Efficacy of Enamel Derivatives to Improve Keratinized Tissue as Adjunct to Coverage of Gingival Recessions: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol Development and Eligibility Criteria
2.2. Information Sources and Search
2.2.1. Electronic Search
- PUBMED:((((((EMD OR enamel matrix OR emdogain)) AND (recession OR recession coverage)) AND (coronally advanced OR coronally advanced flap OR surgical treatment OR crowned advanced)) AND “clinical study”[Publication Type])) NOT (intrabony OR intrabony defect OR intraosseous OR intraosseous defect OR infraosseous OR infra OR infrabony)
- SCOPUS:(TITLE-ABS-KEY (emd OR enamel AND matrix OR emdogain) AND TITLE-ABS-KEY (recession OR recession AND coverage) AND TITLE-ABS-KEY (coronally AND advanced OR coronally AND advanced AND flap OR surgical AND treatment OR crowned AND advanced) AND NOT TITLE-ABS-KEY (intrabony OR intrabony AND defect OR intraosseous OR intraosseous AND defect OR infraosseous OR infra OR infrabony)) AND PUBYEAR > 1999
- (P) Type of Participants: patients with a clinical diagnosis of localized or multiple gingival recessions. Studies involving only heavy smokers (≥10 cigarettes/day) were not enclosed.
- (I) Type of Interventions: any type of periodontal plastic procedure aimed to cover gingival recession with the adjunctive use of EMD.
- (C) Comparison between interventions: any type of periodontal plastic procedure for root coverage with and without enamel matrix derivatives with at least 6 months of follow-up.
- (O) Type of Outcome measures: primary outcome was the improvement of keratinized tissue.
2.2.2. Hand Search
2.3. Study Selection and Data Collection
2.4. Data Items
2.5. Risk of Bias in Individual Studies
2.6. Summary Measures and Synthesis of the Results
2.7. Risk of Bias across Studies
2.8. Assessment of the Quality of Evidence Using GRADE
3. Results
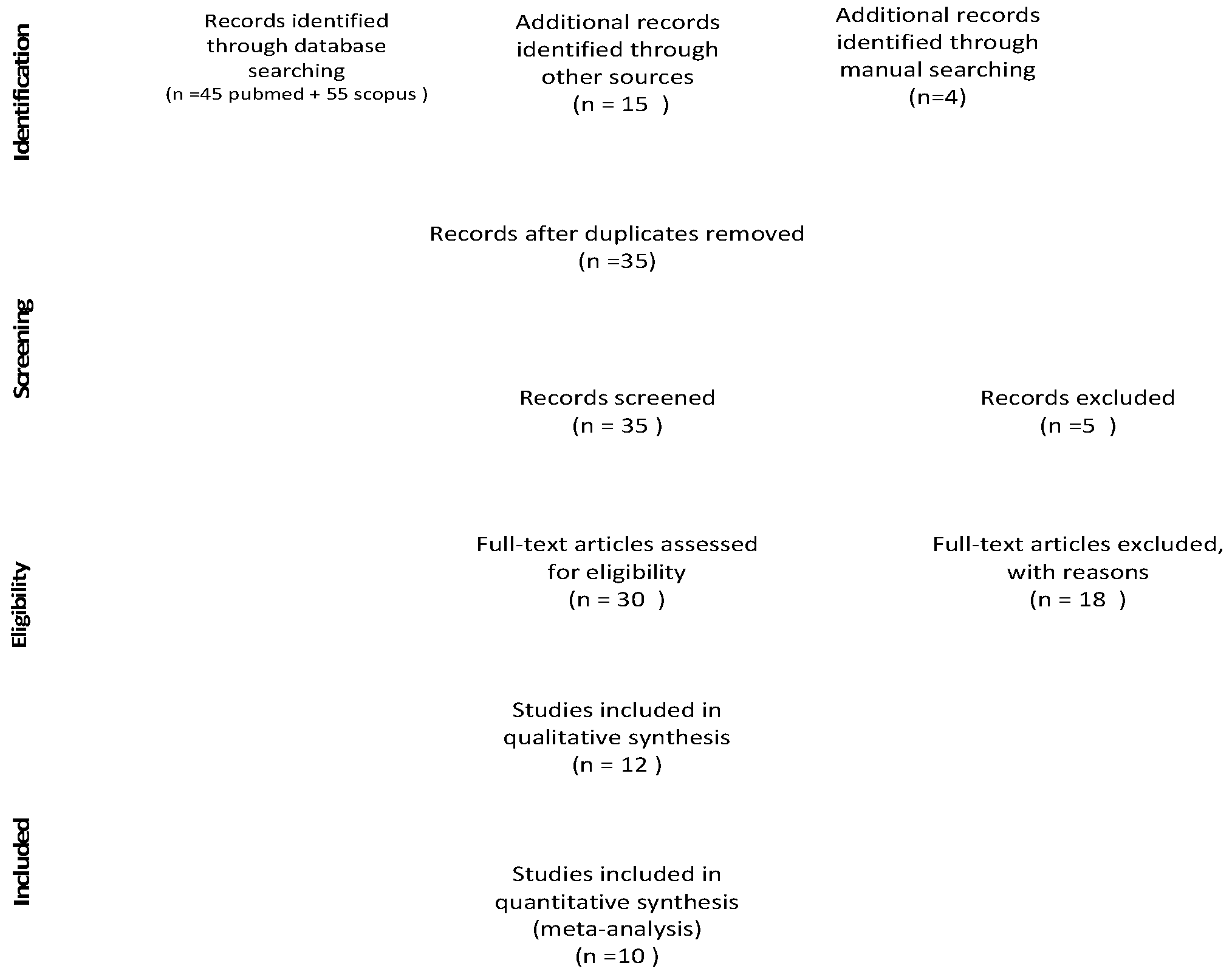
3.1. Study Selection
3.2. Study Characteristics
3.2.1. Study Design and Study Population
3.2.2. Type of Interventions
3.3. Synthesis of the Results
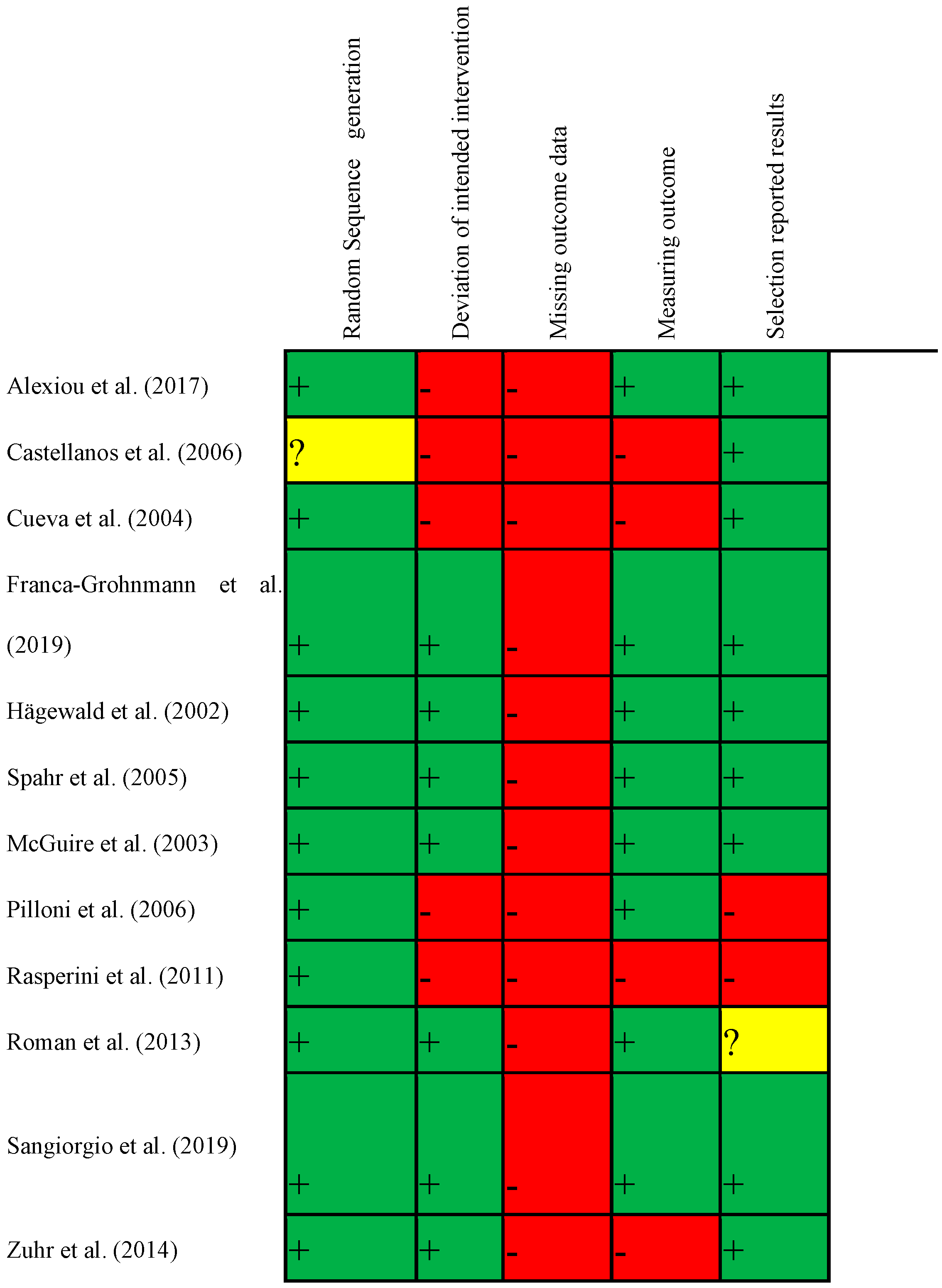
3.4. Risk of Bias in Individual Studies
3.5. Assessment of the Quality of Evidence
3.6. Additional Analysis
- (a)
- (b)
4. Discussion
Author Contributions
Funding
Conflicts of Interest
Appendix A
| Authors, Year | Main Reason for Exclusion (2: Selective Reporting; 3: Less 6 Months; 4: Not Randomized; 5: Smokers; 6: Absence of Control; 7: Less Than 10 Patients) | Comments | Timing of Exclusion (8: Abstract; 9: Full Text) |
|---|---|---|---|
| Abolfazl et al. (2009) | 4 | not specified | 9 |
| Alkan (2011) | 4 | coin toss | 9 |
| Alkan et al. (2013) | 4 | coin toss | 9 |
| Alves et al. (2012) | 5 | 8 | |
| Andrade et al. (2010) | 6 | 9 | |
| Aroca et al. (2010) | 4 | coin toss | 9 |
| Aydinyurt et al. (2019) | 4 | coin toss | 9 |
| Berlucchi et al. (2002) | 4 | coin toss | 9 |
| Berlucchi et al. (2005) | 6 | 8 | |
| Cordaro et al. (2012) | 4 | coin toss | 9 |
| Costa et al. (2016) | 5 | 8 | |
| Del Pizzo et al. (2005) | 4 | coin toss | 9 |
| Henriques et al. (2010) | 4 | 8 | |
| Jaiswal et al. (2012) | 4 | 9 | |
| Jancovic et al. (2010) | 4 | coin toss | 9 |
| McGuire et al. (2012) | n patient <10 | 9 | |
| Modica et al. (2000) | 4 | coin toss | 9 |
| Moses et al. (2006) | 4 | surgeon choice | 9 |
| Nemcovsky et al. (2004) | 4 | surgeon choice | 9 |
| Pourabbas et al. (2009) | 2 | ||
| Shin et al. (2007) | 4 | coin toss | 9 |
| Trabulsi et al. (2004) | 4 | coin toss | 9 |
| Wallace et al. (2014) | 3 | 8 |
| Authors, Year | Title | 0: Exclusion; 1: Inclusion for Abstract Evaluation | Main Reason for Exclusion (3: Not Periodontal Plastic Surgery; 4: Not with EMD; 5: Only Smokers; 6: Not RCT; 7: Not KT; 8: Not Control; 9: Not Human) |
|---|---|---|---|
| Abolfazli 2009 | A comparative study of the long-term results of root coverage with connective tissue graft or enamel matrix protein: 24-month results | 1 | |
| Adam 2019 | Root coverage using a connective tissue graft with epithelial striation in combination with enamel matrix derivatives—a long-term retrospective clinical interventional study | 0 | 6 |
| Alexiou 2017 | Comparison of enamel matrix derivative (Emdogain) and subepithelial connective tissue graft for root coverage in patients with multiple gingival recession defects: a randomized controlled clinical study | 1 | |
| Alkan 2011 | EMD or subepithelial connective tissue graft for the treatment of single gingival recessions: a pilot study | 1 | |
| Alkan 2013 | Enamel matrix derivative (emdogain) or subepithelial connective tissue graft for the treatment of adjacent multiple gingival recessions: a pilot study | 1 | |
| Alves 2012 | Acellular dermal matrix graft with or without enamel matrix derivative for root coverage in smokers: a randomized clinical study | 1 | |
| Andersen 2003 | Altered healing following mucogingival surgery in a patient with Crohn’s disease: a literature review and case report | 0 | 6 |
| Andrade 2010 | Comparison between micro- and macrosurgical techniques for the treatment of localized gingival recessions using coronally positioned flaps and enamel matrix derivative | 1 | |
| Aroca 2010 | Treatment of class III multiple gingival recessions: a randomized-clinical trial | 1 | |
| Aydinyurt 2019 | The effect of enamel matrix derivatives on root coverage: a 12-month follow-up of a randomized clinical trial | 1 | |
| Ayub 2012 | A Randomized comparative clinical study of two surgical procedures to improve root coverage with the acellular dermal matrix graft | 0 | 4 |
| Berlucchi 2002 | Enamel matrix proteins (Emdogain) in combination with coronally advanced flap or subepithelial connective tissue graft in the treatment of shallow gingival recessions | 1 | |
| Berlucchi 2005 | The influence of anatomical features on the outcome of gingival recessions treated with coronally advanced flap and enamel matrix derivative: a 1-year prospective study | 1 | |
| Bokan 2006 | Primary flap closure combined with Emdogain alone or Emdogain and Cerasorb in the treatment of intra-bony defects | 0 | 3 |
| Buti 2014 | Bayesian network meta-analysis of root coverage procedures: ranking efficacy and identification of best treatment | 0 | 6 |
| Cairo 2014 | Efficacy of periodontal plastic surgery procedures in the treatment of localized facial gingival recessions. A systematic review | 0 | 6 |
| Cairo 2016 | Root coverage procedures improve patient aesthetics. A systematic review and Bayesian network meta-analysis | 0 | 6 |
| Castellanos 2006 | Enamel matrix derivative and coronal flaps to cover marginal tissue recessions | 1 | |
| Chambrone 2009 | Root coverage procedures for the treatment of localised recession-type defects | 0 | 6 |
| Chambrone 2010 | Root-coverage procedures for the treatment of localized recession-type defects: a Cochrane systematic review | 0 | 6 |
| Chambrone 2015 | Periodontal soft tissue root coverage procedures: a systematic review from the AAP regeneration workshop | 0 | 6 |
| Chambrone 2018 | Root coverage procedures for treating localised and multiple recession-type defects | 0 | 6 |
| Chambrone 2019 | The concepts of evidence-based periodontal plastic surgery: application of the principles of evidence-based dentistry for the treatment of recession-type defects | 0 | 6 |
| Cheng 2015 | Root coverage by coronally advanced flap with connective tissue graft and/or enamel matrix derivative: a meta-analysis | 0 | 6 |
| Cordaro 2012 | Split-mouth comparison of a coronally advanced flap with or without enamel matrix derivative for coverage of multiple gingival recession defects: 6- and 24-month follow-up | 1 | |
| Cortellini 2008 | Single minimally invasive surgical technique with an enamel matrix derivative to treat multiple adjacent intra-bony defects: clinical outcomes and patient morbidity | 0 | 3 |
| Cortellini 2012 | Coronally advanced flap and combination therapy for root coverage. Clinical strategies based on scientific evidence and clinical experience | 0 | 6 |
| Costa 2016 | Root Coverage in Smokers with Acellular Dermal Matrix Graft and Enamel Matrix Derivative: a 12-Month Randomized Clinical Trial | 1 | |
| Cueva 2004 | A comparative study of coronally advanced flaps with and without the addition of enamel matrix derivative in the treatment of marginal tissue recession | 1 | |
| De Lima 2016 | Coronally advanced flap surgery with enamel matrix derivative in the treatment of gingival recession: a systematic review | 0 | 6 |
| De Sanctis 2014 | Flap approaches in plastic periodontal and implant surgery: critical elements in design and execution | 0 | 6 |
| Del Pizzo 2005 | Coronally advanced flap with or without enamel matrix derivative for root coverage: a 2-year study | 1 | |
| Di Tullio 2013 | Treatment of supra-alveolar-type defects by a simplified papilla preservation technique for access flap surgery with or without enamel matrix proteins | 0 | 3 |
| Fickl 2009 | Microsurgical access flap in conjunction with enamel matrix derivative for the treatment of intra-bony defects: a controlled clinical trial | 0 | 3 |
| França-Grohmann 2018 | Does enamel matrix derivative application improve clinical outcomes after semilunar flap surgery? A randomized clinical trial | 1 | |
| Hägewald 2002 | Comparative study of Emdogain and coronally advanced flap technique in the treatment of human gingival recessions. A prospective controlled clinical study | 1 | |
| Henriques 2010 | Application of subepithelial connective tissue graft with or without enamel matrix derivative for root coverage: a split-mouth randomized study | 1 | |
| Hofmanner 2012 | Predictability of surgical techniques used for coverage of multiple adjacent gingival recessions-A systematic review | 0 | 6 |
| Jaiswal 2013 | Evaluation of the effectiveness of enamel matrix derivative, bone grafts, and membrane in the treatment of mandibular Class II furcation defects | 1 | |
| Jankovic 2010 | The coronally advanced flap in combination with platelet-rich fibrin (PRF) and enamel matrix derivative in the treatment of gingival recession: a comparative study | 1 | |
| Lukács 2011 | The management of a single Miller-I type gingival recession at the maxillar incisor with single tunnel technique combined with enamel matrix derivative and connective tissue graft. A case report | 0 | 6 |
| Mao 2018 | The applications of periodontal gingival surgery. II: alternative materials | 0 | 6 |
| McGuire 2003 | Evaluation of human recession defects treated with coronally advanced flaps and either enamel matrix derivative or connective tissue. Part 1: comparison of clinical parameters | 1 | |
| McGuire 2012 | Evaluation of human recession defects treated with coronally advanced flaps and either enamel matrix derivative or connective tissue: comparison of clinical parameters at 10 years | 1 | |
| McGuire 2016 | A prospective, case-controlled study evaluating the use of enamel matrix derivative on human buccal recession defects: A human histologic examination | 0 | 6 |
| Meyle 2004 | A randomized clinical trial comparing enamel matrix derivative and membrane treatment of buccal class II furcation involvement in mandibular molars. Part II: secondary outcomes | 0 | 3 |
| Meyle 2011 | A multi-centre randomized controlled clinical trial on the treatment of intra-bony defects with enamel matrix derivatives/synthetic bone graft or enamel matrix derivatives alone: results after 12 months | 0 | 3 |
| Modica 2000 | Coronally advanced flap for the treatment of buccal gingival recessions with and without enamel matrix derivative. A split-mouth study | 1 | |
| Moraschini 2019 | Clinical efficacy of xenogeneic collagen matrix in the treatment of gingival recession: a systematic review and meta-analysis | 0 | 6 |
| Moses 2006 | Comparative study of two root coverage procedures: a 24-month follow-up multicenter study | 1 | |
| Nemcovsky 2004 | A multicenter comparative study of two root coverage procedures: coronally advanced flap with addition of enamel matrix proteins and subpedicle connective tissue graft | 1 | |
| Peres 2013 | Hydroxyapatite/β-tricalcium phosphate and enamel matrix derivative for treatment of proximal class II furcation defects: a randomized clinical trial | 0 | 3 |
| Pilloni 2006 | Root coverage with a coronally positioned flap used in combination with enamel matrix derivative: 18-month clinical evaluation | 1 | |
| Pini-Prato 2014 | Surgical treatment of single gingival recessions: clinical guidelines | 0 | 6 |
| Pourabbas 2009 | Coronally advanced flap in combination with acellular dermal matrix with or without enamel matrix derivatives for root coverage | 1 | |
| Rasperini 2011 | Subepithelial connective tissue graft for treatment of gingival recessions with and without enamel matrix derivative: a multicenter, randomized controlled clinical trial | 1 | |
| Rebele 2014 | Tunnel technique with connective tissue graft versus coronally advanced flap with enamel matrix derivative for root coverage: a RCT using 3D digital measuring methods. Part II. Volumetric studies on healing dynamics and gingival dimensions | 0 | 7 |
| Rocha Dos Santos 2017 | Xenogenous Collagen Matrix and/or Enamel Matrix Derivative for Treatment of Localized Gingival Recessions: A Randomized Clinical Trial. Part II: Patient-Reported Outcomes | 0 | 7 |
| Roman 2014 | Subepithelial connective tissue graft with or without enamel matrix derivative for the treatment of Miller class I and II gingival recessions: a controlled randomized clinical trial | 1 | |
| Sangiorgio 2017 | Xenogenous Collagen Matrix and/or Enamel Matrix Derivative for Treatment of Localized Gingival Recessions: A Randomized Clinical Trial. Part I: Clinical Outcomes | 1 | |
| Sculean 2007 | Four-year results of a prospective-controlled clinical study evaluating healing of intra-bony defects following treatment with an enamel matrix protein derivative alone or combined with a bioactive glass | 0 | 3 |
| Sculean 2014 | The modified coronally advanced tunnel combined with an enamel matrix derivative and subepithelial connective tissue graft for the treatment of isolated mandibular Miller Class I and II gingival recessions: A report of 16 cases | 0 | 6 |
| Sculean 2016 | Treatment of multiple adjacent maxillary Miller Class I, II, and III gingival recessions with the modified coronally advanced tunnel, enamel matrix derivative, and subepithelial connective tissue graft: a report of 12 cases | 0 | 6 |
| Shin 2007 | A comparative study of root coverage using acellular dermal matrix with and without enamel matrix derivative | 1 | |
| Shirakata 2019 | Split-mouth evaluation of connective tissue graft with or without enamel matrix derivative for the treatment of isolated gingival recession defects in dogs | 0 | 9 |
| Shirakata 2019 | Healing of localized gingival recessions treated with a coronally advanced flap alone or combined with an enamel matrix derivative and a porcine acellular dermal matrix: a preclinical study | 0 | 9 |
| Sipos 2005 | The combined use of enamel matrix proteins and a tetracycline-coated expanded polytetrafluoroethylene barrier membrane in the treatment of intra-osseous defects | 0 | 3 |
| Spahr 2005 | Coverage of Miller class I and II recession defects using enamel matrix proteins versus coronally advanced flap technique: a 2-year report | 1 | |
| Tatakis 2015 | Periodontal soft tissue root coverage procedures: a consensus report from the AAP regeneration workshop | 0 | 6 |
| Tonetti 2014 | Clinical efficacy of periodontal plastic surgery procedures: Consensus Report of Group 2 of the 10th European Workshop on Periodontology | 0 | 6 |
| Trabulsi 2004 | Effect of enamel matrix derivative on collagen guided tissue regeneration-based root coverage procedure | 1 | |
| Vignoletti 2011 | Clinical and histological healing of a new collagen matrix in combination with the coronally advanced flap for the treatment of Miller class-I recession defects: an experimental study in the minipig | 0 | 9 |
| Wallace 2014 | Treating human gingival recession defects with acellular dermis matrix and enamel matrix derivative using coronally advanced flaps | 1 | |
| Wiench 2018 | Efficacy of coronally advanced flap technique with collagen matrix mucoderm in covering multiple recessions – preliminary results | 0 | 4 |
| Ylmaz 2003 | Enamel matrix proteins in the treatment of periodontal sites with horizontal type of bone loss | 0 | 3 |
| Zuhr 2014 | Tunnel technique with connective tissue graft versus coronally advanced flap with enamel matrix derivative for root coverage: a RCT using 3D digital measuring methods. Part I. Clinical and patient-centred outcomes | 1 |
Appendix B
| Study | Date | m1 | sd1 | n1 | m0 | sd0 | n0 |
|---|---|---|---|---|---|---|---|
| Cueva 2004 | 01/07/04 | 0.6 | 1.36 | 17 | −0.05 | 1.7 | 17 |
| Pilloni 2006 | 02/07/06 | 0.13 | 0.06 | 15 | −0.06 | 0.01 | 15 |
| Sangiorgio 2017 | 03/07/17 | 0.36 | 0.9 | 21 | 0.33 | 1.4 | 21 |
| Spahr 2005 | 01/07/05 | 0.65 | 0.99 | 30 | 0.33 | 0.735 | 30 |
| Cstellanos 2006 | 02/07/06 | 0.82 | 0.2 | 22 | 0.04 | 0.01 | 22 |
| Study | Date | m1 | sd1 | n1 | m0 | sd0 | n0 |
|---|---|---|---|---|---|---|---|
| Roman 2013 | 06/06/13 | 1.36 | 1.18 | 21 | 1.56 | 1.22 | 21 |
| Sangiorgio 2017 | 06/06/17 | 0.34 | 0.86 | 17 | 0.35 | 1.04 | 17 |
| Rasperini 2011 | 06/06/11 | 2 | 1 | 30 | 2 | 1.5 | 30 |
References
- Seong, J.; Bartlett, D.; Newcombe, R.; Claydon, N.; Hellin, N.; West, N. Prevalence of gingival recession and study of associated related factors in young UK adults. J. Dent. 2018, 76, 58–67. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira, D.W.D.; Marques, D.P.; Aguiar-Cantuária, I.C.; Flecha, O.D.; Gonçalves, P.F. Effect of Surgical Defect Coverage on Cervical Dentin Hypersensitivity and Quality of Life. J. Periodontol. 2012, 84, 768–775. [Google Scholar] [CrossRef] [PubMed]
- Miller, P.D. A classification of marginal tissue recession. Int. J. Periodontics Restor. Dent. 1985, 5, 8–13. [Google Scholar]
- Sullivan, H.C.; Atkins, J.H. Free autogenous gingival grafts. I. Principles of successful grafting. Periodontics 1968, 6, 121–129. [Google Scholar] [PubMed]
- Cortellini, P.; Bissada, N.F. Mucogingival conditions in the natural dentition: Narrative review, case definitions, and diagnostic considerations. J. Periodontol. 2018, 89, S204–S213. [Google Scholar] [CrossRef] [PubMed]
- Graziani, F.; Gennai, S.; Roldán, S.; Discepoli, N.; Buti, J.; Madianos, P.; Herrera, D. Efficacy of periodontal plastic procedures in the treatment of multiple gingival recessions. J. Clin. Periodontol. 2014, 41, S63–S76. [Google Scholar] [CrossRef] [PubMed]
- Cairo, F.; Nieri, M.; Pagliaro, U. Efficacy of periodontal plastic surgery procedures in the treatment of localized facial gingival recessions. A systematic review. J. Clin. Periodontol. 2014, 41 (Suppl. 15), S44–S62. [Google Scholar] [CrossRef] [PubMed]
- Hammarström, L.; Heijl, L.; Gestrelius, S. Periodontal regeneration in a buccal dehiscence model in monkeys after application of enamel matrix proteins. J. Clin. Periodontol. 1997, 24, 669–677. [Google Scholar] [CrossRef]
- Slavkin, H.C.; Bessem, C.; Fincham, A.G.; Bringas, P.; Santos, V.; Snead, M.L.; Zeichner-David, M. Human and mouse cementum proteins immunologically related to enamel proteins. Biochim. Biophys. Acta BBA Gen. Subj. 1989, 991, 12–18. [Google Scholar] [CrossRef]
- Lyngstadaas, S.; Wohlfahrt, J.; Brookes, S.; Paine, M.; Snead, M.; Reseland, J. Enamel matrix proteins; old molecules for new applications. Orthod. Craniofacial Res. 2009, 12, 243–253. [Google Scholar] [CrossRef]
- Bartlett, J.D.; Ganss, B.; Goldberg, M.; Moradian-Oldak, J.; Paine, M.L.; Snead, M.L.; Wen, X.; White, S.N.; Zhou, Y.L. Protein–Protein Interactions of the Developing Enamel Matrix. Curr. Top. Dev. Biol. 2006, 74, 57–115. [Google Scholar] [PubMed]
- Davenport, D.R.; Mailhot, J.M.; Wataha, J.C.; Billman, M.A.; Sharawy, M.M.; Shrout, M.K. Effects of enamel matrix protein application on the viability, proliferation, and attachment of human periodontal ligament fibroblasts to diseased root surfaces in vitro. J. Clin. Periodontol. 2003, 30, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Yuan, K.; Chen, C.-L.; Lin, M.T. Enamel matrix derivative exhibits angiogenic effect in vitro and in a murine model. J. Clin. Periodontol. 2003, 30, 732–738. [Google Scholar] [CrossRef] [PubMed]
- Grayson, R.E.; Yamakoshi, Y.; Wood, E.J.; Ågren, M.S. The effect of the amelogenin fraction of enamel matrix proteins on fibroblast-mediated collagen matrix reorganization. Biomaterials 2006, 27, 2926–2933. [Google Scholar] [CrossRef] [PubMed]
- Rasperini, G.; Roccuzzo, M.; Francetti, L.; Acunzo, R.; Consonni, D.; Silvestri, M. Subepithelial connective tissue graft for treatment of gingival recessions with and without enamel matrix derivative: A multicenter, randomized controlled clinical trial. Int. J. Periodontics Restor. Dent. 2011, 31, 133–139. [Google Scholar]
- Wennstrom, J.L.; Zucchelli, G. Clinical periodontoiogy Increased gingival dimensions. A significant factor for successful outcome of root coverage procedures? A 2-year prospective clinical study. J. Clin. Perhdonml. 1996, 23, 770–777. [Google Scholar] [CrossRef]
- Prato, G.P.P.; Magnani, C.; Chambrone, L. Long-term evaluation (20 years) of the outcomes of coronally advanced flap in the treatment of single recession-type defects. J. Periodontol. 2018, 89, 265–274. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009, 62, e1–e34. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Higgins, J.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]; Cochrane Group: London, UK, 2011. [Google Scholar]
- Higgins, J.; Savović, J.; Page, M.; Sterne, J. A Revised Cochrane Risk of Bias Tool for Randomized Trials; Chandler, J., McKenzie, J., Boutron, I., Welch, V., Eds.; Cochrane Group: London, UK, 2016. [Google Scholar]
- Moher, D.; Hopewell, S.; Schulz, K.F.; Montori, V.; Gøtzsche, P.C.; Devereaux, P.; Elbourne, D.; Egger, M.; Altman, D.G. CONSORT 2010 explanation and elaboration: Updated guidelines for reporting parallel group randomised trials. Int. J. Surg. 2012, 10, 28–55. [Google Scholar] [CrossRef]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control. Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [PubMed]
- Hedges, L.V.; Olkin, I. Statistical Methodblogy in Meta-Analysis; Academic Press: Cambridge, MA, USA, 1985; ISBN 978-0123363800. [Google Scholar]
- Egger, M.; Smith, G.D. Meta-analysis bias in location and selection of studies. BMJ 1998, 316, 61–66. [Google Scholar] [CrossRef]
- Guyatt, G.H.; Oxman, A.D.; Schünemann, H.J.; Tugwell, P.; Knottnerus, A. GRADE guidelines: A new series of articles in the Journal of Clinical Epidemiology. J. Clin. Epidemiol. 2011, 64, 380–382. [Google Scholar] [CrossRef] [PubMed]
- Alexiou, A.; Vouros, I.; Konstantinidis, A.; Menexes, G. Comparison of enamel matrix derivative (Emdogain) and subepithelial connective tissue graft for root coverage in patients with multiple gingival recession defects: A randomized controlled clinical study. Quintessence Int. 2017, 48, 381–389. [Google Scholar]
- Rocha Dos Santos, M.; Sangiorgio, J.P.M.; Neves, F.L.D.S.; França-Grohmann, I.L.; Nociti FHJr Silverio Ruiz, K.G.; Santamaria, M.P.; Sallum, E.A. Xenogenous Collagen Matrix and/or Enamel Matrix Derivative for Treatment of Localized Gingival Recessions: A Randomized Clinical Trial. Part I: Clinical Outcomes. J. Periodontol. 2017, 88, 1309–1318. [Google Scholar] [CrossRef]
- Cueva, M.A.; Boltchi, F.E.; Hallmon, W.W.; Nunn, M.E.; Rivera-Hidalgo, F.; Rees, T. A Comparative Study of Coronally Advanced Flaps With and Without the Addition of Enamel Matrix Derivative in the Treatment of Marginal Tissue Recession. J. Periodontol. 2005, 75, 949–956. [Google Scholar] [CrossRef]
- Roman, A.; Soancă, A.; Kasaj, A.; Stratul, S.-I.; Stratul, S. Subepithelial connective tissue graft with or without enamel matrix derivative for the treatment of Miller class I and II gingival recessions: A controlled randomized clinical trial. J. Periodontal Res. 2013, 48, 563–572. [Google Scholar] [CrossRef]
- Zuhr, O.; Rebele, S.F.; Schneider, D.; Jung, R.E.; Hürzeler, M.B. Tunnel technique with connective tissue graft versus coronally advanced flap with enamel matrix derivative for root coverage: A RCT using 3D digital measuring methods. Part I. Clinical and patient-centred outcomes. J. Clin. Periodontol. 2014, 41, 582–592. [Google Scholar] [CrossRef]
- Castellanos, A.; de la Rosa, M.; de la Garza, M.; Caffesse, R.G. Enamel Matrix Derivative and Coronal Flaps to Cover Marginal Tissue Recessions. J. Periodontol. 2006, 77, 7–14. [Google Scholar] [CrossRef] [PubMed]
- França-Grohmann, I.L.; Sangiorgio, J.P.M.; Bueno, M.R.; Casarin, R.C.V.; Silvério, K.G.; Nociti, F.H., Jr.; Casati, M.Z.; Sallum, E.A. Does enamel matrix derivative application improve clinical outcomes after semilunar flap surgery? A randomized clinical trial. Clin. Oral Investig. 2019, 23, 879–887. [Google Scholar] [CrossRef] [PubMed]
- McGuire, M.K.; Nunn, M. Evaluation of Human Recession Defects Treated with Coronally Advanced Flaps and Either Enamel Matrix Derivative or Connective Tissue. Part 1: Comparison of Clinical Parameters. J. Periodontol. 2005, 74, 1110–1125. [Google Scholar] [CrossRef] [PubMed]
- Pilloni, A.; Paolantonio, M.; Camargo, P.M. Root Coverage with a Coronally Positioned Flap Used in Combination with Enamel Matrix Derivative: 18-Month Clinical Evaluation. J. Periodontol. 2006, 77, 2031–2039. [Google Scholar] [CrossRef] [PubMed]
- Spahr, A.; Haegewald, S.; Tsoulfidou, F.; Rompola, E.; Heijl, L.; Bernimoulin, J.-P.; Ring, C.; Sander, S.; Haller, B. Coverage of Miller Class I and II Recession Defects Using Enamel Matrix Proteins Versus Coronally Advanced Flap Technique: A 2-Year Report. J. Periodontol. 2005, 76, 1871–1880. [Google Scholar] [CrossRef] [PubMed]
- Lang, N.P.; Löe, H. The Relationship between the Width of Keratinized Gingiva and Gingival Health. J. Periodontol. 2010, 43, 623–627. [Google Scholar] [CrossRef] [PubMed]
- Wennstrom, J.; Lindhe, J.; Nyman, S. Role of keratinized gingiva for gingival health. Clinical and histologic study of normal and regenerated gingival tissue in dogs. J. Clin. Periodontol. 1981, 8, 311–328. [Google Scholar] [CrossRef] [PubMed]
- Jansen, J.P.; Naci, H. Is network meta-analysis as valid as standard pairwise meta-analysis? It all depends on the distribution of effect modifiers. BMC Med. 2013, 11, 159. [Google Scholar] [CrossRef]
- Agudio, G.; Cortellini, P.; Buti, J.; Prato, G.P.; Agudio, G.; Agudio, G.; Buti, J.; Pini-Prato, G.; Cortellini, P. Periodontal Conditions of Sites Treated With Gingival Augmentation Surgery Compared With Untreated Contralateral Homologous Sites: An 18- to 35-Year Long-Term Study. J. Periodontol. 2016, 87, 1371–1378. [Google Scholar] [CrossRef]
- De Sanctis, M.; Zucchelli, G. Coronally advanced flap: A modified surgical approach for isolated recession-type defects: Three-year results. J. Clin. Periodontol. 2007, 34, 262–268. [Google Scholar] [CrossRef]
- Matter, J.; Cimasoni, G. Creeping Attachment After Free Gingival Grafts. J. Periodontol. 2013, 47, 574–579. [Google Scholar] [CrossRef] [PubMed]
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017, 358, j4008. [Google Scholar] [CrossRef] [PubMed]
- Sideri, S.; Papageorgiou, S.N.; Eliades, T. Registration in the international prospective register of systematic reviews (PROSPERO) of systematic review protocols was associated with increased review quality. J. Clin. Epidemiol. 2018, 100, 103–110. [Google Scholar] [CrossRef]
- Altman, D.G.; Moher, D.; Schulz, K.F. Improving the reporting of randomised trials: The CONSORT Statement andbeyond. Stat. Med. 2012, 31, 2985–2997. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Pham, B.; Lawson, M.L.; Klassen, T.P. The inclusion of reports of randomised trials published in languages other than English in systematic reviews. Health Technol. Assess. 2003, 7, 1–90. [Google Scholar] [CrossRef] [PubMed]
- Morrison, A.; Polisena, J.; Husereau, D.; Moulton, K.; Clark, M.; Fiander, M.; Mierzwinski-Urban, M.; Clifford, T.; Hutton, B.; Rabb, D. The effect of english-language restriction on systematic review-based meta-analyses: a systematic review of empirical studies. Int. J. Technol. Assess. Health Care 2012, 28, 138–144. [Google Scholar] [CrossRef] [PubMed]
| First Author, (Year) | Study Design | Follow Up | Sample Size (Control/Test), Mean Age (Range) | Tooth Type | Primary Outcome Measure Type of Measurement; Anatomical Landmarks; Timing in Months | —Recession Classification —Type | Location Site (Setting and Funding) |
|---|---|---|---|---|---|---|---|
| Alexiou et al. (2017) | split-mouth | 6 months | Patient 12 Age 40.01 (23–60) | Incisor, Premolar, Molar | (a) Periodontal Probe (PCP-UNC 15) rounded off at 1 mm (b) Distance between gingival margin and mucogingival junction (c) 0, 6 | Miller 1985 I, II | GR (University) |
| Castellanos et al. (2006) | parallel group | 12 months | Patient 22 Age 42.5 (28–71) | NR | (a) Periodontal Probe (PCP-UNC 15) rounded off at 1 mm (b) From the gingival margin to the mucogingival junction at same point recession depth (c) 0, 6, 12 | Miller 1985 I, II | Mexico (University) |
| Cueva et al. (2004) | split-mouth | 6 months | Patient 17 Age 39 (23–55) | Incisor, Cuspid, Premolar | (a) North Caroline Periodontal probe Rounded off at 0.5 mm (b) Keratinized gingiva was highlighted with a combination of Lugol’s solution and Iodine solution. (c) 0, 3, 6 | Miller 1985 I, II, III | US (University) |
| Franca-Grohmann et al. (2018) | parallel group | 12 months | Patient 30 (15/15) Age 29.52 (23–45) | Cuspid, Premolar | (a) Calliper (0.001 resolution and acrylic stent) (b) Keratinized gingiva was highlighted with Iodine solution (c) 0, 6, 12 | Miller 1985 I | Brazil (University) |
| Hagewald et al. (2002) | split-mouth | 12 months | Patient 36 Age 36 (22–62) | Incisor, Cuspid, Premolar | (a) CP 15 UNC (b) Not specified (c) 0, 6, 12 | Miller 1985 I, II | DE (University) |
| McGuire et al. (2003) | split-mouth | 12 months | Patient 17 Age 44.8 (23–62) | Incisor, Cuspid, Premolar | (a) Automated probe with constant force (b) Identification of the mucogingival junction (c) 0, 3, 6, 9, 12 | Miller 1985 II | US (Private Practice) |
| Pilloni et al. (2006) | parallel group | 18 months | Patient 30 (15/15) Age Mean Age Not Reported (19–67) | Incisor, Cuspid, Premolar | (a) UNC Periodontal Probe rounded off at 0.5 mm (b) Distance between gingival margin and mucogingival junction (c) 0, 3, 6, 12, 18 | Miller 1985 I, II | IT (University) |
| Rasperini et al. (2011) | parallel group | 12 months | Patient 56 (30/26) Age 35.48 Mean Age Not Reported | Incisor, Cuspid, Premolar | (a) CP, UNC 15 rounded to 1 mm (b) Mid-buccal point from the mucogingival junction to the gingival margin (c) 0, 12 | Miller 1985 I, II | IT (NR) |
| Roman et al. (2013) | parallel group | 12 months | Patient 42 (21/21) Age 31 (21–48) | Incisor, Cuspid, Premolar, Molar | (a) CP, UNC 15 rounded to 1 mm (b) Mid-buccal point from the mucogingival junction to the gingival margin (running method) (c) 0, 1, 3, 6, 12 | Cairo 2011 I | Romania (University) |
| Sangiorgio et al. (2017) | parallel group | 6 months | Patient 68 (17/17/17/17) * Age 37.53 Mean Age Not Reported | Cuspid, Premolar | (a) Periodontal probe (b) From the gingival margin to the mucogingival junction evidenced with Iodine solution stain (c) 0, 3, 6 | Miller 1985 I, II | Brazil (University) |
| Spahr et al. (2005) | split-mouth | 24 months | Patient 30 Age 36.5 (23–62) | Incisor, Cuspid, Premolar | (a) CP 15 UNC graded probe (b) Not specified (c) 0, 6, 12, 24 | Miller 1985 I, II | DE (University) |
| Zuhr et al. (2014) | split/parallel design | 12 months | Patient 24 (6 split + 9/9) Age 37.9 (21–55) | Incisor, Cuspid, Premolar | (a) CP 15 UNC graded probe (b) Most apical point of the gingival margin to the mucogingival junction (mid buccal point) (c) 0, 6, 12 | Miller 1985 I, II | DE/CH (Private Practice) |
| First Author, (Year) | Preoperative Preparation | Type of Control | Type of Test | Post-Surgical Treatment | Authors Conclusion |
|---|---|---|---|---|---|
| Alexiou et al. (2017) | OHI, PMPR | Coronally advanced flap without vertical releasing incisions (MCAF) + Connective tissue graft (CTG) | MCAF + Enamel Matrix Derivatives (EMD) | No brushing and chx 0.12% for 3 weeks, NSAIDs, PMPR and OHI at recall visits | The use of EMD in conjunction with a MCAF resulted in similar results as compared to the CTG plus CAF |
| Castellanos et al. (2006) | OHI, PMPR | Crowned advanced flap (CAF) | CAF + EMD | No brushing and chx 0.12% for 3 weeks, NSAIDs, PMPR and OHI at recall visits | The addition of EMD significantly improves the amount of root coverage |
| Cueva et al. (2004) | OHI, SRP | CAF | CAF + EMD | No brushing and chx 0.2% for 4 weeks, PMPR at recall visits | The application of EMD to denuded root surfaces receiving CAF significantly increased the percentage of root coverage compared to CAF without EMD. In addition, EMD application was accompanied by a significant increase in KT 6 months after surgery |
| Franca-Grohmann et al. (2018) | OHI, PMPR | Semilunar flap | Semilunar flap + EMD | Periodontal dressing, No brushing and chx 0.12% for 2 weeks, NSAIDs, PMPR at recall visits | The combination Semilunar flap + EMD provides better aesthetics when compared to the semilunar flap and is effective, but not superior, to semilunar flap for root coverage, after 12 months. |
| Hagewald et al. (2002) | OHI, PMPR | CAF | CAF + EMD | No brushing and chx 0.12% for 3 weeks, NSAIDs, PMPR and OHI at recall visits | There is no clear benefit to combine EMD with this surgical technique |
| McGuire et al. (2003) | OHI | CAF + CTG | CAF + EMD | No brushing and chx 0.12% for 3 weeks, PMPR and OHI at recall visits | The addition of EMD to the coronally advanced flap resulted in root coverage similar to CTG |
| Pilloni et al. (2006) | OHI, SRP | CAF | CAF + EMD | No brushing and chx 0.12% for 4 weeks, NSAIDs, PMPR at recalls | Topical application of EMD is beneficial in augmenting the effects of the CAF in terms of amount of root coverage, gain in CAL, and in increasing the apicocoronal dimension of the keratinized tissue |
| Rasperini et al. (2011) | OHI, PMPR | CAF + CTG | CAF + CTG + EMD | No brushing and chx 0.12% for 3 weeks, NSAIDs, PMPR and OHI at recall visits | The cost-benefit ratio associated with adding EMD to the CTG procedure should be evaluated carefully |
| Roman et al. (2013) | OHI, Full-mouth supragingival scaling, polishing | CAF + CTG | CAF + CTG + EMD | No brushing and chx 0.2% for 3 weeks, NSAIDs, PMPR and OHI at recall visits | The present study failed to demonstrate any additional clinical benefits when EMD was added to CTG plus CAF |
| Sangiorgio et al. (2017) | OHI, Full-mouth supragingival scaling, prophilaxis | CAF + CTG, CAF | CAF + CTG +EMD, CAF + EMD | No brushing and chx 0.12%, NSAIDs for 3 days, PMPR and OHI at recall visits | EMD provides highest levels of complete root coverage; however, the addition of CTG increases gingival thickness. The combination approach does not seem justified |
| Spahr et al. (2005) | OHI, PMPR | CAF | CAF + EMD | No brushing and chx 0.12% for 3 weeks, NSAIDs, PMPR and OHI at recall visits | Enamel matrix derivative seems to provide better long-term results |
| Zuhr et al. (2014) | OHI, prophylaxis, air-polish | Tunnel technique (TUN) + CTG | CAF + EMD | No brushing and chx for 2 weeks, NSAIDs when needed, PMPR and OHI at recall visits | TUN resulted in significantly better clinical outcomes compared with CAF |
| Outcomes | Treatment Effect | No. of Participants (Studies) | Quality of the Evidence (GRADE) a |
|---|---|---|---|
| Mean Difference (MD) | |||
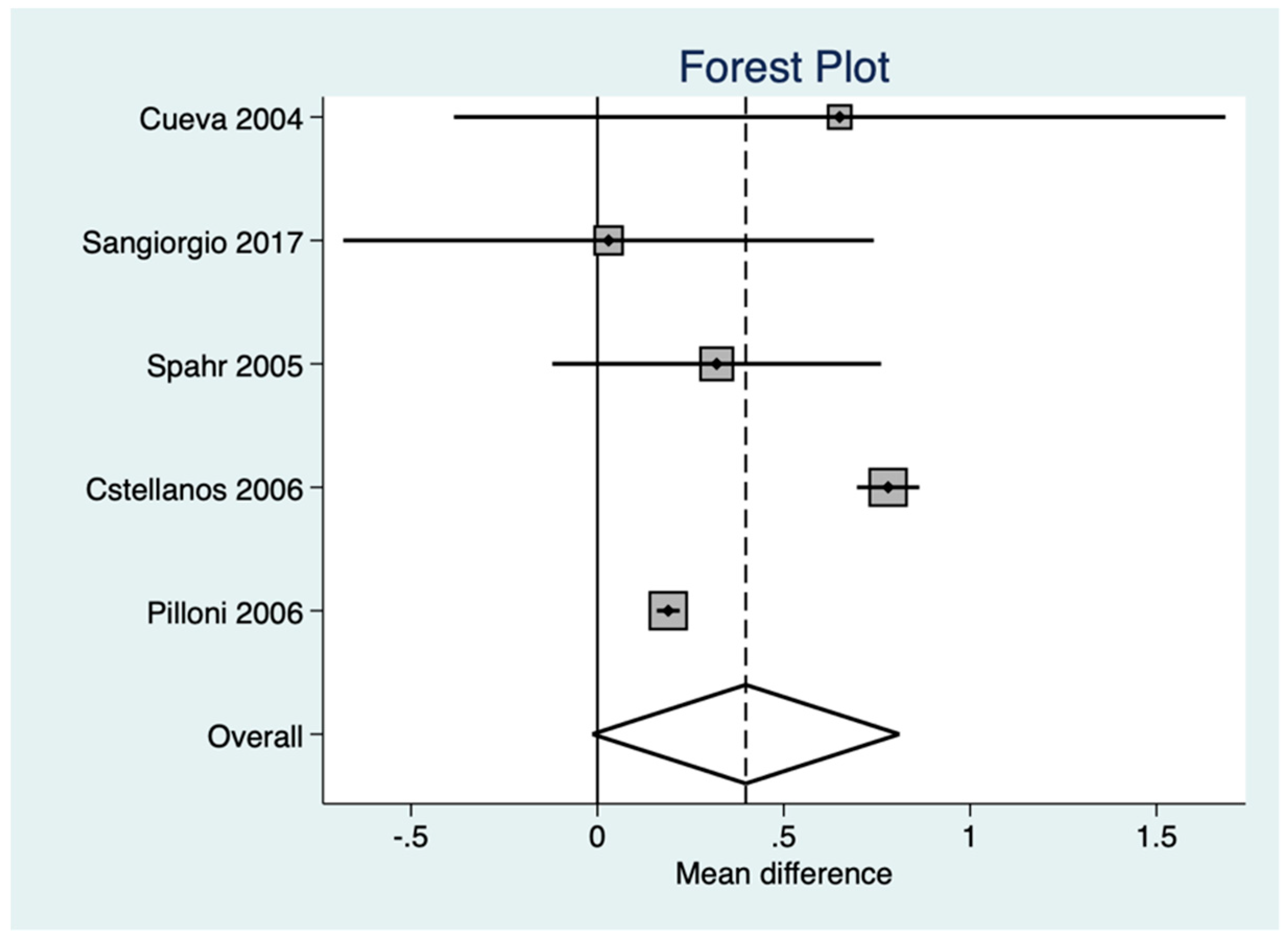
| Gain in Keratinized Tissue Width (KTg)—CAF vs CAF + EMD | MD 0.46 95% C.I. [0.14; 0.77] | 133 (5) | Low 1,2 |
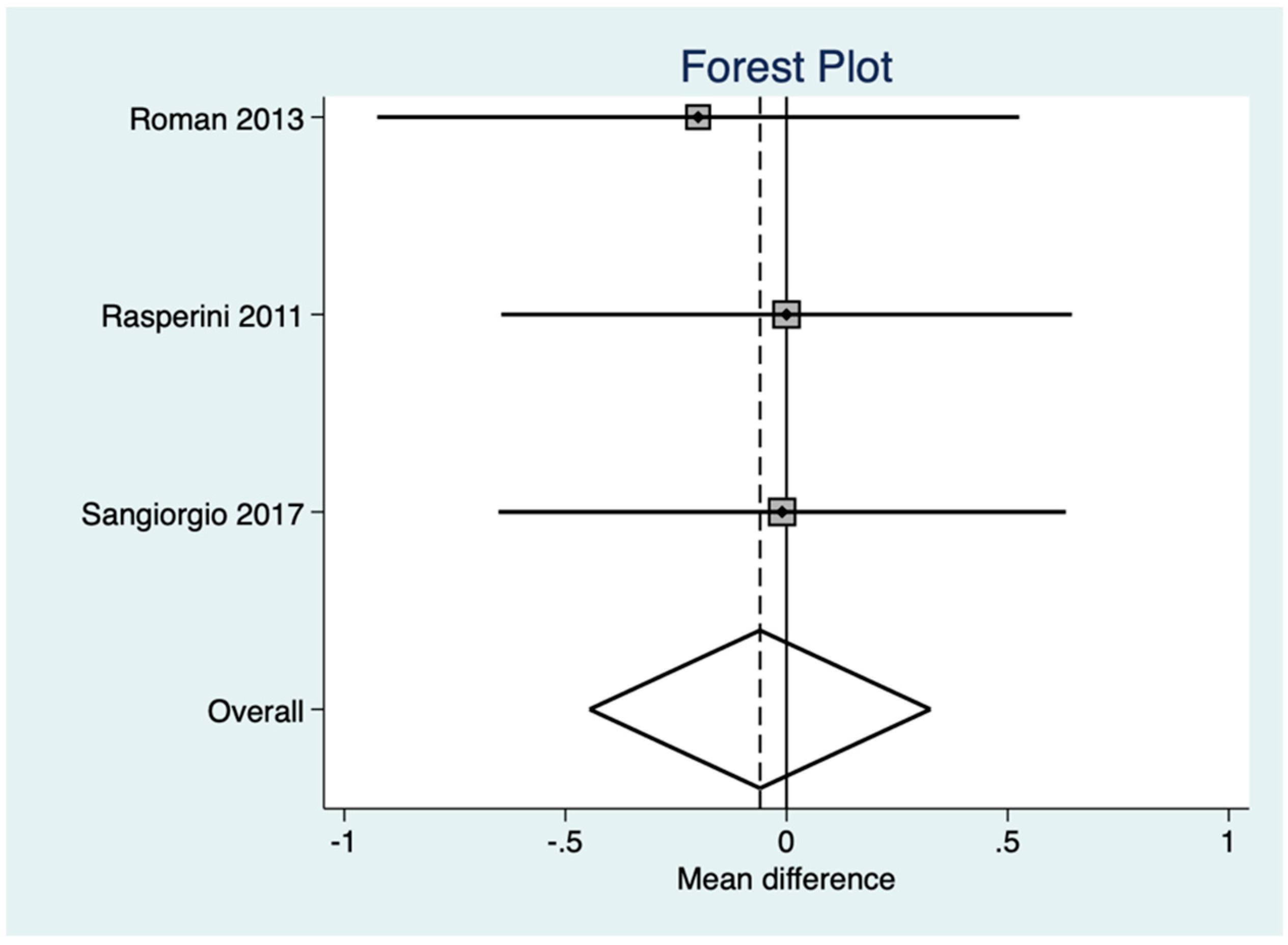
| KTg—CAF + CTG vs. CAF + CTG + EMD | MD −0.06 95% C.I. [−0.44; 0.32] | 132 (3) | Moderate 1 |
| KTg—CAF + CTG vs. CAF + EMD | MD −0.63 95% C.I. [−0.72; −0.55] | 29 (2) | Very low 1,3 |
| Study | Mean Difference | Confidence Interval 95% | Relative IoV Weights | |
|---|---|---|---|---|
| Lower | Upper | |||
| Cueva et al. (2004) | 0.65 | −0.38 | 1.68 | 10.0% |
| Pilloni et al. (2004) | 0.19 | −0.16 | 0.22 | 27.2% |
| Sangiorgio et al. (2017) | 0.03 | −0.70 | 0.76 | 10.7% |
| Spahr et al. 2005 | 0.32 | −0.12 | 0.76 | 20.8% |
| Castellanos et al. 2006 | 0.78 | 0.70 | 0.86 | 27.0% |
| Total | 100% | |||
| Total weights | 22.67 | |||
| Random Effect Model | Estimation | Confidence Interval 95% | Significance | |
|---|---|---|---|---|
| Lower | Upper | |||
| IoV Weighted MD | 0.398 | −0.014 | 0.810 | 0.058 |
| SE | 0.210 | |||
| Heterogeneity Measures: | ||||
| Relative Excess H | 0.670 | 0.305 | 1.47 | |
| SE(lnH) | 0.400 | |||
| Percentage of Var. I2 | 0 | |||
| Homogeneity Chi-Square | 1.79 | 0.773 | ||
| Study | Mean Difference | Confidence Interval 95% | Relative IoV Weights | |
|---|---|---|---|---|
| Lower | Upper | |||
| Roman et al. 2013 | −0.2 | −0.93 | 0.53 | 28.2% |
| Sangiorgio et al. 2017 | −0.01 | −0.65 | 0.63 | 36.1% |
| Rasperini et al. 2011 | 0.0 | −0.65 | 0.65 | 35.7% |
| Total | 100% | |||
| Total weights | 25.85 | |||
| Random Effect Model | Estimation | Confidence Interval 95% | Significance | |
|---|---|---|---|---|
| Lower | Upper | |||
| IoV Weighted MD | −0.60 | −0.445 | 0.325 | 0.760 |
| SE | 0.20 | |||
| Heterogeneity Measures: | ||||
| Relative Excess H | 0.316 | 0.101 | 0.979 | |
| SE(lnH) | 0.577 | |||
| Percentage of Variability I2 | 0 | |||
| Homogeneity Chi-Square | 0.199 | 0.905 | ||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Discepoli, N.; Mirra, R.; Ferrari, M. Efficacy of Enamel Derivatives to Improve Keratinized Tissue as Adjunct to Coverage of Gingival Recessions: A Systematic Review and Meta-Analysis. Materials 2019, 12, 2790. https://doi.org/10.3390/ma12172790
Discepoli N, Mirra R, Ferrari M. Efficacy of Enamel Derivatives to Improve Keratinized Tissue as Adjunct to Coverage of Gingival Recessions: A Systematic Review and Meta-Analysis. Materials. 2019; 12(17):2790. https://doi.org/10.3390/ma12172790
Chicago/Turabian StyleDiscepoli, Nicola, Raffaele Mirra, and Marco Ferrari. 2019. "Efficacy of Enamel Derivatives to Improve Keratinized Tissue as Adjunct to Coverage of Gingival Recessions: A Systematic Review and Meta-Analysis" Materials 12, no. 17: 2790. https://doi.org/10.3390/ma12172790
APA StyleDiscepoli, N., Mirra, R., & Ferrari, M. (2019). Efficacy of Enamel Derivatives to Improve Keratinized Tissue as Adjunct to Coverage of Gingival Recessions: A Systematic Review and Meta-Analysis. Materials, 12(17), 2790. https://doi.org/10.3390/ma12172790






