Comparison of Postural Features and Muscle Strength between Children with Idiopathic Short Stature and Healthy Peers in Relation to Physical Exercise
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Maximum Isometric Handgrip Strength Assessment
2.4. Explosive-Elastic Lower Limbs’ Strength Assessment
2.5. Stabilometric and Baropodometric Analysis
2.6. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Deodati, A.; Cianfarani, S. Impact of growth hormone therapy on adult height of children with idiopathic short stature: Systematic review. BMJ 2011, 342, c7157. [Google Scholar] [CrossRef] [PubMed]
- Wit, J.; Clayton, R.; Rogol, A.; Savage, M.; Saenger, P.; Cohen, P. Idiopathic short stature: Definition, epidemiology, and diagnostic evaluation. Growth Horm. IGF Res. 2008, 18, 89–110. [Google Scholar] [CrossRef] [PubMed]
- Wheeler, P.G.; Bresnahan, K.; Shephard, B.A.; Lau, J.; Balk, E.M. Short Stature and Functional Impairment. Arch. Pediatr. Adolesc. Med. 2004, 158, 236. [Google Scholar] [CrossRef] [PubMed]
- Bryant, J.; Cavé, C.; Milne, R. Recombinant growth hormone for idiopathic short stature in children and adolescents. Cochrane Database Syst. Rev. 2003, 2003. [Google Scholar] [CrossRef]
- Cohen, P.; Rogol, A.D.; Deal, C.L.; Saenger, P.; Reiter, E.O.; Ross, J.L.; Chernausek, S.D.; Savage, M.O.; Wit, J.M.; 2007 ISS Consensus Workshop Participants. Consensus Statement on the Diagnosis and Treatment of Children with Idiopathic Short Stature: A Summary of the Growth Hormone Research Society, the Lawson Wilkins Pediatric Endocrine Society, and the European Society for Paediatric Endocrinology Workshop. J. Clin. Endocrinol. Metab. 2008, 93, 4210–4217. [Google Scholar] [CrossRef]
- Kelnar, C.; Albertsson-Wikland, K.; Hintz, R.; Ranke, M.B.; Rosenfeld, R. Should We Treat Children with Idiopathic Short Stature? Horm. Res. Paediatr. 1999, 52, 150–157. [Google Scholar] [CrossRef]
- Wit, J.; Reiter, E.; Ross, J.; Saenger, P.; Savage, M.; Rogol, A.; Cohen, P. Idiopathic short stature: Management and growth hormone treatment. Growth Horm. IGF Res. 2008, 18, 111–135. [Google Scholar] [CrossRef]
- Finkelstein, B.S.; Imperiale, T.F.; Speroff, T.; Marrero, U.; Radcliffe, D.J.; Cuttler, L. Effect of Growth Hormone Therapy on Height in Children With Idiopathic Short Stature. Arch. Pediatr. Adolesc. Med. 2002, 156, 230. [Google Scholar] [CrossRef]
- Schena, L.; Meazza, C.; Pagani, S.; Paganelli, V.; Bozzola, E.; Tinelli, C.; Buzi, F.; Bozzola, M. Efficacy of long-term growth hormone therapy in short non-growth hormone-deficient children. J. Pediatr. Endocrinol. Metab. 2017, 30. [Google Scholar] [CrossRef]
- Sandberg, D.E. Quality of life and self-esteem in children treated for idiopathic short stature. J. Pediatr. 2003, 143, 691. [Google Scholar] [CrossRef]
- Quitmann, J.; Bullinger, M.; Sommer, R.; Rohenkohl, A.C.; Silva, N. Associations between Psychological Problems and Quality of Life in Pediatric Short Stature from Patients’ and Parents’ Perspectives. PLoS ONE 2016, 11, e0153953. [Google Scholar] [CrossRef] [PubMed]
- Jeong, H.R.; Shim, Y.S.; Lee, H.S.; Hwang, J.S. The effect of growth hormone treatment on height in children with idiopathic short stature. J. Pediatr. Endocrinol. Metab. 2014, 27. [Google Scholar] [CrossRef] [PubMed]
- Dahlgren, J. Metabolic Benefits of Growth Hormone Therapy in Idiopathic Short Stature. Horm. Res. Paediatr. 2011, 76, 56–58. [Google Scholar] [CrossRef] [PubMed]
- Yackobovitch-Gavan, M.; Gat-Yablonski, G.; Shtaif, B.; Hadani, S.; Abargil, S.; Phillip, M.; Lazar, L. Growth hormone therapy in children with idiopathic short stature–the effect on appetite and appetite-regulating hormones: A pilot study. Endocr. Res. 2018, 44, 16–26. [Google Scholar] [CrossRef] [PubMed]
- Gardner, M.; Boshart, M.; Yeguez, C.; Desai, K.; Sandberg, D. Coming up short: Risks of bias in studies assessing psychological outcomes associated with growth hormone therapy for short stature. J. Clin. Endocrinol. Metab. 2016, 101, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Chaplin, J.E.; Kriström, B.; Jonsson, B.; Tuvemo, T.; Albertsson-Wikland, K. Growth Hormone Treatment Improves Cognitive Function in Short Children with Growth Hormone Deficiency. Horm. Res. Paediatr. 2015, 83, 390–399. [Google Scholar] [CrossRef]
- Hunter, W.M.; Fonseka, C.C.; Passmore, R. Growth Hormone: Important Role in Muscular Exercise in Adults. Science 1965, 150, 1051–1053. [Google Scholar] [CrossRef]
- Pagani, S.; Cappa, M.; Meazza, C.; Ubertini, G.; Travaglino, P.; Bozzola, E.; Bozzola, M. Growth hormone isoforms release in response to physiological and pharmacological stimuli. J. Endocrinol. Investig. 2008, 31, 520–524. [Google Scholar] [CrossRef]
- Curtis, V.; Allen, D.B. Boosting the Late-Blooming Boy. Sports Heal. A Multidiscip. Approach 2010, 3, 32–40. [Google Scholar] [CrossRef]
- Krzykała, M.; Czerniak, U.; DeMuth, A. [Physical and motor development of preschool children in aspect of short stature]. Pediatr. Endocrinol. Diabetes Metab. 2008, 14, 135–140. [Google Scholar]
- Tomaszewski, P.; Milde, K.; Sienkiewicz-Dianzenza, E.; Nowicki, D. [Physical fitness of short-statured children at the early-school age]. Pediatr. Endocrinol. Diabetes Metab. 2007, 13, 125–128. [Google Scholar] [PubMed]
- Liu, M.; Wu, L.; Ming, Q. How Does Physical Activity Intervention Improve Self-Esteem and Self-Concept in Children and Adolescents? Evidence from a Meta-Analysis. PLoS ONE 2015, 10, e0134804. [Google Scholar] [CrossRef] [PubMed]
- Bidzan-Bluma, I.; Lipowska, M. Physical Activity and Cognitive Functioning of Children: A Systematic Review. Int. J. Environ. Res. Public Health 2018, 15, 800. [Google Scholar] [CrossRef] [PubMed]
- Harridge, S.D.R.; Lazarus, N. Physical Activity, Aging, and Physiological Function. Physiol. 2017, 32, 152–161. [Google Scholar] [CrossRef]
- Battaglia, G.; Giustino, V.; Messina, G.; Faraone, M.; Brusa, J.; Bordonali, A.; Barbagallo, M.; Palma, A.; Dominguez, L.-J. Walking in Natural Environments as Geriatrician’s Recommendation for Fall Prevention: Preliminary Outcomes from the “Passiata Day” Model. Sustainable 2020, 12, 2684. [Google Scholar] [CrossRef]
- Scoppa, F.; Gallamini, M.; Belloni, G.; Messina, G. Clinical Stabilometry Standardization: Feet Position in the Static Stabilometric Assessment of Postural Stability. Acta Medica. Mediterr. 2017, 33, 707–713. [Google Scholar] [CrossRef]
- The Jamovi Project (2020). jamovi (Version 1.2) [Computer Software]. Available online: https://www.jamovi.org.
- Bryant, J.; Baxter, L.; Cave, C.B.; Milne, R. Recombinant growth hormone for idiopathic short stature in children and adolescents. Cochrane Database Syst. Rev. 2007, 2007, CD004440. [Google Scholar] [CrossRef]
- Wit, J.M.; Ranke, M.B.; Kelnar, C.J.H. ESPE Classification of Paediatric Endocrine Diagnoses; Karger, S., Ed.; Supplement Issue (Suppl. 2); Hormone Research: Basel, Switzerland, 2007; Volume 68. [Google Scholar]
- Eika, F.; Blomkvist, A.W.; Rahbek, M.T.; Eikhof, K.D.; Hansen, M.D.; Søndergaard, M.; Ryg, J.; Andersen, S.; Jorgensen, M. Reference data on hand grip and lower limb strength using the Nintendo Wii balance board: A cross-sectional study of 354 subjects from 20 to 99 years of age. BMC Musculoskelet. Disord. 2019, 20, 21. [Google Scholar] [CrossRef]
- Hasegawa, R.; Islam, M.M.; Lee, S.C.; Koizumi, D.; Rogers, M.E.; Takeshima, N. Threshold of lower body muscular strength necessary to perform ADL independently in community-dwelling older adults. Clin. Rehabil. 2008, 22, 902–910. [Google Scholar] [CrossRef]
- Bohannon, R.W.; Magasi, S.R.; Bubela, D.J.; Wang, Y.-C.; Gershon, R.C. Grip and knee extension muscle strength reflect a common construct among adults. Muscle Nerve 2012, 46, 555–558. [Google Scholar] [CrossRef] [PubMed]
- Ortega, F.B.; Silventoinen, K.; Tynelius, P.; Rasmussen, F. Muscular strength in male adolescents and premature death: Cohort study of one million participants. BMJ 2012, 345, e7279. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, A.G.; Elhadidy, E.I.; Hamza, M.S.; Mohamed, N.E. Determining correlations between hand grip strength and anthropometric measurements in preschool children. J. Taibah Univ. Med. Sci. 2020, 15, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Bohannon, R.W. Muscle strength. Curr. Opin. Clin. Nutr. Metab. Care 2015, 18, 465–470. [Google Scholar] [CrossRef] [PubMed]
- Molenaar, H.M.; Selles, R.W.; Zuidam, J.M.; Willemsen, S.P.; Stam, H.J.; Hovius, S.E.R. Growth Diagrams for Grip Strength in Children. Clin. Orthop. Relat. Res. 2009, 468, 217–223. [Google Scholar] [CrossRef] [PubMed]
- Berndt, C.; Schweizer, R.; Ranke, M.B.; Binder, G.; Martin, D. Height, Muscle, Fat and Bone Response to Growth Hormone in Short Children with Very Low Birth Weight Born Appropriate for Gestational Age and Small for Gestational Age. Horm. Res. Paediatr. 2014, 82, 81–88. [Google Scholar] [CrossRef]
- Mainenti, M.; Vigário, P.S.; Teixeira, P.F.S.; Maia, M.D.L.; Oliveira, F.P.; Vaisman, M. Effect of levothyroxine replacement on exercise performance in subclinical hypothyroidism. J. Endocrinol. Investig. 2009, 32, 470–473. [Google Scholar] [CrossRef]
- Macfaul, R.; Dorner, S.; Brett, E.M.; Grant, D.B. Neurological abnormalities in patients treated for hypothyroidism from early life. Arch. Dis. Child. 1978, 53, 611–619. [Google Scholar] [CrossRef]
- Sartorio, A.; Narici, M.; Conti, A.; Monzani, M.; Faglia, G. Quadriceps and hand-grip strength in adults with childhood-onset growth hormone deficiency. Eur. J. Endocrinol. 1995, 132, 37–41. [Google Scholar] [CrossRef]
- Battaglia, G.; Bellafiore, M.; Bianco, A.; Paoli, A.; Palma, A. Effects of a dynamic balance training protocol on podalic support in older women. Pilot Study. Aging Clin. Exp. Res. 2009, 22, 418–424. [Google Scholar] [CrossRef]
- Bellafiore, M.; Battaglia, G.; Bianco, A.; Paoli, A.; Farina, F.; Palma, A. Improved postural control after dynamic balance training in older overweight women. Aging Clin. Exp. Res. 2010, 70, 614–618. [Google Scholar] [CrossRef] [PubMed]
- Kempers, M.; Veer, L.V.D.S.; Van Der Sanden, M.W.G.N.; Kooistra, L.; Wiedijk, B.M.; Faber, I.R.; Last, B.F.; De Vijlder, J.J.M.; Grootenhuis, M.A.; Vulsma, T. Intellectual and Motor Development of Young Adults with Congenital Hypothyroidism Diagnosed by Neonatal Screening. J. Clin. Endocrinol. Metab. 2006, 91, 418–424. [Google Scholar] [CrossRef] [PubMed]
- Hauri-Hohl, A.; Dusoczky, N.; Dimitropoulos, A.; Leuchter, R.H.-V.; Molinari, L.; Caflisch, J.; Jenni, O.G.; Latal, B. Impaired Neuromotor Outcome in School-Age Children With Congenital Hypothyroidism Receiving Early High-Dose Substitution Treatment. Pediatr. Res. 2011, 70, 614–618. [Google Scholar] [CrossRef] [PubMed]
- Donze, S.H.; Damen, L.; Mahabier, E.F.; Hokken-Koelega, A.C.S. Improved Mental and Motor Development During 3 Years of GH Treatment in Very Young Children With Prader-Willi Syndrome. J. Clin. Endocrinol. Metab. 2018, 103, 3714–3719. [Google Scholar] [CrossRef] [PubMed]
- Mauras, N.; Hayes, V.; Welch, S.; Rini, A.; Helgeson, K.; Dokler, M.; Veldhuis, J.D.; Urban, R.J. Testosterone Deficiency in Young Men: Marked Alterations in Whole Body Protein Kinetics, Strength, and Adiposity1. J. Clin. Endocrinol. Metab. 1998, 83, 1886–1892. [Google Scholar] [CrossRef] [PubMed]
- Schweizer, R.; Schwarze, C.P.; Binder, G.; Georgiadou, A.; Ihle, J.; Ranke, M.B.; Martin, D.D. Cortical Bone Density Is Normal in Prepubertal Children with Growth Hormone (GH) Deficiency, but Initially Decreases during GH Replacement due to Early Bone Remodeling. J. Clin. Endocrinol. Metab. 2003, 88, 5266–5272. [Google Scholar] [CrossRef] [PubMed][Green Version]

| Characteristics | ISS | HC | p |
|---|---|---|---|
| Age (years) | 10.96 ± 1.68 | 10.19 ± 1.06 | 0.068 |
| Height (cm) | 122.28 ± 9.61 | 140.08 ± 8.14 | 0.001 * |
| Weight (kg) | 24.56 ± 4.44 | 39.36 ± 9.83 | 0.001 * |
| BMI (kg/m2) | 16.41 ± 2.15 | 19.85 ± 4.20 | 0.003 * |
| Measures | ISS | HC | p |
|---|---|---|---|
| Limbs’ strength | |||
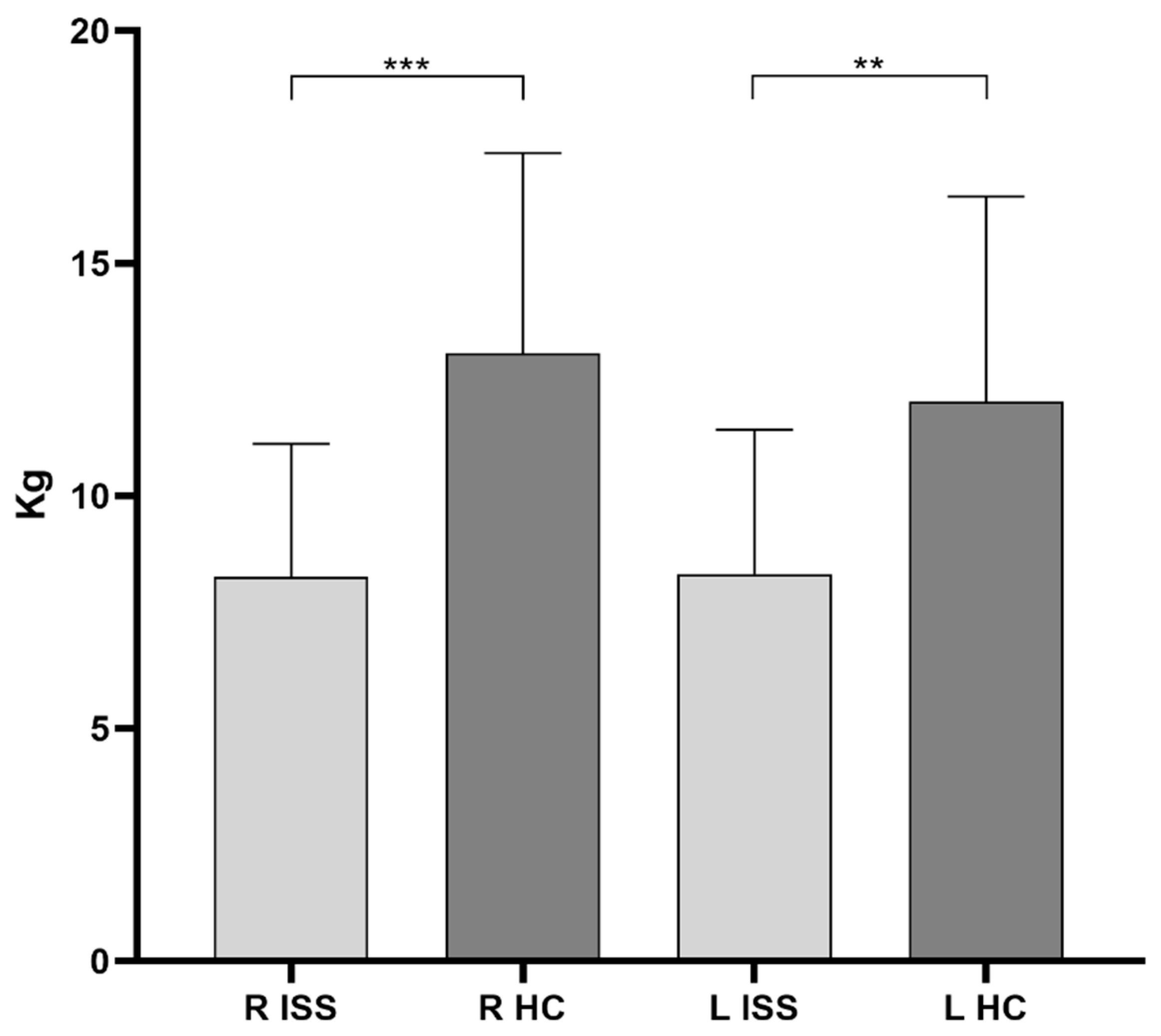
| R MIHS (kg) | 8.26 ± 2.86 | 13.07 ± 4.31 | 0.001 * |
| L MIHS (kg) | 8.32 ± 3.1 | 12.03 ± 4.41 | 0.004 * |
| EELLS (cm) | 13.33 ± 6.06 | 15.88 ± 5.78 | 0.165 |
| Posturographic measures | |||
| SPL (mm) | 229.08 ± 282.54 | 315.07 ± 298.87 | 0.343 |
| ES (mm2) | 733.24 ± 313.66 | 616.66 ± 201.84 | 0.141 |
| R Foot load (%) | 53.78 ± 8.32 | 48.42 ± 4.88 | 0.010 * |
| L Foot load (%) | 46.22 ± 8.32 | 51.58 ± 4.88 | 0.010 * |
| Measures | ISS Active | HC Active | p | ISS Inactive | HC Inactive | p |
|---|---|---|---|---|---|---|
| Limbs’ strength | ||||||
| R MIHS (kg) | 7.33 ± 2.48 | 14.03 ± 4.67 | 0.01 * | 8.75 ± 2.92 | 12.55 ± 4.15 | 0.01 * |
| L MIHS (kg) | 7.17 ± 2.59 | 12.81 ± 4.97 | 0.02 * | 8.94 ± 3.16 | 11.61 ± 4.19 | 0.07 |
| EELLS (cm) | 17.43 ± 7.66 | 20.56 ± 5.25 | 0.35 | 12.17 ± 5.67 | 13.41 ± 4.43 | 0.51 |
| Posturographic measures | ||||||
| SPL (mm) | 273.66 ± 432.82 | 257.07 ± 206.76 | 0.25 | 185.78 ± 147.54 | 345.78 ± 339.56 | 0.61 |
| ES (mm2) | 831.34 ± 437.48 | 628.26 ± 239.03 | 0.92 | 648.7 ± 208.57 | 610.53 ± 187.02 | 0.13 |
| R Foot load (%) | 47.14 ± 7.76 | 51.22 ± 5.74 | 0.25 | 45.42 ± 8.6 | 51.76 ± 4.55 | 0.02 * |
| L Foot load (%) | 52.86 ± 7.76 | 48.78 ± 5.74 | 0.25 | 54.58 ± 8.6 | 48.24 ± 4.55 | 0.02 * |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brusa, J.; Maggio, M.C.; Zangla, D.; Giustino, V.; Thomas, E.; Palma, R.; Messina, G.; Palma, A.; Corsello, G.; Bellafiore, M. Comparison of Postural Features and Muscle Strength between Children with Idiopathic Short Stature and Healthy Peers in Relation to Physical Exercise. Sustainability 2020, 12, 3639. https://doi.org/10.3390/su12093639
Brusa J, Maggio MC, Zangla D, Giustino V, Thomas E, Palma R, Messina G, Palma A, Corsello G, Bellafiore M. Comparison of Postural Features and Muscle Strength between Children with Idiopathic Short Stature and Healthy Peers in Relation to Physical Exercise. Sustainability. 2020; 12(9):3639. https://doi.org/10.3390/su12093639
Chicago/Turabian StyleBrusa, Jessica, Maria Cristina Maggio, Daniele Zangla, Valerio Giustino, Ewan Thomas, Romilda Palma, Giuseppe Messina, Antonio Palma, Giovanni Corsello, and Marianna Bellafiore. 2020. "Comparison of Postural Features and Muscle Strength between Children with Idiopathic Short Stature and Healthy Peers in Relation to Physical Exercise" Sustainability 12, no. 9: 3639. https://doi.org/10.3390/su12093639
APA StyleBrusa, J., Maggio, M. C., Zangla, D., Giustino, V., Thomas, E., Palma, R., Messina, G., Palma, A., Corsello, G., & Bellafiore, M. (2020). Comparison of Postural Features and Muscle Strength between Children with Idiopathic Short Stature and Healthy Peers in Relation to Physical Exercise. Sustainability, 12(9), 3639. https://doi.org/10.3390/su12093639










