Abstract
Obesity is one of the world’s most serious health issues. Therefore, therapists have looked for methods to fight obesity. Currently, technology-based intervention options in medical settings are very common. One such technology is virtual reality (VR) which has been used in the treatment of obesity since the late 1990s. The main objective of this study is to review the literature on the use of VR in the treatment of obesity and overweight to better understand the role of VR-based interventions in this field. To this end, four databases (PubMed, Medline, Scopus, and Web of Science) were searched for related publications from 2000 to 2022 using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). From the 645 articles identified, 24 were selected. The main strength of this study is that it is the first systematic review to focus completely on the use of VR in the treatment of obesity. It includes most research in which VR was utilized to carry out the intervention. Although several limitations were detected in the reviewed studies, the findings of this review suggest that employing VR for self-monitoring of diet, physical activity, and/or weight is effective in supporting weight loss as well as improving satisfaction of body image and promoting health self-efficacy in overweight or obese persons.
1. Introduction
Obesity is one of the world’s most serious health issues. There has been a substantial increase in the prevalence of obesity in recent decades and it is now considered a global epidemic [1]. Over two billion adults around the world are overweight or at high risk of becoming obese, with over 650 million obese individuals worldwide in 2020 [2]. Since 1975, the global obesity rate has almost tripled [3]. Between 1975 and 2014, the prevalence of obesity in adult men increased from 3.2 to 10.8% and in adult women increased from 6.4 to 14.9% [4]. Owing to its widespread prevalence, obesity is regarded as one of the most serious health issues in both developed and developing countries and regarded as a chronic and progressive disease with high morbidity and mortality rates [5,6,7]. Moreover, obesity can lower an individual’s quality of life and put them at risk for serious chronic conditions, such as heart disease, type 2 diabetes, and cancer [8,9,10].
As the first line for obesity treatment, behavioral lifestyle intervention (BLI) is recommended by therapists since it consistently results in clinically substantial weight loss [11]. BLI enhances weight loss by improving patterns of diet and physical activity through a number of behavioral strategies, such as self-monitoring, goal setting, stimulus control, problem-solving, and self-reinforcement [12]. Although BLI has been shown to be effective in clinical trials, it has not been widely used due to its prohibitive costs, as treatment often entails group or individual therapy sessions led by specialized trainers over a period of many weeks or months [12,13].
Given the limits of BLI, new intervention approaches based on technological potential have been created to improve the scalability, reach, and affordability of BLI [14,15,16]. Virtual reality (VR) is one of many appealing technologies now available to assist individuals to lose weight [13]. VR is a computer-created enhanced human–computer interface that creates a virtual environment and enables users to traverse and interact with it as if they were in another world. It is accomplished by fully immersing the user’s senses through the use of high-performance computers and sensory equipment such as headsets, position trackers, and other tools [17]. VR is effective in terms of motivating emotional feelings, changing behavior, and changing lifestyle, thereby making it more appropriate for healthcare applications [17,18].
VR allows for the construction of virtual scenarios that are quite similar to those in the real world [19]. This enables for precise control of situational aspects while preserving ecological validity [20]. VR also provides a safe and adaptable setting in which individuals can approach frightening events at their own speed, lessening their resistance to exposure [21]. Other benefits include the ability to self-train and the ability for therapists to conduct treatments that are impossible or extremely difficult to implement in real-life situations [20]. Furthermore, VR is far more immersive than images exposure because it engages many sensory modalities (auditory, visual, and sensory) [22]. This makes it good choice for individuals who have trouble imagining scenes and allows them to be more emotionally involved [21].
VR has been used in the treatment of obesity since the late 1990s. Riva and his team were the most researched on this topic [23]. The increased scientific interest in finding novel therapy alternatives for obesity combined with the rapid technological advancement in the VR field has resulted in breakthrough VR-based applications for evaluating and treating obesity. The use of avatars is one of the most recent technological developments [24,25,26,27]. VR has been used to treat obesity by immersing patients in realistic avatars in stressful virtual scenarios, such as grocery shopping, which helps patients improve body image perceptions and encourage healthier habits [28]. The so-called Proteus effect, a phenomenon in which individuals are more likely to perform a certain behavior when they see an avatar of themselves performing that behavior in a virtual environment, has led to more interest in using VR to encourage healthy eating behavior [29,30,31]. New discoveries regarding the multimodal nature of body representations have resulted in the invention of novel protocols, such as “bodily illusions” [32]. Additionally, recent studies have focused on improving the outcomes of weight management commercial online programs [33] and the immersion of participants in a more realistic representation of space and narrative [34]. Due to the growing popularity of mobile devices, new VR-enabled dieting apps have also been developed [35,36].
The main objective of this study is to review the literature on the use of VR in the treatment of obesity and overweight to better understand the role of VR-based interventions in this field. It must be highlighted that the goal is not to examine every study that has employed VR to alter weight or a weight-related behavior. Instead, various novel techniques are presented and analyzed in the context of current clinical practice and future objectives. Furthermore, this review adds to the growing body of knowledge regarding VR in medical settings and helps in the development of new methodologies that include VR technologies.
2. Materials and Methods
The PRISMA guidelines were utilized to guide the review’s conduct. PRISMA consists of a 27-item checklist intended to facilitate the preparation and reporting of a robust protocol for the systematic review [37]. We used PRISMA to identify, select, and critically appraise relevant research while minimizing bias in order to optimize the quality of reporting and make the peer review process more efficient. Using the PRISMA statement, we conducted a search to identify studies using VR in the assessment and treatment of overweight and obesity. Study selection and data extraction were carried out by two independent reviewers. The reviewers′ decision to include or exclude studies were recorded. Following the completion of the article review, the outcomes of the data abstraction were compared. Any conflicts or discrepancies were addressed by consensus, taking into account the defined selection criteria. In the event of a persistent disagreement between the reviewers, a third reviewer would decide on inclusion or exclusion. The article’s full text was then retrieved, and its quality assessed in order to determine whether it was appropriate to include in the review. Finally, tables were created to organize the essential points of the selected articles.
2.1. Data Collection
The scope of this study was limited to electronic databases. PubMed, Medline, Scopus, and Web of Science were used as data sources [38]. These sources were selected because they were considered relevant to weight loss, health interventions, and digital technologies. Searches were limited to studies published from 2000 to January 2022 because before the year 2000, VR research was rather limited. Furthermore, we utilized the English language for the search phrases. Additional articles were discovered by looking through the references of some articles founded in the search results.
2.2. Search Terms
The terminology employed in the search was pertaining to the use of VR in the treatment of overweight and obese patients. To guarantee that all studies satisfying the inclusion criteria were found, broad search phrases were utilized. The search string was created by combining key terms that best matched the study goal, which resulted in the following search terms: ((virtual reality AND obesity) OR (virtual reality AND overweight) OR (virtual reality AND weight loss) OR (virtual environment AND obesity) OR (virtual environment AND overweight) OR (virtual environment AND weight loss) OR (virtual world AND obesity) OR (virtual world AND overweight) OR (virtual world AND weight loss)).
2.3. Inclusion/Exclusion Criteria
The following aspects were the inclusion criteria of this study: (i) full-text publications written in English; (ii) articles with participants aged 18 or older, overweight or obese; and (iii) articles having protocols for VR intervention to treat obesity along with associated results.
The following aspects were the exclusion criteria of this study: (i) papers not connected to the study’s subject or protocols of intervention with no results; (ii) reviews or meta-analyses; (iii) documents that are book chapters; and (iv) the presence of serious pathologies not related to obesity, such as mental illnesses and cancer.
2.4. Quality Assessment and Data Extraction
Two authors independently performed quality assessment of the included studies concurrently with data extraction. The data extracted from the articles include the year of publication (2000–2022), country of origin, participants’ mean age, participants’ mean weight, sample size, objective of the study, study type, duration of the intervention, number of groups in the study, technologies used in weight loss and/or the design of weight maintenance programs, and weight changes and other related intervention outcomes (such as improving self-efficacy for diet and physical activity). To critically evaluate the quality of selected studies, we used an adapted version of the Newcastle–Ottawa Quality Assessment Scale [39]. Each study is given a maximum of nine points on this scale. Studies with a score of less than 6 are considered low-quality studies, whereas those with a score of 6 or more are considered high-quality studies and were therefore included in the review.
3. Results
Figure 1 depicts the study selection procedure. After a preliminary electronic search, we found 1151 studies that used VR-based environments in overweight or obese patients. In addition, hand-searching the references in the original and review papers yielded 22 research papers. We deleted 528 items due to duplication and then eliminated 587 items after reviewing their titles and abstracts. The remaining 58 articles were downloaded for a full-text review, after which we eliminated another 34 articles: ten articles presented a protocol without results, five articles reported previous studies, five articles evaluated healthy-weight participants, four articles did not target adults, three articles did not exist, three articles described non-VR intervention, two articles were book chapters, one article reported studies already included, and one study reported preliminary data. The resulting set of 24 distinct studies that matched the inclusion criteria were analyzed. Table 1 lists the articles included in this review and Table 2 explains the characteristics and results of the studies included.
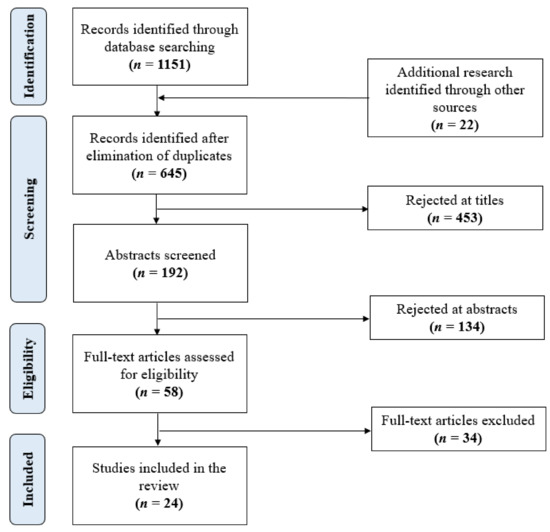
Figure 1.
PRISMA flow diagram of study selection.

Table 1.
List of studies included in the review.

Table 2.
Characteristics and results of the examined studies.
3.1. Study Authors, Year of Publication, and Country of Origin
There was a total of 24 articles included in this review. Riva and his team were the most researched on this topic (10/24, 42%). To the best of our knowledge, there is no single review dedicated to using VR in the treatment of obesity. However, there are a few reviews that included this topic, such as [21], which included articles that were published up to 2013 and reported six studies on obesity. Since then, 18 (75%) of the articles in our selection have been published, thereby indicating an increase in interest in using VR for obese patients (Figure 2). All articles were in English and were published between 2000 and 2021. Most trials were conducted in Europe and the USA.
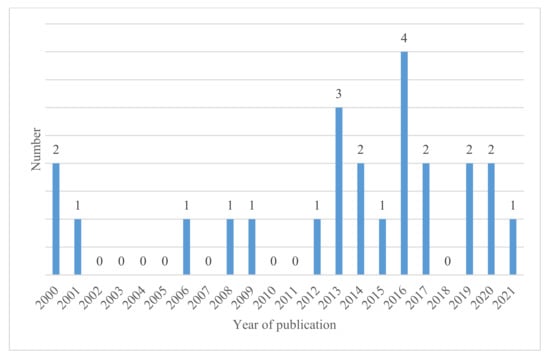
Figure 2.
The number of articles included in the review by year of publication.
3.2. Population, Sample Size, and Study Type
In total, more than 1493 people participated in the 24 trials. There were 15 trials that had only women, and 1 trial in which there were only men. In the remaining eight studies, there were both men and women. Approximately 93% of the participants were women, whereas only 7% were men. All the trials were conducted on adults. The average age of the participants was between 18 and 79 years. The majority of the inclusion criteria were based on body mass index (BMI). The review study participants had a BMI of at least 25 kg/m2. Further, in terms of study methodology, there were 11 randomized controlled studies, 2 clinical case studies, and 11 studies had a variety of other study designs.
3.3. Objectives of the Studies
The studies included in this review focused mostly on exposure to psychological, diet, or physical activity as virtual stimuli to promote behavioral weight loss treatment. The most commonly utilized verbs in study objectives statements were “evaluate” (n = 4), “examine” (n = 4), and “describe” (n = 4). Researchers also used “investigate” (n = 2), “test” (n = 2), or “compare” (n = 2). The majority of studies were centered on the participants’ weight loss (n = 14) and/or on experiences related to certain phenomena related to weight loss (n = 10).
3.4. Technology Used
To provide a greater sense of immersion, isolation, and possible vulnerability, half of the trials used visual immersive technology with a head-mounted display (HMD) and voice communication (12/24, 50%). A total of 11 studies used audio and visual stimuli via PC or mobile device and headsets to enable interaction between the user and the virtual world (11/24, 46%). One more study used a motion sensing input device with RGB cameras and infrared projectors and detectors (1/24, 4%). Motion sensors are used to measure the movement of the participants in order to motivate them.
3.5. Outcomes
The most important findings from the articles studied indicate that patients’ weight loss was greater in the VR intervention groups, although the differences between the control and comparison groups were not statistically significant. However, this result cannot be generalized for weight maintenance, as most studies have not addressed this issue. In addition to weight loss, there were interesting weight-loss related results. For example, the effectiveness of VR in the development of health self-efficacy, body image satisfaction, and motivation to change has been demonstrated.
4. Discussion
This systematic review of the use of VR-based settings in the treatment of overweight and obese people complemented previous reviews [21,35,57,58] by focusing solely on weight management in overweight and obese people and including more recent research in the field. From the 24 studies selected, 14 were classified as treatment studies because they investigated the utility of VR as a potential therapeutic strategy for weight loss, and 10 studies were classified as assessment studies because they investigated the impact of VR on various obesity-related aspects. Based on the papers reviewed, the use of VR in the treatment of overweight and obese people is still a developing field that requires additional research.
This review can lead to a number of inferences. First, the findings support the hypothesis that patients with overweight and obesity who were immersed in VR environments had a sense of presence, thereby enhancing the ecological validity of the processes in this group of individuals. Second, the findings imply that using VR technology for monitoring diet, physical activity, and/or weight can help individuals who are overweight or obese to lose weight. Third, studies involving VR technologies in conjunction with cognitive behavioral procedures or behavioral weight loss interventions reveal that they have the potential to enhance clinically significant weight loss; however, regaining weight is a problem, and a substantial percentage of participants do not maintain their weight loss over time [34,59]. Finally, commercial online weight loss programs have emerged as a potentially cost-effective alternative to standard empirically validated behavioral weight-loss programs, which differ greatly in terms of the extent to which they combine evidence-based weight loss methods and skills [60].
In fact, even though the quality of studies included in this review was moderate to high, on average, the different types of interventions and time durations of the interventions as well as the different study designs made it impractical to have a direct comparison of outcomes. However, the evidence suggests that weight loss was greater in groups in which VR was used as part of or as a complement to the intervention [24,25,26,27,33,34,41,42,45,46,48,49,50,54], even if in certain studies the differences between the control and comparison groups were not statistically significant. Nevertheless, this cannot be affirmed with regard to weight maintenance because most studies did not include this outcome. In addition to weight loss, there were interesting weight loss-related results. For example, the effectiveness of VR in improving health self-efficacy, body image satisfaction, and motivation to change has been proved.
Although VR treatment has a few advantages over reality, its goal is not to replace actual experiences but to serve as a substitute for fictitious exposure. VR exposure has the ability to overcome the limits of traditional behavioral weight loss by enabling users to engage in desired weight management activities with the frequency and intensity required to form long-term habits. The evidence presented in this systematic review suggests that using VR combined with low-calorie meals and exercise could help individuals lose weight and feel satisfied about themselves while also lowering anxiety and emotional eating [61]. Furthermore, in the VR exposure condition, exposures can be specifically adjusted by the therapist, which can assist patients to cope with stimuli or complex surroundings in a more practical and controlled manner. The ability to monitor the patient’s responses is also a benefit over actual exposure [62]. Moreover, it has already been reported that patients may go through their VR exposure hierarchy more quickly due to a sense of improved control and safety [63]. Additionally, VR exposure can aid to disrupt the reconsolidation of negative food/situation memories by reducing the anxiety associated with eating during and after exposure to virtual meals and surroundings [64]. Apart from these benefits, these VR-based devices are affordable and have a strong cost–effectiveness ratio [65].
The increased scientific interest in finding novel therapy alternatives for obesity combined with the rapid technological advancement in the VR field has resulted in breakthrough VR-based applications for evaluating and treating obesity. The use of avatars is one of the most recent technological developments. Therapists employed realistic “avatars” of their patients as a first step in the treatment of obesity because many obese persons have a distorted perspective of their own body, which makes therapy more difficult. The findings of this review imply that incorporating avatar technology into weight reduction therapies results in more weight loss and weight maintenance than standard interventions; however, the differences are not statistically or clinically significant [24,25,26,27]. Moreover, avatar personalization may provide a few extra benefits by engaging and maintaining interest and motivation to adhere to a predetermined weight loss program, but the evidence for this is limited [24,48]. Further, discoveries made recently regarding the multimodal nature of body representations have resulted in the invention of novel protocols, such as “bodily illusions.” Research on body ownership illusions has recently shifted from the embodiment of a single body part (such as the hand [66,67] or the foot [68]) to the full body. Scarpina et al. (2017) were the first to employ the full body illusion in obese patients [32]. They compared the effects of illusionary ownership over a slim virtual body (i.e., the VR-FBI) on body images in a group of obese people with a group of healthy people. Their studies demonstrated that obese people can effectively experience illusory ownership over a full virtual body, with possible modifications in hip circumference measurement. Consequently, VR-FBI could be a viable tool for use in rehabilitative settings, including obesity [32]. Recent studies have also focused on improving the outcomes of weight management commercial online programs [33] and the immersion of participants in a more realistic representation of space and narrative [34].
One of the important observations that draws attention in this study is the weak participation of males in studies included in this review. This is in accordance with a review study of the management of obesity in males, which indicated that men were less likely than women to participate in mixed-gender weight loss programs [69]. While the reason for women’s appetite for weight loss programs appears to be the social pressures they are exposed to, the reasons behind the recruitment gender polarization remains unclear and merit further exploration [69].
It goes without saying that the most important key to the success of weight loss interventions is adherence. However, the common problems that face all weight loss programs are attrition and non-adherence. Attrition in weight loss programs reported rates ranging from 10% to over 80% [70]. It is noted that reasonable recruitment and attrition rates were attained in the studies included in this review. This is inconsistent with another review that suggests a general interest and acceptability of VR as a weight loss tool [57].
The main strength of this study is that it is the first systematic review to focus completely on the use of virtual reality in the treatment of obesity. It includes most research in which VR was utilized to carry out the intervention. However, it has some limitations. First, the vast range of study designs included in this review limits the conclusions that can be drawn. Second, the search was limited to English-language publications, which may not have incorporated all available studies. Third, the time periods of the intervention were heterogeneous, as were the sample sizes, which may have influenced the strength of outcomes and conclusions. Future research could build on these constraints to figure out the best way to use virtual reality in clinical settings to cure obesity.
Although VR for weight loss will undoubtedly continue to advance at a rapid pace in the coming years, the time and price required to perform these trials imply that the results will frequently not be available until the next generation of technology is ready. Nonetheless, it is critical that this research continues, as there are valuable lessons to be learned about how VR may be utilized to help people lose weight that can be applied to a number of intervention platforms.
5. Conclusions
As the studies in this review demonstrate, virtual reality technology has the potential to be used to assess and treat obesity. Virtual reality has a lot of potential benefits: it is highly interactive, flexible, tailored to the individual, and it fits well with established psychological theory and practice. The evidence that people react to virtual worlds as if they were real is compelling, and patients are generally accepting of the technology. Studies reveal that VR technologies have the potential to promote clinically significant weight loss when used in conjunction with cognitive behavioral procedures or behavioral weight loss therapies; nevertheless, regaining weight is yet a challenge.
The use of VR in the treatment of overweight and obese people is still a developing field that requires additional research. Future research should include more high-quality randomized control trials, with large sample numbers and long-term follow-ups to investigate deeply the effects of VR-based interventions on obesity. Upcoming research should also compare VR-based interventions in more homogenous groups of obese patients with healthy subjects.
Author Contributions
Conceptualization, W.A. and M.D.L.; methodology, A.A.-R.; validation, E.A.; formal analysis, A.A.-R.; investigation, M.A. (Mai Alduailij) and M.A. (Mona Alduailij); resources, S.A.; data curation, S.A.; writing—original draft preparation, A.A.-R.; writing—review and editing, E.A., M.A. (Mai Alduailij) and M.A. (Mona Alduailij); visualization, E.A. and M.A. (Mona Alduailij); supervision, M.D.L.; project administration, W.A.; funding acquisition, M.A. (Mona Alduailij). All authors have read and agreed to the published version of the manuscript.
Funding
This work was funded by the Deanship of Scientific Research at Princess Nourah Bint Abdulrahman University through the Research Groups Program Grant no. (RGP-1440-0026).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data is contained within the article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Haththotuwa, R.N.; Wijeyaratne, C.N.; Senarath, U. Worldwide epidemic of obesity. In Obesity and Obstetrics; Elsevier: Amsterdam, The Netherlands, 2020; pp. 3–8. [Google Scholar]
- Mqnsia BIOTECH. Obesity and Diabetes in the World. Available online: https://www.a-mansia.com/obesity-and-diabetes-in-the-world/ (accessed on 5 February 2021).
- World Health Organization. Obesity and Overweight. 2021. Available online: http://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 28 June 2021).
- Blüher, M. Obesity: Global epidemiology and pathogenesis. Nat. Rev. Endocrinol. 2019, 15, 288–298. [Google Scholar] [CrossRef] [PubMed]
- Agha, M.; Agha, R. The rising prevalence of obesity: Part B—Public health policy solutions. Int. J. Surg. Oncol. 2017, 2, e19. [Google Scholar] [CrossRef] [PubMed]
- Abdelaal, M.; Le Roux, C.W.; Docherty, N. Morbidity and mortality associated with obesity. Ann. Transl. Med. 2017, 5, 161. [Google Scholar] [CrossRef]
- Hill, J.O.; Peters, J.C. Environmental contributions to the obesity epidemic. Science 1998, 280, 1371–1374. [Google Scholar] [CrossRef] [PubMed]
- Malik, V.S.; Popkin, B.M.; Bray, A.G.; Després, J.-P.; Frank, B.H. Sugar-sweetened beverages, obesity, type 2 diabetes mellitus, and cardiovascular disease risk. Circulation 2010, 121, 1356–1364. [Google Scholar] [CrossRef]
- Popkin, B.M. Urbanization, lifestyle changes and the nutrition transition. World Dev. 1999, 27, 1905–1916. [Google Scholar] [CrossRef]
- Raziani, Y.; Raziani, S. Investigating the predictors of overweight and obesity in children. Int. J. Adv. Stud. Humanit. Soc. Sci. 2020, 9, 262–280. [Google Scholar]
- LeBlanc, E.S.; Patnode, C.D.; Webber, E.M.; Redmond, N.; Rushkin, M.; O’Connor, E.A. Behavioral and pharmacotherapy weight loss interventions to prevent obesity-related morbidity and mortality in adults: Updated evidence repevidence report and systematic review for the US Preventive Services Task Force. JAMA 2018, 320, 1172–1191. [Google Scholar] [CrossRef]
- Wadden, T.A.; Tronieri, J.S.; Butryn, M.L. Lifestyle modification approaches for the treatment of obesity in adults. Am. Psychol. 2020, 75, 235–251. [Google Scholar] [CrossRef]
- Gorini, A.; Gaggioli, A.; Vigna, C.; Riva, G. A second life for eHealth: Prospects for the use of 3-D virtual worlds in clinical psychology. J. Med. Internet Res. 2008, 10, e21. [Google Scholar] [CrossRef]
- Thomas, J.G.; Goldstein, C.M.; Bond, D.S.; Lillis, J.; Hekler, E.B.; Emerson, J.A.; Espel-Huynh, H.M.; Goldstein, S.P.; Dunsiger, S.I.; Evans, E.W.; et al. Evaluation of intervention components to maximize outcomes of behavioral obesity treatment delivered online: A factorial experiment following the multiphase optimization strategy framework. Contemp. Clin. Trials 2021, 100, 106217. [Google Scholar] [CrossRef] [PubMed]
- Topol, E.J.; Hill, D. The Creative Destruction of Medicine: How the Digital Revolution Will Create Better Health Care; Basic Books: New York, NY, USA, 2012. [Google Scholar]
- Meskó, B.; Drobni, Z.D.; Bényei, É.; Gergely, B.; Győrffy, Z. Digital health is a cultural transformation of traditional healthcare. mHealth 2017, 3, 38. [Google Scholar] [CrossRef] [PubMed]
- Riva, G.; Gaggioli, A. Virtual clinical therapy. In Digital Human Modeling; Springer: Berlin/Heidelberg, Germany, 2008; pp. 90–107. [Google Scholar]
- Pillai, A.S.; Mathew, P.S. Impact of virtual reality in healthcare: A review. In Virtual and Augmented Reality in Mental Health Treatment; IGI Global: Hershey, PA, USA, 2019; pp. 17–31. [Google Scholar]
- Kohler, T.; Matzler, K.; Füller, J. Avatar-based innovation: Using virtual worlds for real-world innovation. Technovation 2009, 29, 395–407. [Google Scholar] [CrossRef]
- Mantovani, F.; Castelnuovo, G.; Gaggioli, A.; Riva, G. Virtual reality training for health-care professionals. CyberPsychol. Behav. 2003, 6, 389–395. [Google Scholar] [CrossRef] [PubMed]
- Ferrer-Garcia, M.; Gutiérrez-Maldonado, J.; Riva, G. Virtual reality based treatments in eating disorders and obesity: A review. J. Contemp. Psychother. 2013, 43, 207–221. [Google Scholar] [CrossRef]
- Slater, M.; Lotto, B.; Arnold, M.M.; Sánchez-Vives, M.V. How we experience immersive virtual environments: The concept of presence and its measurement. Anu. Psicol. 2009, 40, 193–210. [Google Scholar]
- Riva, G.; Malighetti, C.; Serino, S. Virtual reality in the treatment of eating disorders. Clin. Psychol. Psychother. 2021, 28, 477–488. [Google Scholar] [CrossRef]
- Ossolinski, G.; Jiwa, M.; McManus, A.; Parsons, R. Do images of a personalised future body shape help with weight loss? A randomised controlled study. Trials 2017, 18, 1. [Google Scholar] [CrossRef]
- Behm-Morawitz, E.; Lewallen, J.; Choi, G. A second chance at health: How a 3D virtual world can improve health self-efficacy for weight loss management among adults. Cyberpsychol. Behav. Soc. Netw. 2016, 19, 74–79. [Google Scholar] [CrossRef]
- Manzoni, G.M.; Cesa, G.L.; Bacchetta, M.; Castelnuovo, G.; Conti, S.; Gaggioli, A.; Mantovani, F.; Molinari, E.; Cárdenas-López, G.; Riva, G. Virtual reality–enhanced cognitive–behavioral therapy for morbid obesity: A randomized controlled study with 1 year follow-up. Cyberpsychol. Behav. Soc. Netw. 2016, 19, 134–140. [Google Scholar] [CrossRef]
- Cesa, G.L.; Manzoni, G.M.; Bacchetta, M.; Castelnuovo, G.; Conti, S.; Gaggioli, A.; Mantovani, F.; Molinari, E.; Cárdenas-López, G.; Riva, G. Virtual reality for enhancing the cognitive behavioral treatment of obesity with binge eating disorder: Randomized controlled study with one-year follow-up. J. Med. Internet Res. 2013, 15, e113. [Google Scholar] [CrossRef] [PubMed]
- Wiederhold, B.K. The Potential for Virtual Reality to Improve Health Care; The Virtual Reality Medical Centre (VRMC): San Diego, CA, USA, 2006. [Google Scholar]
- Boulos, M.N.K.; Hetherington, L.; Wheeler, S. Second Life: An overview of the potential of 3-D virtual worlds in medical and health education. Health Inf. Libr. J. 2007, 24, 233–245. [Google Scholar] [CrossRef] [PubMed]
- Alturki, R.; Gay, V. Augmented and virtual reality in mobile fitness applications: A survey. In Applications of Intelligent Technologies in Healthcare; Springer: Cham, Switzerland, 2019; pp. 67–75. [Google Scholar] [CrossRef]
- Heide, V.D.; Brandon, E.M.S.; Peterson, A.M.; Jones, E.B. The Proteus effect in dyadic communication: Examining the effect of avatar appearance in computer-mediated dyadic interaction. Commun. Res. 2013, 40, 838–860. [Google Scholar] [CrossRef]
- Scarpina, F.; Serino, S.; Keizer, A.; Chirico, A.; Scacchi, M.; Castelnuovo, G.; Mauro, A.; Riva, G. The effect of a virtual-reality full-body illusion on body representation in obesity. J. Clin. Med. 2019, 8, 1330. [Google Scholar] [CrossRef] [PubMed]
- Thomas, J.G.; Goldstein, C.M.; Bond, D.S.; Hadley, W.; Tuerk, P.W. Web-based virtual reality to enhance behavioural skills training and weight loss in a commercial online weight management programme: The Experience Success randomized trial. Obes. Sci. Pract. 2020, 6, 587–595. [Google Scholar] [CrossRef]
- Phelan, S.; Peruvemba, S.; Levinson, D.; Stulberg, N.; Lacy, A.; Legato, M.; Werner, J.P. Feasibility of a virtual reality-based approach to improve behavioral weight management outcomes. Pilot Feasibility Stud. 2021, 7, 129. [Google Scholar] [CrossRef] [PubMed]
- Thomas, J.G.; Bond, D.S. Review of innovations in digital health technology to promote weight control. Curr. Diabetes Rep. 2014, 14, 485. [Google Scholar] [CrossRef]
- Tufano, J.T.; Karras, B.T.; Buchan, I. Mobile eHealth interventions for obesity: A timely opportunity to leverage convergence trends. J. Med. Internet Res. 2005, 7, e58. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef]
- Bramer, W.M.; Rethlefsen, M.L.; Kleijnen, J.; Franco, O.H. Optimal database combinations for literature searches in systematic reviews: A prospective exploratory study. Syst. Rev. 2017, 6, 245. [Google Scholar] [CrossRef]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses; Ottawa Hospital Research Institute: Ottawa, ON, Canada, 2011; pp. 1–12. [Google Scholar]
- Navarro, J.; Cebolla, A.; Llorens, R.; Borrego, A.; Baños, R.M. Manipulating self-avatar body dimensions in virtual worlds to complement an internet-delivered intervention to increase physical activity in overweight women. Int. J. Environ. Res. Public Health 2020, 17, 4045. [Google Scholar] [CrossRef] [PubMed]
- Nosek, M.A.; Robinson-Whelen, S.; Ledoux, T.A.; Hughes, R.B.; O’Connor, D.P.; Lee, R.E.; Goe, R.; Silveira, S.L.; Markley, R.; Nosek, T.M.; et al. A pilot test of the GoWoman weight management intervention for women with mobility impairments in the online virtual world of Second Life®. Disabil. Rehabilit. 2019, 41, 2718–2729. [Google Scholar] [CrossRef] [PubMed]
- Sgobbi, F.S.; Tarouco, L.M.R.; Reategui, E.B. The pedagogical use of the Internet of Things in virtual worlds to encourage a behavior change in obese individuals. In Proceedings of the 2017 IEEE International Conference on Internet of Things (iThings) and IEEE Green Computing and Communications (GreenCom) and IEEE Cyber, Physical and Social Computing (CPSCom) and IEEE Smart Data (SmartData), Exeter, UK, 21–23 June 2017. [Google Scholar]
- Perpiñá, C.; Roncero, M. Similarities and differences between eating disorders and obese patients in a virtual environment for normalizing eating patterns. Compr. Psychiatry 2016, 67, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Serino, S.; Scarpina, F.; Keizer, A.; Pedroli, E.; Dakanalis, A.; Castelnuovo, G.; Chirico, A.; Novelli, M.; Gaudio, S.; Riva, G. A novel technique for improving bodily experience in a non-operable super–super obesity case. Front. Psychol. 2016, 7, 837. [Google Scholar] [CrossRef] [PubMed]
- Lopez, G.C.; Martinez, P.; Riva, G.; Duran-Baca, X.; Torres, G. Virtual reality environments as auxiliaries in the treatment of obesity. In Proceedings of the 2015 Virtual Reality International Conference, Laval, France, 8–10 April 2015. [Google Scholar] [CrossRef]
- Lopez, G.C.; Torres-Villalobos, G.; Martinez, P.; Carreño, V.; Duran, X.; Dakanalis, A.; Gaggioli, A.; Riva, G. Virtual reality for improving body image disorders and weight loss after gastric band surgery: A case series. In Medicine Meets Virtual Reality 21; IOS Press: Amsterdam, The Netherlands, 2014; pp. 43–47. [Google Scholar]
- Thomas, J.G.; Spitalnick, J.S.; Hadley, W.; Bond, D.S.; Wing, R.R. Development of and feedback on a fully automated virtual reality system for online training in weight management skills. J. Diabetes Sci. Technol. 2014, 9, 145–148. [Google Scholar] [CrossRef]
- Napolitano, M.A.; Hayes, S.; Russo, G.; Muresu, D.; Giordano, A.; Foster, G.D. Using avatars to model weight loss behaviors: Participant attitudes and technology development. J. Diabetes Sci. Technol. 2013, 7, 1057–1065. [Google Scholar] [CrossRef]
- Sullivan, D.K.; Goetz, J.R.; Gibson, C.A.; Washburn, R.A.; Smith, B.K.; Lee, J.; Gerald, S.; Fincham, T.; Donnelly, J.E. Improving weight maintenance using virtual reality (second life). J. Nutr. Educ. Behav. 2013, 45, 264–268. [Google Scholar] [CrossRef]
- Johnston, J.D.; Massey, A.P.; DeVaneaux, C. Innovation in weight loss intervention programs: An examination of a 3D virtual world approach. In Proceedings of the 2012 45th Hawaii International Conference on System Sciences, Maui, HI, USA, 4–7 January 2012. [Google Scholar] [CrossRef]
- Manzoni, G.M.; Pagnini, F.; Gorini, A.; Preziosa, A.; Castelnuovo, G.; Molinari, E.; Riva, G. Can relaxation training reduce emotional eating in women with obesity? An exploratory study with 3 months of follow-up. J. Am. Diet. Assoc. 2009, 109, 1427–1432. [Google Scholar] [CrossRef]
- Manzoni, G.M.; Gorini, A.; Preziosa, A.; Pagnini, F.; Castelnuovo, G.; Molinari, E.; Riva, G. New technologies and relaxation: An explorative study on obese patients with emotional eating. J. Cyberther. Rehabilit. 2008, 1, 182–192. [Google Scholar]
- Riva, G.; Bacchetta, M.; Cesa, G.; Conti, S.; Castelnuovo, G.; Mantovani, F.; Molinari, E. Is severe obesity a form of addiction?: Rationale, clinical approach, and controlled clinical trial. Cyberpsychol. Behav. 2006, 9, 457–479. [Google Scholar] [CrossRef]
- Riva, G.; Bacchetta, M.; Baruffi, M.; Molinari, E. Virtual Reality–based multidimensional therapy for the treatment of body image disturbances in obesity: A controlled study. CyberPsychol. Behav. 2001, 4, 511–526. [Google Scholar] [CrossRef] [PubMed]
- Riva, G.; Bacchetta, M.; Baruffi, M.; Cirillo, G.; Molinari, E. Virtual reality environment for body image modification: A multidimensional therapy for the treatment of body image in obesity and related pathologies. CyberPsychol. Behav. 2000, 3, 421–431. [Google Scholar] [CrossRef]
- Riva, G.; Bacchetta, M.; Baruffi, M.; Rinaldi, S.; Vincelli, F.; Molinari, E. Virtual reality-based experiential cognitive treatment of obesity and binge-eating disorders. Clin. Psychol. Psychother. 2000, 7, 209–219. [Google Scholar] [CrossRef]
- Horne, M.; Hill, A.; Murells, T.; Ugail, H.; Irving; Chinnadorai, R.; Hardy, M. Using avatars in weight management settings: A systematic review. Internet Interv. 2020, 19, 100295. [Google Scholar] [CrossRef] [PubMed]
- Rumbo-Rodríguez, L.; Sánchez-SanSegundo, M.; Ruiz-Robledillo, N.; Albaladejo-Blázquez, N.; Ferrer-Cascales, R.; Zaragoza-Martí, A. Use of technology-based interventions in the treatment of patients with overweight and obesity: A systematic review. Nutrients 2020, 12, 3634. [Google Scholar] [CrossRef]
- Castelnuovo, G.; Pietrabissa, G.; Manzoni, G.M.; Cattivelli, R.; Rossi, A.; Novelli, M.; Varallo, G.; Molinari, E. Cognitive behavioral therapy to aid weight loss in obese patients: Current perspectives. Psychol. Res. Behav. Manag. 2017, 10, 165–173. [Google Scholar] [CrossRef]
- Bardus, M.; van Beurden, S.B.; Smith, J.R.; Abraham, C. A review and content analysis of engagement, functionality, aesthetics, information quality, and change techniques in the most popular commercial apps for weight management. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 35. [Google Scholar] [CrossRef]
- Dascal, J.; Reid, M.; Ishak, W.W.; Spiegel, B.; Recacho, J.; Rosen, B.; Danovitch, I. Virtual reality and medical inpatients: A systematic review of randomized, controlled trials. Innov. Clin. Neurosci. 2017, 14, 14. [Google Scholar]
- Kuo, H.-C.; Lee, C.-C.; Chiou, W.-B. The power of the virtual ideal self in weight control: Weight-reduced avatars can enhance the tendency to delay gratification and regulate dietary practices. Cyberpsychol. Behav. Soc. Netw. 2016, 19, 80–85. [Google Scholar] [CrossRef]
- Matsangidou, M.; Otkhmezuri, B.; Ang, C.S.; Avraamides, M.; Riva, G.; Gaggioli, A.; Iosif, D.; Karekla, M. “Now I can see me” designing a multi-user virtual reality remote psychotherapy for body weight and shape concerns. Hum.-Comput. Interact. 2020, 1–27. [Google Scholar] [CrossRef]
- Young, K.S.; Rennalls, S.J.; Leppanen, J.; Mataix-Cols, D.; Simmons, A.; Suda, M.; Campbell, I.C.; O’Daly, O.; Cardi, V. Exposure to food in anorexia nervosa and brain correlates of food-related anxiety: Findings from a pilot study. J. Affect. Disord. 2020, 274, 1068–1075. [Google Scholar] [CrossRef] [PubMed]
- De Carvalho, M.R.; Dias, T.R.D.S.; Duchesne, M.; Nardi, A.E.; Appolinario, J.C. Virtual reality as a promising strategy in the assessment and treatment of bulimia nervosa and binge eating disorder: A systematic review. Behav. Sci. 2017, 7, 43. [Google Scholar] [CrossRef] [PubMed]
- Botvinick, M.; Cohen, J. Rubber hands ‘feel’ touch that eyes see. Nature 1998, 391, 756. [Google Scholar] [CrossRef] [PubMed]
- Tagini, S.; Scarpina, F.; Bruni, F.; Scacchi, M.; Mauro, A.; Zampini, M. The virtual hand illusion in obesity: Dissociation between multisensory interactions supporting illusory experience and self-location recalibration. Multisens. Res. 2020, 33, 337–361. [Google Scholar] [CrossRef]
- Crea, S.; D’Alonzo, M.; Vitiello, N.; Cipriani, C. The rubber foot illusion. J. Neuro Eng. Rehabilit. 2015, 12, 77. [Google Scholar] [CrossRef]
- Robertson, C.; Archibald, D.; Avenell, A.; Douglas, F.; Hoddinott, P.; van Teijlingen, E.; Boyers, D.; Stewart, F.; Boachie, C.; Fioratou, E.; et al. Systematic reviews of and integrated report on the quantitative, qualitative and economic evidence base for the management of obesity in men. Health Technol. Assess. 2014, 18, 35. [Google Scholar] [CrossRef]
- Dombrowski, S.U.; Knittle, K.; Avenell, A.; Araujo-Soares, V.; Sniehotta, F.F. Long term maintenance of weight loss with non-surgical interventions in obese adults: Systematic review and meta-analyses of randomised controlled trials. BMJ 2014, 348, g2646. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).