- Article
An Assessment of Melatonin Levels in the Saliva of Patients with Chronic Urticaria in Comparison with Their Sleep Quality and Dermatologic Quality of Life
- Iva Bešlić,
- Alen Vrtarić and
- Liborija Lugović-Mihić
- + 3 authors
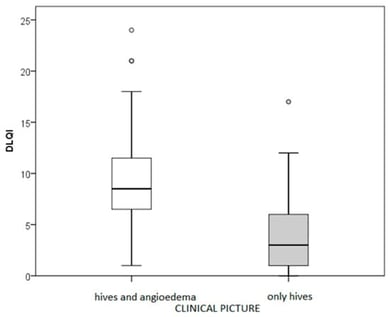
Background: For the majority of chronic spontaneous urticaria (CSU) sufferers, nocturnal itch has a profound effect on quality of life (QoL), as it leads to sleep disturbances. To ensure good sleep quality (SQ), the body must produce an adequate amount of melatonin, which regulates the sleep cycle. Methods: This study examines the levels of salivary melatonin in 38 CSU patients and 38 healthy controls, as well as the relationship between CSU severity, QoL and SQ. The Enzyme-Linked Immunosorbent Assay (ELISA), Dermatology Quality of Life Index (DLQI), and Pittsburgh Sleep Quality Index (PSQI) were used to determine salivary melatonin levels, QoL, and SQ. In addition, the CSU participants were given the Urticaria Activity Score (UAS) and the Urticaria Control Test. Results: The median value of salivary melatonin in CSU patients was lower than that in healthy individuals (0.2 vs. 15.985 pg/mL; p < 0.001). A decreased melatonin level was seen in 90% of CSU patients and 18% of healthy individuals. Individuals with lower melatonin levels were significantly more likely to have CSU compared with those with higher melatonin levels (OR = 37.6; 95% CI 10.0–141.1). Melatonin was linearly related to QoL and sleep quality in the whole sample (r = −0.606 and −0.536; p < 0.001) but not in CSU patients. Impaired QoL in patients correlated with itch intensity and the number of hives (r = 0.740 and 0.646). The severity and activity of CSU are linearly related to impaired QoL and sleep quality (r = −0.606 and −0.536; p < 0.001). Sleep quality acts as the mediator of the association between QoL and salivary melatonin, when controlling for the effect of age and gender (B = −0.347; 95% CI = −0.679 to −0.080). Conclusions: The data suggest that melatonin may be more a non-specific marker of sleep disturbance than the severity of CSU. Sleep quality may act as a mediator linking dermatology-related QoL, circadian dysregulation and reduced melatonin secretion.
6 February 2026