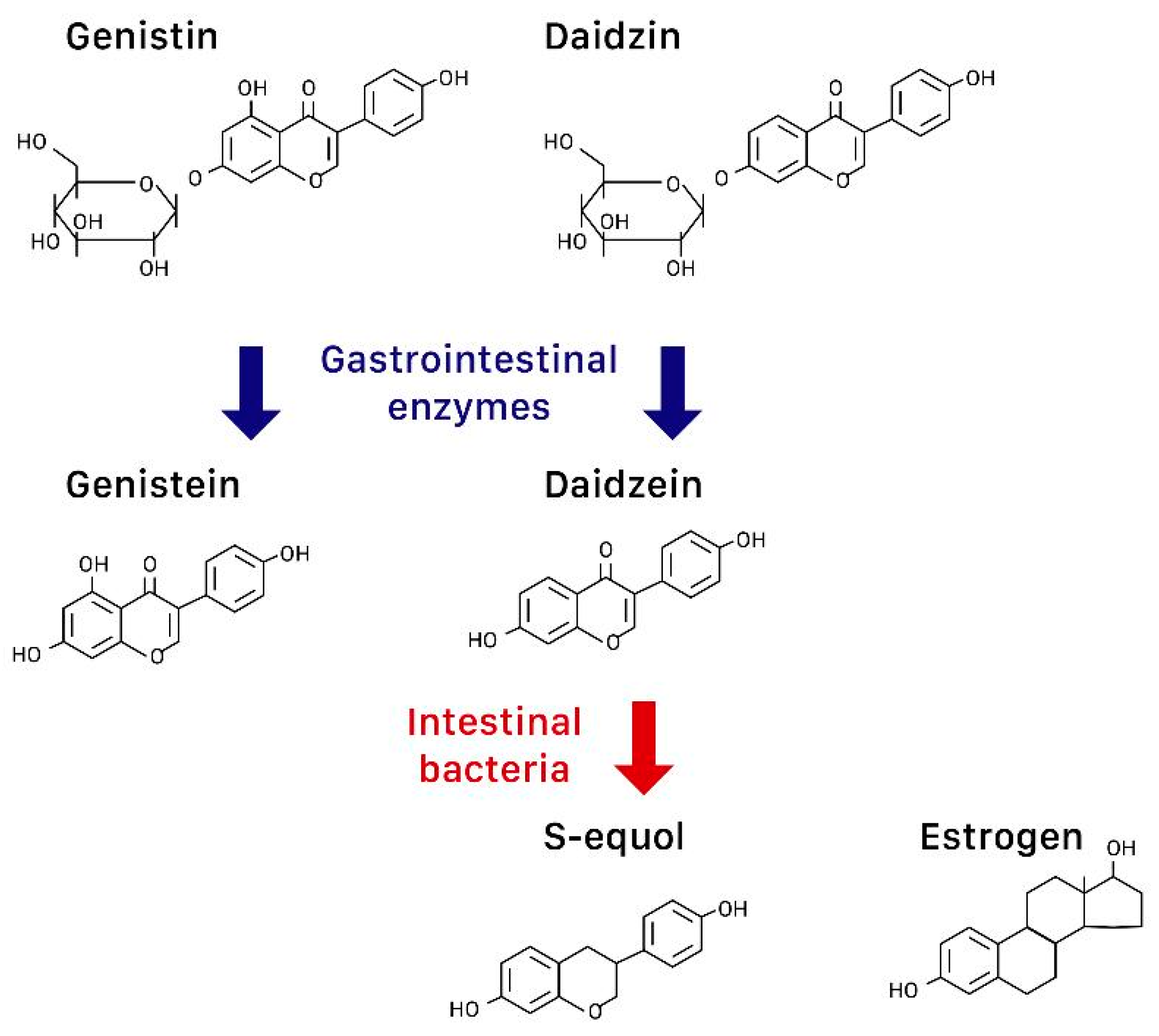
2.1. Isoflavones (Genistin, Daidzin), Genistein, Daidzein
2.2. Equol
3. Effects of Isoflavones on Menopausal Syndromes and Others
3.1. Hot Flashes
3.2. Bone Mineral Density
3.3. Cardiovascular Profile
3.4. Metabolic Syndrome
3.5. Cancer Risk
3.6. Female Urogenital Tract
3.7. Cognition
3.8. Side Effects
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Krebs, E.E.; Ensrud, K.E.; MacDonald, R.; Wilt, T.J. Phytoestrogens for treatment of menopausal symptoms: A systematic review. Obstet. Gynecol. 2004, 104, 824–836. [Google Scholar] [CrossRef] [PubMed]
- Croden, J.; Ross, S.; Yuksel, N.; Sydora, B.C. A survey of the availability in Canadian pharmacy chains of over-the-counter natural health products for menopause symptoms. BMC Complement. Altern. Med. 2015, 15, 86. [Google Scholar] [CrossRef] [PubMed]
- Russell, L.; Hicks, G.S.; Low, A.K.; Shepherd, J.M.; Brown, C.A. Phytoestrogens: A viable option? Am. J. Med. Sci. 2002, 324, 185–188. [Google Scholar] [CrossRef] [PubMed]
- Guo, P.P.; Li, P.; Zhang, X.H.; Liu, N.; Wang, J.; Chen, D.D.; Sun, W.J.; Zhang, W. Complementary and alternative medicine for natural and treatment-induced vasomotor symptoms: An overview of systematic reviews and meta-analyses. Complement. Ther. Clin. Pract. 2019, 36, 181–194. [Google Scholar] [CrossRef] [PubMed]
- Hill, D.A.; Crider, M.; Hill, S.R. Hormone therapy and other treatments for symptoms of menopause. Am. Fam. Physician 2016, 94, 884–889. [Google Scholar] [PubMed]
- Chen, L.R.; Ko, N.Y.; Chen, K.H. Medical Treatment for osteoporosis: From molecular to clinical opinions. Int. J. Mol. Sci. 2019, 20, 2213. [Google Scholar] [CrossRef]
- National Osteoporosis Foundation. Clinician’s Guide to Prevention and Treatment of Osteoporosis; National Osteoporosis Foundation: Washington, DC, USA, 2010. [Google Scholar]
- De Franciscis, P.; Colacurci, N.; Riemma, G.; Conte, A.; Pittana, E.; Guida, M.; Schiattarella, A. A nutraceutical approach to menopausal complaints. Medicina 2019, 55, 544. [Google Scholar] [CrossRef]
- Welty, F.K.; Lee, K.S.; Lew, N.S.; Nasca, M.; Zhou, J.R. The association between soy nut consumption and decreased menopausal symptoms. J. Womens Health 2007, 16, 361–369. [Google Scholar] [CrossRef]
- Reed, S.D.; Lampe, J.W.; Qu, C.; Gundersen, G.; Fuller, S.; Copeland, W.K.; Newton, K.M. Self-reported menopausal symptoms in a racially diverse population and soy food consumption. Maturitas 2013, 75, 152–158. [Google Scholar] [CrossRef]
- Ewies, A.A.A. Phytoestrogens in the management of the menopause: Up-to-date. Obstet. Gynecol. Surv. 2002, 57, 306–313. [Google Scholar] [CrossRef]
- Lambert, M.N.T.; Thorup, A.C.; Hansen, E.S.S.; Jeppesen, P.B. Combined Red Clover isoflavones and probiotics potently reduce menopausal vasomotor symptoms. PLoS ONE 2017, 12, e0176590. [Google Scholar] [CrossRef] [PubMed]
- Britt, K.L.; Simpson, E.R.; Findlay, J.K. Effects of phytoestrogens on the ovarian and pituitary phenotypes of estrogen-deficient female aromatase knockout mice. Menopause 2005, 12, 174–185. [Google Scholar] [CrossRef] [PubMed]
- Levis, S.; Strickman-Stein, N.; Doerge, D.R.; Krischer, J. Design and baseline characteristics of the soy phytoestrogens as replacement estrogen (SPARE) study—A clinical trial of the effects of soy isoflavones in menopausal women. Contemp. Clin. Trials 2010, 31, 293–302. [Google Scholar] [CrossRef] [PubMed]
- North American Menopause Society. The role of isoflavones in menopausal health: Consensus opinion of The North American Menopause Society. Menopause 2000, 7, 215–229. [Google Scholar] [CrossRef]
- Tsourounis, C. Clinical effects of phytoestrogens. Clin. Obstet. Gynecol. 2001, 44, 836–842. [Google Scholar] [CrossRef]
- North American Menopause Society. The role of soy isoflavones in menopausal health: Report of The North American Menopause Society/Wulf H. Utian Translational Science Symposium in Chicago, IL (October 2010). Menopause 2011, 18, 732–753. [Google Scholar] [CrossRef]
- Jackson, R.L.; Greiwe, J.S.; Desai, P.B.; Schwen, R.J. Single-dose and steady-state pharmacokinetic studies of S-equol, a potent nonhormonal, estrogen receptor β-agonist being developed for the treatment of menopausal symptoms. Menopause 2011, 18, 185–193. [Google Scholar] [CrossRef]
- Newton, K.M.; Reed, S.D.; Uchiyama, S.; Qu, C.; Ueno, T.; Iwashita, S.; Gunderson, G.; Fuller, S.; Lampe, J.W. A cross-sectional study of equol producer status and self-reported vasomotor symptoms. Menopause 2015, 22, 489–495. [Google Scholar] [CrossRef]
- Setchell, K.D.R. The history and basic science development of soy isoflavones. Menopause 2017, 24, 1338–1350. [Google Scholar] [CrossRef]
- Guadamuro, L.; Dohrmann, A.B.; Tebbe, C.C.; Mayo, B.; Delgado, S. Bacterial communities and metabolic activity of faecal cultures from equol producer and non-producer menopausal women under treatment with soy isoflavones. BMC Microbiol. 2017, 17, 93. [Google Scholar] [CrossRef]
- Ishiwata, N.; Melby, M.K.; Mizuno, S.; Watanabe, S. New equol supplement for relieving menopausal symptoms: Randomized, placebo-controlled trial of Japanese women. Menopause 2009, 16, 141–148. [Google Scholar] [CrossRef] [PubMed]
- St Germain, A.; Peterson, C.T.; Robinson, J.G.; Alekel, D.L. Isoflavone-rich or isoflavone-poor soy protein does not reduce menopausal symptoms during 24 weeks of treatment. Menopause 2001, 8, 17–26. [Google Scholar] [CrossRef] [PubMed]
- Tice, J.A.; Ettinger, B.; Ensrud, K.; Wallace, R.; Blackwell, T.; Cummings, S.R. Phytoestrogen supplements for the treatment of hot flashes: The Isoflavone Clover Extract (ICE) Study: A randomized controlled trial. JAMA 2003, 290, 207–214. [Google Scholar] [CrossRef] [PubMed]
- Cancellieri, F.; De Leo, V.; Genazzani, A.D.; Nappi, C.; Parenti, G.L.; Polatti, F.; Ragni, N.; Savoca, S.; Teglio, L.; Finelli, F.; et al. Efficacy on menopausal neurovegetative symptoms and some plasma lipids blood levels of an herbal product containing isoflavones and other plant extracts. Maturitas 2007, 56, 249–256. [Google Scholar] [CrossRef]
- Cheng, G.; Wilczek, B.; Warner, M.; Gustafsson, J.-A.; Landgren, B.M. Isoflavone treatment for acute menopausal symptoms. Menopause 2007, 14, 468–473. [Google Scholar] [CrossRef]
- Thomas, A.; Ismail, R.; Taylor-Swanson, L.; Cray, L.; Schnall, J.G.; Mitchell, E.S.; Woods, N.F. Effects of isoflavones and amino acid therapies for hot flashes and co-occurring symptoms during the menopausal transition and early post menopause: A systematic review. Maturitas 2014, 78, 263–276. [Google Scholar] [CrossRef]
- Washburn, S.; Burke, G.L.; Morgan, T.; Anthony, M. Effect of soy protein supplementation on serum lipoproteins, blood pressure, and menopausal symptoms in perimenopausal women. Menopause 1999, 6, 7–13. [Google Scholar] [CrossRef]
- Khaodhiar, L.; Ricciotti, H.A.; Li, L.; Pan, W.; Schickel, M.; Zhou, J.; Blackburn, G.L. Daidzein-rich isoflavone aglycones are potentially effective in reducing hot flashes in menopausal women. Menopause 2008, 15, 125–132. [Google Scholar] [CrossRef]
- Cianci, A.; Colacurci, N.; Paoletti, A.M.; Perino, A.; Cicinelli, E.; Maffei, S.; Di Martino, M.; Daguati, R.; Stomati, M.; Pilloni, M.; et al. Soy isoflavones, inulin, calcium, and vitamin D3 in post-menopausal hot flushes: An observational study. Clin. Exp. Obstet. Gynecol. 2015, 42, 743–745. [Google Scholar]
- Carmignani, L.O.; Pedro, A.O.; Costa-Paiva, L.H.; Pinto-Neto, A.M. The effect of dietary soy supplementation compared to estrogen and placebo on menopausal symptoms: A randomized controlled trial. Maturitas 2010, 67, 262–269. [Google Scholar] [CrossRef]
- Bolaños-Díaz, R.; Zavala-Gonzales, J.-C.; Mezones-Holguín, E.; Francia-Romero, J. Soy extracts versus hormone therapy for reduction of menopausal hot flushes: Indirect comparison. Menopause 2011, 18, 825–829. [Google Scholar] [CrossRef] [PubMed]
- Amato, P.; Young, R.L.; Steinberg, F.M.; Murray, M.J.; Lewis, R.D.; Cramer, M.A.; Barnes, S.; Ellis, K.J.; Shypailo, R.J.; Fraley, J.K.; et al. Effect of soy isoflavone supplementation on menopausal quality of life. Menopause 2013, 20, 443–447. [Google Scholar] [CrossRef] [PubMed]
- Daily, J.W.; Ko, B.S.; Ryuk, J.; Liu, M.; Zhang, W.; Park, S. Equol decreases hot flashes in postmenopausal women: A systematic review and meta-analysis of randomized clinical trials. J. Med. Food 2019, 22, 127–139. [Google Scholar] [CrossRef] [PubMed]
- Lambert, M.N.T.; Hu, L.M.; Jeppesen, P.B. A systematic review and meta-analysis of the effects of isoflavone formulations against estrogen-deficient bone resorption in peri- and postmenopausal women. Am. J. Clin. Nutr. 2017, 106, 801–811. [Google Scholar] [CrossRef]
- Ma, D.-F.; Qin, L.-Q.; Wang, P.-Y.; Katoh, R. Soy isoflavone intake increases bone mineral density in the spine of menopausal women: Meta-analysis of randomized controlled trials. Clin. Nutr. 2008, 27, 57–64. [Google Scholar] [CrossRef]
- Van der Schouw, Y.T.; Kreijkamp-Kaspers, S.; Peeters, P.H.M.; Keinan-Boker, L.; Rimm, E.B.; Grobbee, D.E. Prospective study on usual dietary phytoestrogen intake and cardiovascular disease risk in Western women. Circulation 2005, 111, 465–471. [Google Scholar] [CrossRef]
- Nestel, P.J.; Yamashita, T.; Sasahara, T.; Pomeroy, S.; Dart, A.; Komesaroff, P.; Owen, A.; Abbey, M. Soy isoflavones improve systemic arterial compliance but not plasma lipids in menopausal and perimenopausal women. Arterioscler. Thromb. Vasc. Biol. 1997, 17, 3392–3398. [Google Scholar] [CrossRef]
- Brzezinski, A.; Danenberg, H.D. Sex hormones, soy, and myocardial injury. Menopause 2008, 15, 217–220. [Google Scholar] [CrossRef]
- Wong, W.W.; Taylor, A.A.; Smith, E.O.; Barnes, S.; Hachey, D.L. Effect of soy isoflavone supplementation on nitric oxide metabolism and blood pressure in menopausal women. Am. J. Clin. Nutr. 2012, 95, 1487–1494. [Google Scholar] [CrossRef]
- Suparto, I.H.; Williams, J.K.; Fox, J.L.; Yusuf, J.T.L.; Sajuthi, D. Effects of hormone therapy and dietary soy on myocardial ischemia/reperfusion injury in ovariectomized atherosclerotic monkeys. Menopause 2008, 15, 256–263. [Google Scholar] [CrossRef]
- Sathyapalan, T.; Aye, M.; Rigby, A.S.; Thatcher, N.J.; Dargham, S.R.; Kilpatrick, E.S.; Atkin, S.L. Soy isoflavones improve cardiovascular disease risk markers in women during the early menopause. Nutr. Metab. Cardiovasc. Dis. 2018, 28, 691–697. [Google Scholar] [CrossRef] [PubMed]
- Stuenkel, C.A. Isoflavones and cardiovascular risk in postmenopausal women: No free lunch. Menopause 2007, 14, 606–608. [Google Scholar] [CrossRef] [PubMed]
- Mueller, M.; Jungbauer, A. Red clover extract: A putative source for simultaneous treatment of menopausal disorders and the metabolic syndrome. Menopause 2008, 15, 1120–1131. [Google Scholar] [CrossRef] [PubMed]
- Reiter, E.; Beck, V.; Medjakovic, S.; Mueller, M.; Jungbauer, A. Comparison of hormonal activity of isoflavone-containing supplements used to treat menopausal complaints. Menopause 2009, 16, 1049–1060. [Google Scholar] [CrossRef] [PubMed]
- Hirose, K.; Imaeda, N.; Tokudome, Y.; Goto, C.; Wakai, K.; Matsuo, K.; Ito, H.; Toyama, T.; Iwata, H.; Tokudome, S.; et al. Soybean products and reduction of breast cancer risk: A case—Control study in Japan. Br. J. Cancer 2005, 93, 15–22. [Google Scholar] [CrossRef]
- Alipour, S.; Afshar, S.; Moini, A.; Dastjerdi, M.; Saberi, A.; Bayani, L.; Eslami, B.; Hosseini, L. Clinical and ultrasonographic changes of the breast after use of soy isoflavones. APJCP 2012, 13, 6093–6095. [Google Scholar] [CrossRef]
- Shike, M.; Doane, A.S.; Russo, L.; Cabal, R.; Reis-Filho, J.S.; Gerald, W.; Cody, H.; Khanin, R.; Bromberg, J.; Norton, L. The effects of soy supplementation on gene expression in breast cancer: A randomized placebo-controlled study. J. Natl. Cancer Inst. 2014, 106, dju189. [Google Scholar] [CrossRef]
- Kang, X.; Zhang, Q.; Wang, S.; Huang, X.; Jin, S. Effect of soy isoflavones on breast cancer recurrence and death for patients receiving adjuvant endocrine therapy. CMAJ 2010, 182, 1857–1862. [Google Scholar] [CrossRef]
- Shin, A.; Lee, J.; Lee, J.; Park, M.S.; Park, J.W.; Park, S.C.; Oh, J.H.; Kim, J. Isoflavone and soyfood intake and colorectal cancer risk: A case-control study in Korea. PLoS ONE 2015, 10, e0143228. [Google Scholar] [CrossRef]
- Waetjen, L.E.; Leung, K.; Crawford, S.L.; Huang, M.-H.; Gold, E.B.; Greendale, G.A. Study of women’s health across the nation relationship between dietary phytoestrogens and development of urinary incontinence in midlife women. Menopause 2013, 20, 428–436. [Google Scholar] [CrossRef][Green Version]
- Reed, S.D.; Newton, K.M.; LaCroix, A.Z.; Grothaus, L.C.; Grieco, V.S.; Ehrlich, K. Vaginal, endometrial, and reproductive hormone findings: Randomized, placebo-controlled trial of black cohosh, multibotanical herbs, and dietary soy for vasomotor symptoms: The Herbal Alternatives for Menopause (HALT) Study. Menopause 2008, 15, 51–58. [Google Scholar] [CrossRef] [PubMed]
- Burton, J.L.; Wells, M. The effect of phytoestrogens on the female genital tract. J. Clin. Pathol. 2002, 55, 401–407. [Google Scholar] [CrossRef] [PubMed]
- Vitale, S.G.; Caruso, S.; Rapisarda, A.M.C.; Cianci, S.; Cianci, A. Isoflavones, calcium, vitamin D and inulin improve quality of life, sexual function, body composition and metabolic parameters in menopausal women: Result from a prospective, randomized, placebo-controlled, parallel-group study. Prz. Menopauzalny 2018, 17, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Greendale, G.A.; Huang, M.-H.; Leung, K.; Crawford, S.L.; Gold, E.B.; Wight, R.; Waetjen, E.; Karlamangla, A.S. Dietary phytoestrogen intakes and cognitive function during the menopausal transition: Results from the study of women’s health across the nation phytoestrogen Study. Menopause 2012, 19, 894–903. [Google Scholar] [CrossRef]
- Clement, Y.N.; Onakpoya, I.; Hung, S.K.; Ernst, E. Effects of herbal and dietary supplements on cognition in menopause: A systematic review. Maturitas 2011, 68, 256–263. [Google Scholar] [CrossRef]
- Rachoń, D.; Menche, A.; Vortherms, T.; Seidlová-Wuttke, D.; Wuttke, W. Effects of dietary equol administration on the mammary gland in ovariectomized Sprague-Dawley rats. Menopause 2008, 15, 340–345. [Google Scholar] [CrossRef]
- Eden, J.A. Phytoestrogens for menopausal symptoms: A review. Maturitas 2012, 72, 157–159. [Google Scholar] [CrossRef]
- Bolaños, R.; Del Castillo, A.; Francia, J. Soy isoflavones versus placebo in the treatment of climacteric vasomotor symptoms: Systematic review and meta-analysis. Menopause 2010, 17, 660–666. [Google Scholar] [CrossRef]
- Nelson, H.D.; Vesco, K.K.; Haney, E.; Fu, R.; Nedrow, A.; Miller, J.; Nicolaidis, C.; Walker, M.; Humphrey, L. Nonhormonal therapies for menopausal hot flashes: Systematic review and meta-analysis. JAMA 2006, 295, 2057–2071. [Google Scholar] [CrossRef]
- Taku, K.; Melby, M.K.; Kronenberg, F.; Kurzer, M.S.; Messina, M. Extracted or synthesized soybean isoflavones reduce menopausal hot flash frequency and severity: Systematic review and meta-analysis of randomized controlled trials. Menopause 2012, 19, 776–790. [Google Scholar] [CrossRef]
- Li, L.; Lv, Y.; Xu, L.; Zheng, Q. Quantitative efficacy of soy isoflavones on menopausal hot flashes. Br. J. Clin. Pharmacol. 2015, 79, 593–604. [Google Scholar] [CrossRef] [PubMed]
- Wuttke, W.; Jarry, H.; Seidlová-Wuttke, D. Isoflavones—Safe food additives or dangerous drugs? Ageing Res. Rev. 2007, 6, 150–188. [Google Scholar] [CrossRef] [PubMed]
- Messina, M. Soybean isoflavones warrant greater consideration as a treatment for the alleviation of menopausal hot flashes. Womens Health 2014, 10, 549–553. [Google Scholar] [CrossRef] [PubMed]
- Utian, W.H.; Jones, M.; Setchell, K.D.R. S-equol: A potential nonhormonal agent for menopause-related symptom relief. J. Womens Health 2015, 24, 200–208. [Google Scholar] [CrossRef] [PubMed]
- Crawford, S.L.; Jackson, E.A.; Churchill, L.; Lampe, J.W.; Leung, K.; Ockene, J.K. The impact of dose, frequency of administration, and equol production on efficacy of isoflavones for menopausal hot flashes: A pilot randomized trial. Menopause 2013, 20, 911–921. [Google Scholar] [CrossRef] [PubMed]
- Su Wei Poh, M.; Voon Chen Yong, P.; Viseswaran, N.; Chia, Y.Y. Estrogenicity of glabridin in Ishikawa cells. PLoS ONE 2015, 10. [Google Scholar] [CrossRef] [PubMed]
| Studies (Ref. No.) | Study Design | Contents | Main Results |
|---|---|---|---|
| Hot flashes | |||
| [23] St Germain | RCT | soy | no difference |
| [24] Tice | RCT | isoflavone tablets | no difference |
| [25] Cancellieri | RCT | isoflavone from herbal supplement | isoflavones more effective than placebo |
| [26] Cheng | prospective study | isoflavones extracted from soya bean | isoflavones more effective than placebo |
| [9] Welty | RCT, crossover | soy nut | soy more effective than placebo |
| [27] Thomas | systematic review | natural vs. synthetic isoflavones | synthetic or combination isoflavones more effective than natural soy |
| [28] Washburn | randomized crossover trial | soy protein | soy protein more effective than placebo |
| [29] Khaodhiar | RCT | daidzein-rich isoflavone aglycones | daidzein-rich isoflavone aglycones more effective than placebo |
| [30] Cianci | observational prospective study | calcium, vitamin D3, inulin, soy isoflavones | soy supplement + inulin effective |
| [31] Carmignani | RCT | soy vs. HRT | HRT more effective than soy; both are superior to placebo |
| [32] Bolanos-Dıaz | meta-analysis | soy extracts vs. HRT | HRT more effective than soy extracts; both are superior to placebo |
| [33] Amato | multicenter RCT | aglycone hypocotyl soy isoflavone | no difference |
| [34] Daily | systematic review, meta-analysis | soy isoflavone and equol | equol or isoflavone in equol-producers more effective than placebo |
| [19] Newton | observational study | equol-producer status | soy in equol-producers more effective than non-producers |
| [12] Lambert | RCT | red clover extracts | red clover extracts more effective than placebo |
| BMD | |||
| [36] Ma | meta-analysis | isoflavone | increase spinal BMD |
| [33] Amato | multicenter RCT | aglycone hypocotyl soy isoflavone | slow BMD loss |
| [35] Lambert | systematic review and meta-analysis | isoflavone aglycone | preserve BMD |
| CV | |||
| [37] van der Schouw | prospective study | food phytoestrogens | low dose phytoestrogen not protective |
| [38] Nestel | randomized crossover trial | purified soybean extract | may improve systemic arterial compliance |
| [26] Cheng | prospective study | isoflavones extracted from soya bean | no difference in lipoprotein lipids |
| [40] Wong | RCT | soy hypocotyl isoflavones | no effect on nitric oxide metabolism or blood pressure |
| [41] Suparto | animal study | soy protein | HRT + soy harmful, soy or HRT not beneficial |
| [42] Sathyapalan | double blind randomised study | soy protein +/− soy isoflavone | soy protein with isoflavones improved CVR markers compared to soy protein alone |
| Metabolic syndrome | |||
| [43] Stuenkel | randomized clinical trial | isoflavone supplements | loss of weight and fat mass, but interpretation difficult |
| [44] Mueller | in vitro study | PPARgamma binding and transactivational activity | red clover extracts may be used to treat metabolic syndrome |
| Cancer risk | |||
| [46] Hirose | case-control study | soy products as part of daily intake | lower risk of breast cancer in premenopausal women |
| [47] Alipour | case-control study | soy extracts | soy extracts may cause benign changes in breast |
| [49] Kang | cohort study | dietary intake of soy isoflavones | lower recurrence in postmenopausal women with estrogen- and progesterone-receptor positive breast cancers receiving anastrazole therapy after surgery |
| [50] Shin | case-control study | dietary soyfood and isoflavone intake | reduced risk for overall colorectal cancer |
| Urogenital tract | |||
| [52] Reed | RCT | black cohosh or dietary soy | no effect on vaginal cytology |
| [51] Waetjen | prospective cohort study | dietary intake of isoflavones | no effect on stress or urge incontinence |
| [54] Vitale | prospective, randomized, placebo-controlled study | isoflavones, calcium, vitamin D, inulin | improves sexual function |
| Cognition | |||
| [55] Greendale | cohort study | dietary phytoestrogens | better processing speed, but worse verbal memory |
| [56] Clement | systematic review | isoflavones and soy | may improve cognition |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, L.-R.; Ko, N.-Y.; Chen, K.-H. Isoflavone Supplements for Menopausal Women: A Systematic Review. Nutrients 2019, 11, 2649. https://doi.org/10.3390/nu11112649
Chen L-R, Ko N-Y, Chen K-H. Isoflavone Supplements for Menopausal Women: A Systematic Review. Nutrients. 2019; 11(11):2649. https://doi.org/10.3390/nu11112649
Chicago/Turabian StyleChen, Li-Ru, Nai-Yu Ko, and Kuo-Hu Chen. 2019. "Isoflavone Supplements for Menopausal Women: A Systematic Review" Nutrients 11, no. 11: 2649. https://doi.org/10.3390/nu11112649
APA StyleChen, L.-R., Ko, N.-Y., & Chen, K.-H. (2019). Isoflavone Supplements for Menopausal Women: A Systematic Review. Nutrients, 11(11), 2649. https://doi.org/10.3390/nu11112649






