The When, What & How of Measuring Vitamin D Metabolism in Clinical Medicine
Abstract
:1. Introduction
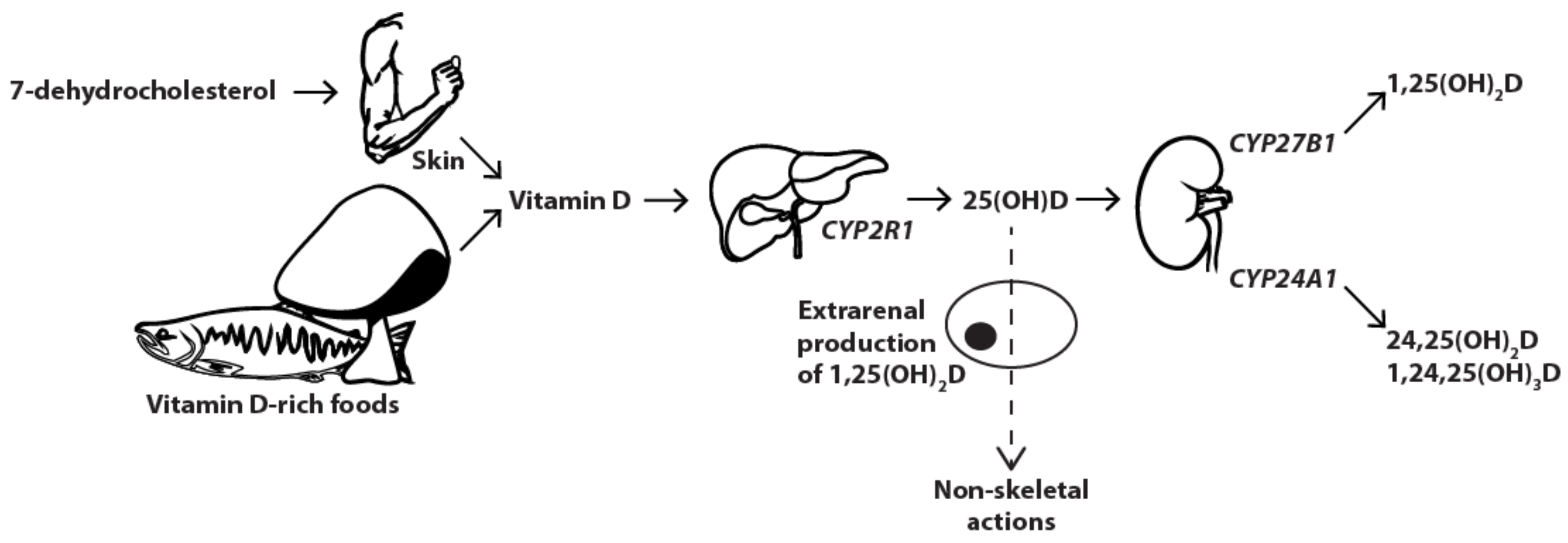
2. Vitamin D Metabolism
3. When & What: Assessing Vitamin D Metabolism Misbalance
3.1. 25(OH)D
3.2. 1,25(OH)2D
3.3. 24,25(OH)2D
3.4. Other Metabolites
4. How: Importance of the Choice of Method
4.1. 25(OH)D
4.2. 1,25(OH)2D
4.3. 24,25(OH)2D
4.4. Other Metabolites
5. Discussion and Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Heaney, R.P.; Recker, R.R.; Grote, J.; Horst, R.L.; Armas, L.A. Vitamin D(3) is more potent than vitamin D(2) in humans. J. Clin. Endocrinol. Metab. 2011, 96, E447–E452. [Google Scholar] [CrossRef] [PubMed]
- Kamao, M.; Tatematsu, S.; Hatakeyama, S.; Sakaki, T.; Sawada, N.; Inouye, K.; Ozono, K.; Kubodera, N.; Reddy, G.S.; Okano, T. C-3 epimerization of vitamin D3 metabolites and further metabolism of C-3 epimers: 25-hydroxyvitamin D3 is metabolized to 3-epi-25-hydroxyvitamin D3 and subsequently metabolized through C-1alpha or C-24 hydroxylation. J. Biol. Chem. 2004, 279, 15897–15907. [Google Scholar] [CrossRef] [PubMed]
- Saito, H.; Kusano, K.; Kinosaki, M.; Ito, H.; Hirata, M.; Segawa, H.; Miyamoto, K.; Fukushima, N. Human fibroblast growth factor-23 mutants suppress Na+-dependent phosphate co-transport activity and 1alpha,25-dihydroxyvitamin D3 production. J. Biol. Chem. 2003, 278, 2206–2211. [Google Scholar] [CrossRef] [PubMed]
- Bikle, D. Nonclassic actions of vitamin D. J. Clin. Endocrinol. Metab. 2009, 94, 26–34. [Google Scholar] [CrossRef] [PubMed]
- Liu, P.T.; Stenger, S.; Li, H.; Wenzel, L.; Tan, B.H.; Krutzik, S.R.; Ochoa, M.T.; Schauber, J.; Wu, K.; Meinken, C.; et al. Toll-like receptor triggering of a vitamin D-mediated human antimicrobial response. Science 2006, 311, 1770–1773. [Google Scholar] [CrossRef] [PubMed]
- Lips, P. Relative value of 25(OH)D and 1,25(OH)2D measurements. J. Bone Miner. Res. Off. J. Am. Soc. Bone Miner. Res. 2007, 22, 1668–1671. [Google Scholar] [CrossRef] [PubMed]
- Holick, M.F. Vitamin D deficiency. N. Engl. J. Med. 2007, 357, 266–281. [Google Scholar] [CrossRef] [PubMed]
- Holick, M.F. Vitamin D status: Measurement, interpretation, and clinical application. Ann. Epidemiol. 2009, 19, 73–78. [Google Scholar] [CrossRef] [PubMed]
- Hollis, B.W. Assessment and interpretation of circulating 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D in the clinical environment. Endocrinol. Metab. Clin. North Am. 2010, 39, 271–286. [Google Scholar] [CrossRef] [PubMed]
- Bouillon, R.; Van Schoor, N.M.; Gielen, E.; Boonen, S.; Mathieu, C.; Vanderschueren, D.; Lips, P. Optimal vitamin D status: A critical analysis on the basis of evidence-based medicine. J. Clin. Endocrinol. Metab. 2013, 98, E1283–E1304. [Google Scholar] [CrossRef] [PubMed]
- Ross, A.C.; Manson, J.E.; Abrams, S.A.; Aloia, J.F.; Brannon, P.M.; Clinton, S.K.; Durazo-Arvizu, R.A.; Gallagher, J.C.; Gallo, R.L.; Jones, G.; et al. The 2011 report on dietary reference intakes for calcium and vitamin D from the institute of medicine: What clinicians need to know. J. Clin. Endocrinol. Metab. 2011, 96, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Manson, J.E.; Brannon, P.M.; Rosen, C.J.; Taylor, C.L. Vitamin D deficiency—Is there really a pandemic? N. Engl. J. Med. 2016, 375, 1817–1820. [Google Scholar] [CrossRef] [PubMed]
- Bischoff-Ferrari, H.A.; Giovannucci, E.; Willett, W.C.; Dietrich, T.; Dawson-Hughes, B. Estimation of optimal serum concentrations of 25-hydroxyvitamin d for multiple health outcomes. Am. J. Clin. Nutr. 2006, 84, 18–28. [Google Scholar] [CrossRef] [PubMed]
- Norman, A.W.; Bouillon, R.; Whiting, S.J.; Vieth, R.; Lips, P. 13th workshop consensus for vitamin D nutritional guidelines. J. Steroid Biochem. Mol. Biol. 2007, 103, 204–205. [Google Scholar] [CrossRef] [PubMed]
- Ross, A.C. The 2011 report on dietary reference intakes for calcium and vitamin D. Public Health Nutr. 2011, 14, 938–939. [Google Scholar] [CrossRef] [PubMed]
- Holick, M.F.; Binkley, N.C.; Bischoff-Ferrari, H.A.; Gordon, C.M.; Hanley, D.A.; Heaney, R.P.; Murad, M.H.; Weaver, C.M. Evaluation, treatment, and prevention of vitamin D deficiency: An endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 2011, 96, 1911–1930. [Google Scholar] [CrossRef] [PubMed]
- Dirks, N.F.; Martens, F.; Vanderschueren, D.; Billen, J.; Pauwels, S.; Ackermans, M.T.; Endert, E.; Heijer, M.D.; Blankenstein, M.A.; Heijboer, A.C. Determination of human reference values for serum total 1,25-dihydroxyvitamin D using an extensively validated 2D ID-UPLC-MS/MS method. J. Steroid Biochem. Mol. Biol. 2016, 164, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Zalewski, A.; Ma, N.S.; Legeza, B.; Renthal, N.; Fluck, C.E.; Pandey, A.V. Vitamin D-dependent rickets type 1 caused by mutations in CYP27B1 affecting protein interactions with adrenodoxin. J. Clin. Endocrinol. Metab. 2016, 101, 3409–3418. [Google Scholar] [CrossRef] [PubMed]
- Francis, F.; Hennig, S.; Korn, B.; Reinhardrdt, R.; de Jong, P.; Poustka, A.; Lehrach, H.; Rowe, P.S.N.; Goulding, J.N.; Summerfield, T.; et al. A gene (PEX) with homologies to endopeptidases is mutated in patients with x-linked hypophosphatemic rickets. The HYP consortium. Nat. Genet. 1995, 11, 130–136. [Google Scholar] [CrossRef] [PubMed]
- Imel, E.A.; DiMeglio, L.A.; Hui, S.L.; Carpenter, T.O.; Econs, M.J. Treatment of x-linked hypophosphatemia with calcitriol and phosphate increases circulating fibroblast growth factor 23 concentrations. J. Clin. Endocrinol. Metab. 2010, 95, 1846–1850. [Google Scholar] [CrossRef] [PubMed]
- Chong, W.H.; Molinolo, A.A.; Chen, C.C.; Collins, M.T. Tumor-induced osteomalacia. Endocr.-Relat. Cancer 2011, 18, R53–R77. [Google Scholar] [CrossRef] [PubMed]
- Nagata, Y.; Imanishi, Y.; Ishii, A.; Kurajoh, M.; Motoyama, K.; Morioka, T.; Naka, H.; Mori, K.; Miki, T.; Emoto, M.; et al. Evaluation of bone markers in hypophosphatemic rickets/osteomalacia. Endocrine 2011, 40, 315–317. [Google Scholar] [CrossRef] [PubMed]
- Consortium, A. Autosomal dominant hypophosphataemic rickets is associated with mutations in FGF23. Nat. Genet. 2000, 26, 345–348. [Google Scholar]
- White, K.E.; Carn, G.; Lorenz-Depiereux, B.; Benet-Pages, A.; Strom, T.M.; Econs, M.J. Autosomal-dominant hypophosphatemic rickets (ADHR) mutations stabilize FGF-23. Kidney Int. 2001, 60, 2079–2086. [Google Scholar] [CrossRef] [PubMed]
- Levy-Litan, V.; Hershkovitz, E.; Avizov, L.; Leventhal, N.; Bercovich, D.; Chalifa-Caspi, V.; Manor, E.; Buriakovsky, S.; Hadad, Y.; Goding, J.; et al. Autosomal-recessive hypophosphatemic rickets is associated with an inactivation mutation in the ENPP1 gene. Am. J. Hum. Genet. 2010, 86, 273–278. [Google Scholar] [CrossRef] [PubMed]
- Rafaelsen, S.H.; Raeder, H.; Fagerheim, A.K.; Knappskog, P.; Carpenter, T.O.; Johansson, S.; Bjerknes, R. Exome sequencing reveals FAM20c mutations associated with fibroblast growth factor 23-related hypophosphatemia, dental anomalies, and ectopic calcification. J. Bone Miner. Res. 2013, 28, 1378–1385. [Google Scholar] [CrossRef] [PubMed]
- Riminucci, M.; Collins, M.T.; Fedarko, N.S.; Cherman, N.; Corsi, A.; White, K.E.; Waguespack, S.; Gupta, A.; Hannon, T.; Econs, M.J.; et al. FGF-23 in fibrous dysplasia of bone and its relationship to renal phosphate wasting. J. Clin. Investig. 2003, 112, 683–692. [Google Scholar] [CrossRef] [PubMed]
- Farrow, E.G.; Davis, S.I.; Mooney, S.D.; Beighton, P.; Mascarenhas, L.; Gutierrez, Y.R.; Pitukcheewanont, P.; White, K.E. Extended mutational analyses of FGFR1 in osteoglophonic dysplasia. Am. J. Med. Genet. Part A 2006, 140, 537–539. [Google Scholar] [CrossRef] [PubMed]
- Avitan-Hersh, E.; Tatur, S.; Indelman, M.; Gepstein, V.; Shreter, R.; Hershkovitz, D.; Brick, R.; Bergman, R.; Tiosano, D. Postzygotic HRAS mutation causing both keratinocytic epidermal nevus and thymoma and associated with bone dysplasia and hypophosphatemia due to elevated FGF23. J. Clin. Endocrinol. Metab. 2014, 99, E132–E136. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; Dwivedi, A.; Patel, P.; Gupta, S. Hypophosphatemic osteomalacia in von recklinghausen neurofibromatosis: Case report and literature review. Indian J. Radiol. Imaging 2015, 25, 63–66. [Google Scholar] [CrossRef] [PubMed]
- Brownstein, C.A.; Adler, F.; Nelson-Williams, C.; Iijima, J.; Li, P.; Imura, A.; Nabeshima, Y.; Reyes-Mugica, M.; Carpenter, T.O.; Lifton, R.P. A translocation causing increased alpha-klotho level results in hypophosphatemic rickets and hyperparathyroidism. Proc. Natl. Acad. Sci. USA 2008, 105, 3455–3460. [Google Scholar] [CrossRef] [PubMed]
- Brown, W.W.; Juppner, H.; Langman, C.B.; Price, H.; Farrow, E.G.; White, K.E.; McCormick, K.L. Hypophosphatemia with elevations in serum fibroblast growth factor 23 in a child with jansen’s metaphyseal chondrodysplasia. J. Clin. Endocrinol. Metab. 2009, 94, 17–20. [Google Scholar] [CrossRef] [PubMed]
- Chanakul, A.; Zhang, M.Y.; Louw, A.; Armbrecht, H.J.; Miller, W.L.; Portale, A.A.; Perwad, F. FGF-23 regulates CYP27B1 transcription in the kidney and in extra-renal tissues. PLoS ONE 2013, 8, e72816. [Google Scholar] [CrossRef] [PubMed]
- Lorenz-Depiereux, B.; Benet-Pages, A.; Eckstein, G.; Tenenbaum-Rakover, Y.; Wagenstaller, J.; Tiosano, D.; Gershoni-Baruch, R.; Albers, N.; Lichtner, P.; Schnabel, D.; et al. Hereditary hypophosphatemic rickets with hypercalciuria is caused by mutations in the sodium-phosphate cotransporter gene SLC34A3. Am. J. Hum. Genet. 2006, 78, 193–201. [Google Scholar] [CrossRef] [PubMed]
- Tieder, M.; Modai, D.; Shaked, U.; Samuel, R.; Arie, R.; Halabe, A.; Maor, J.; Weissgarten, J.; Averbukh, Z.; Cohen, N.; et al. “Idiopathic” hypercalciuria and hereditary hypophosphatemic rickets. Two phenotypical expressions of a common genetic defect. N. Engl. J. Med. 1987, 316, 125–129. [Google Scholar] [CrossRef] [PubMed]
- Goto, S.; Fujii, H.; Kono, K.; Watanabe, K.; Nakai, K.; Nishi, S. Serum FGF23 levels may not be associated with serum phosphate and 1,25-dihydroxyvitamin D levels in patients with fanconi syndrome–induced hypophosphatemia. Clin. Kidney J. 2016, 9, 677–681. [Google Scholar] [CrossRef] [PubMed]
- Adams, J.S.; Hewison, M. Extrarenal expression of the 25-hydroxyvitamin d-1-hydroxylase. Arch. Biochem. Biophys. 2012, 523, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Donovan, P.J.; Sundac, L.; Pretorius, C.J.; d’Emden, M.C.; McLeod, D.S. Calcitriol-mediated hypercalcemia: Causes and course in 101 patients. J. Clin. Endocrinol. Metab. 2013, 98, 4023–4029. [Google Scholar] [CrossRef] [PubMed]
- Abreu, M.T.; Kantorovich, V.; Vasiliauskas, E.A.; Gruntmanis, U.; Matuk, R.; Daigle, K.; Chen, S.; Zehnder, D.; Lin, Y.C.; Yang, H.; et al. Measurement of vitamin D levels in inflammatory bowel disease patients reveals a subset of crohn’s disease patients with elevated 1,25-dihydroxyvitamin D and low bone mineral density. Gut 2004, 53, 1129–1136. [Google Scholar] [CrossRef] [PubMed]
- Karakelides, H.; Geller, J.L.; Schroeter, A.L.; Chen, H.; Behn, P.S.; Adams, J.S.; Hewison, M.; Wermers, R.A. Vitamin D-mediated hypercalcemia in slack skin disease: Evidence for involvement of extrarenal 25-hydroxyvitamin D 1alpha-hydroxylase. J. Bone Miner. Res. Off. J. Am. Soc. Bone Miner. Res. 2006, 21, 1496–1499. [Google Scholar] [CrossRef] [PubMed]
- Jones, G.; Strugnell, S.A.; DeLuca, H.F. Current understanding of the molecular actions of vitamin D. Physiol. Rev. 1998, 78, 1193–1231. [Google Scholar] [CrossRef] [PubMed]
- St-Arnaud, R.; Glorieux, F.H. 24,25-dihydroxyvitamin D—Active metabolite or inactive catabolite? Endocrinology 1998, 139, 3371–3374. [Google Scholar] [CrossRef] [PubMed]
- St-Arnaud, R. Novel findings about 24,25-dihydroxyvitamin D: An active metabolite? Curr. Opin. Nephrol. Hypertens. 1999, 8, 435–441. [Google Scholar] [CrossRef] [PubMed]
- Wagner, D.; Hanwell, H.E.; Schnabl, K.; Yazdanpanah, M.; Kimball, S.; Fu, L.; Sidhom, G.; Rousseau, D.; Cole, D.E.; Vieth, R. The ratio of serum 24,25-dihydroxyvitamin D(3) to 25-hydroxyvitamin D(3) is predictive of 25-hydroxyvitamin D(3) response to vitamin D(3) supplementation. J. Steroid Biochem. Mol. Biol. 2011, 126, 72–77. [Google Scholar] [CrossRef] [PubMed]
- Kaufmann, M.; Gallagher, J.C.; Peacock, M.; Schlingmann, K.P.; Konrad, M.; DeLuca, H.F.; Sigueiro, R.; Lopez, B.; Mourino, A.; Maestro, M.; et al. Clinical utility of simultaneous quantitation of 25-hydroxyvitamin D and 24,25-dihydroxyvitamin D by LC-MS/MS involving derivatization with DMEQ-TAD. J. Clin. Endocrinol. Metab. 2014, 99, 2567–2574. [Google Scholar] [CrossRef] [PubMed]
- Schlingmann, K.P.; Kaufmann, M.; Weber, S.; Irwin, A.; Goos, C.; John, U.; Misselwitz, J.; Klaus, G.; Kuwertz-Broking, E.; Fehrenbach, H.; et al. Mutations in CYP24A1 and idiopathic infantile hypercalcemia. N. Engl. J. Med. 2011, 365, 410–421. [Google Scholar] [CrossRef] [PubMed]
- Dinour, D.; Beckerman, P.; Ganon, L.; Tordjman, K.; Eisenstein, Z.; Holtzman, E.J. Loss-of-function mutations of CYP24A1, the vitamin D 24-hydroxylase gene, cause long-standing hypercalciuric nephrolithiasis and nephrocalcinosis. J. Urol. 2013, 190, 552–557. [Google Scholar] [CrossRef] [PubMed]
- Sayers, J.; Hynes, A.M.; Srivastava, S.; Dowen, F.; Quinton, R.; Datta, H.K.; Sayer, J.A. Successful treatment of hypercalcaemia associated with a CYP24A1 mutation with fluconazole. Clin. Kidney J. 2015, 8, 453–455. [Google Scholar] [CrossRef] [PubMed]
- Nesterova, G.; Malicdan, M.C.; Yasuda, K.; Sakaki, T.; Vilboux, T.; Ciccone, C.; Horst, R.; Huang, Y.; Golas, G.; Introne, W.; et al. 1,25-(OH)2D-24 hydroxylase (CYP24A1) deficiency as a cause of nephrolithiasis. Clin. J. Am. Soc. Nephrol. CJASN 2013, 8, 649–657. [Google Scholar] [CrossRef] [PubMed]
- Molin, A.; Baudoin, R.; Kaufmann, M.; Souberbielle, J.C.; Ryckewaert, A.; Vantyghem, M.C.; Eckart, P.; Bacchetta, J.; Deschenes, G.; Kesler-Roussey, G.; et al. CYP24A1 mutations in a cohort of hypercalcemic patients: Evidence for a recessive trait. J. Clin. Endocrinol. Metab. 2015, 100, E1343–E1352. [Google Scholar] [CrossRef] [PubMed]
- Cashman, K.D.; Hayes, A.; Galvin, K.; Merkel, J.; Jones, G.; Kaufmann, M.; Hoofnagle, A.N.; Carter, G.D.; Durazo-Arvizu, R.A.; Sempos, C.T. Significance of serum 24,25-dihydroxyvitamin D in the assessment of vitamin D status: A double-edged sword? Clin. Chem. 2015, 61, 636–645. [Google Scholar] [CrossRef] [PubMed]
- Depreter, B.; Heijboer, A.C.; Langlois, M.R. Accuracy of three automated 25-hydroxyvitamin D assays in hemodialysis patients. Clin. Chim. Acta Int. J. Clin. Chem. 2013, 415, 255–260. [Google Scholar] [CrossRef] [PubMed]
- Ong, L.; Saw, S.; Sahabdeen, N.B.; Tey, K.T.; Ho, C.S.; Sethi, S.K. Current 25-hydroxyvitamin D assays: Do they pass the test? Clin. Chim. Acta Int. J. Clin. Chem. 2012, 413, 1127–1134. [Google Scholar] [CrossRef] [PubMed]
- Farrell, C.J.; Martin, S.; McWhinney, B.; Straub, I.; Williams, P.; Herrmann, M. State-of-the-art vitamin D assays: A comparison of automated immunoassays with liquid chromatography-tandem mass spectrometry methods. Clin. Chem. 2012, 58, 531–542. [Google Scholar] [CrossRef] [PubMed]
- Heijboer, A.C.; Blankenstein, M.A.; Kema, I.P.; Buijs, M.M. Accuracy of 6 routine 25-hydroxyvitamin D assays: Influence of vitamin d binding protein concentration. Clin. Chem. 2012, 58, 543–548. [Google Scholar] [CrossRef] [PubMed]
- Wise, S.A.; Phinney, K.W.; Tai, S.S.; Camara, J.E.; Myers, G.L.; Durazo-Arvizu, R.; Tian, L.; Hoofnagle, A.N.; Bachmann, L.M.; Young, I.S.; et al. Baseline assessment of 25-hydroxyvitamin D assay performance: A vitamin D standardization program (VDSP) interlaboratory comparison study. J. AOAC Int. 2017, 100, 1244–1252. [Google Scholar] [CrossRef] [PubMed]
- Cavalier, E.; Lukas, P.; Bekaert, A.C.; Peeters, S.; Le Goff, C.; Yayo, E.; Delanaye, P.; Souberbielle, J.C. Analytical and clinical evaluation of the new Fujirebio Lumipulse® G non-competitive assay for 25(OH)-vitamin D and three immunoassays for 25(OH)D in healthy subjects, osteoporotic patients, third trimester pregnant women, healthy African subjects, hemodialyzed and intensive care patients. Clin. Chem. Lab. Med. 2016, 54, 1347–1355. [Google Scholar] [PubMed]
- Elsenberg, E.; Ten Boekel, E.; Huijgen, H.; Heijboer, A.C. Standardization of automated 25-hydroxyvitamin D assays: How successful is it? Clin. Biochem. 2017, 50, 1126–1130. [Google Scholar] [CrossRef] [PubMed]
- Freeman, J.; Wilson, K.; Spears, R.; Shalhoub, V.; Sibley, P. Influence of vitamin d binding protein on accuracy of 25-hydroxyvitamin D measurement using the advia centaur vitamin d total assay. Int. J. Endocrinol. 2014, 2014, 691679. [Google Scholar] [PubMed]
- Hsu, S.A.; Soldo, J.; Gupta, M. Evaluation of two automated immunoassays for 25-OH vitamin D: Comparison against LC-MS/MS. J. Steroid Biochem. Mol. Biol. 2013, 136, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Janssen, M.J.; Wielders, J.P.; Bekker, C.C.; Boesten, L.S.; Buijs, M.M.; Heijboer, A.C.; van der Horst, F.A.; Loupatty, F.J.; van den Ouweland, J.M. Multicenter comparison study of current methods to measure 25-hydroxyvitamin D in serum. Steroids 2012, 77, 1366–1372. [Google Scholar] [CrossRef] [PubMed]
- Chouiali, A.; Mallet, P.L.; Fink, G.; Biron, S.; Langlois, M.F. Comparison of two methods for measuring 25-OH vitamin D in the follow-up of patients after bilio-pancreatic diversion bariatric surgery. Clin. Biochem. 2017, 50, 210–216. [Google Scholar] [CrossRef] [PubMed]
- Brock, A.T.; Strickland, S.W.; Bazydlo, L.A.L.; Haverstick, D.M. An underestimation of 25-OH vitamin D in patients with renal disease by the abbott architect immunoassay. J. Appl. Lab. Med. AACC Publ. 2017, 2, 449–451. [Google Scholar]
- Shu, I.; Pina-Oviedo, S.; Quiroga-Garza, G.; Meng, Q.H.; Wang, P. Influence of vitamin D2 percentage on accuracy of 4 commercial total 25-hydroxyvitamin D assays. Clin. Chem. 2013, 59, 1273–1275. [Google Scholar] [CrossRef] [PubMed]
- Tolan, N.V.; Yoon, E.J.; Brady, A.R.; Horowitz, G.L. Price of high-throughput 25-hydroxyvitamin D immunoassays: Frequency of inaccurate results. J. Appl. Lab. Med. AACC Publ. 2017, 2. [Google Scholar] [CrossRef]
- Le Goff, C.; Peeters, S.; Crine, Y.; Lukas, P.; Souberbielle, J.C.; Cavalier, E. Evaluation of the cross-reactivity of 25-hydroxyvitamin D2 on seven commercial immunoassays on native samples. Clin. Chem. Lab. Med. 2012, 50, 2031–2032. [Google Scholar] [CrossRef] [PubMed]
- Carter, G.D.; Jones, J.C.; Shannon, J.; Williams, E.L.; Jones, G.; Kaufmann, M.; Sempos, C. 25-hydroxyvitamin D assays: Potential interference from other circulating vitamin D metabolites. J. Steroid Biochem. Mol. Biol. 2016, 164, 134–138. [Google Scholar] [CrossRef] [PubMed]
- Dowling, K.G.; Hull, G.; Sundvall, J.; Lamberg-Allardt, C.; Cashman, K.D. Improved accuracy of an tandem liquid chromatography-mass spectrometry method measuring 24R,25-dihydroxyvitamin D3 and 25-hydroxyvitamin D metabolites in serum using unspiked controls and its application to determining cross-reactivity of a chemiluminescent microparticle immunoassay. J. Chromatogr. A 2017, 1497, 102–109. [Google Scholar] [PubMed]
- Burdette, C.Q.; Camara, J.E.; Nalin, F.; Pritchett, J.; Sander, L.C.; Carter, G.D.; Jones, J.; Betz, J.M.; Sempos, C.T.; Wise, S.A. Establishing an accuracy basis for the vitamin D external quality assessment scheme (DEQAS). J. AOAC Int. 2017, 100, 1277–1287. [Google Scholar] [CrossRef] [PubMed]
- Ooms, N.; van Daal, H.; Beijers, A.M.; Gerrits, G.P.; Semmekrot, B.A.; van den Ouweland, J.M. Time-course analysis of 3-epi-25-hydroxyvitamin D3 shows markedly elevated levels in early life, particularly from vitamin D supplementation in preterm infants. Pediatr. Res. 2016, 79, 647–653. [Google Scholar] [CrossRef] [PubMed]
- Van den Ouweland, J.M.; Beijers, A.M.; van Daal, H. Overestimation of 25-hydroxyvitamin D3 by increased ionisation efficiency of 3-epi-25-hydroxyvitamin D3 in LC-MS/MS methods not separating both metabolites as determined by an LC-MS/MS method for separate quantification of 25-hydroxyvitamin D3, 3-epi-25-hydroxyvitamin D3 and 25-hydroxyvitamin D2 in human serum. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2014, 967, 195–202. [Google Scholar]
- Carter, G.D. Accuracy of 25-hydroxyvitamin D assays: Confronting the issues. Curr. Drug Targets 2011, 12, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Fabregat-Cabello, N.; Farre-Segura, J.; Huyghebaert, L.; Peeters, S.; Le Goff, C.; Souberbielle, J.-C.; Cavalier, É. A fast and simple method for simultaneous measurements of 25(OH)D, 24,25(OH)2D and the vitamin D metabolite ratio (VMR) in serum samples by LC-MS/MS. Clin. Chim. Acta 2017, 473, 116–123. [Google Scholar] [CrossRef] [PubMed]
- Jenkinson, C.; Taylor, A.E.; Hassan-Smith, Z.K.; Adams, J.S.; Stewart, P.M.; Hewison, M.; Keevil, B.G. High throughput LC-MS/MS method for the simultaneous analysis of multiple vitamin D analytes in serum. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2016, 1014, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Muller, M.J.; Stokes, C.S.; Lammert, F.; Volmer, D.A. Chemotyping the distribution of vitamin D metabolites in human serum. Sci. Rep. 2016, 6, 21080. [Google Scholar] [CrossRef] [PubMed]
- Van den Ouweland, J.M.; Beijers, A.M.; van Daal, H. Fast separation of 25-hydroxyvitamin D3 from 3-epi-25-hydroxyvitamin D3 in human serum by liquid chromatography-tandem mass spectrometry: Variable prevalence of 3-epi-25-hydroxyvitamin D3 in infants, children, and adults. Clin. Chem. 2011, 57, 1618–1619. [Google Scholar] [CrossRef] [PubMed]
- Carter, G.D.; Jones, J.C. Use of a common standard improves the performance of liquid chromatography-tandem mass spectrometry methods for serum 25-hydroxyvitamin-D. Ann. Clin. Biochem. 2009, 46, 79–81. [Google Scholar] [CrossRef] [PubMed]
- Dirks, N.F.; Vesper, H.W.; van Herwaarden, A.E.; van den Ouweland, J.M.; Kema, I.P.; Krabbe, J.G.; Heijboer, A.C. Various calibration procedures result in optimal standardization of routinely used 25(OH)D ID-LC-MS/MS methods. Clin. Chim. Acta Int. J. Clin. Chem. 2016, 462, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Hawkes, C.P.; Schnellbacher, S.; Singh, R.J.; Levine, M.A. 25-hydroxyvitamin D can interfere with a common assay for 1,25-dihydroxyvitamin D in vitamin D intoxication. J. Clin. Endocrinol. Metab. 2015, 100, 2883–2889. [Google Scholar] [CrossRef] [PubMed]
- Strathmann, F.G.; Laha, T.J.; Hoofnagle, A.N. Quantification of 1alpha,25-dihydroxy vitamin D by immunoextraction and liquid chromatography-tandem mass spectrometry. Clin. Chem. 2011, 57, 1279–1285. [Google Scholar] [CrossRef] [PubMed]
- Kimball, S.M.; Vieth, R. A comparison of automated methods for the quantitation of serum 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D. Clin. Biochem. 2007, 40, 1305–1310. [Google Scholar] [CrossRef] [PubMed]
- Zittermann, A.; Ernst, J.B.; Becker, T.; Dreier, J.; Knabbe, C.; Gummert, J.F.; Kuhn, J. Measurement of circulating 1,25-dihydroxyvitamin D: Comparison of an automated method with a liquid chromatography tandem mass spectrometry method. Int. J. Anal. Chem. 2016, 2016, 8501435. [Google Scholar] [CrossRef] [PubMed]
- Valcour, A.; Zierold, C.; Podgorski, A.L.; Olson, G.T.; Wall, J.V.; DeLuca, H.F.; Bonelli, F. A novel, fully-automated, chemiluminescent assay for the detection of 1,25-dihydroxyvitamin D in biological samples. J. Steroid Biochem. Mol. Biol. 2016, 164, 120–126. [Google Scholar] [CrossRef] [PubMed]
- Miller, N.; Gruson, D. Implementation of automated testing for 1,25-dihydroxyvitamin D: Return of experience from a core-laboratory. Clin. Biochem. 2016, 49, 298–301. [Google Scholar] [CrossRef] [PubMed]
- Pauwels, S.; Jans, I.; Billen, J.; Heijboer, A.; Verstuyf, A.; Carmeliet, G.; Mathieu, C.; Maestro, M.; Waelkens, E.; Evenepoel, P.; et al. 1beta,25-dihydroxyvitamin D3: A new vitamin d metabolite in human serum. J. Steroid Biochem. Mol. Biol. 2017, 173, 341–348. [Google Scholar] [CrossRef] [PubMed]
- Duan, X.; Weinstock-Guttman, B.; Wang, H.; Bang, E.; Li, J.; Ramanathan, M.; Qu, J. Ultrasensitive quantification of serum vitamin D metabolites using selective solid-phase extraction coupled to microflow liquid chromatography and isotope-dilution mass spectrometry. Anal. Chem. 2010, 82, 2488–2497. [Google Scholar] [CrossRef] [PubMed]
- Hedman, C.J.; Wiebe, D.A.; Dey, S.; Plath, J.; Kemnitz, J.W.; Ziegler, T.E. Development of a sensitive LC/MS/MS method for vitamin D metabolites: 1,25 dihydroxyvitamin D2&3 measurement using a novel derivatization agent. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2014, 953–954, 62–67. [Google Scholar]
- Wang, Z.; Senn, T.; Kalhorn, T.; Zheng, X.E.; Zheng, S.; Davis, C.L.; Hebert, M.F.; Lin, Y.S.; Thummel, K.E. Simultaneous measurement of plasma vitamin D(3) metabolites, including 4beta,25-dihydroxyvitamin D(3), using liquid chromatography-tandem mass spectrometry. Anal. Biochem. 2011, 418, 126–133. [Google Scholar] [CrossRef] [PubMed]
- Casetta, B.; Jans, I.; Billen, J.; Vanderschueren, D.; Bouillon, R. Development of a method for the quantification of 1alpha,25(OH)2-vitamin D3 in serum by liquid chromatography tandem mass spectrometry without derivatization. Eur. J. Mass Spectrom. 2010, 16, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Fang, H.; Yu, S.; Cheng, Q.; Cheng, X.; Han, J.; Qin, X.; Xia, L.; Jiang, X.; Qiu, L. Determination of 1,25-dihydroxyvitamin D2 and 1,25-dihydroxyvitamin D3 in human serum using liquid chromatography with tandem mass spectrometry. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2016, 1027, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Kissmeyer, A.M.; Sonne, K. Sensitive analysis of 1alpha,25-dihydroxyvitamin D3 in biological fluids by liquid chromatography-tandem mass spectrometry. J. Chromatogr. A 2001, 935, 93–103. [Google Scholar] [CrossRef]
- Yuan, C.; Kosewick, J.; He, X.; Kozak, M.; Wang, S. Sensitive measurement of serum 1alpha,25-dihydroxyvitamin D by liquid chromatography/tandem mass spectrometry after removing interference with immunoaffinity extraction. Rapid Commun. Mass Spectrom. 2011, 25, 1241–1249. [Google Scholar] [CrossRef] [PubMed]
- Tang, J.C.Y.; Nicholls, H.; Piec, I.; Washbourne, C.J.; Dutton, J.J.; Jackson, S.; Greeves, J.; Fraser, W.D. Reference intervals for serum 24,25-dihydroxyvitamin D and the ratio with 25-hydroxyvitamin D established using a newly developed LC–MS/MS method. J. Nutr. Biochem. 2017, 46, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Baecher, S.; Leinenbach, A.; Wright, J.A.; Pongratz, S.; Kobold, U.; Thiele, R. Simultaneous quantification of four vitamin D metabolites in human serum using high performance liquid chromatography tandem mass spectrometry for vitamin D profiling. Clin. Biochem. 2012, 45, 1491–1496. [Google Scholar] [CrossRef] [PubMed]
- Mena-Bravo, A.; Priego-Capote, F.; Luque de Castro, M.D. Study of blood collection and sample preparation for analysis of vitamin D and its metabolites by liquid chromatography-tandem mass spectrometry. Anal. Chim. Acta 2015, 879, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Tai, S.S.; Nelson, M.A. Candidate reference measurement procedure for the determination of (24R),25-dihydroxyvitamin D3 in human serum using isotope-dilution liquid chromatography-tandem mass spectrometry. Anal. Chem. 2015, 87, 7964–7970. [Google Scholar] [CrossRef] [PubMed]
- Wise, S.A.; Tai, S.S.; Nelson, M.A.; Burdette, C.Q.; Camara, J.E.; Hoofnagle, A.N.; Laha, T.J.; Carter, G.D.; Jones, J.; Williams, E.L.; et al. Interlaboratory comparison for the determination of 24,25-dihydroxyvitamin D(3) in human serum using liquid chromatography with tandem mass spectrometry. J. AOAC Int. 2017, 100, 1308–1317. [Google Scholar] [CrossRef] [PubMed]
- Groenestege, W.M.T.; Bui, H.N.; Kate, J.T.; Menheere, P.P.C.A.; Oosterhuis, W.P.; Vader, H.L.; Heijboer, A.C.; Janssen, M.J.W. Accuracy of first and second generation testosterone assays and improvement through sample extraction. Clin. Chem. 2012, 58, 1154–1156. [Google Scholar] [CrossRef] [PubMed]
| Metabolite | LC-MS/MS | Immunoassay | ||
|---|---|---|---|---|
| 25(OH)D | Advantages:
| Disadvantages:
| Advantages *:
| Disadvantages:
|
| 1,25(OH)2D | Advantages:
| Disadvantages:
| Advantages:
| Disadvantages:
|
| 24,25(OH)2D | Advantages:
| Disadvantages:
| N/A † | N/A † |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dirks, N.F.; Ackermans, M.T.; Lips, P.; De Jongh, R.T.; Vervloet, M.G.; De Jonge, R.; Heijboer, A.C. The When, What & How of Measuring Vitamin D Metabolism in Clinical Medicine. Nutrients 2018, 10, 482. https://doi.org/10.3390/nu10040482
Dirks NF, Ackermans MT, Lips P, De Jongh RT, Vervloet MG, De Jonge R, Heijboer AC. The When, What & How of Measuring Vitamin D Metabolism in Clinical Medicine. Nutrients. 2018; 10(4):482. https://doi.org/10.3390/nu10040482
Chicago/Turabian StyleDirks, Niek F., Mariëtte T. Ackermans, Paul Lips, Renate T. De Jongh, Marc G. Vervloet, Robert De Jonge, and Annemieke C. Heijboer. 2018. "The When, What & How of Measuring Vitamin D Metabolism in Clinical Medicine" Nutrients 10, no. 4: 482. https://doi.org/10.3390/nu10040482
APA StyleDirks, N. F., Ackermans, M. T., Lips, P., De Jongh, R. T., Vervloet, M. G., De Jonge, R., & Heijboer, A. C. (2018). The When, What & How of Measuring Vitamin D Metabolism in Clinical Medicine. Nutrients, 10(4), 482. https://doi.org/10.3390/nu10040482





