Biodegradable Iron-Based Materials—What Was Done and What More Can Be Done?
Abstract
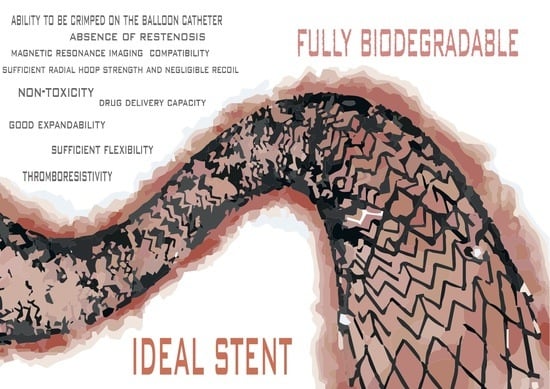
1. Introduction
2. Biodegradability of Pure Iron
- (1)
- Proteins: All pseudo-physiological fluids are designed to simulate the pH and ionic concentrations of blood plasma. However, they do not contain proteins, which are the most important component of blood plasma. Proteins can bind metal ions and then transport them from the implant surface, but also they could create a layer of adsorbed proteins, which then works as a barrier between the metal surface of the stent and the environment, thus inhibiting biodegradation. This same layer in slightly different conditions could also limit the diffusion of oxygen to certain regions of the surface and, in this way, cause a breakdown of the passive layer and preferential corrosion of oxygen-deficient regions [37].
- (2)
- Atmosphere: most degradation tests are carried out in air. However, in blood vessels, there is an atmosphere containing around 5% of CO2, whose influence could change the type of degradation products [38].
- (3)
- Cells: During healing of the wound caused by the implantation operation, the surface of the implant is covered with a layer of cells after a few weeks. When the barrier formation is complete, the implant functions in a different environment than before. This may be the main reason for the differences in long-term in vivo and in vitro corrosion [25].
- (4)
- Dissolved oxygen: Blood has about 3 cm3/dm3 of dissolved oxygen, (4.3 mg/dm3) while, for example, most solutions used in cell-based tests (Hank’s solution) have almost twice the level of dissolved oxygen—about 8 mg/dm3. This factor is probably the most important of all, and nevertheless it is very often omitted when simulating corrosion [35].
Corrosion Tests In Vitro
3. Iron Metabolism
4. Biological Properties of Iron-Based Materials
4.1. Cellular Biocompatibility
4.2. Tissue Biocompatibility
4.3. Hemocompatibility
4.4. Clinical Biocompatibility
5. Production of Iron Biodegradable Devices
5.1. Spark Plasma Sintering (SPS)
5.2. Vacuum Induction Melting (VIM)
5.3. Vacuum Arc Melting (VAM)
5.4. Electroforming
5.5. Powder Metallurgy (PM)
5.6. Mechanical Treatments, Inducing Plastic Deformation
5.7. Template-Based Formation of Porous Material
5.8. 3D Printing of Iron Materials
6. Iron Materials Modifications
6.1. Additions
6.2. Iron-Manganese Alloys
- (1)
- (2)
- (3)
- Elements from the second group, Mg and Ca, have strong negative electrochemical potentials (Mg = −2.38 V vs. SHE, Ca = −2.76 V vs. SHE). In addition to a Fe-Mn matrix creates alloys possessing active corrosion potentials. After analysing Tafel curves, Hong et al. suggested that the Fe-Mn-Ca alloys have a greater tendency to corrode than the Fe-Mn-Mg alloys [133].
- (4)
6.3. Surface Modification
6.4. Coatings
6.5. Drug Delivery from Iron-Based Stents
7. Conclusions and Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lloyd-Jones, D.; Adams, R.; Carnethon, M.; De Simone, G.; Ferguson, T.B.; Flegal, K.; Ford, E.; Furie, K.; Go, A.; Greenlund, K.; et al. Heart Disease and Stroke Statistics—2009 Update: A Report From the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2009, 119, e21–e181. [Google Scholar] [CrossRef] [PubMed]
- Byrne, R.A.; Stone, G.W.; Ormiston, J.; Kastrati, A. Coronary Balloon Angioplasty, Stents, and Scaffolds. Lancet 2017, 390, 781–792. [Google Scholar] [CrossRef]
- Garg, S.; Serruys, P.W. Coronary Stents. J. Am. Coll. Cardiol. 2010, 56, S43–S78. [Google Scholar] [CrossRef] [PubMed]
- Tan, C.; Schatz, R.A. The History of Coronary Stenting. Interv. Cardiol. Clin. 2016, 5, 271–280. [Google Scholar] [CrossRef]
- Sigwart, U.; Puel, J.; Mirkovitch, V.; Joffre, F.; Kappenberger, L. Intravascular Stents to Prevent Occlusion and Re-Stenosis after Transluminal Angioplasty. N. Engl. J. Med. 1987, 316, 701–706. [Google Scholar] [CrossRef]
- Mani, G.; Feldman, M.D.; Patel, D.; Agrawal, C.M. Coronary Stents: A Materials Perspective. Biomaterials 2007, 28, 1689–1710. [Google Scholar] [CrossRef]
- Chesta, F.; Rizvi, Z.H.; Oberoi, M.; Buttar, N. The Role of Stenting in Patients with Variceal Bleeding. Tech. Innov. Gastrointest. Endosc. 2020, 22, 205–211. [Google Scholar] [CrossRef]
- Law, M.A.; Shamszad, P.; Nugent, A.W.; Justino, H.; Breinholt, J.P.; Mullins, C.E.; Ing, F.F. Pulmonary Artery Stents: Long-Term Follow-Up. Catheter. Cardiovasc. Interv. 2010, 75, 757–764. [Google Scholar] [CrossRef]
- Breinholt, J.P.; Nugent, A.W.; Law, M.A.; Justino, H.; Mullins, C.E.; Ing, F.F. Stent Fractures in Congenital Heart Disease. Catheter. Cardiovasc. Interv. 2008, 72, 977–982. [Google Scholar] [CrossRef]
- Lejay, A.; Koncar, I.; Diener, H.; de Ceniga, V.M.; Chakfé, N. Post-Operative Infection of Prosthetic Materials or Stents Involving the Supra-Aortic Trunks: A Comprehensive Review. Eur. J. Vasc. Endovasc. Surg. 2018, 56, 885–900. [Google Scholar] [CrossRef]
- Zheng, Y.; Yang, H. Manufacturing of cardiovascular stents. In Metallic Biomaterials Processing and Medical Device Manufacturing; Elsevier: Amsterdam, The Netherlands, 2020; pp. 317–340. ISBN 978-0-08-102965-7. [Google Scholar]
- Reddy, S.R.V.; Welch, T.R.; Nugent, A.W. Biodegradable Stent Use for Congenital Heart Disease. Prog. Pediatr. Cardiol. 2021, 61, 101349. [Google Scholar] [CrossRef]
- Tamai, H.; Igaki, K.; Kyo, E.; Kosuga, K.; Kawashima, A.; Matsui, S.; Komori, H.; Tsuji, T.; Motohara, S.; Uehata, H. Initial and 6-Month Results of Biodegradable Poly-l-Lactic Acid Coronary Stents in Humans. Circulation 2000, 102, 399–404. [Google Scholar] [CrossRef]
- Campos, C.A.; Zhang, Y.-J.; Bourantas, C.V.; Muramatsu, T.; Garcia-Garcia, H.M.; Lemos, P.A.; Iqbal, J.; Onuma, Y.; Serruys, P.W. Bioresorbable Vascular Scaffolds in the Clinical Setting. Interv. Cardiol. 2013, 5, 639–646. [Google Scholar] [CrossRef]
- Abizaid, A.; Carrié, D.; Frey, N.; Lutz, M.; Weber-Albers, J.; Dudek, D.; Chevalier, B.; Weng, S.-C.; Costa, R.A.; Anderson, J.; et al. 6-Month Clinical and Angiographic Outcomes of a Novel Radiopaque Sirolimus-Eluting Bioresorbable Vascular Scaffold. JACC Cardiovasc. Interv. 2017, 10, 1832–1838. [Google Scholar] [CrossRef]
- McMahon, S.; Bertollo, N.; Cearbhaill, E.D.O.; Salber, J.; Pierucci, L.; Duffy, P.; Dürig, T.; Bi, V.; Wang, W. Bio-Resorbable Polymer Stents: A Review of Material Progress and Prospects. Prog. Polym. Sci. 2018, 83, 79–96. [Google Scholar] [CrossRef]
- Zhao, F.; Sun, J.; Xue, W.; Wang, F.; King, M.W.; Yu, C.; Jiao, Y.; Sun, K.; Wang, L. Development of a Polycaprolactone/Poly(p-Dioxanone) Bioresorbable Stent with Mechanically Self-Reinforced Structure for Congenital Heart Disease Treatment. Bioact. Mater. 2021, 6, 2969–2982. [Google Scholar] [CrossRef]
- Qi, Y.; Qi, H.; He, Y.; Lin, W.; Li, P.; Qin, L.; Hu, Y.; Chen, L.; Liu, Q.; Sun, H.; et al. Strategy of Metal–Polymer Composite Stent to Accelerate Biodegradation of Iron-Based Biomaterials. ACS Appl. Mater. Interfaces 2018, 10, 182–192. [Google Scholar] [CrossRef]
- Beshchasna, N.; Saqib, M.; Kraskiewicz, H.; Wasyluk, Ł.; Kuzmin, O.; Duta, O.C.; Ficai, D.; Ghizdavet, Z.; Marin, A.; Ficai, A.; et al. Recent Advances in Manufacturing Innovative Stents. Pharmaceutics 2020, 12, 349. [Google Scholar] [CrossRef]
- Dong, H.; Lin, F.; Boccaccini, A.R.; Virtanen, S. Corrosion Behavior of Biodegradable Metals in Two Different Simulated Physiological Solutions: Comparison of Mg, Zn and Fe. Corros. Sci. 2021, 182, 109278. [Google Scholar] [CrossRef]
- Qin, Y.; Wen, P.; Guo, H.; Xia, D.; Zheng, Y.; Jauer, L.; Poprawe, R.; Voshage, M.; Schleifenbaum, J.H. Additive Manufacturing of Biodegradable Metals: Current Research Status and Future Perspectives. Acta Biomater. 2019, 98, 3–22. [Google Scholar] [CrossRef]
- Li, Y.; Jahr, H.; Zhou, J.; Zadpoor, A.A. Additively Manufactured Biodegradable Porous Metals. Acta Biomater. 2020, 115, 29–50. [Google Scholar] [CrossRef] [PubMed]
- Zartner, P.; Cesnjevar, R.; Singer, H.; Weyand, M. First Successful Implantation of a Biodegradable Metal Stent into the Left Pulmonary Artery of a Preterm Baby. Catheter. Cardiovasc. Interv. 2005, 66, 590–594. [Google Scholar] [CrossRef] [PubMed]
- Bowen, P.K.; Shearier, E.R.; Zhao, S.; Guillory, R.J.; Zhao, F.; Goldman, J.; Drelich, J.W. Biodegradable Metals for Cardiovascular Stents: From Clinical Concerns to Recent Zn-Alloys. Adv. Healthc. Mater. 2016, 5, 1121–1140. [Google Scholar] [CrossRef] [PubMed]
- Loffredo, S.; Paternoster, C.; Mantovani, D. Iron-Based Degradable Implants. In Encyclopedia of Biomedical Engineering; Elsevier: Amsterdam, The Netherlands, 2019; pp. 374–385. ISBN 978-0-12-805144-3. [Google Scholar]
- Zhou, Y.; Wu, P.; Yang, Y.; Gao, D.; Feng, P.; Gao, C.; Wu, H.; Liu, Y.; Bian, H.; Shuai, C. The Microstructure, Mechanical Properties and Degradation Behavior of Laser-Melted Mg Sn Alloys. J. Alloys Compd. 2016, 687, 109–114. [Google Scholar] [CrossRef]
- Ng, C.C.; Savalani, M.M.; Lau, M.L.; Man, H.C. Microstructure and Mechanical Properties of Selective Laser Melted Magnesium. Appl. Surf. Sci. 2011, 257, 7447–7454. [Google Scholar] [CrossRef]
- Wen, P.; Voshage, M.; Jauer, L.; Chen, Y.; Qin, Y.; Poprawe, R.; Schleifenbaum, J.H. Laser Additive Manufacturing of Zn Metal Parts for Biodegradable Applications: Processing, Formation Quality and Mechanical Properties. Mater. Des. 2018, 155, 36–45. [Google Scholar] [CrossRef]
- Song, B.; Dong, S.; Deng, S.; Liao, H.; Coddet, C. Microstructure and Tensile Properties of Iron Parts Fabricated by Selective Laser Melting. Opt. Laser Technol. 2014, 56, 451–460. [Google Scholar] [CrossRef]
- Song, B.; Dong, S.; Liu, Q.; Liao, H.; Coddet, C. Vacuum Heat Treatment of Iron Parts Produced by Selective Laser Melting: Microstructure, Residual Stress and Tensile Behavior. Mater. Des. 1980–2015 2014, 54, 727–733. [Google Scholar] [CrossRef]
- Peuster, M. A Novel Approach to Temporary Stenting: Degradable Cardiovascular Stents Produced from Corrodible Metal—Results 6–18 Months after Implantation into New Zealand White Rabbits. Heart 2001, 86, 563–569. [Google Scholar] [CrossRef]
- Revie, R.W.; Uhlig, H.H. Corrosion and Corrosion Control: An Introduction to Corrosion Science and Engineering; Wiley: Hoboken, NJ, USA, 2008; ISBN 978-0-470-27725-6. [Google Scholar]
- Zhu, S.; Huang, N.; Xu, L.; Zhang, Y.; Liu, H.; Sun, H.; Leng, Y. Biocompatibility of Pure Iron: In Vitro Assessment of Degradation Kinetics and Cytotoxicity on Endothelial Cells. Mater. Sci. Eng. C 2009, 29, 1589–1592. [Google Scholar] [CrossRef]
- Ulum, M.F.; Arafat, A.; Noviana, D.; Yusop, A.H.; Nasution, A.K.; Kadir, A.M.R.; Hermawan, H. In Vitro and in Vivo Degradation Evaluation of Novel Iron-Bioceramic Composites for Bone Implant Applications. Mater. Sci. Eng. C 2014, 36, 336–344. [Google Scholar] [CrossRef]
- Qi, Y.; Li, X.; He, Y.; Zhang, D.; Ding, J. Mechanism of Acceleration of Iron Corrosion by a Polylactide Coating. ACS Appl. Mater. Interfaces 2019, 11, 202–218. [Google Scholar] [CrossRef]
- Kraus, T.; Moszner, F.; Fischerauer, S.; Fiedler, M.; Martinelli, E.; Eichler, J.; Witte, F.; Willbold, E.; Schinhammer, M.; Meischel, M.; et al. Biodegradable Fe-Based Alloys for Use in Osteosynthesis: Outcome of an in Vivo Study after 52 weeks. Acta Biomater. 2014, 10, 3346–3353. [Google Scholar] [CrossRef]
- Pierson, D.; Edick, J.; Tauscher, A.; Pokorney, E.; Bowen, P.; Gelbaugh, J.; Stinson, J.; Getty, H.; Lee, C.H.; Drelich, J.; et al. A Simplified in Vivo Approach for Evaluating the Bioabsorbable Behavior of Candidate Stent Materials. J. Biomed. Mater. Res. B Appl. Biomater. 2012, 100B, 58–67. [Google Scholar] [CrossRef]
- Mouzou, E.; Paternoster, C.; Tolouei, R.; Chevallier, P.; Biffi, C.A.; Tuissi, A.; Mantovani, D. CO2-Rich Atmosphere Strongly Affects the Degradation of Fe-21Mn-1C for Biodegradable Metallic Implants. Mater. Lett. 2016, 181, 362–366. [Google Scholar] [CrossRef]
- J01 Committee. Guide for Laboratory Immersion Corrosion Testing of Metals; ASTM International: West Conshohocken, PA, USA, 2012. [Google Scholar]
- G01 Committee. Test Method for Conducting Potentiodynamic Polarization Resistance Measurements; ASTM International: West Conshohocken, PA, USA, 2009. [Google Scholar]
- G01 Committee. Practice for Verification of Algorithm and Equipment for Electrochemical Impedance Measurements; ASTM International: West Conshohocken, PA, USA, 2015. [Google Scholar]
- Papanikolaou, G.; Pantopoulos, K. Iron Metabolism and Toxicity. Toxicol. Appl. Pharmacol. 2005, 202, 199–211. [Google Scholar] [CrossRef]
- Uchmanowicz, I. Oxidative Stress, Frailty and Cardiovascular Diseases: Current Evidence. In Frailty and Cardiovascular Diseases; Veronese, N., Ed.; Advances in Experimental Medicine and Biology; Springer International Publishing: Cham, Switzerland, 2020; Volume 1216, pp. 65–77. ISBN 978-3-030-33329-4. [Google Scholar]
- Andrews, N.C. Iron Deficiency and Iron Overload. Annu. Rev. Genom. Hum. Genet. 2000, 1, 75–98. [Google Scholar] [CrossRef]
- Andrews, N.C. Disorders of Iron Metabolism. N. Engl. J. Med. 1999, 341, 1986–1995. [Google Scholar] [CrossRef]
- Pivina, L.; Semenova, Y.; Doşa, M.D.; Dauletyarova, M.; Bjørklund, G. Iron Deficiency, Cognitive Functions, and Neurobehavioral Disorders in Children. J. Mol. Neurosci. 2019, 68, 1–10. [Google Scholar] [CrossRef]
- Georgieff, M.K. Iron Deficiency in Pregnancy. Am. J. Obstet. Gynecol. 2020, 223, 516–524. [Google Scholar] [CrossRef]
- Muckenthaler, M.U.; Rivella, S.; Hentze, M.W.; Galy, B. A Red Carpet for Iron Metabolism. Cell 2017, 168, 344–361. [Google Scholar] [CrossRef] [PubMed]
- Boutrand, J.-P. (Ed.) Biocompatibility and Performance of Medical Devices; Woodhead Publishing Series in Biomaterials; Woodhead Publishing: Philadelphia, PA, USA, 2012; ISBN 978-0-85709-070-6. [Google Scholar]
- Virtanen, S. Corrosion of Biomedical Implant Materials. Corros. Rev. 2008, 26, 148–171. [Google Scholar] [CrossRef]
- Huang, T.; Cheng, Y.; Zheng, Y. In Vitro Studies on Silver Implanted Pure Iron by Metal Vapor Vacuum Arc Technique. Colloids Surf. B Biointerfaces 2016, 142, 20–29. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.; Zheng, Y.F. In Vitro Study on Newly Designed Biodegradable Fe-X Composites (X = W, CNT) Prepared by Spark Plasma Sintering. J. Biomed. Mater. Res. B Appl. Biomater. 2013, 101B, 485–497. [Google Scholar] [CrossRef]
- Čapek, J.; Msallamová, Š.; Jablonská, E.; Lipov, J.; Vojtěch, D. A Novel High-Strength and Highly Corrosive Biodegradable Fe-Pd Alloy: Structural, Mechanical and in Vitro Corrosion and Cytotoxicity Study. Mater. Sci. Eng. C 2017, 79, 550–562. [Google Scholar] [CrossRef]
- Liu, B.; Zheng, Y.F.; Ruan, L. In Vitro Investigation of Fe30Mn6Si Shape Memory Alloy as Potential Biodegradable Metallic Material. Mater. Lett. 2011, 65, 540–543. [Google Scholar] [CrossRef]
- Paim, T.C.; Wermuth, D.P.; Bertaco, I.; Zanatelli, C.; Naasani, L.I.S.; Slaviero, M.; Driemeier, D.; Schaeffer, L.; Wink, M.R. Evaluation of in Vitro and in Vivo Biocompatibility of Iron Produced by Powder Metallurgy. Mater. Sci. Eng. C 2020, 115, 111129. [Google Scholar] [CrossRef]
- Eliaz, N. Corrosion of Metallic Biomaterials: A Review. Materials 2019, 12, 407. [Google Scholar] [CrossRef]
- Swinney, D.C. Molecular Mechanism of Action (MMoA) in Drug Discovery. In Annual Reports in Medicinal Chemistry; Elsevier: Amsterdam, The Netherlands, 2011; Volume 46, pp. 301–317. ISBN 978-0-12-386009-5. [Google Scholar]
- Anderson, J.M.; Rodriguez, A.; Chang, D.T. Foreign Body Reaction to Biomaterials. Semin. Immunol. 2008, 20, 86–100. [Google Scholar] [CrossRef]
- Waksman, R.; Pakala, R.; Baffour, R.; Seabron, R.; Hellinga, D.; Tio, F.O. Short-Term Effects of Biocorrodible Iron Stents in Porcine Coronary Arteries. J. Intervent. Cardiol. 2008, 21, 15–20. [Google Scholar] [CrossRef]
- Liu, Y.; Zheng, Y.; Chen, X.; Yang, J.; Pan, H.; Chen, D.; Wang, L.; Zhang, J.; Zhu, D.; Wu, S.; et al. Fundamental Theory of Biodegradable Metals—Definition, Criteria, and Design. Adv. Funct. Mater. 2019, 29, 1805402. [Google Scholar] [CrossRef]
- F04 Committee. Practice for Assessment of Hemolytic Properties of Materials; ASTM International: West Conshohocken, PA, USA, 2017. [Google Scholar]
- Cheng, J.; Huang, T.; Zheng, Y.F. Microstructure, Mechanical Property, Biodegradation Behavior, and Biocompatibility of Biodegradable Fe-Fe2O3 Composites: Biodegradable Fe-Fe2O3 Composites. J. Biomed. Mater. Res. A 2014, 102, 2277–2287. [Google Scholar] [CrossRef]
- Cheng, J.; Huang, T.; Zheng, Y.F. Relatively Uniform and Accelerated Degradation of Pure Iron Coated with Micro-Patterned Au Disc Arrays. Mater. Sci. Eng. C 2015, 48, 679–687. [Google Scholar] [CrossRef]
- Sharma, P.; Jain, K.G.; Pandey, P.M.; Mohanty, S. In Vitro Degradation Behaviour, Cytocompatibility and Hemocompatibility of Topologically Ordered Porous Iron Scaffold Prepared Using 3D Printing and Pressureless Microwave Sintering. Mater. Sci. Eng. C 2020, 106, 110247. [Google Scholar] [CrossRef]
- Oriňaková, R.; Gorejová, R.; Králová, Z.O.; Haverová, L.; Oriňak, A.; Maskaľová, I.; Kupková, M.; Džupon, M.; Baláž, M.; Hrubovčáková, M.; et al. Evaluation of Mechanical Properties and Hemocompatibility of Open Cell Iron Foams with Polyethylene Glycol Coating. Appl. Surf. Sci. 2020, 505, 144634. [Google Scholar] [CrossRef]
- Králová, Z.O.; Gorejová, R.; Oriňaková, R.; Petráková, M.; Oriňak, A.; Kupková, M.; Hrubovčáková, M.; Sopčák, T.; Baláž, M.; Maskaľová, I.; et al. Biodegradable Zinc-Iron Alloys: Complex Study of Corrosion Behavior, Mechanical Properties and Hemocompatibility. Prog. Nat. Sci. Mater. Int. 2021, 31, 279–287. [Google Scholar] [CrossRef]
- Huang, T.; Zheng, Y.; Han, Y. Accelerating Degradation Rate of Pure Iron by Zinc Ion Implantation. Regen. Biomater. 2016, 3, 205–215. [Google Scholar] [CrossRef]
- Fântânariu, M.; Trincă, L.C.; Solcan, C.; Trofin, A.; Strungaru, Ş.; Şindilar, E.V.; Plăvan, G.; Stanciu, S. A New Fe–Mn–Si Alloplastic Biomaterial as Bone Grafting Material: In Vivo Study. Appl. Surf. Sci. 2015, 352, 129–139. [Google Scholar] [CrossRef]
- Traverson, M.; Eiden, M.; Stanciu, L.; Nauman, E. In Vivo Evaluation of Biodegradability AndBiocompatibility of Fe30Mn Alloy. Vet. Comp. Orthop. Traumatol. 2017, 31, 10–16. [Google Scholar] [CrossRef]
- Lin, W.; Qin, L.; Qi, H.; Zhang, D.; Zhang, G.; Gao, R.; Qiu, H.; Xia, Y.; Cao, P.; Wang, X.; et al. Long-Term in Vivo Corrosion Behavior, Biocompatibility and Bioresorption Mechanism of a Bioresorbable Nitrided Iron Scaffold. Acta Biomater. 2017, 54, 454–468. [Google Scholar] [CrossRef]
- Drynda, A.; Hassel, T.; Bach, F.W.; Peuster, M. In Vitro and in Vivo Corrosion Properties of New Iron–Manganese Alloys Designed for Cardiovascular Applications. J. Biomed. Mater. Res. B Appl. Biomater. 2015, 103, 649–660. [Google Scholar] [CrossRef] [PubMed]
- Dargusch, M.S.; Venezuela, J.; Dehghan-Manshadi, A.; Johnston, S.; Yang, N.; Mardon, K.; Lau, C.; Allavena, R. In Vivo Evaluation of Bioabsorbable Fe-35Mn-1Ag: First Reports on In Vivo Hydrogen Gas Evolution in Fe-Based Implants. Adv. Healthc. Mater. 2021, 10, 2000667. [Google Scholar] [CrossRef] [PubMed]
- Mandal, S.; Ummadi, R.; Bose, M.; Balla, V.K.; Roy, M. Fe–Mn–Cu Alloy as Biodegradable Material with Enhanced Antimicrobial Properties. Mater. Lett. 2019, 237, 323–327. [Google Scholar] [CrossRef]
- Mitchell, B.S. An Introduction to Materials Engineering and Science for Chemical and Materials Engineers; John Wiley: Hoboken, NJ, USA, 2004; ISBN 978-0-471-43623-2. [Google Scholar]
- Ratner, B.D. (Ed.) Biomaterials Science: An Introduction to Materials in Medicine, 3rd ed.; Elsevier: Amsterdam, The Netherlands; Academic Press: Boston, MA, USA, 2013; ISBN 978-0-12-374626-9. [Google Scholar]
- Garbiec, D. Iskrowe Spiekanie Plazmowe (SPS): Teoria i Praktyka. Inż. Mater. 2015, 1, 10–14. [Google Scholar] [CrossRef]
- Huang, T.; Cheng, J.; Zheng, Y.F. In Vitro Degradation and Biocompatibility of Fe–Pd and Fe–Pt Composites Fabricated by Spark Plasma Sintering. Mater. Sci. Eng. C 2014, 35, 43–53. [Google Scholar] [CrossRef]
- Liu, B.; Zheng, Y.F. Effects of Alloying Elements (Mn, Co, Al, W, Sn, B, C and S) on Biodegradability and in Vitro Biocompatibility of Pure Iron. Acta Biomater. 2011, 7, 1407–1420. [Google Scholar] [CrossRef]
- ASM International; Stefanescu, D.M. ASM Handbook 4: Casting, 10th ed.; ASM International, Ed.; ASM International: Novelty, OH, USA, 1998; ISBN 978-0-87170-021-6. [Google Scholar]
- Schinhammer, M.; Steiger, P.; Moszner, F.; Löffler, J.F.; Uggowitzer, P.J. Degradation Performance of Biodegradable FeMnC(Pd) Alloys. Mater. Sci. Eng. C 2013, 33, 1882–1893. [Google Scholar] [CrossRef]
- Mathabathe, M.N.; Bolokang, A.S.; Govender, G.; Siyasiya, C.W.; Mostert, R.J. Cold-Pressing and Vacuum Arc Melting of γ-TiAl Based Alloys. Adv. Powder Technol. 2019, 30, 2925–2939. [Google Scholar] [CrossRef]
- Wang, Y.B.; Li, H.F.; Zheng, Y.F.; Li, M. Corrosion Performances in Simulated Body Fluids and Cytotoxicity Evaluation of Fe-Based Bulk Metallic Glasses. Mater. Sci. Eng. C 2012, 32, 599–606. [Google Scholar] [CrossRef]
- Drevet, R.; Zhukova, Y.; Malikova, P.; Dubinskiy, S.; Korotitskiy, A.; Pustov, Y.; Prokoshkin, S. Martensitic Transformations and Mechanical and Corrosion Properties of Fe-Mn-Si Alloys for Biodegradable Medical Implants. Metall. Mater. Trans. A 2018, 49, 1006–1013. [Google Scholar] [CrossRef]
- Moravej, M.; Purnama, A.; Fiset, M.; Couet, J.; Mantovani, D. Electroformed Pure Iron as a New Biomaterial for Degradable Stents: In Vitro Degradation and Preliminary Cell Viability Studies. Acta Biomater. 2010, 6, 1843–1851. [Google Scholar] [CrossRef]
- Hermawan, H.; Dubé, D.; Mantovani, D. Degradable Metallic Biomaterials: Design and Development of Fe-Mn Alloys for Stents. J. Biomed. Mater. Res. A 2009, 93, 1–11. [Google Scholar] [CrossRef]
- Schaffer, J.E.; Nauman, E.A.; Stanciu, L.A. Cold Drawn Bioabsorbable Ferrous and Ferrous Composite Wires: An Evaluation of in Vitro Vascular Cytocompatibility. Acta Biomater. 2013, 9, 8574–8584. [Google Scholar] [CrossRef] [PubMed]
- Alavi, R.; Trenggono, A.; Champagne, S.; Hermawan, H. Investigation on Mechanical Behavior of Biodegradable Iron Foams under Different Compression Test Conditions. Metals 2017, 7, 202. [Google Scholar] [CrossRef]
- Ray, S.; Thormann, U.; Eichelroth, M.; Budak, M.; Biehl, C.; Rupp, M.; Sommer, U.; El Khassawna, T.; Alagboso, F.I.; Kampschulte, M.; et al. Strontium and Bisphosphonate Coated Iron Foam Scaffolds for Osteoporotic Fracture Defect Healing. Biomaterials 2018, 157, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Čapek, J.; Kubasek, J.; Vojtěch, D. Microstructural, Mechanical, Corrosion and Cytotoxicity Characterization of the Hot Forged FeMn30 (Wt.%) Alloy. Mater. Sci. Eng. C 2016, 58, 900–908. [Google Scholar] [CrossRef]
- Li, Y.; Jahr, H.; Lietaert, K.; Pavanram, P.; Yilmaz, A.; Fockaert, L.I.; Leeflang, M.A.; Pouran, B.; Gonzalez-Garcia, Y.; Weinans, H.; et al. Additively Manufactured Biodegradable Porous Iron. Acta Biomater. 2018, 77, 380–393. [Google Scholar] [CrossRef]
- Heiden, M.; Nauman, E.; Stanciu, L. Bioresorbable Fe-Mn and Fe-Mn-HA Materials for Orthopedic Implantation: Enhancing Degradation through Porosity Control. Adv. Healthc. Mater. 2017, 6, 1700120. [Google Scholar] [CrossRef]
- Zhang, Q.; Cao, P. Degradable Porous Fe-35 wt.% Mn Produced via Powder Sintering from NH4HCO3 Porogen. Mater. Chem. Phys. 2015, 163, 394–401. [Google Scholar] [CrossRef]
- Panwar, A.; Tan, L. Current Status of Bioinks for Micro-Extrusion-Based 3D Bioprinting. Molecules 2016, 21, 685. [Google Scholar] [CrossRef]
- Ren, L.; Zhou, X.; Song, Z.; Zhao, C.; Liu, Q.; Xue, J.; Li, X. Process Parameter Optimization of Extrusion-Based 3D Metal Printing Utilizing PW–LDPE–SA Binder System. Materials 2017, 10, 305. [Google Scholar] [CrossRef] [PubMed]
- Bishop, E.S.; Mostafa, S.; Pakvasa, M.; Luu, H.H.; Lee, M.J.; Wolf, J.M.; Ameer, G.A.; He, T.-C.; Reid, R.R. 3-D Bioprinting Technologies in Tissue Engineering and Regenerative Medicine: Current and Future Trends. Genes Dis. 2017, 4, 185–195. [Google Scholar] [CrossRef] [PubMed]
- Taylor, S.L.; Jakus, A.E.; Shah, R.N.; Dunand, D.C. Iron and Nickel Cellular Structures by Sintering of 3D-Printed Oxide or Metallic Particle Inks: Iron and Nickel Cellular Structures by Sintering. Adv. Eng. Mater. 2017, 19, 1600365. [Google Scholar] [CrossRef]
- Oghbaei, M.; Mirzaee, O. Microwave versus Conventional Sintering: A Review of Fundamentals, Advantages and Applications. J. Alloys Compd. 2010, 494, 175–189. [Google Scholar] [CrossRef]
- Sharma, P.; Pandey, P.M. Rapid Manufacturing of Biodegradable Pure Iron Scaffold Using Amalgamation of Three-Dimensional Printing and Pressureless Microwave Sintering. Proc. Inst. Mech. Eng. Part C J. Mech. Eng. Sci. 2019, 233, 1876–1895. [Google Scholar] [CrossRef]
- Asgari, M.; Hang, R.; Wang, C.; Yu, Z.; Li, Z.; Xiao, Y. Biodegradable Metallic Wires in Dental and Orthopedic Applications: A Review. Metals 2018, 8, 212. [Google Scholar] [CrossRef]
- Crangle, J. Ferromagnetism in Pd-Rich Palladium-Iron Alloys. Philos. Mag. 1960, 5, 335–342. [Google Scholar] [CrossRef]
- Geurtsen, W. Biocompatibility of Dental Casting Alloys. Crit. Rev. Oral Biol. Med. 2002, 13, 71–84. [Google Scholar] [CrossRef]
- Gao, C.; Yao, M.; Li, S.; Feng, P.; Peng, S.; Shuai, C. Highly Biodegradable and Bioactive Fe-Pd-Bredigite Biocomposites Prepared by Selective Laser Melting. J. Adv. Res. 2019, 20, 91–104. [Google Scholar] [CrossRef]
- Hulander, M.; Hong, J.; Andersson, M.; Gervén, F.; Ohrlander, M.; Tengvall, P.; Elwing, H. Blood Interactions with Noble Metals: Coagulation and Immune Complement Activation. ACS Appl. Mater. Interfaces 2009, 1, 1053–1062. [Google Scholar] [CrossRef]
- Okamoto, H.; Massalski, T.B. Methods for Phase Diagram Determination. In Methods for Phase Diagram Determination; Elsevier: Amsterdam, The Netherlands, 2007; pp. 51–107. ISBN 978-0-08-044629-5. [Google Scholar]
- Bosetti, M.; Massè, A.; Tobin, E.; Cannas, M. Silver Coated Materials for External Fixation Devices: In Vitro Biocompatibility and Genotoxicity. Biomaterials 2002, 23, 887–892. [Google Scholar] [CrossRef]
- Li, J.; Liu, X.; Qiao, Y.; Zhu, H.; Ding, C. Antimicrobial Activity and Cytocompatibility of Ag Plasma-Modified Hierarchical TiO2 Film on Titanium Surface. Colloids Surf. B Biointerfaces 2014, 113, 134–145. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.; Cheng, J.; Bian, D.; Zheng, Y. Fe-Au and Fe-Ag Composites as Candidates for Biodegradable Stent Materials: FE-AU AND FE-AG COMPOSITES FOR STENT MATERIALS. J. Biomed. Mater. Res. B Appl. Biomater. 2016, 104, 225–240. [Google Scholar] [CrossRef] [PubMed]
- Loffredo, S.; Paternoster, C.; Giguère, N.; Barucca, G.; Vedani, M.; Mantovani, D. The Addition of Silver Affects the Deformation Mechanism of a Twinning-Induced Plasticity Steel: Potential for Thinner Degradable Stents. Acta Biomater. 2019, 98, 103–113. [Google Scholar] [CrossRef]
- Čapek, J.; Stehlíková, K.; Michalcová, A.; Msallamová, Š.; Vojtěch, D. Microstructure, Mechanical and Corrosion Properties of Biodegradable Powder Metallurgical Fe-2 Wt% X (X = Pd, Ag and C) Alloys. Mater. Chem. Phys. 2016, 181, 501–511. [Google Scholar] [CrossRef]
- Wang, H.; Zheng, Y.; Liu, J.; Jiang, C.; Li, Y. In Vitro Corrosion Properties and Cytocompatibility of Fe-Ga Alloys as Potential Biodegradable Metallic Materials. Mater. Sci. Eng. C 2017, 71, 60–66. [Google Scholar] [CrossRef]
- Feng, Q.; Zhang, D.; Xin, C.; Liu, X.; Lin, W.; Zhang, W.; Chen, S.; Sun, K. Characterization and in Vivo Evaluation of a Bio-Corrodible Nitrided Iron Stent. J. Mater. Sci. Mater. Med. 2013, 24, 713–724. [Google Scholar] [CrossRef]
- Lin, W.; Zhang, G.; Cao, P.; Zhang, D.; Zheng, Y.; Wu, R.; Qin, L.; Wang, G.; Wen, T. Cytotoxicity and Its Test Methodology for a Bioabsorbable Nitrided Iron Stent: Cytocompatibility of Bioabsorbable Iron-Based Materials. J. Biomed. Mater. Res. B Appl. Biomater. 2015, 103, 764–776. [Google Scholar] [CrossRef]
- Lin, W.-J.; Zhang, D.-Y.; Zhang, G.; Sun, H.-T.; Qi, H.-P.; Chen, L.-P.; Liu, Z.-Q.; Gao, R.-L.; Zheng, W. Design and Characterization of a Novel Biocorrodible Iron-Based Drug-Eluting Coronary Scaffold. Mater. Des. 2016, 91, 72–79. [Google Scholar] [CrossRef]
- Hermawan, H.; Moravej, M.; Dubé, D.; Fiset, M.; Mantovani, D. Degradation Behaviour of Metallic Biomaterials for Degradable Stents. Adv. Mater. Res. 2006, 15–17, 113–118. [Google Scholar] [CrossRef]
- O’Neal, S.L.; Zheng, W. Manganese Toxicity upon Overexposure: A Decade in Review. Curr. Environ. Health Rep. 2015, 2, 315–328. [Google Scholar] [CrossRef]
- Rutchik, J.S.; Zheng, W.; Jiang, Y.; Mo, X. How Does an Occupational Neurologist Assess Welders and Steelworkers for a Manganese-Induced Movement Disorder? An International Team’s Experiences in Guanxi, China, Part I. J. Occup. Environ. Med. 2012, 54, 1432–1434. [Google Scholar] [CrossRef]
- Rutchik, J.S.; Zheng, W.; Jiang, Y.; Mo, X. How Does an Occupational Neurologist Assess Welders and Steelworkers for a Manganese-Induced Movement Disorder? An International Team’s Experiences in Guanxi, China Part II. J. Occup. Environ. Med. 2012, 54, 1562–1564. [Google Scholar] [CrossRef]
- Chen, P.; Bornhorst, J.; Aschner, M. Manganese Metabolism in Humans. Postprints Univ. Potsdam Math. Nat. Reihe 2019, 711, 25. [Google Scholar] [CrossRef]
- Carluccio, D.; Xu, C.; Venezuela, J.; Cao, Y.; Kent, D.; Bermingham, M.; Demir, A.G.; Previtali, B.; Ye, Q.; Dargusch, M. Additively Manufactured Iron-Manganese for Biodegradable Porous Load-Bearing Bone Scaffold Applications. Acta Biomater. 2020, 103, 346–360. [Google Scholar] [CrossRef]
- Hermawan, H. Biodegradable Metals; Springer: Berlin/Heidelberg, Germany, 2012; ISBN 978-3-642-31169-7. [Google Scholar]
- Field, D.M.; Baker, D.S.; Van Aken, D.C. On the Prediction of α-Martensite Temperatures in Medium Manganese Steels. Metall. Mater. Trans. A 2017, 48, 2150–2163. [Google Scholar] [CrossRef]
- Chou, D.-T.; Wells, D.; Hong, D. Novel Processing of Iron–Manganese Alloy-Based Biomaterials by Inkjet 3-D Printing. Acta Biomater. 2013, 9, 8593–8603. [Google Scholar] [CrossRef]
- Safaie, N.; Khakbiz, M.; Sheibani, S. Synthesizing of Nanostructured Fe-Mn Alloys by Mechanical Alloying Process. Procedia Mater. Sci. 2015, 11, 381–385. [Google Scholar] [CrossRef]
- Huang, S.M.; Nauman, E.A.; Stanciu, L.A. Investigation of Porosity on Mechanical Properties, Degradation and in-Vitro Cytotoxicity Limit of Fe30Mn Using Space Holder Technique. Mater. Sci. Eng. C 2019, 99, 1048–1057. [Google Scholar] [CrossRef]
- Sotoudehbagha, P.; Sheibani, S.; Khakbiz, M.; Ebrahimi-Barough, S.; Hermawan, H. Novel Antibacterial Biodegradable Fe-Mn-Ag Alloys Produced by Mechanical Alloying. Mater. Sci. Eng. C 2018, 88, 88–94. [Google Scholar] [CrossRef]
- Schinhammer, M.; Hänzi, A.C.; Löffler, J.F.; Uggowitzer, P.J. Design Strategy for Biodegradable Fe-Based Alloys for Medical Applications. Acta Biomater. 2010, 6, 1705–1713. [Google Scholar] [CrossRef] [PubMed]
- Moszner, F.; Sologubenko, A.S.; Schinhammer, M.; Lerchbacher, C.; Hänzi, A.C.; Leitner, H.; Uggowitzer, P.J.; Löffler, J.F. Precipitation Hardening of Biodegradable Fe–Mn–Pd Alloys. Acta Mater. 2011, 59, 981–991. [Google Scholar] [CrossRef]
- Mandal, S.; Kishore, V.; Bose, M.; Nandi, S.K.; Roy, M. In Vitro and in Vivo Degradability, Biocompatibility and Antimicrobial Characteristics of Cu Added Iron-Manganese Alloy. J. Mater. Sci. Technol. 2021, 84, 159–172. [Google Scholar] [CrossRef]
- Liu, R.-Y.; He, R.-G.; Chen, Y.-X.; Guo, S.-F. Effect of Ag on the Microstructure, Mechanical and Bio-Corrosion Properties of Fe–30Mn Alloy. Acta Metall. Sin. Engl. Lett. 2019, 32, 1337–1345. [Google Scholar] [CrossRef]
- Liu, R.-Y.; He, R.-G.; Xu, L.-Q.; Guo, S.-F. Design of Fe–Mn–Ag Alloys as Potential Candidates for Biodegradable Metals. Acta Metall. Sin. Engl. Lett. 2018, 31, 584–590. [Google Scholar] [CrossRef]
- Spandana, D.; Desai, H.; Chakravarty, D.; Vijay, R.; Hembram, K. Fabrication of a Biodegradable Fe-Mn-Si Alloy by Field Assisted Sintering. Adv. Powder Technol. 2020, 31, 4577–4584. [Google Scholar] [CrossRef]
- Trincă, L.C.; Burtan, L.; Mareci, D.; Fernández-Pérez, B.M.; Stoleriu, I.; Stanciu, T.; Stanciu, S.; Solcan, C.; Izquierdo, J.; Souto, R.M. Evaluation of in Vitro Corrosion Resistance and in Vivo Osseointegration Properties of a FeMnSiCa Alloy as Potential Degradable Implant Biomaterial. Mater. Sci. Eng. C 2021, 118, 111436. [Google Scholar] [CrossRef]
- Hong, D.; Chou, D.-T.; Velikokhatnyi, O.I.; Roy, A.; Lee, B.; Swink, I.; Issaev, I.; Kuhn, H.A.; Kumta, P.N. Binder-Jetting 3D Printing and Alloy Development of New Biodegradable Fe-Mn-Ca/Mg Alloys. Acta Biomater. 2016, 45, 375–386. [Google Scholar] [CrossRef]
- Schinhammer, M.; Pecnik, C.M.; Rechberger, F.; Hänzi, A.C.; Löffler, J.F.; Uggowitzer, P.J. Recrystallization Behavior, Microstructure Evolution and Mechanical Properties of Biodegradable Fe–Mn–C(–Pd) TWIP Alloys. Acta Mater. 2012, 60, 2746–2756. [Google Scholar] [CrossRef]
- Gebert, A.; Kochta, F.; Voß, A.; Oswald, S.; Fernandez-Barcia, M.; Kühn, U.; Hufenbach, J. Corrosion Studies on Fe-30Mn-1C Alloy in Chloride-Containing Solutions with View to Biomedical Application. Mater. Corros. 2018, 69, 167–177. [Google Scholar] [CrossRef]
- Harjanto, S.; Pratesa, Y.; Suharno, B.; Syarif, J. Corrosion Behavior of Fe-Mn-C Alloy as Degradable Materials Candidate Fabricated via Powder Metallurgy Process. Adv. Mater. Res. 2012, 576, 386–389. [Google Scholar] [CrossRef]
- Fiocchi, J.; Biffi, C.A.; Gambaro, S.; Paternoster, C.; Mantovani, D.; Tuissi, A. Effect of Laser Welding on the Mechanical and Degradation Behaviour of Fe-20Mn-0.6C Bioabsorbable Alloy. J. Mater. Res. Technol. 2020, 9, 13474–13482. [Google Scholar] [CrossRef]
- Venezuela, J.; Dargusch, M.S. Addressing the Slow Corrosion Rate of Biodegradable Fe-Mn: Current Approaches and Future Trends. Curr. Opin. Solid State Mater. Sci. 2020, 24, 100822. [Google Scholar] [CrossRef]
- Zhu, S.; Huang, N.; Xu, L.; Zhang, Y.; Liu, H.; Lei, Y.; Sun, H.; Yao, Y. Biocompatibility of Fe–O Films Synthesized by Plasma Immersion Ion Implantation and Deposition. Surf. Coat. Technol. 2009, 203, 1523–1529. [Google Scholar] [CrossRef]
- Zhou, J.; Yang, Y.; Frank, A.M.; Detsch, R.; Boccaccini, A.R.; Virtanen, S. Accelerated Degradation Behavior and Cytocompatibility of Pure Iron Treated with Sandblasting. ACS Appl. Mater. Interfaces 2016, 8, 26482–26492. [Google Scholar] [CrossRef]
- Huang, T.; Zheng, Y. Uniform and Accelerated Degradation of Pure Iron Patterned by Pt Disc Arrays. Sci. Rep. 2016, 6, 23627. [Google Scholar] [CrossRef]
- Chen, H.; Zhang, E.; Yang, K. Microstructure, Corrosion Properties and Bio-Compatibility of Calcium Zinc Phosphate Coating on Pure Iron for Biomedical Application. Mater. Sci. Eng. C 2014, 34, 201–206. [Google Scholar] [CrossRef]
- Wang, H.; Zheng, Y.; Li, Y.; Jiang, C. Improvement of in Vitro Corrosion and Cytocompatibility of Biodegradable Fe Surface Modified by Zn Ion Implantation. Appl. Surf. Sci. 2017, 403, 168–176. [Google Scholar] [CrossRef]
- Wang, H.; Zheng, Y.; Jiang, C.; Li, Y.; Fu, Y. In Vitro Corrosion Behavior and Cytocompatibility of Pure Fe Implanted with Ta. Surf. Coat. Technol. 2017, 320, 201–205. [Google Scholar] [CrossRef]
- Yusop, A.H.M.; Daud, N.M.; Nur, H.; Kadir, M.R.A.; Hermawan, H. Controlling the Degradation Kinetics of Porous Iron by Poly(Lactic-Co-Glycolic Acid) Infiltration for Use as Temporary Medical Implants. Sci. Rep. 2015, 5, 11194. [Google Scholar] [CrossRef]
- Gorejová, R.; Oriňaková, R.; Králová, O.Z.; Baláž, M.; Kupková, M.; Hrubovčáková, M.; Haverová, L.; Džupon, M.; Oriňak, A.; Kaľavský, F.; et al. In Vitro Corrosion Behavior of Biodegradable Iron Foams with Polymeric Coating. Materials 2020, 13, 184. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.; Ulloa, A.; Nauman, E.; Stanciu, L. Collagen Coating Effects on Fe–Mn Bioresorbable Alloys. J. Orthop. Res. 2020, 38, 523–535. [Google Scholar] [CrossRef] [PubMed]
- Drevet, R.; Zhukova, Y.; Kadirov, P.; Dubinskiy, S.; Kazakbiev, A.; Pustov, Y.; Prokoshkin, S. Tunable Corrosion Behavior of Calcium Phosphate Coated Fe-Mn-Si Alloys for Bone Implant Applications. Metall. Mater. Trans. A 2018, 49, 6553–6560. [Google Scholar] [CrossRef]
- Cimpoeşu, N.; Trincă, L.C.; Dascălu, G.; Stanciu, S.; Gurlui, S.O.; Mareci, D. Electrochemical Characterization of a New Biodegradable FeMnSi Alloy Coated with Hydroxyapatite-Zirconia by PLD Technique. J. Chem. 2016, 2016, 1–9. [Google Scholar] [CrossRef]
- Daud, M.N.; Sing, N.B.; Yusop, A.H.; Majid, A.F.A.; Hermawan, H. Degradation and in Vitro Cell–Material Interaction Studies on Hydroxyapatite-Coated Biodegradable Porous Iron for Hard Tissue Scaffolds. J. Orthop. Transl. 2014, 2, 177–184. [Google Scholar] [CrossRef]
- Majewska, P.; Oledzka, E.; Sobczak, M. Overview of the Latest Developments in the Field of Drug-Eluting Stent Technology. Biomater. Sci. 2020, 8, 544–551. [Google Scholar] [CrossRef]
- Pan, C.J.; Tang, J.J.; Weng, Y.J.; Wang, J.; Huang, N. Preparation, Characterization and Anticoagulation of Curcumin-Eluting Controlled Biodegradable Coating Stents. J. Control. Release 2006, 116, 42–49. [Google Scholar] [CrossRef]
- Forrestal, B.J.; Case, B.C.; Yerasi, C.; Garcia-Garcia, H.M.; Waksman, R. The Orsiro Ultrathin, Bioresorbable-Polymer Sirolimus-Eluting Stent: A Review of Current Evidence. Cardiovasc. Revasc. Med. 2020, 21, 540–548. [Google Scholar] [CrossRef]
- Joung, Y.K.; Kim, H.I.; Kim, S.S.; Chung, K.H.; Jang, Y.S.; Park, K.D. Estrogen Release from Metallic Stent Surface for the Prevention of Restenosis. J. Control. Release 2003, 92, 83–91. [Google Scholar] [CrossRef]
- Yang, X.; Yang, Y.; Guo, J.; Meng, Y.; Li, M.; Yang, P.; Liu, X.; Aung, L.H.H.; Yu, T.; Li, Y. Targeting the Epigenome in In-Stent Restenosis: From Mechanisms to Therapy. Mol. Ther. Nucleic Acids 2021, 23, 1136–1160. [Google Scholar] [CrossRef]
- Yusop, A.H.; Sarian, M.N.; Januddi, F.S.; Ahmed, Q.U.; Kadir, M.R.; Hartanto, D.; Hermawan, H.; Nur, H. Structure, Degradation, Drug Release and Mechanical Properties Relationships of Iron-Based Drug Eluting Scaffolds: The Effects of PLGA. Mater. Des. 2018, 160, 203–217. [Google Scholar] [CrossRef]
- Shi, J.; Miao, X.; Fu, H.; Jiang, A.; Liu, Y.; Shi, X.; Zhang, D.; Wang, Z. In Vivo Biological Safety Evaluation of an Iron-Based Bioresorbable Drug-Eluting Stent. BioMetals 2020, 33, 217–228. [Google Scholar] [CrossRef]
- Cysewska, K.; Karczewski, J.; Jasiński, P. Influence of the Electrosynthesis Conditions on the Spontaneous Release of Anti-Inflammatory Salicylate during Degradation of Polypyrrole Coated Iron for Biodegradable Cardiovascular Stent. Electrochim. Acta 2019, 320, 134612. [Google Scholar] [CrossRef]
- Sharipova, A.; Unger, R.E.; Sosnik, A.; Gutmanas, E. Dense Drug-Eluting Biodegradable Fe-Ag Nanocomposites. Mater. Des. 2021, 204, 109660. [Google Scholar] [CrossRef]
- Cooper, C.E. Nitric oxide and iron proteins. Biochim. Biophys. Acta BBA Bioenerg. 1999, 1411, 290–309. [Google Scholar] [CrossRef]
| Yield Strength (MPa) | Young’s Modulus (GPa] | Tensile Strength (MPa) | Shear Modulus (GPa) | Elastic Modulus (GPa) | Hardness (HV) | Ref | |
|---|---|---|---|---|---|---|---|
| Mg | 51 | 44–45.5 | 175–235 | 16–18 | 44–48 | 38 | [26,27] |
| Zn | 285–325 | 90–110 | 90–200 | 35–45 | 14–32 | 42 | [28] |
| Fe | 108–122 | 204–212 | 230–345 | 78–84 | 195–235 | 157 | [29,30] |
| Material | Shape | Animal | Implantation Place | Duration | Results | Ref |
|---|---|---|---|---|---|---|
| Pure iron | Stent | White rabbit | Native descending aorta | 6, 12, 18 months | Toxicity wasn’t observed, there was no neointimal proliferation and no excess inflammatory reaction | [31] |
| Pure iron | Zig-zag stent | Domestic swine | Left coronary ostium | 28 days | Stents started degradation without signs of thrombosis or immoderate inflammation | [59] |
| Pure iron | Discs | Rats | Dorsal area | 1 week, 3, 6 months | Lower degradation rate of iron samples in vivo than in vitro | [55] |
| Fe28.5Mn28.5Si | Rectangular | Wistar rats | Bone (tibiae) and subcutaneously (back) | 14, 28 days | Concentration of iron at implant surface after 28 days significantly decreased in bone and subcutaneous implants, mass of bone implant decreased after implantation whilst mass of subcutaneous implant increased | [68] |
| Fe | Pin | Rats | Femoral bone | 4, 12, 24, 52 weeks | Fe ions from degradation were transported 1mm into tissue surrounding implant, but no local toxicity | [36] |
| Fe10Mn1Pd | Pin | Rats | Femoral bone | 4, 12, 24, 52 weeks | No significant change to degradation rate of implant, no local toxicity | [36] |
| Fe21Mn0.7C1Pd | Pin | Rats | Femoral bone | 4, 12, 24, 52 weeks | Slower degradation rate than previous samples, but change was not significant, no local toxicity | [36] |
| Fe30Mn | Wire | Rats | Femoral bone | 6 months | Bone on growth was observed for bone in contact with implant, alloy did not cause adverse effects, and an iron oxide layer was observed on the implant surface | [69] |
| Fe-5%HA composite | Plate | Sheep | Tibiae | 3, 9, 14, 35, 50, and 70 days | Degradation rate was slower than degradation rate of pure iron implant | [34] |
| Fe-5%TCP composite | Plate | Sheep | Tibiae | 3, 9, 14, 35, 50, and 70 days | Higher degradation rate in contrast with pure iron implant | [34] |
| Fe-3%HA-2%TCP composite | Plate | Sheep | Tibiae | 3, 9, 14, 35, 50, and 70 days | Increase of radiopacity of implant on day 35, probably caused by accelerated bone growth and healing of tissues, degradation rate higher than pure iron implant | [34] |
| Fe0,074N | Stent | Rabbit, Minipigs | abdominal aorta, left anterior descending, right coronary artery | 12, 36 months | Nitride modified scaffold showed non-uniform corrosion, higher corrosion rate after implantation in contrast with pure iron stent, no unusual reactions, no pathological changes to tissues | [70] |
| FeXMn (X = 0.5, 2.7, 6.9) | Cylindrical plate | Mice | Back (subcutaneous) | 3, 6, 9 | There was no significant corrosion after implantation. Implants degraded slowly probably, because of phosphate layers on surface of corroding implant | [71] |
| Fe35Mn1Ag | Rods | Rats | Subcutaneous | 4, 12 weeks | The addition on silver increases corrosion rate in vivo, almost two times higher rate than Fe35Mn alloy | [72] |
| FeMn10Cu | Rods | Rabbit | Femur | 30, 90 days | Addition of copper increased corrosion rate in vivo in comparison to base FeMn alloy | [73] |
| Method | Material | Corrosion Rate (mm/Year) | Ref. |
|---|---|---|---|
| SPS | Fe | 0.016 | [52] |
| Fe2W | 0.075 | [52] | |
| Fe5W | 0.138 | [52] | |
| Fe35Mn5Si | 0.025 | [77] | |
| Fe25Mn10Cu | 0.258 | [73] | |
| Fe34Mn1Cu | 0.032 | [73] | |
| Fe | 0.105 | [78] | |
| Fe3Mn | 0.105 | [78] |
| Method | Material | Corrosion Rate (mm/Year) | Ref. |
|---|---|---|---|
| VIM | Fe3Co | 0.128 | [78] |
| Fe3Al | 0.112 | [78] | |
| Fe3W | 0.151 | [78] | |
| Fe3B | 0.175 | [78] | |
| Fe3C | 0.187 | [78] | |
| Fe3S | 0.145 | [78] | |
| FeMnC | 0.13 | [80] | |
| TWIP1Pd | 0.21 | [80] | |
| Fe | 0.11 | [80] |
| Method | Material | Corrosion Rat (mm/Year) | Ref. |
|---|---|---|---|
| VAM | Fe | 0.027 | [51] |
| Fe implanted Ag | 0.046 | [51] | |
| Fe | 0.1 | [83] | |
| Fe30Mn | 0.24 | [83] | |
| F330Mn5Si | 0.76 | [83] | |
| F3e26Mn5Si | 0.56 | [83] | |
| Fe23Mn5Si | 0.44 | [83] |
| Method | Material | Corrosion Rate (mm/Year) | Ref. |
|---|---|---|---|
| Electroforming | Fe | 0.4 | [83] |
| Fe | 0.85 | [84] |
| Method | Material | Corrosion Rate (mm/Year) | Ref. |
|---|---|---|---|
| PM | Fe20Mn | 1.3 | [84] |
| Fe25Mn | 1.1 | [84] | |
| Fe30Mn | 0.7 | [84] | |
| Fe35Mn | 0.4 | [84] | |
| Fe | 0.2 | [84] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gąsior, G.; Szczepański, J.; Radtke, A. Biodegradable Iron-Based Materials—What Was Done and What More Can Be Done? Materials 2021, 14, 3381. https://doi.org/10.3390/ma14123381
Gąsior G, Szczepański J, Radtke A. Biodegradable Iron-Based Materials—What Was Done and What More Can Be Done? Materials. 2021; 14(12):3381. https://doi.org/10.3390/ma14123381
Chicago/Turabian StyleGąsior, Gabriela, Jonasz Szczepański, and Aleksandra Radtke. 2021. "Biodegradable Iron-Based Materials—What Was Done and What More Can Be Done?" Materials 14, no. 12: 3381. https://doi.org/10.3390/ma14123381
APA StyleGąsior, G., Szczepański, J., & Radtke, A. (2021). Biodegradable Iron-Based Materials—What Was Done and What More Can Be Done? Materials, 14(12), 3381. https://doi.org/10.3390/ma14123381