Clinical Acceptance of Digitally Produced Zirconia and Metal Post and Cores, Based on the Impression Method
Abstract
1. Introduction
2. Materials and Methods
- 1.
- Following the completion of endodontic treatment, gutta-percha removal from the tooth is performed using burs (Gates Glidden, Pulpdent Corp., Watertown, MA, USA) to achieve the desired post length, ensuring the preservation of the apical seal.
- 2.
- The coronal aspect of the tooth is then prepared to eliminate acute angles between the post surfaces and the apical surface of the core. This adjustment facilitates optimal reading by the intraoral scanner at the core-post junction. Special attention is given to ensuring that the core-post junction possesses sufficient width to prevent fracture during the milling of zirconia. Additionally, the post is shaped with rounded internal line angles where it interfaces with the tooth surfaces.
- 3.
- A fully digital workflow was implemented for each zirconia or metal post. The digital post impression was captured using an intraoral scanner (TRIOS 4, 3Shape, Copenhagen, Denmark) and the completeness of the digital impression of the prepared root canal was verified on the scanner’s display. Also, the rules of taking a good TRIOS scan were respected according with the manufacturer’s recommendations, and the clinician dried the teeth well before scanning [17].
- 4.
- The STL dataset was utilized to design the post and core in CAD software (Exocad 3.1 Rijeka, EXOCAD GmbH, Darmstadt, Germany). The cement gap parameter was set to 50 µm.
- 5a.
- After completing the design, the STL files of the post and cores were transmitted to the 5-axis milling machine (CORiTEC® 250i Loader PRO, Imes Icore GmbH, Eiterfeld, Germany) to mill the zirconia disk (Luxen, Dentalmax, Cheonan-si, Republic of Korea). Subsequently, the attachment points of the post to the CAD/CAM disk were cut and smoothed. The posts underwent sintering in a zirconia furnace (AUSTROMAT Series 6, DEKEMA Dental-Keramiköfen GmbH, Salzburg, Germany) for 11 h at a maximum temperature of 1530 °C.
- 5b.
- Upon finalizing the design, STL files of the post and cores were transferred to the 3D metal printer (MySint100, Sisma, Vicenza, Italy), employing Cr-Co powder for the laser sintering of metal posts. Subsequently, attachment points of the printed post underwent cutting and smoothing.
- 1.
- Following endodontic therapy, gutta-percha removal utilized burs (Gates Glidden, Pulpdent Corp., Watertown, MA, USA) to achieve the desired post length, preserving the apical seal.
- 2.
- The coronal aspect underwent preparation to eliminate acute angles between post surfaces and the core’s apical surface. This adjustment optimized the flow of impression material, with a focus on ensuring a sufficiently wide core-post junction to prevent fractures during zirconia milling.
- 3.
- Impression recording for post and core preparation involved addition silicone impression material (Elite HD, Zhermack, Badia Polesine, Italy). The silicone was injected into the canal with a disposable dispenser. In addition, alginate (Hydrogum 5, Zhermack, Badia Polesine, Italy) recorded antagonists, while bite registration silicone (Occlufast, Zhermack, Badia Polesine, Italy) recorded intermaxillary relations. Arch impressions were promptly sent to the dental laboratory and poured into plaster models (Elite Rock, Zhermack, Badia Polesine, Italy). For assuring the quality and precision of the plaster models, technicians respected the instructions for use from the manufacturer: water/powder ratio of 20 mL/100 g, 12 min working time, 14 min setting time for a 2 h setting expansion of 0.08%.
- 4.
- From this point, the workflow became digital, scanning the plaster models with a laboratory scanner (Medit T510, Medit, Seoul, Republic of Korea).
- 5.
- The STL dataset facilitated post and core design in CAD software (Exocad Rijeka, EXOCAD GmbH, Darmstadt, Germany). The cement gap parameter was set at 50 µm.
- 6a.
- After completing the design, the STL files of the zirconia post and cores were transmitted to the 5-axis milling machine (CORiTEC® 250i Loader PRO, Imes Icore GmbH, Eiterfeld, Germany) to mill the zirconia disk (Luxen, Dentalmax, Republic of Korea). Subsequently, the attachment points of the post to the CAD/CAM disk were cut and smoothed. The posts underwent sintering in a high-speed furnace (AUSTROMAT Series 6, DEKEMA Dental-Keramiköfen GmbH, Salzburg, Germany) for 11 h at a maximum temperature of 1530 degrees.
- 6b.
- Upon finalizing the design, STL files of the post and cores were transferred to the 3D metal printer (MySint100, Sisma, Vicenza, Italy), employing Cr-Co powder for the laser sintering of metal posts. Subsequently, attachment points of the printed post underwent cutting and smoothing.
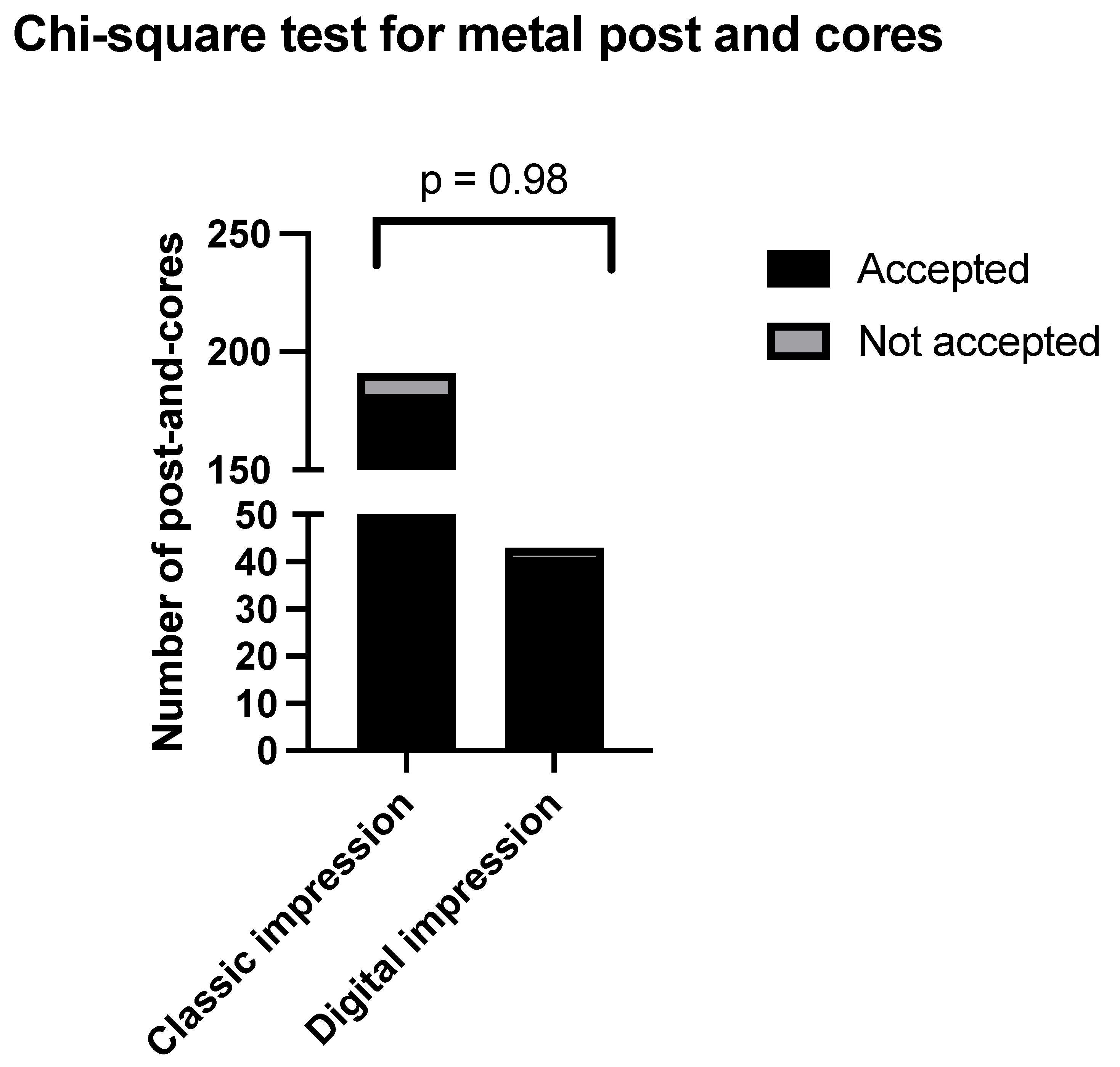
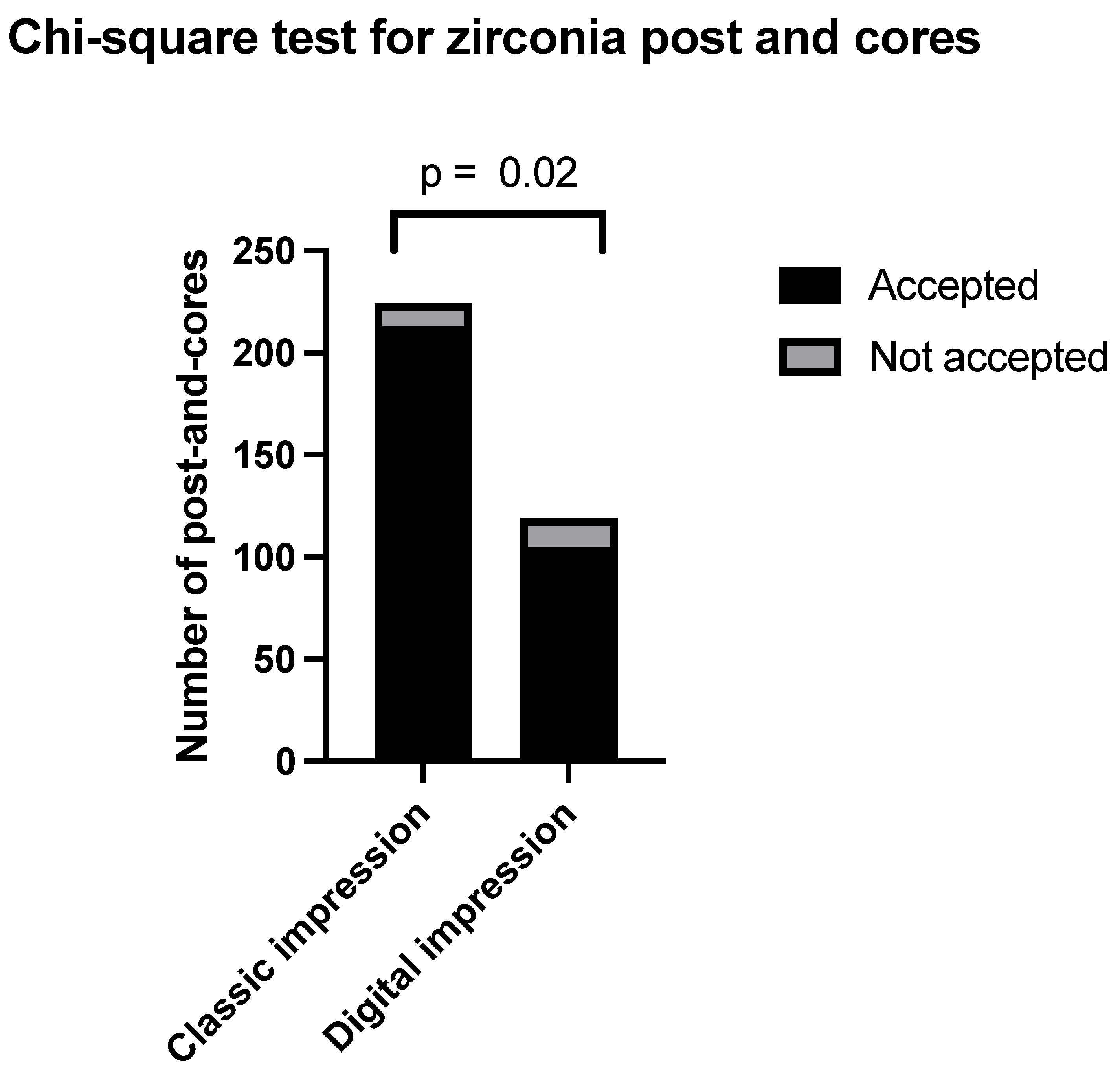
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Maroulakos, G.; Nagy, W.W.; Kontogiorgos, E.D. Fracture resistance of compromised endodontically treated teeth restored with bonded post and cores: An in vitro study. J. Prosthet. Dent. 2015, 114, 390–397. [Google Scholar] [CrossRef] [PubMed]
- Giovani, A.R.; Vansan, L.P.; de Sousa Neto, M.D.; Paulino, S.M. In vitro fracture resistance of glass-fiber and cast metal posts with different lengths. J. Prosthet. Dent. 2009, 101, 183–188. [Google Scholar] [CrossRef]
- Fernandes, A.S.; Shetty, S.; Coutinho, I. Factors determining post selection: A literature review. J. Prosthet. Dent. 2003, 90, 556–562. [Google Scholar] [CrossRef] [PubMed]
- Bilgin, M.S.; Erdem, A.; Dilber, E.; Ersoy, İ. Comparison of fracture resistance between cast, CAD/CAM milling, and direct metal laser sintering metal post systems. J. Prosthodont. Res. 2016, 60, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Revilla León, M.; Klemm, I.M.; García-Arranz, J.; Özcan, M. 3D Metal Printing—Additive Manufacturing Technologies for Frameworks of Implant-Borne Fixed Dental Prosthesis. Eur. J. Prosthodont. Restor. Dent. 2017, 25, 143–147. [Google Scholar] [CrossRef]
- Baysal, N.; Tuğba Kalyoncuoğlu, Ü.; Ayyıldız, S. Mechanical Properties and Bond Strength of Additively Manufactured and Milled Dental Zirconia: A Pilot Study. J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2022, 31, 629–634. [Google Scholar] [CrossRef]
- Zhang, D.; Sun, S.; Qiu, D.; Gibson, M.A.; Dargusch, M.S.; Brandt, M.; Qian, M.; Easton, M. Metal Alloys for Fusion-Based Additive Manufacturing. Adv. Eng. Mater. 2018, 20, 1700952. [Google Scholar] [CrossRef]
- Vinothkumar, T.S.; Kandaswamy, D.; Chanana, P. CAD/CAM fabricated single-unit all-ceramic post–core–crown restoration. J. Conserv. Dent. JCD 2011, 14, 86–89. [Google Scholar] [CrossRef]
- Streacker, A.B.; Geissberger, M. The milled ceramic post and core: A functional and esthetic alternative. J. Prosthet. Dent. 2007, 98, 486–487. [Google Scholar] [CrossRef]
- Meyenberg, K.H.; Lüthy, H.; Schärer, P. Zirconia posts: A new all-ceramic concept for nonvital abutment teeth. J. Esthet. Dent. 1995, 7, 73–80. [Google Scholar] [CrossRef]
- Calabro, D.E.; Kojima, A.N.; Gallego Arias Pecorari, V.; Helena Coury Saraceni, C.; Blatz, M.B.; Özcan, M.; Mikail Melo Mesquita, A. A 10-Year Follow-Up of Different Intra-Radicular Retainers in Teeth Restored with Zirconia Crowns. Clin. Cosmet. Investig. Dent. 2019, 11, 409–417. [Google Scholar] [CrossRef] [PubMed]
- Bateli, M.; Kern, M.; Wolkewitz, M.; Strub, J.R.; Att, W. A retrospective evaluation of teeth restored with zirconia ceramic posts: 10-year results. Clin. Oral Investig. 2014, 18, 1181–1187. [Google Scholar] [CrossRef] [PubMed]
- Altitinchi, A.; Hussein, A.; Saemundsson, S.; Clark, W.; Culp, L.; Sulaiman, T.A. Anatomic CAD-CAM post-and-core systems: A mastication simulation study. J. Prosthet. Dent. 2024, 132, 586–591. [Google Scholar] [CrossRef] [PubMed]
- Türker, S.A.; Özçelik, B.; Yilmaz, Z. Evaluation of the Bond Strength and Fracture Resistance of Different Post Systems. J. Contemp. Dent. Pract. 2015, 16, 788–793. [Google Scholar] [CrossRef] [PubMed]
- Martins, M.D.; Junqueira, R.B.; de Carvalho, R.F.; Lacerda, M.F.L.S.; Faé, D.S.; Lemos, C.A.A. Is a fiber post better than a metal post for the restoration of endodontically treated teeth? A systematic review and meta-analysis. J. Dent. 2021, 112, 103750. [Google Scholar] [CrossRef]
- Lin, L.; Zhuo, Y.; Cai, P.; Chen, X.; Zheng, Z.; Lin, J. Use of an intraoral scanner and CAD-CAM for simultaneous restoration with a personalized titanium post-core and a zirconia crown. J. Oral Sci. 2024, 66, 82–84. [Google Scholar] [CrossRef]
- Goujat, A.; Abouelleil, H.; Colon, P.; Jeannin, C.; Pradelle, N.; Seux, D.; Grosgogeat, B. Marginal and internal fit of CAD-CAM inlay/onlay restorations: A systematic review of in vitro studies. J. Prosthet. Dent. 2019, 121, 590–597.e3. [Google Scholar] [CrossRef]
- Ferrairo, B.M.; Piras, F.F.; Lima, F.F.; Honório, H.M.; Duarte, M.A.H.; Borges, A.F.S.; Rubo, J.H. Comparison of marginal adaptation and internal fit of monolithic lithium disilicate crowns produced by 4 different CAD/CAM systems. Clin. Oral Investig. 2021, 25, 2029–2036. [Google Scholar] [CrossRef]
- Farah, R.I.; Alresheedi, B. Evaluation of the marginal and internal fit of CAD/CAM crowns designed using three different dental CAD programs: A 3-dimensional digital analysis study. Clin. Oral Investig. 2023, 27, 263–271. [Google Scholar] [CrossRef]
- da Costa, J.B.; Pelogia, F.; Hagedorn, B.; Ferracane, J.L. Evaluation of Different Methods of Optical Impression Making on the Marginal Gap of Onlays Created with CEREC 3D. Oper Dent. 2010, 35, 324–329. [Google Scholar] [CrossRef]
- Alajaji, N.K.; Bardwell, D.; Finkelman, M.; Ali, A. Micro-CT Evaluation of Ceramic Inlays: Comparison of the Marginal and Internal Fit of Five and Three Axis CAM Systems with a Heat Press Technique. J. Esthet. Restor. Dent. 2017, 29, 49–58. [Google Scholar] [CrossRef] [PubMed]
- Krämer, N.; Lohbauer, U.; Frankenberger, R. Adhesive luting of indirect restorations. Am. J. Dent. 2000, 13, 60D–76D. [Google Scholar] [PubMed]
- Roperto, R.; Assaf, H.; Soares-Porto, T.; Lang, L.; Teich, S. Are different generations of CAD/CAM milling machines capable to produce restorations with similar quality? J. Clin. Exp. Dent. 2016, 8, e423–e428. [Google Scholar] [CrossRef] [PubMed]
- Kale, E.; Seker, E.; Yilmaz, B.; Özcelik, T.B. Effect of cement space on the marginal fit of CAD-CAM-fabricated monolithic zirconia crowns. J. Prosthet. Dent. 2016, 116, 890–895. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.Y.; Kim, J.H.; Kim, H.Y.; Kim, W.C. Comparison and evaluation of marginal and internal gaps in cobalt-chromium alloy copings fabricated using subtractive and additive manufacturing. J. Prosthodont. Res. 2018, 62, 56–64. [Google Scholar] [CrossRef]
- McLean, J.W.; von Fraunhofer, J.A. The estimation of cement film thickness by an in vivo technique. Br. Dent. J. 1971, 131, 107–111. [Google Scholar] [CrossRef]
- Belser, U.C.; MacEntee, M.I.; Richter, W.A. Fit of three porcelain-fused-to-metal marginal designs in vivo: A scanning electron microscope study. J. Prosthet. Dent. 1985, 53, 24–29. [Google Scholar] [CrossRef]
- Sailer, I.; Fehér, A.; Filser, F.; Gauckler, L.J.; Lüthy, H.; Hämmerle, C.H.F. Five-year clinical results of zirconia frameworks for posterior fixed partial dentures. Int. J. Prosthodont. 2007, 20, 383–388. [Google Scholar]
- Mously, H.A.; Finkelman, M.; Zandparsa, R.; Hirayama, H. Marginal and internal adaptation of ceramic crown restorations fabricated with CAD/CAM technology and the heat-press technique. J. Prosthet. Dent. 2014, 112, 249–256. [Google Scholar] [CrossRef]
- Lins, L.; Bemfica, V.; Queiroz, C.; Canabarro, A. In vitro evaluation of the internal and marginal misfit of CAD/CAM zirconia copings. J. Prosthet. Dent. 2015, 113, 205–211. [Google Scholar] [CrossRef]
- Alfaro, D.P.; Ruse, N.D.; Carvalho, R.M.; Wyatt, C.C. Assessment of the Internal Fit of Lithium Disilicate Crowns Using Micro-CT. J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2015, 24, 381–386. [Google Scholar] [CrossRef] [PubMed]
- Pinto, A.; Arcuri, L.; Carosi, P.; Nardi, R.; Libonati, A.; Ottria, L.; Campanella, V. In vitro evaluation of the post-space depth reading with an intraoral scanner (IOS) compared to a traditional silicon impression. Oral Implantol. 2017, 10, 360–368. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Shu, X.; Zhang, Y.; Yang, B.; Jian, Y.; Zhao, K. Evaluation of fiber posts vs metal posts for restoring severely damaged endodontically treated teeth: A systematic review and meta-analysis. Quintessence Int. Berl. Ger. 1985. 2019, 50, 8–20. [Google Scholar] [CrossRef]
- Sarkis-Onofre, R.; Amaral Pinheiro, H.; Poletto-Neto, V.; Bergoli, C.D.; Cenci, M.S.; Pereira-Cenci, T. Randomized controlled trial comparing glass fiber posts and cast metal posts. J. Dent. 2020, 96, 103334. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Perlea, P.; Stefanescu, C.; Petre, A.E. Clinical Acceptance of Digitally Produced Zirconia and Metal Post and Cores, Based on the Impression Method. Clin. Pract. 2024, 14, 2533-2541. https://doi.org/10.3390/clinpract14060199
Perlea P, Stefanescu C, Petre AE. Clinical Acceptance of Digitally Produced Zirconia and Metal Post and Cores, Based on the Impression Method. Clinics and Practice. 2024; 14(6):2533-2541. https://doi.org/10.3390/clinpract14060199
Chicago/Turabian StylePerlea, Paula, Cosmin Stefanescu, and Alexandru Eugen Petre. 2024. "Clinical Acceptance of Digitally Produced Zirconia and Metal Post and Cores, Based on the Impression Method" Clinics and Practice 14, no. 6: 2533-2541. https://doi.org/10.3390/clinpract14060199
APA StylePerlea, P., Stefanescu, C., & Petre, A. E. (2024). Clinical Acceptance of Digitally Produced Zirconia and Metal Post and Cores, Based on the Impression Method. Clinics and Practice, 14(6), 2533-2541. https://doi.org/10.3390/clinpract14060199






