Manifestation of Pancytopenia Associated with COVID-19 as Paroxysmal Nocturnal Hemoglobinuria (PNH) and Aplastic Anemia (AA)
Abstract
1. Introduction
2. Methods
3. Case Series
3.1. Case 1
3.2. Case 2
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jha, P.; Brown, P.E.; Ansumana, R. Counting the global COVID-19 dead. Lancet 2022, 399, 1937–1938. [Google Scholar] [CrossRef] [PubMed]
- Rahman, A.; Niloofa, R.; Jayarajah, U.; De Mel, S.; Abeysuriya, V.; Seneviratne, S.L. Hematological Abnormalities in COVID-19: A Narrative Review. Am. J. Trop. Med. Hyg. 2021, 104, 1188–1201. [Google Scholar] [CrossRef] [PubMed]
- Hines, A.; Hakim, N.; Barrientos, J. COVID-19 infection presenting as paroxysmal nocturnal hemoglobinuria. Clin. Case Rep. 2021, 9, e04636. [Google Scholar] [CrossRef]
- Lee, N.C.J.; Patel, B.; Etra, A.; Bat, T.; Ibrahim, I.F.; Vusirikala, M.; Chen, M.; Rosado, F.; Jaso, J.M.; Young, N.S.; et al. SARS-CoV-2 infection associated with aplastic anemia and pure red cell aplasia. Blood Adv. 2022, 6, 3840–3843. [Google Scholar] [CrossRef] [PubMed]
- Otieno, S.B.; Altahan, A.; Kaweeta, F.; Karri, S.; Alnoor, F.; Johnson, R. Severe Hemolysis in a COVID-19 Patient with Paroxysmal Nocturnal Hemoglobinuria. Case Rep. Hematol. 2021, 2021, 6619177. [Google Scholar] [CrossRef] [PubMed]
- Sumbly, V.; Siddiqui, R.; Alshamam, M.; Kurbanova, T.; Rizzo, V. New Onset Aplastic Anemia after a COVID-19 Infection: A Case Report. Am. J. Med. Case Rep. 2021, 9, 451–455. [Google Scholar]
- Hill, A.; DeZern, A.E.; Kinoshita, T.; Brodsky, R.A. Paroxysmal nocturnal haemoglobinuria. Nat. Rev. Dis. Primers 2017, 3, 17028. [Google Scholar] [CrossRef] [PubMed]
- Zhu, X.F.; He, H.L.; Wang, S.Q.; Tang, J.Y.; Han, B.; Zhang, D.H.; Wu, L.Q.; Wu, D.P.; Li, W.; Xia, L.H.; et al. Current Treatment Patterns of Aplastic Anemia in China: A Prospective Cohort Registry Study. Acta Haematol. 2019, 142, 162–170. [Google Scholar] [CrossRef] [PubMed]
- Jalbert, J.J.; Chaudhari, U.; Zhang, H.; Weyne, J.; Shammo, J.M. Epidemiology of PNH and Real-World Treatment Patterns Following an Incident PNH Diagnosis in the US. Blood 2019, 134 (Suppl. S1), 3407. [Google Scholar] [CrossRef]
- Guan, W.J.; Ni, Z.Y.; Hu, Y.; Liang, W.H.; Ou, C.Q.; He, J.X.; Liu, L.; Shan, H.; Lei, C.L.; Hui, D.S.C.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef]
- Taneri, P.E.; Gómez-Ochoa, S.A.; Llanaj, E.; Raguindin, P.F.; Rojas, L.Z.; Roa-Díaz, Z.M.; Salvador, D.; Groothof, D.; Minder, B.; Kopp-Heim, D.; et al. Anemia and iron metabolism in COVID-19: A systematic review and meta-analysis. Eur. J. Epidemiol. 2020, 35, 763–773. [Google Scholar] [CrossRef] [PubMed]
- Hock, H.; Kelly, H.R.; Meyerowitz, E.A.; Frigault, M.J.; Massoth, L.R. Case 31-2021: A 21-Year-Old Man with Sore Throat, Epistaxis, and Oropharyngeal Petechiae. N. Engl. J. Med. 2021, 385, 1511–1520. [Google Scholar] [CrossRef] [PubMed]
- Chakravarthy, R.; Murphy, M.L.; Ann Thompson, M.; McDaniel, H.L.; Zarnegar-Lumley, S.; Borinstein, S.C. SARS-CoV-2 infection coincident with newly diagnosed severe aplastic anemia: A report of two cases. Pediatr. Blood Cancer 2022, 69, e29433. [Google Scholar] [CrossRef] [PubMed]
- Iannuzzi, A.; Parrella, A.; De Ritis, F.; Cammarota, A.; Berloco, L.; Paudice, F.; D’Angelo, G.; Aliberti, E.; Iannuzzo, G. Pancytopenia in a Case of Aplastic Anaemia/Paroxysmal Nocturnal Haemoglobinuria Unmasked by SARS-CoV-2 Infection: A Case Report. Medicina 2022, 58, 1282. [Google Scholar] [CrossRef] [PubMed]
- Avenoso, D.; Marsh, J.C.W.; Potter, V.; Pagliuca, A.; Slade, S.; Dignan, F.; Tholouli, E.; Mittal, S.; Davis, B.; Tauro, S.; et al. SARS-CoV-2 infection in aplastic anemia. Haematologica 2022, 107, 541–543. [Google Scholar] [CrossRef] [PubMed]
- Fara, A.; Mitrev, Z.; Rosalia, R.A.; Assas, B.M. Cytokine storm and COVID-19: A chronicle of pro-inflammatory cytokines. Open Biol. 2020, 10, 200160. [Google Scholar] [CrossRef] [PubMed]
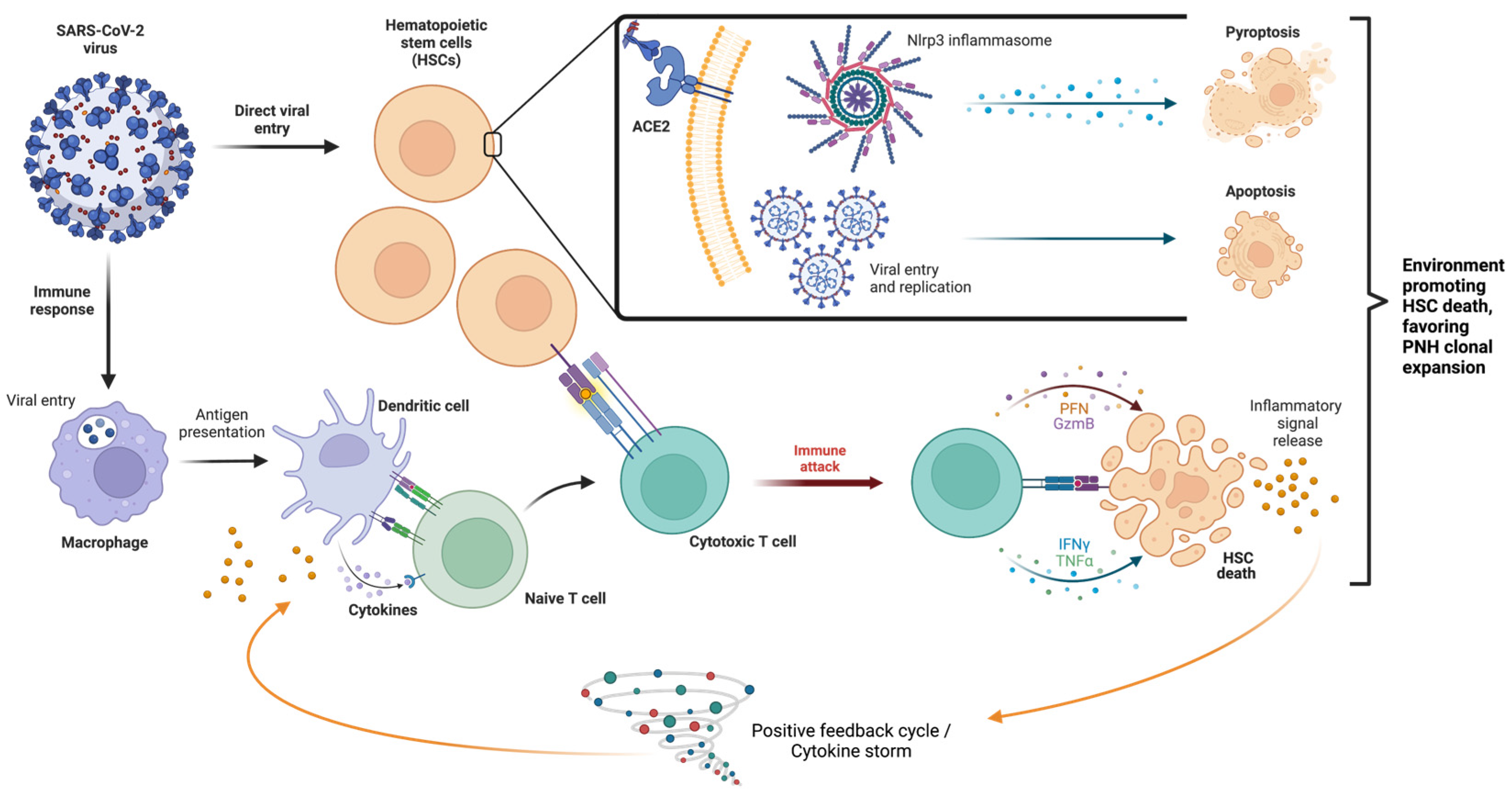
- Ratajczak, M.Z.; Kucia, M. SARS-CoV-2 infection and overactivation of Nlrp3 inflammasome as a trigger of cytokine “storm” and risk factor for damage of hematopoietic stem cells. Leukemia 2020, 34, 1726–1729. [Google Scholar] [CrossRef] [PubMed]
- Kucia, M.; Ratajczak, J.; Bujko, K.; Adamiak, M.; Ciechanowicz, A.; Chumak, V.; Brzezniakiewicz-Janus, K.; Ratajczak, M.Z. An evidence that SARS-CoV-2/COVID-19 spike protein (SP) damages hematopoietic stem/progenitor cells in the mechanism of pyroptosis in Nlrp3 inflammasome-dependent manner. Leukemia 2021, 35, 3026–3029. [Google Scholar] [CrossRef] [PubMed]
- Zeng, Y.; Katsanis, E. The complex pathophysiology of acquired aplastic anaemia. Clin. Exp. Immunol. 2015, 180, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Fattizzo, B.; Ireland, R.; Dunlop, A.; Yallop, D.; Kassam, S.; Large, J.; Gandhi, S.; Muus, P.; Manogaran, C.; Sanchez, K.; et al. Clinical and prognostic significance of small paroxysmal nocturnal hemoglobinuria clones in myelodysplastic syndrome and aplastic anemia. Leukemia 2021, 35, 3223–3231. [Google Scholar] [CrossRef]

| Variable | Patient Case | ||
|---|---|---|---|
| 1 | 2 | ||
| Age | 21 | 52 | |
| Sex | Male | Female | |
| Interval between COVID infection and pancytopenia | 4 months | 1 month | |
| CBC | WBC | 4.1 | 3.0 |
| ANC | 1.2 | 0.9 | |
| Platelets | 34 | 18 | |
| HGB | 9.3 | 11.6 | |
| MCV | 106.2 | 94 | |
| Bone Marrow Biopsy Cellularity | 10–20% | 10–15% | |
| PNH clones | Granulocytes | 19.53% | N/A |
| Monocytes | 19.77% | 0.5% | |
| RBCs | 3.61% | N/A | |
| History of autoimmune disease | None | Anterior uveitis | |
| SARS-CoV-2 Vaccination | None | Johnson and Johnson/Janssen Seven months later, Pfizer–BioNtech booster | |
| Treatment | Ravulizumab | N/A | |
| Clinical Data | Diagnosis | Bone Marrow Biopsy Cellularity | Onset of Cytopenia after COVID Infection | AA/PNH Therapy | COVID-19 Treatment | Reference(s) |
|---|---|---|---|---|---|---|
| 21, M * | Hemolytic PNH/aplastic anemia | 10–20% | 4 months | Ravulizumab | Supportive | This report |
| 52, F * | Aplastic anemia (with subclinical PNH clones) | 10–15% | 1 month | Observation | Paxlovid | This report |
| 35, M | Hemolytic PNH | Normal | 0 days ‡ | Eculizumab, transfusion support | 3-day course of pulse steroids, and IVIG | [3] |
| 22, F | Severe aplastic anemia | 5% | 10 days | Sibling HSCT | Supportive | [4] |
| 69, F | Severe aplastic anemia | 5–10% | 2 days | Cyclosporine, antithymocyte globulin, eltrombopag | Supportive | [4] |
| 76, M | Pure red cell aplasia | 20–30% | 4 months | Cyclosporine | Supportive | [4] |
| 21, M | Severe aplastic anemia (with subclinical PNH clones) | <5% | <1 month | Cyclosporine, antithymocyte globulin, eltrombopag, eculizumab † | Supportive | [4] |
| 69, F | Severe aplastic anemia (with subclinical PNH clones) | 5% | 5 months | Cyclosporine, antithymocyte globulin, eltrombopag | Supportive | [4] |
| 19, F | Hemolytic PNH | 40–50% § | 0 days ‡ | Eculizumab, Ravulizumab | Supportive | [5] |
| 28, F | Severe aplastic anemia | 20–30% | 3 months | Cyclosporine, antithymocyte globulin, eltrombopag, prednisone | Supportive | [4,6] |
| 21, M | Severe aplastic anemia | <5% | 2 months | Sibling HSCT | Supportive | [12] |
| 12, F | Severe aplastic anemia | 10% | 0 days ‡ | Antithymocyte globulin, cyclosporine | Paxlovid | [13] |
| 18, M | Severe aplastic anemia | 10% | 0 days ‡ | Antithymocyte globulin, cyclosporine | Supportive | [13] |
| 78, F | Hemolytic PNH/aplastic anemia | Poor | 0 days ‡ | -- || | Supportive | [14] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aguilar, J.J.; Dhillon, V.; Balasubramanian, S. Manifestation of Pancytopenia Associated with COVID-19 as Paroxysmal Nocturnal Hemoglobinuria (PNH) and Aplastic Anemia (AA). Hematol. Rep. 2024, 16, 42-49. https://doi.org/10.3390/hematolrep16010005
Aguilar JJ, Dhillon V, Balasubramanian S. Manifestation of Pancytopenia Associated with COVID-19 as Paroxysmal Nocturnal Hemoglobinuria (PNH) and Aplastic Anemia (AA). Hematology Reports. 2024; 16(1):42-49. https://doi.org/10.3390/hematolrep16010005
Chicago/Turabian StyleAguilar, Jeff Justin, Vikram Dhillon, and Suresh Balasubramanian. 2024. "Manifestation of Pancytopenia Associated with COVID-19 as Paroxysmal Nocturnal Hemoglobinuria (PNH) and Aplastic Anemia (AA)" Hematology Reports 16, no. 1: 42-49. https://doi.org/10.3390/hematolrep16010005
APA StyleAguilar, J. J., Dhillon, V., & Balasubramanian, S. (2024). Manifestation of Pancytopenia Associated with COVID-19 as Paroxysmal Nocturnal Hemoglobinuria (PNH) and Aplastic Anemia (AA). Hematology Reports, 16(1), 42-49. https://doi.org/10.3390/hematolrep16010005







