1. Introduction
Nowadays, the importance of knowledge management cannot be neglected and it has become a key strategic resource. Organizations need the knowledge to survive in the rapidly changing environment. Knowledge is the source of sustainable competitive advantage [
1,
2] and organizations are building knowledge assets to improve their competitiveness [
3]. This can be achieved by implementing knowledge management (KM). To gain a sustainable competitive advantage, KM is considered as a significant instrument for development and sustainability of organizational knowledge [
4]. KM aims to create, use, manage and share knowledge and information of an organization [
5]. The (explicit) knowledge may be shared in different ways, for example, through reports, databases, procedures, books, journals, and guidelines. KM also encourages the sharing of tacit knowledge, the knowledge that employees gain through experience and is not in written form. KM is crucial for organizations that want to achieve effectiveness and efficiency. KM has proved to be useful to organizations in a fast-changing environment [
6,
7].
KM is being used by various fields such as business, public policy, and information science. A multi-sectorial survey (consisting of organizations from healthcare, manufacturing, retail/wholesale, utilities and telecommunication, financial services and other sectors) revealed that 43% of organizations have a KM initiative in place, and one in ten considered knowledge management to be transforming the way they do business [
8]. The healthcare industry, however, is a late adopter of the KM concept compared to the business sector [
9]. Researchers and scholars have recently started working on KM for the healthcare industry; KM has quickly and swiftly made its way into the organizational and managerial processes of the healthcare sector [
10].
In recent years, the healthcare industry has grown exponentially; it is generating a lot of knowledge. The doctors and researchers in the medical field are continuously learning about new diseases, treatments, and care pathways. To capture this knowledge, the healthcare industry is methodically trying to adopt knowledge management (KM) because the customers are expecting to receive better healthcare services. To provide better health service, KM is an appropriate strategy [
11,
12] to transform the current traditional system of knowledge sharing. KM helps the healthcare industry by creation, identification, acquisition, development, preservation, dissemination and the utilization of healthcare knowledge [
13]. The application of this knowledge will significantly improve the quality of patient care. The presence of relevant knowledge available to the healthcare professional at the right time would significantly help in making the best patient care decisions. The developed countries have realized the importance of KM in healthcare and have moved towards its adoption [
14,
15]. However, the developing countries are lagging, although some countries (e.g., Iran [
11]) are now looking towards KM adoption. Pakistan is at the early stage of KM adoption, and its adoption is hindered by some barriers, e.g., top management support, insufficient strategic planning, the complexity of system, etc.
Pakistan as a developing country is facing multiple challenges in the healthcare system that need to be addressed e.g., it has a lot of people infected with hepatitis B and C which is about 7.6% of the population. Pakistan has the 5th highest number of people affected by tuberculosis, 4.3% of them are drug-resistant while 19% are among previously treated. Malaria is a big problem; the amount of affected people is quite high. HIV is also a growing concern, 0.1% of the population has it, and 77% among them got it through drug injection or blood transfusion (World Health Organization [
16]). Pakistan has the highest rate for unscreened blood transfusions. There have been many outbreaks of Dengue and Measles. Other than these issues Pakistan has faced many other problems such as floods, droughts, earthquakes, human-made emergencies as well as disease outbreaks. Other than diseases, there are many managerial issues in the hospitals of Pakistan; most of the patient dealing is done in the outpatient department (OPD) of government hospitals. The management has been burdened with providing health faculties to a large public with minimal resources; as a result, there is a shortage of facilities [
17]. KM helps to establish a better healthcare support system that can codify, and deliver medical practices by improving knowledge.
Keeping in mind the issues mentioned above, implementation of KM in healthcare is not an easy task; it faces numerous barriers. These barriers can be overcome with the help of a systematic and scientific study in this area. Therefore, this study aims to first, identify the key barriers to KM adoption in developing countries, especially in Pakistan through a systematic literature review; secondly, determine the interrelationship between the different barriers to KM adoption and construct their hierarchal structure model using Interpretive Structural Modeling (ISM); finally, to determine the driving and dependence power of these barriers through MICMAC analysis. Since this is a pioneer study on the barriers to KM implementation in healthcare of Pakistan, it will assist in understanding the barriers that KM has to face in the healthcare sector. The ISM and MICMAC approach is used to analyze the barriers to KM in the healthcare sector of Pakistan, in order to better understand the hierarchy of the barriers. This study will assist the relevant authorities to understand the barriers and to develop decisive policies to effectively deal with the barriers.
This paper is divided into six sections.
Section 1 has the introduction,
Section 2 provides a literature review,
Section 3 contains the research methodology,
Section 4 provides the methodology,
Section 5 provides the results and discussion, and, finally,
Section 6 provides the conclusions.
3. Research Methodology
Initially, many peer-reviewed publications on KM were carefully studied to determine the initial set of barriers to KM and research gap. These publications were searched using several databases such as Google Scholar, Scopus, Web of Science, Emerald, Taylor & Francis and Science Direct. The keywords used to search for these papers were: “knowledge management”, “healthcare” and “barriers”. By using these keywords, more than 155 papers from 55 journals were found. After obtaining these papers, the duplication was removed. Then, the papers’ abstract was studied, to ensure they were relevant to this research. After removing the duplication and irrelevant papers, there were 39 papers from 27 journals, two conference proceedings, and one book was left. Some of the famous journals that were used for this research along with the amount of papers are: Journal of Knowledge Management (5 papers), Sustainability (4 papers), Journal of Management in Engineering (2 papers), International Journal of Management Science and Engineering Management (2 papers), Journal of Management Information Systems (2 papers), Expert Systems with Applications (1 paper) and Behaviour & Information Technology (1 paper).
At the second stage, the barriers were discussed with eight experts to facilitate data analysis. The ISM-MICMAC approach provides the ease of selecting experts according to the convenience of the researcher. Therefore, different experts were screened out by their knowledge of KM and their willingness to participate in the research. Their knowledge was tested by asking them very basic questions related to KM. The total number of experts that participated in this research is 8; they are from different fields, two of them were academic professors, two were Head of Department of the hospital (Doctors), one Assistant Admin, two were nurses and one Deputy Director Health Department Khyber Pakhtunkhwa (KPK). The main reason to involve the experts was to analyze the barriers through group discussions. The main questions asked were:
Q1: Which barriers are impeding the implementation of KM in the healthcare sector?
Q2: What is the interaction between most relevant barriers impeding the implementation of KM in the healthcare sector Pakistan?
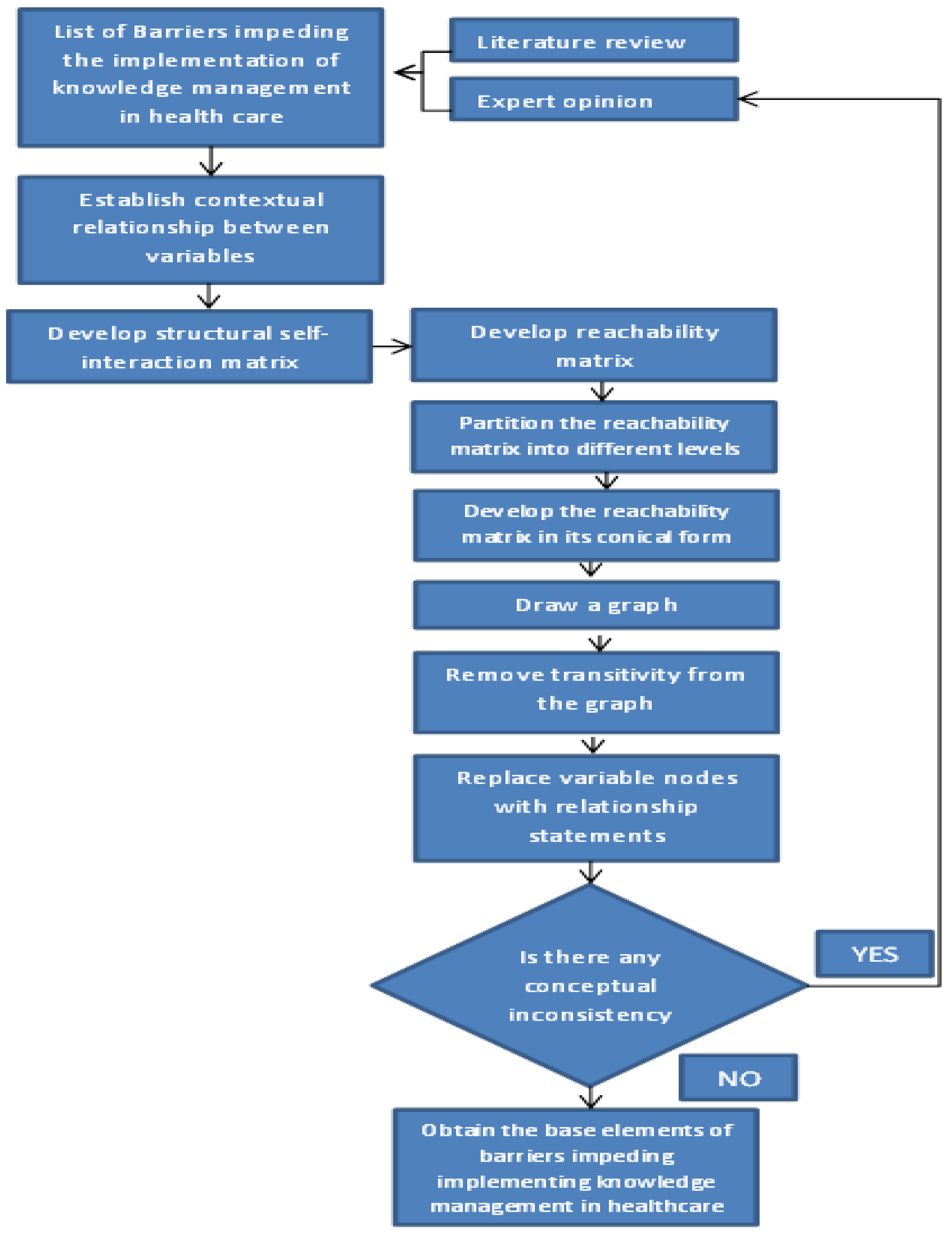
After detailed discussion, the responses were recorded. With the help of these responses, the structural self-interaction matrix (SSIM) table was made. After further analysis, a contextual relationship between these barriers was made. The research methodology for this study is given in
Figure 1.
5. Results and Discussion
Knowledge management has gained a considerable amount of importance over the past few years. It is considered a key to success and sustainable competitive advantage [
22]. KM can be used to enhance organizational performance and learning. It can be applied in different types of industries such as healthcare, manufacturing, supply chain, etc. In this study, we have considered it for healthcare. Healthcare is a ‘knowledge rich’ area; a lot of knowledge is being generated. With the help of KM, this information will be recorded and used to improve healthcare performance. KM is a rather new concept in the area of healthcare for developing countries, e.g., Pakistan. In the case of Pakistan, KM is at the stage of infancy. The healthcare industry is willing to learn from its past mistakes and improve its performance.
Pakistan is looking towards the adoption of KM to improve its healthcare service. Implementing KM will not be easy, and it faces several barriers. The main aim of this study is to identify the barriers that most affect knowledge management implementation in the healthcare sector of Pakistan so that they can be dealt with. In this study, the ISM and MICMAC technique is being used. The application of these techniques has given the following results:
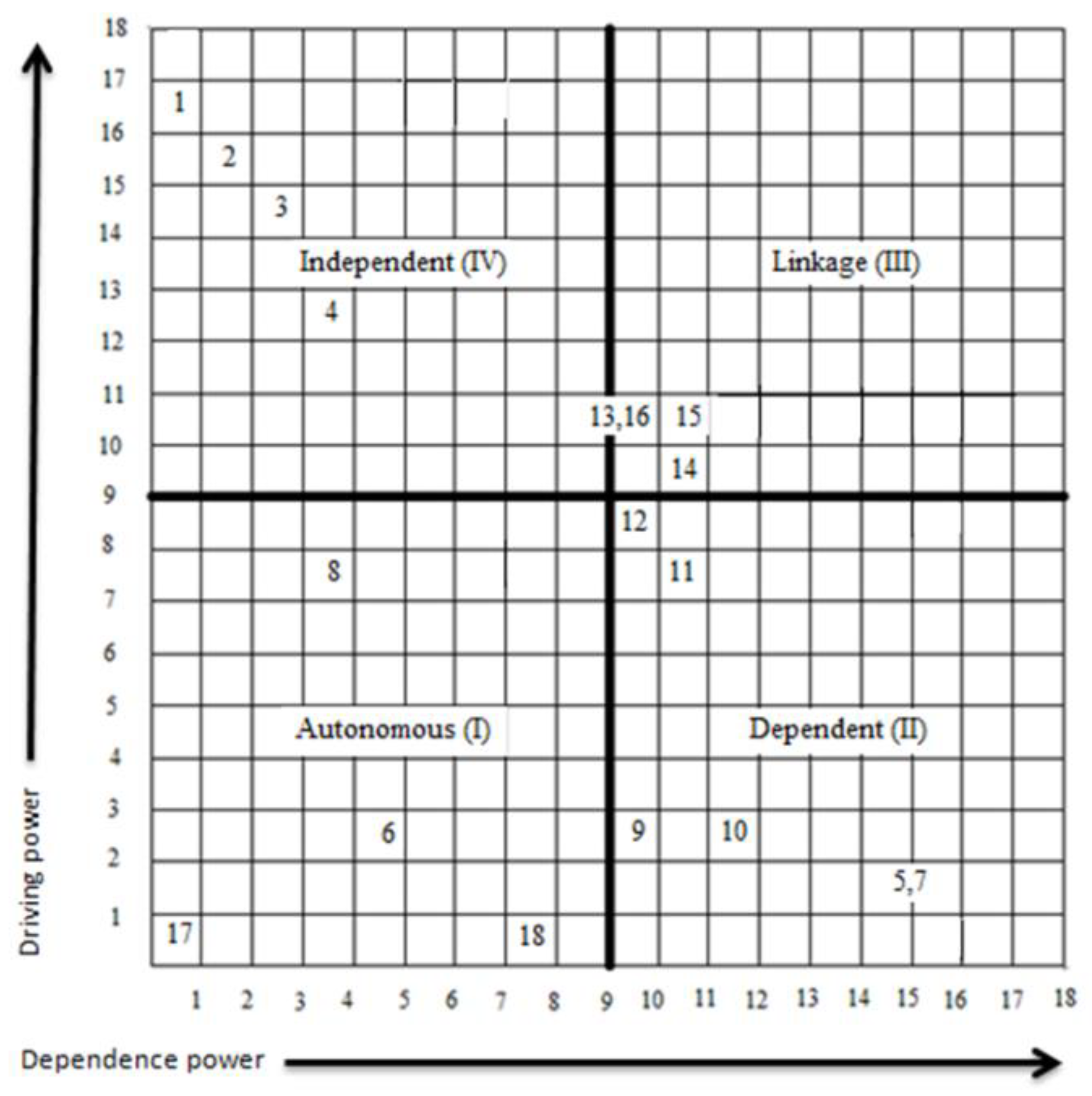
Autonomous barriers: The barriers that are placed in this quadrant (I) have weak driving and dependence power. These barriers are disconnected from the system. According to this study, four of the barriers lie in this category. Barrier 6 (Complexity of system), Barrier 7 (Cost of KM implementation), Barrier 17 (Lack of common definition) and Barrier 18 (Fear of embarrassment for sharing incorrect information). These barriers have lessor impact on the implementation of KM in the healthcare sector of Pakistan.
Dependent barriers: The barriers that are placed in this quadrant (II) have weak driving power but a strong dependence power. According to this study, six barriers lie in this quadrant. Barrier 5 (Uncertainty about the effectiveness of KM), barrier 7 (Lack of KM integration), barrier 9 (Scarcity of resources), barrier 10 (Lack of information quality) barrier 11 (Resistance to change) and barrier 12 (No lessons learned). These barriers play a significantly lesser role in impeding KM implementation. These barriers should still be handled carefully; this is because even though they have low driving power, they still have dependence power.
Linkage barriers: The barriers that are placed in this quadrant (III) are amongst the key barriers. These barriers have strong driving and dependence power. These barriers are unstable, any action made on them will result in affecting other barriers including themselves. Due to this, these barriers must be handled with maximum care. According to this study, four barriers lie in this quadrant. Barrier 13 (Employee conflict), barrier 14 (Lack of teamwork), barrier 15 (Lack of employees motivation) and barrier 16 (Employee reluctance to share information).
Independent barriers: The barriers that are placed in this quadrant (IV) are the key barriers or the root cause for other barriers. These barriers have strong driving but weak dependence power. According to this study, four barriers lie in this quadrant. Barrier 1 (Lack of support from Top management), barrier 2 (Insufficient Strategic planning), barrier 3 (Lack of support from organization structure) and barrier 4 (Non-supporting organizational culture).
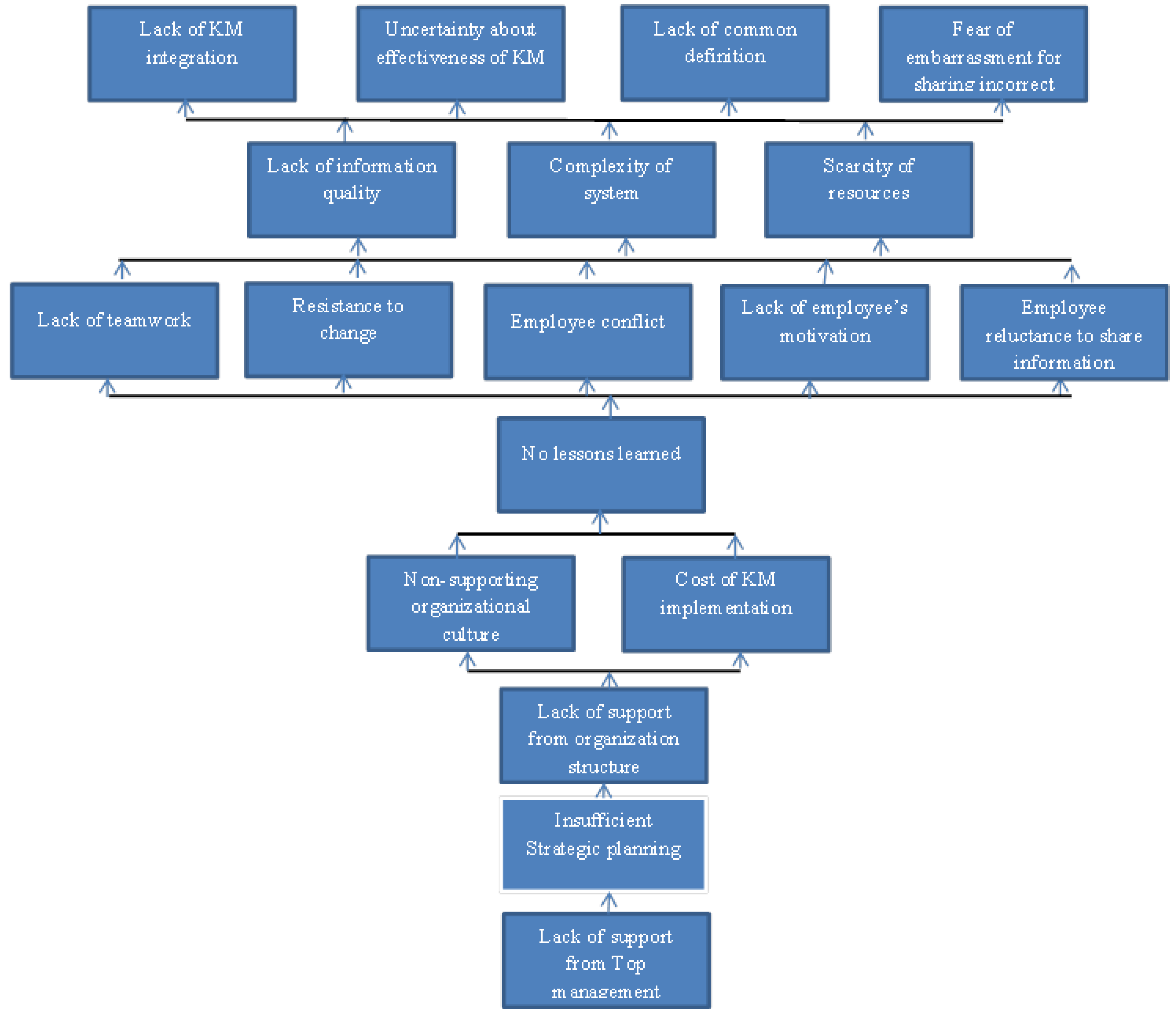
The ISM model of the current study shows the hierarchy of the barriers to KM implementation in the healthcare sector of Pakistan, lack of support from top management (barrier 1) forms the foundation of that hierarchical structure implying that it impedes the implementation of KM in the healthcare sector of Pakistan the most. In some previous studies [
11,
34], it has been considered as the topmost barrier. In the healthcare sector, the top management controls the administration of the hospital, but has no control over the working condition that affects physicians. The physician deals with clinical decision-making. The top management of healthcare needs to show leadership qualities to motivate the participation of physician and other stakeholders (nurses, management staff, paramedics, etc.) [
77] for KM implementation. It is the responsibility of the top management to remove the departmental and professional barriers that are impeding cross-functional teams from KM implementation. The healthcare infrastructure of Pakistan is among the largest in the world. Due to the large infrastructure, there is a great deal of centralization, (the ministry of health being at the top) making it very difficult to manage. Centralization impedes the flow of knowledge, hence impeding KM implementation in the healthcare sector. In the private sector of Pakistan, the hospitals are a sole proprietorship or a partnership model of organization, and very few belong to the ‘corporate public limited’ category, they are better off since the larger hospitals are more focused on information management. They need to be brought more towards KM to improve further.
It is the lack of support from Top management that leads to insufficient Strategic planning (barrier 2). Kotter (1988) mentioned that only the top management, the CEO [
78] of the hospital must promote the strategic plan and make it move ahead. The top management must analyze the current situation with the help of others (stakeholders) and create a shared vision towards the adoption of KM. Singh et al. [
32] in his work considered barrier 2 as one of the important barriers, it also specifies that, if top management is not committed to the implementation of KM, effective strategic planning would not be possible. The study done by Ibe´rica [
79] mentions the importance of strategic planning in healthcare organizations; it portrays that the patients these days are non-loyal because they are well informed, therefore the healthcare organization should provide better care. Schwartz, and Cohn [
30], in their work, mentioned that the healthcare organizations need strategic planning to meet the constraints of a lean economy, rapidly changing technologies, and an unprecedented need to provide quality services at affordable prices; the healthcare industry should clarify their mission, vision, and values. Realizing the importance of strategic planning, the private sector healthcare organizations of Pakistan have started making it. The private sector is better when it comes to strategic planning; these hospitals have a definite direction. The public sector is, however, lagging, the government has made a National Health Vision [
23] and are making several awareness programs, but their implementation is another issue [
25]. The success of strategic planning depends on the agreement of stakeholders, including physicians, nurses, and managers. Otherwise, it is a failure. The government of Pakistan at times tends to neglect considering the physicians and nurses [
80,
81]. The government of Pakistan has to focus on the implementation of its strategic planning since it is crucial for KM implementation in the healthcare sector.
If there is insufficient strategic planning, it will lead to a lack of support from organization structure (barrier 3). Rhodes [
82] mentioned that it is strategic planning that leads to the organization structure. The strategic plan should be reflected in the structure [
83] of the hospital. Strategic planning helps the hospitals to move in a certain direction towards the desired future [
79], if the structure is not supportive, then it will be difficult to achieve that target. If the structure of the hospital is not well designed, then it will have several adverse effects: (1) the hospital strategic direction will be affected, (2) the roles of doctors, managers and nursing staff would not be well defined, (3) low-quality patient care, and (4) restricted information flow. The private hospitals in Pakistan are relatively small, and their structure can be managed, but the structure of the public healthcare in Pakistan is very complex; with the Ministry of Health at the top and health houses and outreach workers at the bottom, there are many levels between them [
84]; this severely affects the flow of knowledge, which impedes KM implementation in the healthcare sector of Pakistan.
These barriers lead to non-supporting organizational culture (barrier 4) and cost of KM implementation (barrier 7). The organization culture develops around the structure [
85]. If the structure of the organization is not proper, it will result in non-supporting culture. The organizational culture helps to leverage intellectual assets [
86], the culture of the healthcare unit should be a problem solving one [
87] and should promote lifelong learning [
88]. The culture of healthcare highly influences employees’ behavior, creation, use and sharing of knowledge; it is the culture that helps in the retention of knowledge and not technology [
89]. However, the importance of technology cannot be ignored, and it is necessary for ensuring effective KM implementation in healthcare. Cost of KM implementation is high because it requires an IT infrastructure which in itself requires funds. The healthcare is highly dependent on technology. However, the use of technology in the public sector of Pakistan is limited, there is no IT, no record maintenance and a poor infrastructure [
90]. There is no Health Management Information System (HMIS) in the public sector. The Government of Pakistan (GoP) has realized the shortcoming of technology in its healthcare sector and has spent about
$3.04 billion on healthcare in 2018; this is 31.75% more compared to the previous year. According to Business Monitor International, the medical devices market in Pakistan is worth
$457.1 million and is expected to increase to
$537.5 million by 2020 [
91]. The private sector hospitals have invested heavily in technology and for them to move towards KM would not be costly. These two barriers will lead to no lesson being learned (barrier 12). When the flow of information is hindered by the organizational structure and culture, then there is no flow of information and hence no learning.
No lessons learned (barrier 12) gives rise to several other barriers, resistance to change (barrier 11), employees conflict (Barrier 13), lack of teamwork (barrier 14), lack of employee motivation (barrier 15), and employee reluctance to share information (barrier 16). All of these barriers are interrelated and affect each other. Since no lesson is being learned, employees are not learning from their past mistakes. They are not willing to work in teams and are not willing to share their knowledge. The employees are not willing to change the way they work because they are not motivated, resulting in conflicts at times. These barriers collectively give rise to other barriers such as the complexity of the system (barrier 6), scarcity of resources (barrier 9), and lack of information quality (barrier 10).
Finally, the barriers that are least impeding the implementation of KM in the healthcare of Pakistan are uncertainty about the effectiveness of KM (barrier 5), lack of KM integration (barrier 7), lack of common definition (barrier 17), and fear of embarrassment for sharing incorrect information (barrier 18). It is very crucial for the doctors, nurses, hospital administration, healthcare professionals, and health ministry to understand these barriers and the relationship between them, in order to effectively implement KM. These barriers need to be handled according to the hierarchy; the critical barriers must be treated first due to their severity.
Knowledge management in healthcare is gaining a considerable amount of importance. Several research works regarding this topic have been done ([
11,
12,
14,
15,
92,
93], etc.). There is a lot of knowledge that is being generated by the healthcare industry. This knowledge, unfortunately, is being lost because it is not properly documented, which can be significantly improved with KM. This knowledge can prove to be useful in the future for improving management and healthcare delivery system. The managing of this knowledge is crucial to achieving a sustainable competitive advantage in the healthcare industry. Many developed countries such as America, Canada, and European Union countries are using KM. It is being used in several industries such as healthcare, supply chain management, total quality management, tourism management, and the manufacturing industry. KM is a new concept for developing countries. KM has become a strategic and managerial topic for top management. The healthcare industry of Pakistan is likely to adopt KM. It will make its way through Iran, which is currently working on it [
11]. To introduce KM in the healthcare of Pakistan, it is important to study the barriers that KM will face.
While doing this study, several studies were reviewed, and there were many studies regarding barriers to KM, but not many (next to none) regarding barriers to KM in healthcare. There were no papers regarding barriers to KM in healthcare of developing countries. This led to the current study; barriers to KM in the health sector of Pakistan, a failure to deal with these barriers will surely impede the process of KM implementation. The contribution of this study is that, with the help of the ISM technique, the interrelationships among the barriers were identified, which will help in their elimination, hence resulting in the effective implementation of KM in the healthcare of Pakistan. This study gives us a clear idea of the issues. It also shows the potential role that KM has to play in the healthcare of Pakistan.
With the help of ISM and MICMAC analysis, several barriers were identified and analyzed in the Pakistan scenario. Therefore, the relevant entities (hospitals, staff unions, health ministry) should work together to try and introduce KM in healthcare. The healthcare industry in developed countries is becoming very competitive and becoming more globalized. They are attracting patients from across borders. Therefore, it would be beneficial for Pakistan to join the race. Thus, the Pakistan healthcare sector should adopt KM to gain a sustainable competitive advantage so that it can compete against rivals in the international market.
6. Conclusions
Both KM and healthcare are important topics. A lot of research has been done on these two topics independently. However, no research exists on KM in the healthcare sector of Pakistan; this is a pioneer study in this area. This study was done to address this area and fill the research gap. For this study, the ISM technique was used. First, a total of eight experts were requested to participate and contribute to this research. These experts were able to identify and shortlist 18 barriers. Secondly, the experts then identified the interrelationships that exist between the barriers. By these interrelationships, the driving and dependence powers were determined. Thirdly, by studying extensive literature on KM in healthcare, a clear idea was derived as to which barriers need to be dealt with to ensure effective implementation of KM in the healthcare of Pakistan.
While doing the level partition in this study, eight levels were developed, meaning that there are eight hierarchal levels. The 18 barriers are divided among the levels based on driving and dependence power. In ISM, the barriers at level 1 are less critical, and, as the levels grow, so does the criticality. The barriers of level 1 are lack of KM integration, uncertainty about the effectiveness of KM, lack of common definition and fear of embarrassment for sharing incorrect information. The barriers of level 2 are a scarcity of resources, the complexity of the system and lack of information quality. The barriers of level 3 are lack of teamwork, resistance to change, employee conflict, lack of employee’s motivation and employee reluctance to share information. The barriers of level 4 and 5 are no lessons learned, cost of KM implementation, and non-supporting organizational culture.
The most critical or key barriers are at levels 6, 7, and 8. These are the barriers that are impeding the effective implementation of KM in the healthcare sector of Pakistan; hence, these barriers must be tackled first. Since KM in healthcare is at the infancy stage, the lack of support from organization structure, insufficient strategic planning and lack of support from top management are obvious initial barriers. Without proper strategic planning along with little or nonexistent support from top management, nothing can be accomplished. These two barriers are of utmost importance. It is recommended that relevant authorities should handle these barriers.
There are a few limitations to this study; firstly, the model of this study has been conducted keeping in mind the situation of Pakistan, and Pakistani experts were used. The interrelationships between the barriers are dependent on the experts’ opinion; their views might change over time. The model may vary from a real-world situation. Secondly, the ISM technique does not statistically validate the relationship, ISM is a tool that helps in developing initial models, and SEM can statistically validate them. Therefore, it is suggested to do SEM on this study.