Energy Usage Assessment and Energy Savings Estimation in a Radiology Department in Italy
Abstract
1. Introduction
2. Materials and Methods
2.1. Overview of Methods
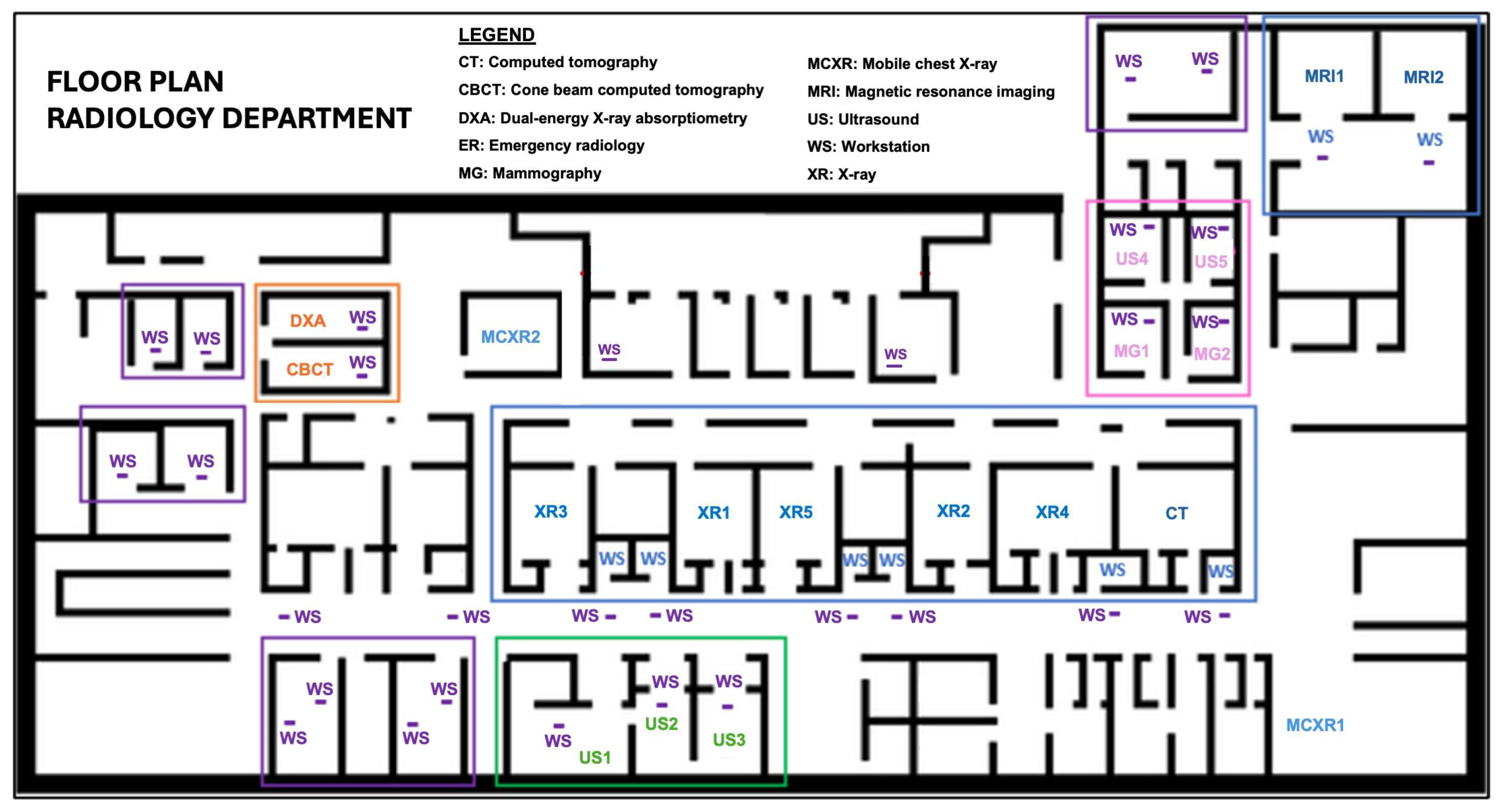
2.2. Study Setting
2.3. Study Design
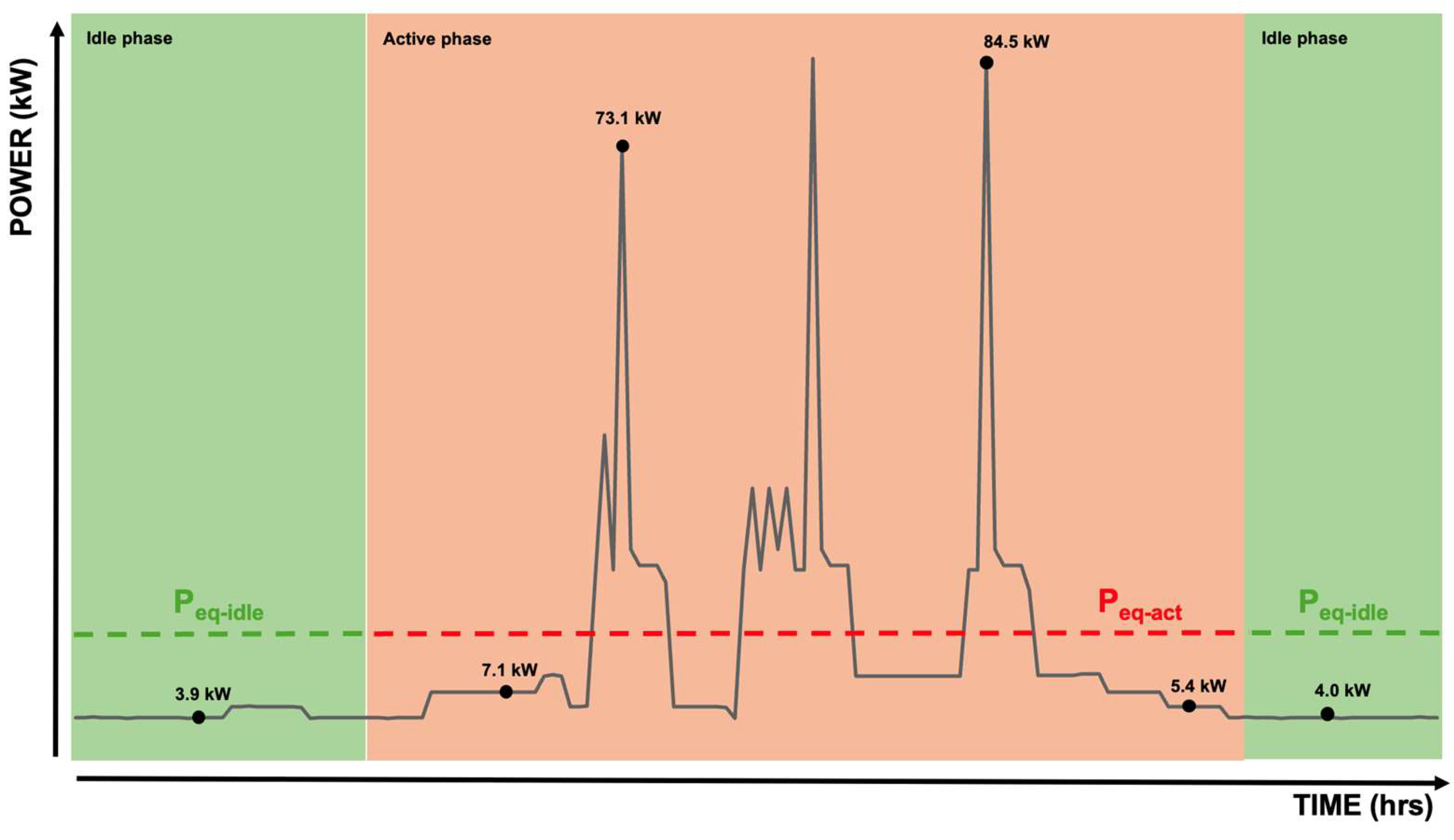
2.4. Estimation of Energy Usage
- Active period: the productive time, which includes patient or scanner positioning and image acquisition;
- Idle period: the non-productive waiting time interval between “active” time periods, when devices are “on” but not working.
- Active period: the production time during which workstations are actively used by department staff;
- Idle period: the non-productive waiting time interval between “active” time periods, when workstations are “on” but not working;
- Stand-by period: the non-productive time that the equipment was switched on but there was no related imaging activity. During the stand-by period, workstations are able to consume less power while being able to resume its normal functions quickly.
3. Results
3.1. Energy Usage
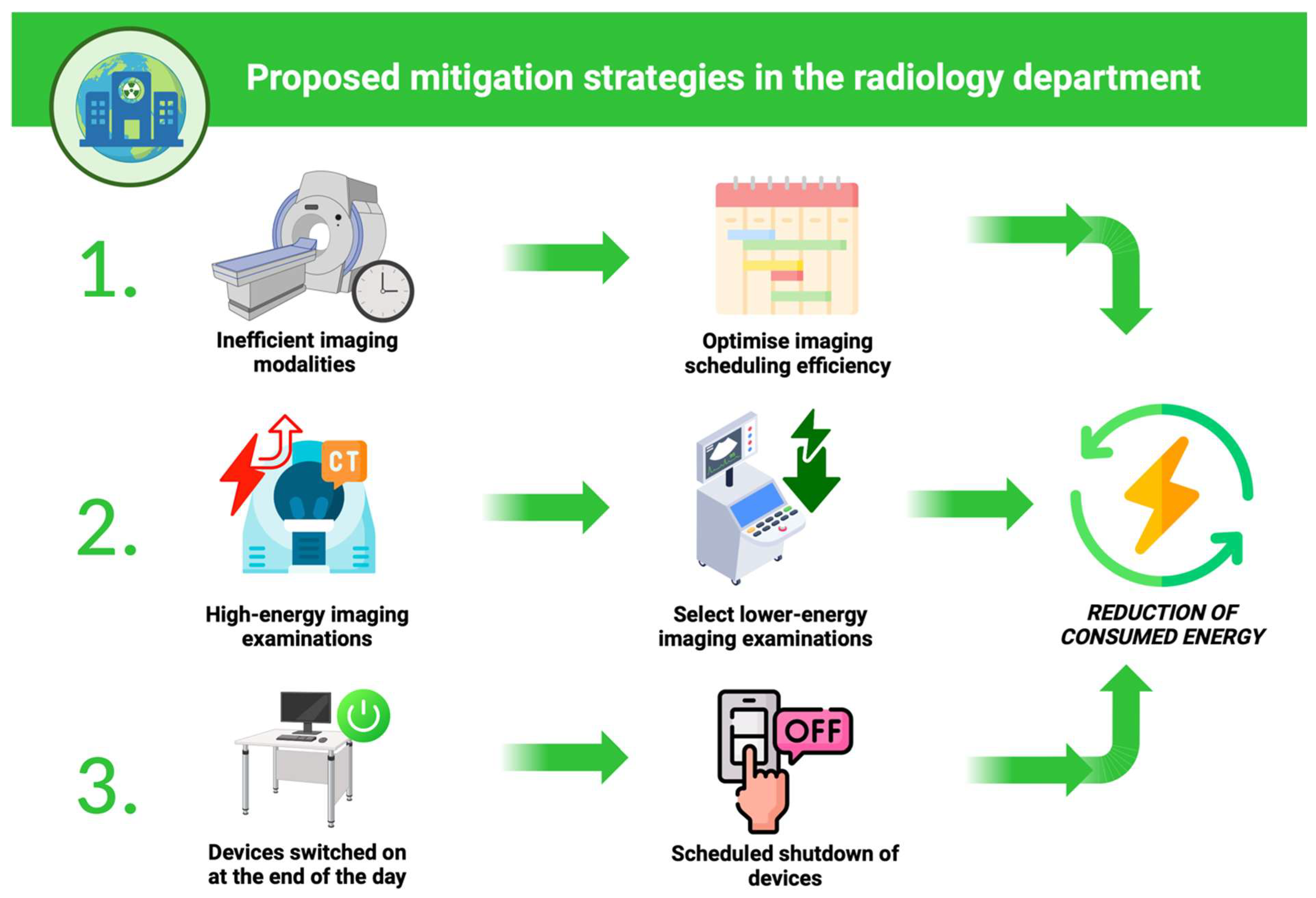
3.2. Mitigation Strategies
3.2.1. Mitigation Strategy 1: Optimize Imaging Scheduling Efficiency
- Reduction in XR5 activity, which is exclusively ambulatory and do not include unscheduled urgent examinations, from 5 to 3 working days by redistributing exams on scheduled days.
- Reduction in CBCT activity times based on the number of patients booked and the early closure of diagnostics at the end of scheduled activity.
- Redistribution of MG1 mode activity to MG2, keeping both modes active.
- Exclusive use of MCXR2, keeping MCXR1 switched off, concentrating activity on a single device.
3.2.2. Mitigation Strategy 2: Select Lower-Energy Imaging Examinations
3.2.3. Mitigation Strategy 3: Scheduled Shutdown of Devices
4. Discussion
5. Conclusions
- Optimize imaging scheduling efficiency −16.6% of energy usage;
- Select lower-energy imaging examinations −80.4% of energy usage;
- Scheduled shutdown of devices −40.9% of energy usage.
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
| CT | Computed tomography |
| CBCT | Cone beam computed tomography |
| DXA | Dual-energy X-ray absorptiometry |
| E | Energy |
| GHG | Greenhouse gas |
| MG | Mammography |
| MCXR | Mobile chest X-ray |
| MRI | Magnetic resonance imaging |
| Peq | Equivalent mean power demand |
| PACS | Picture archiving and communication system |
| RIS | Radiology information system |
| RWS | Reporting workstation |
| US | Ultrasound |
| WS | Workstation |
| XR | X-ray |
Appendix A
| XR1 | Samsung AccE GC85A (Samsung Healthcare, Seoul, Republic of Korea) |
| XR2 | Samsung AccE GC85A (Samsung Healthcare, Seoul, Republic of Korea) |
| XR3 | Carestream DRX-Compass (Carestream Health, Rochester, NY, USA) |
| XR4 | Carestream DRX-Compass (Carestream Health, Rochester, NY, USA) |
| XR5 | Discovery RF180 Radiography and Fluoroscopy System (GE HealthCare, Chicago, IL, USA) |
| CT | Discovery HD750 CT scanner (GE HealthCare, Chicago, IL, USA) |
| MRI1 | Philips Ingenia 1.5-T MRI scanner (Philips Healthcare, Best, Netherlands) |
| MRI2 | Philips Ingenia 1.5-T MRI scanner (Philips Healthcare, Best, Netherlands) |
| CBCT | Cone Beam 3D imaging New Tom Giano HD (NewTom Official, Imola, Italy) |
| DXA | GE Lunar iDXA (GE HealthCare, Chicago, IL, USA) |
| MG1 | Hologic 3D Dimensions (Hologic Inc, Marlborough, MA, USA) |
| MG2 | Hologic 3D Dimensions (Hologic Inc, Marlborough, MA, USA) |
| MCXR1 | Carestreams DRX-Revolution (Carestream Health, Rochester, NY, USA) |
| MCXR2 | Carestreams DRX-Revolution (Carestream Health, Rochester, NY, USA) |
| US1 | Esaote MyLab X8c (Esaote SpA, Genoa, Italy) |
| US2 | Esaote MyLab X8c (Esaote SpA, Genoa, Italy) |
| US3 | Esaote MyLab X8c (Esaote SpA, Genoa, Italy) |
| US4 | Samsung Ultrasound system RS85 (Samsung Healthcare, Seoul, Republic of Korea) |
| US5 | Samsung Ultrasound system RS85 (Samsung Healthcare, Seoul, Republic of Korea) |
| Reporting workstations (RWS) (n = 10) | Barco Nio Gray 5.8 MP (Branco NV, Kortrijk, Belgium) |
| RIS/PACS workstations (WS) (n = 27) | HP z600 computer (HP Inc., Palo Alto, CA, USA) |
References
- McKee, H.; Brown, M.J.; Kim, H.H.R.; Doo, F.X.; Panet, H.; Rockall, A.G.; Omary, R.A.; Hanneman, K.; Atzen, S. Planetary Health and Radiology: Why We Should Care and What We Can Do. Radiology 2024, 311, e240219. [Google Scholar] [CrossRef] [PubMed]
- Benmamoun, Z.; Fethallah, W.; Bouazza, S.; Abdo, A.A.; Serrou, D.; Benchekroun, H. A framework for sustainability evaluation and improvement of radiology service. J. Clean. Prod. 2023, 401, 136796. [Google Scholar] [CrossRef]
- Zigmund, B.; Hijaz, T.; Northrup, B.E.; Schoen, J.H.; Hanneman, K.; Brown, M.; Dave, P.; Gross, J.S.; Henry, C.E.; Leschied, J.R.; et al. Public Health Statement of the Association of University Radiologists Committee on Climate Change and Sustainability. Acad. Radiol. 2023, 30, 2358–2361. [Google Scholar] [CrossRef] [PubMed]
- Woolen, S.A.; Kim, C.J.; Hernandez, A.M.; Becker, A.; Martin, A.J.; Kuoy, E.; Pevec, W.C.; Tutton, S. Radiology Environmental Impact: What Is Known and How Can We Improve? Acad. Radiol. 2023, 30, 625–630. [Google Scholar] [CrossRef] [PubMed]
- Sumner, C.; Ikuta, I.; Garg, T.; Martin, J.G.; Mansoori, B.; Chalian, M.; Englander, B.S.; Chertoff, J.; Woolen, S.; Caplin, D.; et al. Approaches to Greening Radiology. Acad. Radiol. 2023, 30, 528–535. [Google Scholar] [CrossRef]
- Martin, M.F.; Maturen, K.E.; Foster, C.; Woolen, S.; Dunnick, N.R. Environmental stewardship and healthcare: Global reflections for radiology. Chin. J. Acad. Radiol. 2022, 5, 244–248. [Google Scholar] [CrossRef]
- Picano, E.; Mangia, C.; D’Andrea, A. Climate Change, Carbon Dioxide Emissions, and Medical Imaging Contribution. J. Clin. Med. 2022, 12, 215. [Google Scholar] [CrossRef]
- Brown, M.; Schoen, J.H.; Gross, J.; Omary, R.A.; Hanneman, K. Climate Change and Radiology: Impetus for Change and a Toolkit for Action. Radiology 2023, 307, e230229. [Google Scholar] [CrossRef]
- Woolen, S.A.; Becker, A.E.; Martin, A.J.; Knoerl, R.; Lam, V.; Folsom, J.; Eusemann, C.; Hess, C.P.; Deshpande, V. Ecodesign and Operational Strategies to Reduce the Carbon Footprint of MRI for Energy Cost Savings. Radiology 2023, 307, e230441. [Google Scholar] [CrossRef]
- Brown, M.; Snelling, E.; De Alba, M.; Ebrahimi, G.; Forster, B.B. Quantitative Assessment of Computed Tomography Energy Use and Cost Savings Through Overnight and Weekend Power Down in a Radiology Department. Can. Assoc. Radiol. J. 2022, 74, 298–304. [Google Scholar] [CrossRef]
- Alshqaqeeq, F.; McGuire, C.; Overcash, M.; Ali, K.; Twomey, J. Choosing radiology imaging modalities to meet patient needs with lower environmental impact. Resour. Conserv. Recycl. 2020, 155, 104657. [Google Scholar] [CrossRef]
- McAlister, S.; McGain, F.; Petersen, M.; Story, D.; Charlesworth, K.; Ison, G.; Barratt, A. The carbon footprint of hospital diagnostic imaging in Australia. Lancet Reg. Health West. Pac. 2022, 24, 100459. [Google Scholar] [CrossRef]
- Martin, M.; Mohnke, A.; Lewis, G.M.; Dunnick, N.R.; Keoleian, G.; Maturen, K.E. Environmental Impacts of Abdominal Imaging: A Pilot Investigation. J. Am. Coll. Radiol. 2018, 15, 1385–1393. [Google Scholar] [CrossRef] [PubMed]
- Javadi, A.; Nezhad, A.E.; Nardelli, P.H.J.; Sahoo, S. Energy Management System for Energy-intensive Radiology Appliances. In Proceedings of the 2023 IEEE International Conference on Environment and Electrical Engineering and 2023 IEEE Industrial and Commercial Power Systems Europe (EEEIC/I&CPS Europe), Madrid, Spain, 6–9 June 2023; pp. 1–6. [Google Scholar] [CrossRef]
- Heye, T.; Knoerl, R.; Wehrle, T.; Mangold, D.; Cerminara, A.; Loser, M.; Plumeyer, M.; Degen, M.; Lüthy, R.; Brodbeck, D.; et al. The energy consumption of Radiology: Energy- And cost-saving opportunities for CT and MRI operation. Radiology 2020, 295, 593–605. [Google Scholar] [CrossRef]
- Esmaeili, A.; McGuire, C.; Overcash, M.; Ali, K.; Soltani, S.; Twomey, J. Environmental impact reduction as a new dimension for quality measurement of healthcare services: The case of magnetic resonance imaging. Int. J. Health Care Qual. Assur. 2018, 31, 910–922. [Google Scholar] [CrossRef]
- Esmaeili, A.; Twomey, J.M.; Overcash, M.R.; Soltani, S.A.; McGuire, C.; Ali, K. Scope for energy improvement for hospital imaging services in the USA. J. Health Serv. Res. Policy 2015, 20, 67–73. [Google Scholar] [CrossRef] [PubMed]
- Hainc, N.; Brantner, P.; Zaehringer, C.; Hohmann, J. “Green Fingerprint” Project: Evaluation of the Power Consumption of Reporting Stations in a Radiology Department. Acad. Radiol. 2020, 27, 1594–1600. [Google Scholar] [CrossRef]
- Büttner, L.; Posch, H.; Auer, T.; Jonczyk, M.; Fehrenbach, U.; Hamm, B.; Bauknecht, H.C.; Böning, G. Switching off for future—Cost estimate and a simple approach to improving the ecological footprint of radiological departments. Eur. J. Radiol. Open 2021, 8, 100320. [Google Scholar] [CrossRef]
- EN 16247-3:2022; Energy Audits—Part 3: Processes. UNI Ente Italiano di Normazione, UNI CEI: Milan, Italy, 2022. Available online: https://www.uni.com (accessed on 31 October 2024).
- ISO 50001:2018; Energy Management Systems—Requirements with Guidance for Use. The International Organization for Standardization: Geneva, Switzerland, 2018. Available online: https://www.iso.org/standard/69426.html (accessed on 31 October 2024).
- Chaban, Y.V.; Vosshenrich, J.; McKee, H.; Gunasekaran, S.; Brown, M.J.; Atalay, M.K.; Heye, T.; Markl, M.; Woolen, S.A.; Simonetti, O.P.; et al. Environmental Sustainability and MRI: Challenges, Opportunities, and a Call for Action. J. Magn. Reson. Imaging 2024, 59, 1149–1167. [Google Scholar] [CrossRef]
- American College of Radiology. ACR Appropriateness Criteria. 2024. Available online: https://www.acr.org/Clinical-Resources/ACR-Appropriateness-Criteria (accessed on 31 October 2024).
- Malik, A.; Padget, M.; Carter, S.; Wakiyama, T.; Maitland-Scott, I.; Vyas, A.; Boylan, S.; Mulcahy, G.; Li, M.; Lenzen, M.; et al. Environmental impacts of Australia’s largest health system. Resour. Conserv. Recycl. 2021, 169, 105556. [Google Scholar] [CrossRef]
- Ibrahim, F.; Cadour, F.; Campbell-Washburn, A.E.; Allen, B.D.; Vosshenrich, J.; Brown, M.J.; Thavendiranathan, P.; Hanneman, K.; Moy, L. Energy and Greenhouse Gas Emission Savings Associated with Implementation of an Abbreviated Cardiac MRI Protocol. Radiology 2024, 311, e240588. [Google Scholar] [CrossRef] [PubMed]
- Leithner, D.; Moy, L.; Morris, E.A.; Marino, M.A.; Helbich, T.H.; Pinker, K. Abbreviated MRI of the Breast: Does It Provide Value? J. Magn. Reson. Imaging 2019, 49, e85–e100. [Google Scholar] [CrossRef] [PubMed]
- Klein, H.-M. A New Approach to the Improvement of Energy Efficiency in Radiology Practices. In RöFo—Fortschritte Auf Dem Gebiet Der Röntgenstrahlen Und Der Bildgebenden Verfahren; Georg Thieme Verlag KG: Stuttgart, Germany, 2023; Volume 195, pp. 416–425. [Google Scholar] [CrossRef]
- Ayde, R.; Senft, T.; Salameh, N.; Sarracanie, M. Deep learning for fast low-field MRI acquisitions. Sci. Rep. 2022, 12, 11394. [Google Scholar] [CrossRef]
- Doo, F.X.; Vosshenrich, J.; Cook, T.S.; Moy, L.; Almeida, E.P.R.P.; Woolen, S.A.; Gichoya, J.W.; Heye, T.; Hanneman, K. Environmental Sustainability and AI in Radiology: A Double-Edged Sword. Radiology 2024, 310, e232030. [Google Scholar] [CrossRef]
- Kopparam, R.V.; Redberg, R.F. The environmental impact of unnecessary imaging: Why less is more. Eur. J. Intern. Med. 2023, 111, 35–36. [Google Scholar] [CrossRef]
- Shahbandegan, A.; Mago, V.; Alaref, A.; van der Pol, C.B.; Savage, D.W. Developing a machine learning model to predict patient need for computed tomography imaging in the emergency department. PLoS ONE 2022, 17, e0278229. [Google Scholar] [CrossRef]
- Rengier, F.; Notohamiprodjo, M.; Weber, M.-A. Thoughts on sustainability in the use of iodinated contrast media in CT: A practice-oriented review based on the example of a hospital and a private practice. In RöFo—Fortschritte Auf Dem Gebiet Der Röntgenstrahlen Und Der Bildgebenden Verfahren; Georg Thieme Verlag KG: Stuttgart, Germany, 2024. [Google Scholar] [CrossRef]
- Dekker, H.M.; Stroomberg, G.J.; Van der Molen, A.J.; Prokop, M. Review of strategies to reduce the contamination of the water environment by gadolinium-based contrast agents. Insights Imaging 2024, 15, 62. [Google Scholar] [CrossRef] [PubMed]
- Clements, W.; Chow, J.; Corish, C.; Tang, V.D.; Houlihan, C. Assessing the Burden of Packaging and Recyclability of Single-Use Products in Interventional Radiology. Cardiovasc. Intervent Radiol. 2020, 43, 910–915. [Google Scholar] [CrossRef]
- Chua, A.L.B.; Amin, R.; Zhang, J.; Thiel, C.L.; Gross, J.S. The Environmental Impact of Interventional Radiology: An Evaluation of Greenhouse Gas Emissions from an Academic Interventional Radiology Practice. J. Vasc. Interv. Radiol. 2021, 32, 907–915.e3. [Google Scholar] [CrossRef]
- Patel, K.B.; Gonzalez, B.D.; Turner, K.; Tabriz, A.A.; Rollison, D.E.; Robinson, E.; Naso, C.; Wang, X.; Spiess, P.E. Estimated Carbon Emissions Savings With Shifts From In-Person Visits to Telemedicine for Patients With Cancer. JAMA Netw. Open 2023, 6, e2253788. [Google Scholar] [CrossRef]
- Dacones, I.; Cave, C.; Furie, G.L.; Ogden, C.A.; Slutzman, J.E. Patient transport greenhouse gas emissions from outpatient care at an integrated health care system in the Northwestern United States, 2015–2020. J. Clim. Change Health 2021, 3, 100024. [Google Scholar] [CrossRef]
- Roletto, A.; Savio, A.; Marchi, B.; Zanoni, S. Towards a Greener Radiology: A Comprehensive Life Cycle Assessment Framework for Diagnostic Imaging. Environ. Clim. Technol. 2024, 28, 303–311. [Google Scholar] [CrossRef]
- Thiel, C.L.; Vigil-Garcia, M.; Nande, S.; Meijer, C.; Gehrels, J.; Struk, O.; Thornander, S.; Pullella, D.; Omary, R.A.; Carver, D.E.; et al. Environmental Life Cycle Assessment of a U.S. Hospital-based Radiology Practice. Radiology 2024, 313, e240398. [Google Scholar] [CrossRef] [PubMed]
- Hanneman, K.; McKee, H.; Nguyen, E.T.; Panet, H.; Kielar, A. Greenhouse Gas Emissions by Diagnostic Imaging Modality in a Hospital-Based Radiology Department. Can. Assoc. Radiol. J. 2024, 75, 950–953. [Google Scholar] [CrossRef]
- Heye, T.; Meyer, M.T.; Merkle, E.M.; Vosshenrich, J. Turn It Off! A Simple Method to Save Energy and CO2 Emissions in a Hospital Setting with Focus on Radiology by Monitoring Nonproductive Energy-consuming Devices. Radiology 2023, 307, e230162. [Google Scholar] [CrossRef]



| Start | End | Opening (h) | Exams per Month | Exams per Day | Exam Time (min) | Time (T) | ||
|---|---|---|---|---|---|---|---|---|
| Active Period (h) | Idle Period (h) | |||||||
| XR 1 | 8:10 | 15:30 | 7.3 | 600 | 30 | 10 | 5.0 | 2.3 |
| XR 2 | 8:10 | 15:30 | 7.3 | 800 | 40 | 10 | 6.7 | 0.6 |
| XR 3 | 8:10 | 15:30 | 7.3 | 200 | 10 | 10 | 1.7 | 5.6 |
| XR 4 | 8:10 | 15:30 | 7.3 | 800 | 40 | 10 | 6.7 | 0.6 |
| XR 5 | 8:10 | 15:30 | 7.3 | 80 | 4 | 10 | 0.6 | 6.7 |
| DXA | 8:10 | 15:30 | 7.3 | 88 | 11 | 10 | 1.8 | 5.5 |
| CBCT | 8:00 | 12:00 | 4.0 | 40 | 10 | 10 | 1.6 | 2.4 |
| CT | 8:10 | 16:30 | 8.3 | 350 | 36 | 10 | 6.2 | 3.1 |
| MRI 1 | 8:10 | 15:30 | 7.3 | 248 | 10 | 35 | 5.8 | 1.5 |
| MRI 2 | 8:10 | 23:30 | 15.3 | 500 | 22 | 35 | 12.8 | 2.5 |
| MG 1 | 8:10 | 19:30 | 11.3 | 660 | 30 | 10 | 5 | 6.3 |
| MG 2 | 8:10 | 15:30 | 7.3 | 40 | 2 | 10 | 0.3 | 7 |
| US 1 | 8:10 | 17:30 | 9.3 | 500 | 25 | 20 | 8.3 | 1 |
| US 2 | 8:10 | 17:30 | 9.3 | 500 | 25 | 20 | 8.3 | 1 |
| US 3 | 8:10 | 15:30 | 7.3 | 200 | 10 | 20 | 3.3 | 4 |
| US 4 | 8:10 | 15:30 | 7.3 | 300 | 15 | 20 | 5 | 2.3 |
| US 5 | 8:10 | 15:30 | 7.3 | 200 | 10 | 20 | 3.3 | 4 |
| MCXR 1 | 0:00 | 24:00 | 24.0 | 10 | 10 | 1.7 | 22.3 | |
| MCXR 2 | 0:00 | 24:00 | 24.0 | 25 | 10 | 4.2 | 19.8 | |
| Different Energy Consumption Periods of Reporting Workstations in the Unit of Radiology | |||
| Active period (h) | Stand-by period (h) | Idle period (h) | |
| RWS 1–2 | 6.5 | 2.1 | 15.4 |
| RWS 3–4 | 5.8 | 2.0 | 16.1 |
| RWS 5–10 | 9.1 | 2.3 | 12.6 |
| Mean | 7.2 | 2.1 | 14.7 |
| Different Energy Consumption Periods of RIS/PACS Workstation in the Unit of Radiology | |||
| Active period (h) | Stand-by period (h) | Idle period (h) | |
| WS (n = 27) Mean | 6.8 | 10.2 | 8.0 |
| Equivalent Mean Power Demand (Peq-act) During Active Phase (kW) | Equivalent Mean Power Demand (Peq-idle) During Idle Phase (kW) | Energy Used (Eact) During Active Period (kWh) | Energy Used (Eidle) During Idle Period (kWh) | |
|---|---|---|---|---|
| XR 1 | 3.7 | 1.1 | 18.5 | 2.5 |
| XR 2 | 3.7 | 1.1 | 24.8 | 0.7 |
| XR 3 | 3.5 | 1.1 | 5.9 | 6.2 |
| XR 4 | 3.5 | 1.1 | 23.4 | 0.7 |
| XR 5 | 3.3 | 1.0 | 2.0 | 7.3 |
| DXA | 2.3 | 0.7 | 4.1 | 3.9 |
| CBCT | 1.9 | 1.5 | 3.0 | 3.6 |
| CT | 16.4 | 4.0 | 45.9 | 12.4 |
| MRI 1 | 19 | 19 | 110.2 | 28.2 |
| MRI 2 | 19 | 19 | 243.2 | 47.5 |
| MG 1 | 4.3 | 1.8 | 21.5 | 11.3 |
| MG 2 | 4.3 | 1.8 | 1.3 | 12.6 |
| US 1 | 1.1 | 1.1 | 9.1 | 1.1 |
| US 2 | 1.1 | 1.1 | 9.1 | 1.1 |
| US 3 | 1.1 | 1.1 | 3.7 | 4.4 |
| US 4 | 1.1 | 1.1 | 5.5 | 2.5 |
| US 5 | 1.1 | 1.1 | 3.7 | 4.4 |
| MCXR 1 | 2.8 | 0.2 | 4.8 | 4.4 |
| MCXR 2 | 2.8 | 0.2 | 11.8 | 3.9 |
| Total | 664.2 | 201.3 |
| Equivalent Mean Power Demand (Peq) (kW) [Active/Idle/Stand-By] | Total Energy Active Period (kWh) | Total Energy Idle Period (kWh) | Total Energy Stand-By Period (kWh) | |
|---|---|---|---|---|
| RW (n = 10) | 0.5/0.28/0.02 | 37.0 | 5.8 | 2.9 |
| WS (n = 27) | 0.3/0.17/0.02 | 55.0 | 46.8 | 4.3 |
| Total | 100.5 | 58.8 | 8 |
| Active Period Before (kWh) | Active Period After (kWh) | Δ Active Period (%) | Idle Period Before (kWh) | Idle Period After (kWh) | Δ Idle Period (%) | Total Energy Before (kWh) | Total Energy After (kWh) | Δ Total Energy (%) | |
|---|---|---|---|---|---|---|---|---|---|
| XR5 | 2 | 3.6 | 80.0% | 7.3 | 6.2 | −15.1% | 9.3 | 9.8 | 5.4% |
| CBCT | 3 | 3.7 | 23.3% | 3.6 | 0.0 | −100% | 6.6 | 3.7 | −44.0% |
| MG1 | 21.5 | 11.6 | −46.0% | 11.4 | 8.3 | −27.2% | 32.9 | 19.9 | |
| MG2 | 1.3 | 11.6 | 792.3% | 12.6 | 8.3 | −34.1% | 13.9 | 19.9 | |
| Total MG | 22.8 | 23.2 | 1.8% | 24 | 16.6 | −30.8% | 46.8 | 39.8 | −15.0% |
| MCXR2 | 11.8 | 16.3 | 38.1% | 3.9 | 3.6 | −7.7% | 15.7 | 19.9 | |
| MCXR1 | 4.8 | 0.0 | −100.0% | 4.4 | 0.0 | −100.0% | 9.2 | 0.0 | |
| Total MCXR | 16.6 | 16.3 | −1.8% | 8.3 | 3.6 | −56.6% | 24.9 | 19.9 | −20.1% |
| Total Modalities | 83.8 | 86.3 | 3.0% | 75.5 | 46.6 | −38.3% | 159.3 | 132.9 | −16.6% |
| Num. Exams | Clinical Question | Diagnostic Exams Performed | Low-Energy Alternative | Actual Energy Consumption (kWh) | Alternative Energy Consumption (kWh) | Δ Total Energy (%) |
|---|---|---|---|---|---|---|
| 22 | Generic abdominal pain | XR | US | 77 | 24.2 | −68.6% |
| 5 | Renal colic | XR + CT | US + XR | 99.5 | 23 | −76.9% |
| 6 | Air-fluid levels | XR + CT | US + XR | 119.4 | 27.6 | −76.9% |
| 8 | Chronic hepatitis | CT | US | 131.2 | 8.8 | −93.3% |
| Total: 41 | 427.1 | 83.6 | −80.4% |
| Active Before (kWh) | Active After (kWh) | Idle Before (kWh) | Idle After (kWh) | Stand-By Before (kWh) | Stand-By After (kWh) | Total Energy Before (kWh) | Total Energy After (kWh) | Δ Total Energy (%) | |
|---|---|---|---|---|---|---|---|---|---|
| WS (n = 27) | 55.0 | 45.3 | 46.7 | 5.5 | 4.3 | 9.3 | 106.0 | 60.1 | −43.3% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Roletto, A.; Savio, A.; Masperi, A.; Bonfitto, G.R.; Pala, F.; Migliorisi, C.; Zanoni, S. Energy Usage Assessment and Energy Savings Estimation in a Radiology Department in Italy. Energies 2025, 18, 1936. https://doi.org/10.3390/en18081936
Roletto A, Savio A, Masperi A, Bonfitto GR, Pala F, Migliorisi C, Zanoni S. Energy Usage Assessment and Energy Savings Estimation in a Radiology Department in Italy. Energies. 2025; 18(8):1936. https://doi.org/10.3390/en18081936
Chicago/Turabian StyleRoletto, Andrea, Anna Savio, Andrea Masperi, Giuseppe Roberto Bonfitto, Fabio Pala, Carmelo Migliorisi, and Simone Zanoni. 2025. "Energy Usage Assessment and Energy Savings Estimation in a Radiology Department in Italy" Energies 18, no. 8: 1936. https://doi.org/10.3390/en18081936
APA StyleRoletto, A., Savio, A., Masperi, A., Bonfitto, G. R., Pala, F., Migliorisi, C., & Zanoni, S. (2025). Energy Usage Assessment and Energy Savings Estimation in a Radiology Department in Italy. Energies, 18(8), 1936. https://doi.org/10.3390/en18081936







