Binocular Advantage in Established Eye–Hand Coordination Tests in Young and Healthy Adults
Abstract
1. Introduction
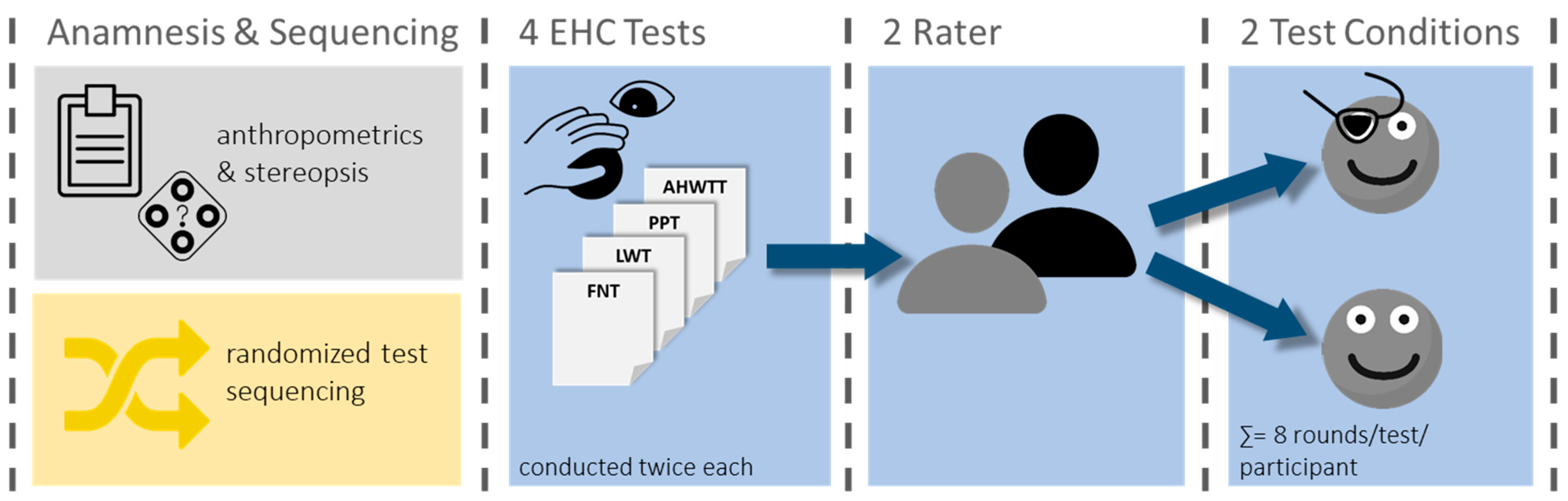
2. Materials and Methods
2.1. Participants
2.2. Eye–Hand Coordination Assessment
2.3. Statistics
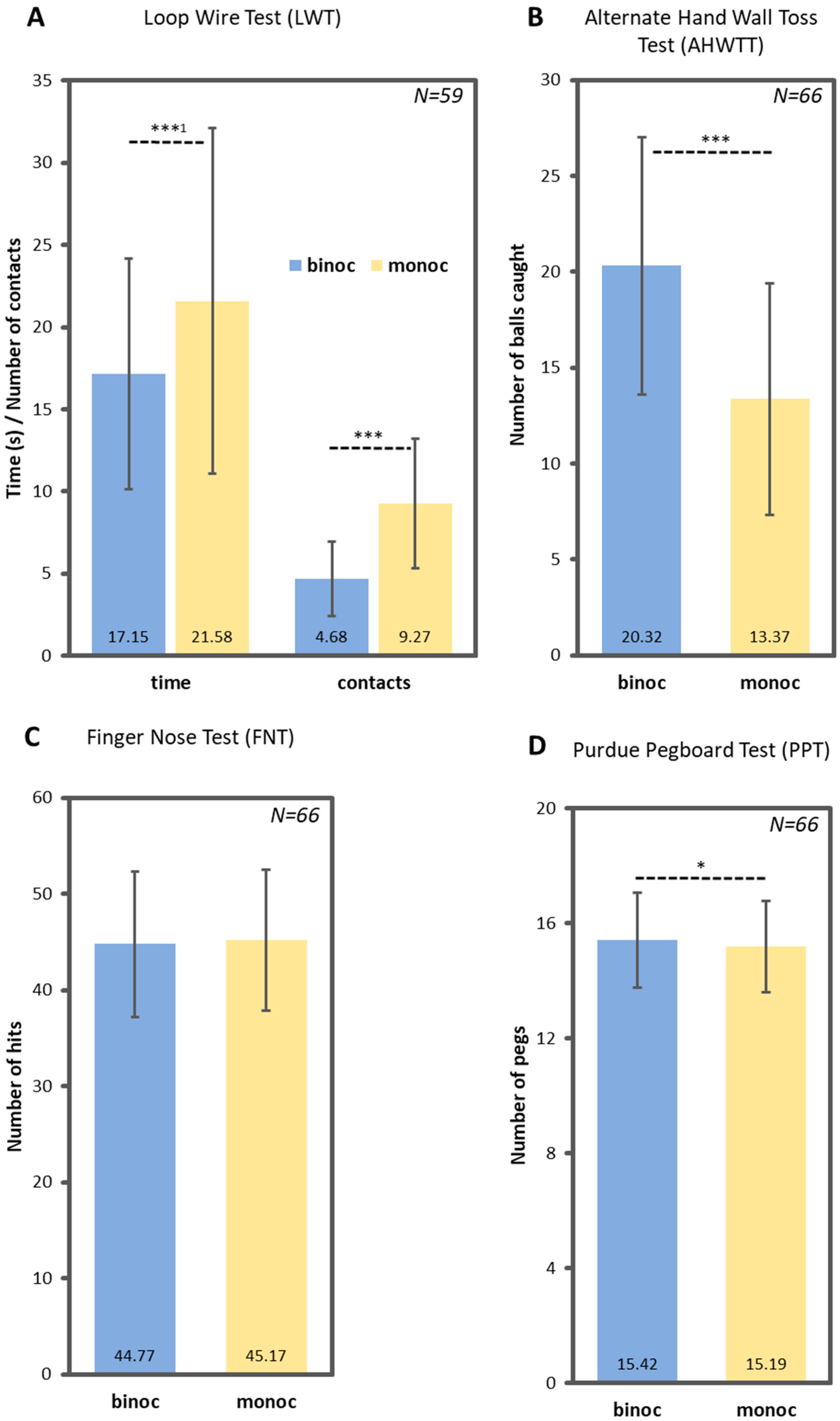
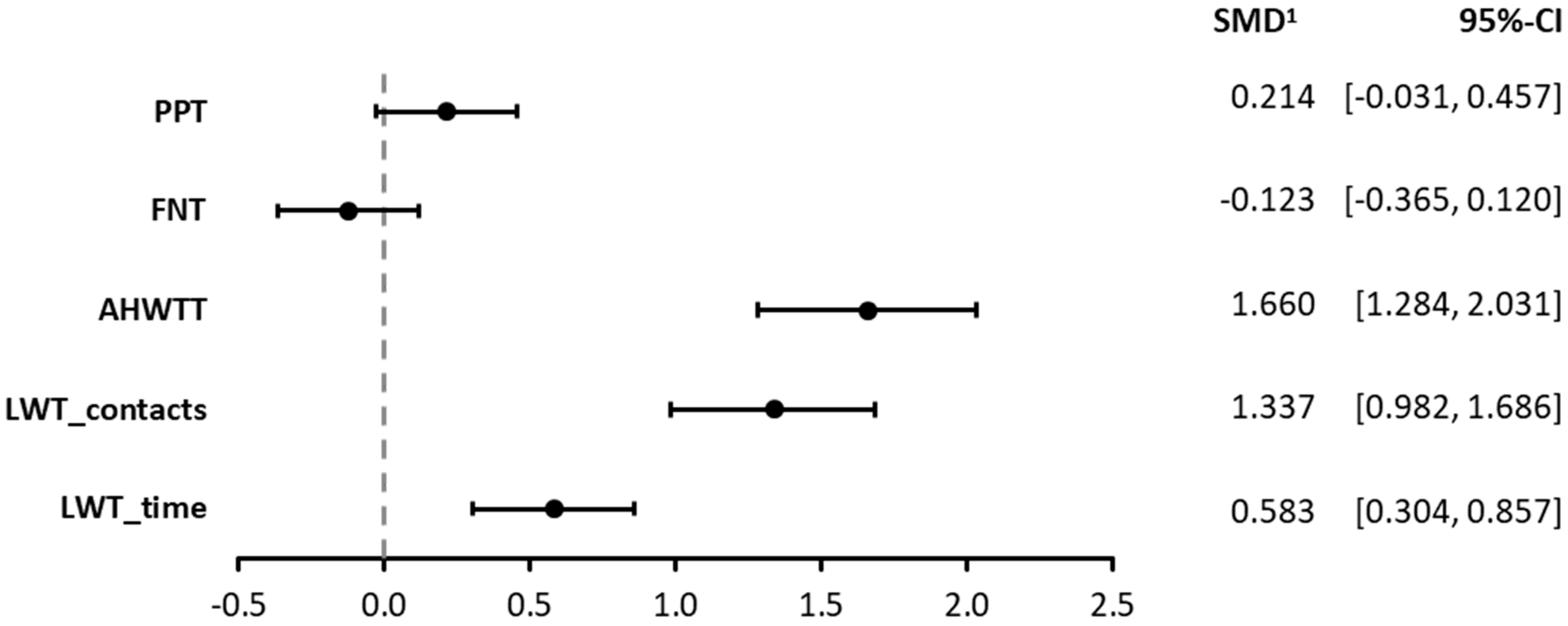
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Correction Statement
Abbreviations
| AHWTT | Alternate Hand Wall Toss Test |
| EHC | Eye–Hand Coordination |
| FNT | Finger–Nose Test |
| LWT | Loop-Wire Test |
| PPT | Purdue Pegboard Test |
References
- Congdon, N.; O’Colmain, B.; Klaver, C.C.W.; Klein, R.; Muñoz, B.; Friedman, D.S.; Kempen, J.; Taylor, H.R.; Mitchell, P.; Eye Diseases Prevalence Research Group. Causes and prevalence of visual impairment among adults in the United States. Arch. Ophthalmol. 2004, 122, 477–485. [Google Scholar] [CrossRef] [PubMed]
- Coday, M.P.; Warner, M.A.; Jahrling, K.V.; Rubin, P.A.D. Acquired monocular vision: Functional consequences from the patient’s perspective. Ophthalmic Plast. Reconstr. Surg. 2002, 18, 56–63. [Google Scholar] [CrossRef]
- Damato, B.; Hope-Stone, L.; Cooper, B.; Brown, S.L.; Salmon, P.; Heimann, H.; Dunn, L.B. Patient-reported Outcomes and Quality of Life After Treatment of Choroidal Melanoma: A Comparison of Enucleation Versus Radiotherapy in 1596 Patients. Am. J. Ophthalmol. 2018, 193, 230–251. [Google Scholar] [CrossRef] [PubMed]
- Groff, M.L.; Choi, B.; Lin, T.; Mcllraith, I.; Hutnik, C.; Malvankar-Mehta, M.S. Anxiety, depression, and sleep-related outcomes of glaucoma patients: Systematic review and meta-analysis. Can. J. Ophthalmol. 2023, 58, 346–355. [Google Scholar] [CrossRef]
- Rees, G.; Xie, J.; Fenwick, E.K.; Sturrock, B.A.; Finger, R.; Rogers, S.L.; Lim, L.; Lamoureux, E.L. Association Between Diabetes-Related Eye Complications and Symptoms of Anxiety and Depression. JAMA Ophthalmol. 2016, 134, 1007–1014. [Google Scholar] [CrossRef] [PubMed]
- Harris, J.M.; McKee, S.P.; Smallman, H.S. Fine-scale processing in human binocular stereopsis. J. Opt. Soc. Am. A Opt. Image Sci. Vis. 1997, 14, 1673–1683. [Google Scholar] [CrossRef]
- Devi, P.; Solomon, J.A.; Tyler, C.W.; Dave, T.V.; Kaliki, S.; Bharadwaj, S.R. Comparison of Depth-Related Visuomotor Task Performance in Uniocular Individuals and in Binocular Controls with and Without Temporary Monocular Occlusion. Invest. Ophthalmol. Vis. Sci. 2024, 65, 32. [Google Scholar] [CrossRef]
- Gonzalez, D.A.; Niechwiej-Szwedo, E. The effects of monocular viewing on hand-eye coordination during sequential grasping and placing movements. Vis. Res. 2016, 128, 30–38. [Google Scholar] [CrossRef]
- Grant, S. Gaze-grasp coordination in obstacle avoidance: Differences between binocular and monocular viewing. Exp. Brain Res. 2015, 233, 3489–3505. [Google Scholar] [CrossRef]
- Schiller, P.H.; Kendall, G.L.; Kwak, M.C.; Slocum, W.M. Depth Perception, Binocular Integration and Hand-Eye Coordination in Intact and Stereo Impaired Human Subjects. J. Clinic. Experiment. Ophthalmol. 2012, 3, 1000210. [Google Scholar] [CrossRef]
- O’Connor, A.R.; Birch, E.E.; Anderson, S.; Draper, H. The functional significance of stereopsis. Invest. Ophthalmol. Vis. Sci. 2010, 51, 2019–2023. [Google Scholar] [CrossRef] [PubMed]
- Read, J.C.A.; Begum, S.F.; McDonald, A.; Trowbridge, J. The binocular advantage in visuomotor tasks involving tools. i-Perception 2013, 4, 101–110. [Google Scholar] [CrossRef] [PubMed]
- Buys, J.H.C.; Ferreira, J.T. The development of protocols and norms for sports vision evaluations. Afr. Vis. Eye Health 2008, 67, 106–117. [Google Scholar] [CrossRef]
- Ihrig, C.; Schaefer, D.P. Acquired Monocular Vision Rehabilitation program. J. Rehabil. Res. Dev. 2007, 44, 593–597. [Google Scholar] [CrossRef]
- Mendes Wefelnberg, M. Four month of exercise intervention improve visuomotor, function and cardiorespiratory capacity in patient with metastatic uveal melanoma: A case study. Case Rep. Ophthalmol. 2024, in press.
- Wefelnberg, M.M.; Moll, M.; von Stein, P.; Guthoff, H.; Heindl, L.M.; Reimer, P.W.M.; Rokohl, A.C.; Simon, M.; Zubac, D.; Baumann, F.T. Eight weeks of exercise intervention improves visuomotor and functional capacity, performance, and physiological profile in a patient with choroidal melanoma. J. Appl. Physiol. 2024, 136, 799–806. [Google Scholar] [CrossRef]
- Robinson, O.C. Sampling in Interview-Based Qualitative Research: A Theoretical and Practical Guide. Qual. Res. Psychol. 2014, 11, 25–41. [Google Scholar] [CrossRef]
- Lang, J.I.; Lang, T.J. Eye Screening with the Lang Stereotest. Am. Orthopt. J. 1988, 38, 48–50. [Google Scholar] [CrossRef]
- Safra, D. Der “Ringtest” zur Prüfung der Augendominanz. [The “Ring Test” for evaluating eye dominance]. Klin Monbl Augenheilkd 1989, 195, 35–36. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Desrosiers, J.; Hébert, R.; Bravo, G.; Dutil, E. The Purdue Pegboard Test: Normative data for people aged 60 and over. Disabil. Rehabil. 1995, 17, 217–224. [Google Scholar] [CrossRef] [PubMed]
- Agnew, J.; Bolla-Wilson, K.; Kawas, C.; Bleecker, M. Purdue pegboard age and sex norms for people 40 years old and older. HDVN 1988, 4, 29–35. [Google Scholar] [CrossRef]
- Mathiowetz, V.; Rogers, S.L.; Dowe-Keval, M.; Donahoe, L.; Rennells, C. The Purdue Pegboard: Norms for 14- to 19-year-olds. Am. J. Occup. Ther. 1986, 40, 174–179. [Google Scholar] [CrossRef]
- Wittich, W.; Nadon, C. The Purdue Pegboard test: Normative data for older adults with low vision. Disabil. Rehabil. Assist. Technol. 2017, 12, 272–279. [Google Scholar] [CrossRef] [PubMed]
- Swaine, B.R.; Desrosiers, J.; Bourbonnais, D.; Larochelle, J.-L. Norms for 15- to 34-year-olds for different versions of the finger-to-nose test. Arch. Phys. Med. Rehabil. 2005, 86, 1665–1669. [Google Scholar] [CrossRef]
- Cho, E.; Yun, H.; So, W. The validity validity of alternative hand wall toss tests in Korean children. JOMH 2020, 16, 10. [Google Scholar] [CrossRef]
- Rosengren, K.S.; Pick, H.L. Hofsten Cvon Role of visual information in ball catching. J. Mot. Behav. 1988, 20, 150–164. [Google Scholar] [CrossRef]
- Mazyn, L.I.N.; Lenoir, M.; Montagne, G.; Savelsbergh, G.J.P. The contribution of stereo vision to one-handed catching. Exp. Brain Res. 2004, 157, 383–390. [Google Scholar] [CrossRef]
- Olivier, I.; Weeks, D.J.; Lyons, J.; Ricker, K.L.; Elliott, D. Monocular and binocular vision in one-hand ball catching: Interocular integration. J. Mot. Behav. 1998, 30, 343–351. [Google Scholar] [CrossRef]
- Sykes Tottenham, L.; Saucier, D.M.; Elias, L.J.; Gutwin, C. Men are more accurate than women in aiming at targets in both near space and extrapersonal space. Percept. Mot. Ski. 2005, 101, 3–12. [Google Scholar] [CrossRef]
- Mazyn, L.I.N.; Lenoir, M.; Montagne, G.; Delaey, C.; Savelsbergh, G.J.P. Stereo vision enhances the learning of a catching skill. Exp. Brain Res. 2007, 179, 723–726. [Google Scholar] [CrossRef] [PubMed]
- Kunoh, K.; Kimura, D.; Murai, S.; Kaiko, T.; Tomiyama, N.; Yamada, K. Relevance of Visual Acuity and Depth Perception to Performance on the Purdue Pegboard Test. Optom. Vis. Perform. 2024, 12, 158–163. [Google Scholar]
- Adrian, J.; Le Brun, J.; Miller, N.R.; Sahel, J.-A.; Saillant, G.; Bodaghi, B. Implications of monocular vision for racing drivers. PLoS ONE 2019, 14, e0226308. [Google Scholar] [CrossRef] [PubMed]
- Stijic, M.; Petrovic, K.; Schwingenschuh, P.; Koini, M.; Schmidt, R. The Purdue Pegboard Test: Normative Data From 1,355 Healthy People from Austria. Am. J. Occup. Ther. 2023, 77, 7703205030. [Google Scholar] [CrossRef]
| Sample | Rater 1 | Rater 1 and 2 |
|---|---|---|
| N | 66 | 45 |
| Age (years), M (SD) | 22.4 (2.8) | 21.7 (2.4) |
| Sex, N (%) | ||
| Female | 28 (42) | 17 (38) |
| Male | 38 (58) | 28 (62) |
| Visual Impairment, N (%) | ||
| Myopia | 15 (23) | 8 (17) |
| Hyperopia | 6 (9) | 5 (12) |
| None | 45 (68) | 32 (71) |
| Stereopsis (Lang Test), N (%) | ||
| Full | 64 (97) | 43 (96) |
| Limited (2/3 of images recognized) | 2 (3) | 2 (4) |
| Eye Dominance, N (%) | ||
| Right | 42 (64) | 27 (60) |
| Left | 24 (36) | 18 (40) |
| Ball Sports, N (%) | ||
| Yes | 31 (47) | 22 (49) |
| No | 35 (53) | 23 (51) |
| Male (N = 38) | Female (N = 28) | |||
|---|---|---|---|---|
| M | SD | M | SD | |
| Binocular | ||||
| LWTtime 1 | 17.28 | 7.86 | 16.78 | 5.87 |
| LWTcontacts 1 | 4.49 | 2.18 | 4.9 | 2.47 |
| AHWTT (balls) | 23.55 | 5.73 | 15.71 | 5.06 |
| PPT (pegs) | 14.60 | 1.52 | 16.71 | 1.19 |
| FNT (contacts) | 44.57 | 8.68 | 45.41 | 5.72 |
| Monocular | ||||
| LWTtime 1 | 22.34 | 10.99 | 19.66 | 8.99 |
| LWTcontacts 1 | 9.38 | 4.11 | 8.68 | 3.47 |
| AHWTT (balls) | 16.28 | 5.40 | 9.11 | 4.32 |
| PPT (pegs) | 14.69 | 1.51 | 16.08 | 1.23 |
| FNT (contacts) | 45.72 | 8.39 | 44.86 | 5.88 |
| Binocular advantage 2 | ||||
| LWTtime 1 | 1.33 | 0.44 | 1.17 | 0.31 |
| LWTcontacts 1 | 2.39 | 1.22 | 2.16 | 1.33 |
| AHWTT (balls) | 1.51 | 0.34 | 1.97 | 0.68 |
| PPT (pegs) | 1.00 | 0.07 | 1.04 | 0.06 |
| FNT (contacts) | 0.97 | 0.07 | 1.02 | 0.07 |
| LWT (N = 38) | AHWTT (N = 45) | FNT (N = 45) | PPT (N = 45) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Bin | Mon | Bin | Mon | Bin | Mon | Bin | Mon | ||
| Time | Contacts | Time | Contacts | ||||||
| 0.83 1 *** | 0.73 2 *** | 0.68 1 *** | 0.66 2 *** | 0.88 2 *** | 0.82 2 *** | 0.60 2 *** | 0.65 2 *** | 0.69 2 *** | 0.67 2 *** |
| Binocular | Monocular | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| (N = 66) | (N = 59) | (N = 66) | (N = 59) | |||||||
| AHWTT | FNT | PPT | LWT | AHWTT | FNT | PPT | LWT | |||
| Time | Contacts | Time | Contacts | |||||||
| LWT | ||||||||||
| Time | −0.16 1 (0.217) | −0.06 1 (0.676) | −0.05 1 (0.712) | 1.00 1 | 0.19 1 (0.154) | −0.08 1 (0.559) | −0.15 1 (0.243) | −0.03 1 (0.852) | 1.00 1 | 0.67 *** 1 (<0.001) |
| Contacts | 0.03 (0.810) | −0.06 (0.670) | −0.08 (0.547) | 0.19 1 (0.154) | 1.00 | 0.03 (0.836) | −0.13 (0.322) | −0.09 (0.491) | 0.67 *** 1 (<0.001) | 1.00 |
| AHWTT | 1.00 | 0.24 (0.055) | −0.29 * (0.017) | −0.16 1 (0.217) | 0.03 (0.810) | 1.00 | 0.33 ** (0.006) | −0.22 (0.076) | −0.08 1 (0.559) | 0.03 (0.836) |
| FNT | 0.24 (0.055) | 1.00 | 0.24 (0.051) | −0.06 1 0.676 | −0.06 0.670 | 0.33 ** (0.006) | 1.00 | 0.23 (0.069) | −0.15 1 0.243 | −0.13 (0.322) |
| PPT | −0.29 * (0.017) | 0.24 (0.051) | 1.00 | −0.05 1 (0.712) | −0.08 (0.547) | −0.22 (0.076) | 0.23 (0.069) | 1.00 | −0.03 1 (0.852) | −0.09 (0.491) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mendes Wefelnberg, M.; Bargstedt, F.; Lippert, M.; Baumann, F.T. Binocular Advantage in Established Eye–Hand Coordination Tests in Young and Healthy Adults. J. Eye Mov. Res. 2025, 18, 14. https://doi.org/10.3390/jemr18030014
Mendes Wefelnberg M, Bargstedt F, Lippert M, Baumann FT. Binocular Advantage in Established Eye–Hand Coordination Tests in Young and Healthy Adults. Journal of Eye Movement Research. 2025; 18(3):14. https://doi.org/10.3390/jemr18030014
Chicago/Turabian StyleMendes Wefelnberg, Michael, Felix Bargstedt, Marcel Lippert, and Freerk T. Baumann. 2025. "Binocular Advantage in Established Eye–Hand Coordination Tests in Young and Healthy Adults" Journal of Eye Movement Research 18, no. 3: 14. https://doi.org/10.3390/jemr18030014
APA StyleMendes Wefelnberg, M., Bargstedt, F., Lippert, M., & Baumann, F. T. (2025). Binocular Advantage in Established Eye–Hand Coordination Tests in Young and Healthy Adults. Journal of Eye Movement Research, 18(3), 14. https://doi.org/10.3390/jemr18030014






