Eye Movements in Mild Traumatic Brain Injury: Clinical Challenges
Abstract
:Introduction
mTBI Diagnosis and Challenges
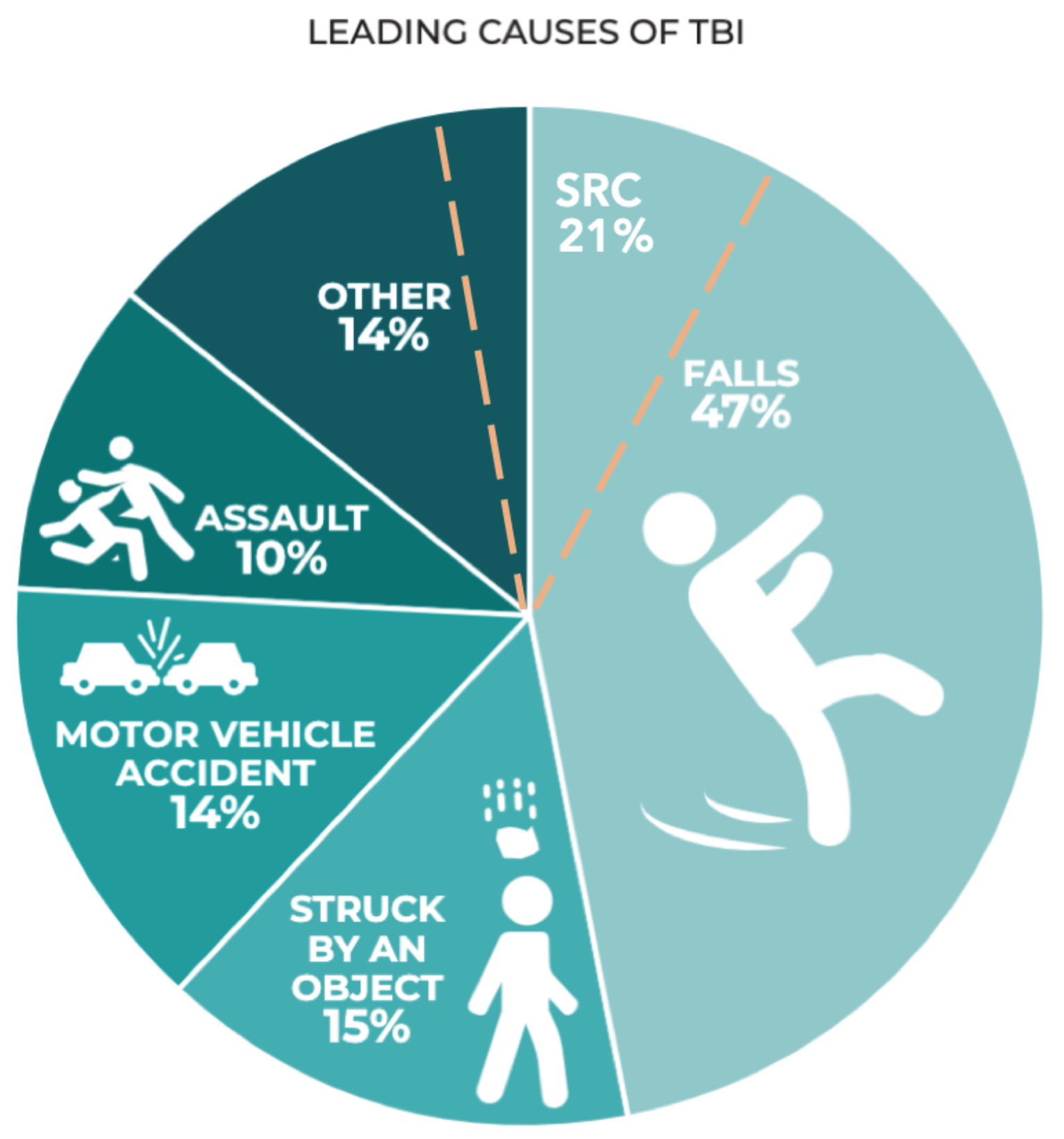
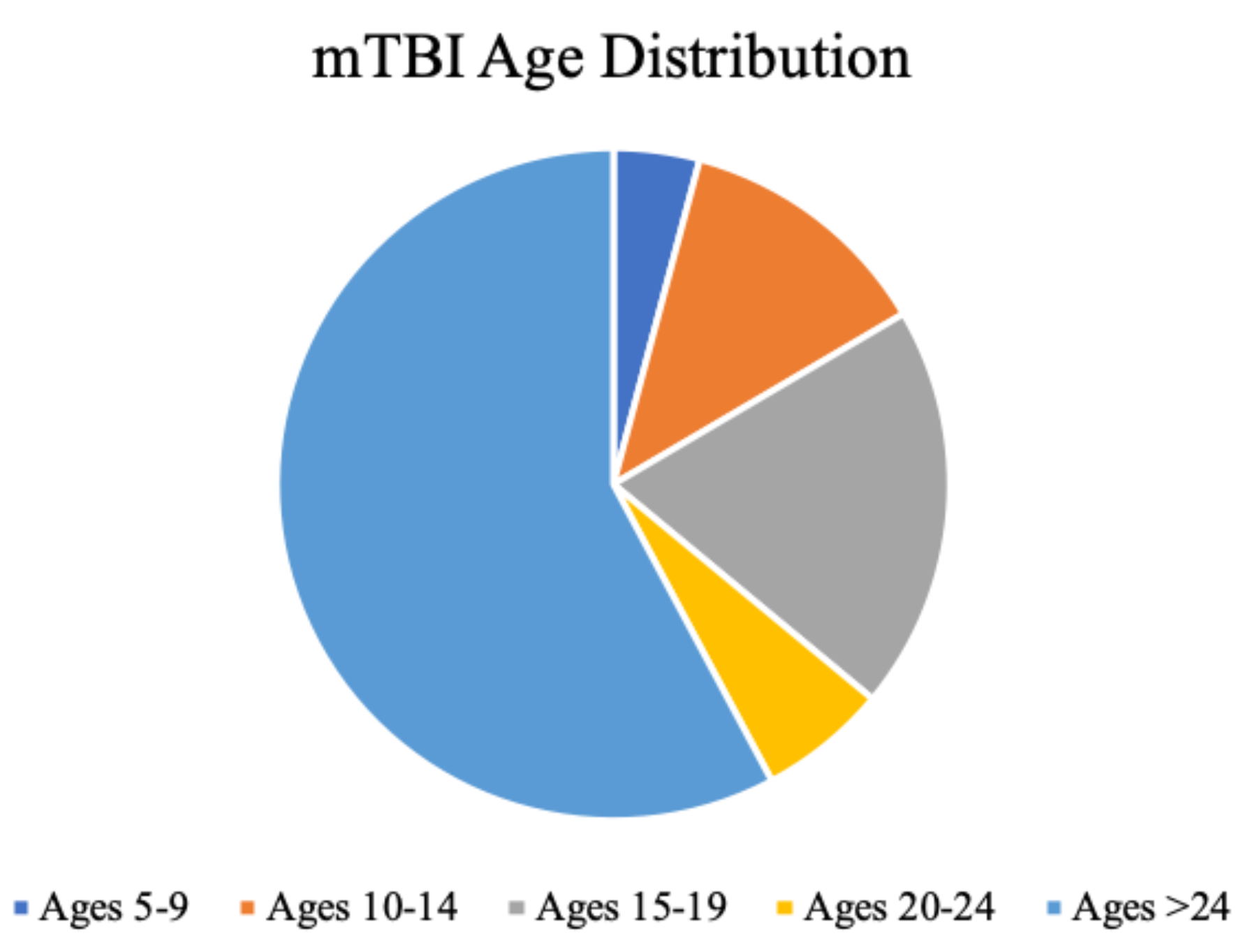
Epidemiology
Gender
Ethnicity
mTBI Subtypes
| Subtype/ “Cluster” | Symptom | Association | Prevalence |
| Migraine | Headache, sensitivity to light/ noise, and nausea | Concomitant cognitive, balance, and vestibulo-ocular motor symptoms which correlated to prolonged recovery | 24% |
| Cognitiveemotional | Difficulty concentrating, remembering, ‘fogginess’, increased emotion, irritability, sadness, nervousness, and ‘feeling slowed down’. | Prolonged recovery, balance deficits, and greater total symptom severity scores | 19% |
| Sleepemotional | Trouble falling asleep, sleeping less (and more), increased emotion, irritiability, sadness, nervousness | Prolonged recovery, lower sleep quantity, cognitive impairment, balance impairment, and greater total symptom severity scores. | 21% |
| Neurological | Blurred vision, vomiting, neck pain, pressure in the head, visual problems, and double vision. | Associated with vestibulo-ocular motor screening symptoms. | 2% |
| Undefined feelings cluster | “Not feeling right” and confusion | No evidence to correlate this to a specific clinical outcome. | Not quantifiable in literature |
Prognosis and Risk Factors
Postconcussion Syndrome (PCS)
Pathophysiology
Conclusion
Ethics and Conflicts of Interest
Acknowledgments
References
- (WHO), W. H. O. 1992. International Statistical Classification of Diseases and Related Health Problems, 10th ed. World Health Organization. [Google Scholar]
- Alosco, M. L., A. B. Kasimis, J. M. Stamm, A. S. Chua, C. M. Baugh, D. H. Daneshvar, C. A. Robbins, M. Mariani, J. Hayden, S. Conneely, R. Au, A. Torres, M. D. McClean, A. C. McKee, R. C. Cantu, J. Mez, C. J. Nowinski, B. M. Martin, C. E. Chaisson, Y. Tripodis, and R. A. Stern. 2017. Age of first exposure to American football and long-term neuropsychiatric and cognitive outcomes [Article]. Translational psychiatry 7, 9: e1236. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association, A. 1994. DSM-IV: Diagnostic and Statistical Manual of Mental Disorders, ed 4. [Google Scholar] [CrossRef]
- American Psychiatric Association, A. 2013. Diagnostic and statistical manual of mental disorders.
- Aungst, S. L., S. V. Kabadi, S. M. Thompson, B. A. Stoica, and A. I. Faden. 2014. Repeated mild traumatic brain injury causes chronic neuroinflammation, changes in hippocampal synaptic plasticity, and associated cognitive deficits. J Cereb Blood Flow Metab 34, 7: 1223–1232. [Google Scholar] [CrossRef]
- Baker, J. F., B. M. Devitt, J. Green, and C. McCarthy. 2013. Concussion among under 20 rugby union players in Ireland: incidence, attitudes and knowledge. Ir J Med Sci 182, 1: 121–125. [Google Scholar] [CrossRef]
- Baker, J. G., J. J. Leddy, S. R. Darling, B. P. Rieger, T. L. Mashtare, T. Sharma, and B. S. Willer. 2015. Factors Associated With Problems for Adolescents Returning to the Classroom After Sport-Related Concussion. Clin Pediatr (Phila) 54, 10: 961–968. [Google Scholar] [CrossRef] [PubMed]
- Baker, J. G., J. J. Leddy, S. R. Darling, J. Shucard, M. Makdissi, and B. S. Willer. 2016. Gender differences in recovery from sports-related concussion in adolescents. Clin Pediatr (Phila) 55, 8: 771–775. [Google Scholar] [CrossRef]
- Barlow, K. M., S. Crawford, B. L. Brooks, B. Turley, and A. Mikrogianakis. 2015. The Incidence of Postconcussion Syndrome Remains Stable Following Mild Traumatic Brain Injury in Children. Pediatric Neurology 53, 6: 491–497. [Google Scholar] [CrossRef] [PubMed]
- Bazarian, J. J., T. Wong, M. Harris, N. Leahey, S. Mookerjee, and M. Dombovy. 1999. Epidemiology and predictors of post-concussive syndrome after minor head injury in an emergency population. Brain Inj 13, 3: 173–189. [Google Scholar] [CrossRef]
- Blaylock, R. L., and J. Maroon. 2011. Immunoexcitotoxicity as a central mechanism in chronic traumatic encephalopathy-A unifying hypothesis. Surgical neurology international 2: 107–107. [Google Scholar] [CrossRef]
- Bloodgood, B., D. Inokuchi, W. Shawver, K. Olson, R. Hoffman, E. Cohen, K. Sarmiento, and K. Muthuswamy. 2013. Exploration of awareness, knowledge, and perceptions of traumatic brain injury among American youth athletes and their parents. J Adolesc Health 53, 1: 34–39. [Google Scholar] [CrossRef]
- Bogduk, N., and J. Govind. 2009. Cervicogenic headache: an assessment of the evidence on clinical diagnosis, invasive tests, and treatment. The Lancet Neurology 8, 10: 959–968. [Google Scholar] [CrossRef] [PubMed]
- Borg, J., L. Holm, J. D. Cassidy, P. M. Peloso, L. J. Carroll, H. von Holst, and K. Ericson. 2004. Diagnostic procedures in mild traumatic brain injury: results of the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. J Rehabil Med, 61–75. [Google Scholar] [CrossRef]
- Broshek, D. K., T. Kaushik, J. R. Freeman, D. Erlanger, F. Webbe, and J. T. Barth. 2005. Sex differences in outcome following sports-related concussion. Journal of Neurosurgery 102, 5: 856–863. [Google Scholar] [CrossRef] [PubMed]
- Carroll, L. J., J. D. Cassidy, L. Holm, J. Kraus, and V. G. Coronado. 2004. Methodological issues and research recommendations for mild traumatic brain injury: the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. J Rehabil Med, 113–125. [Google Scholar] [CrossRef]
- Clausen, M., D. R. Pendergast, B. Willer, and J. Leddy. 2016. Cerebral Blood Flow During Treadmill Exercise Is a Marker of Physiological Postconcussion Syndrome in Female Athletes. J Head Trauma Rehabil 31, 3: 215–224. [Google Scholar] [CrossRef] [PubMed]
- Colvin, A. C., J. Mullen, M. R. Lovell, R. V. West, M. W. Collins, and M. Groh. 2009. The role of concussion history and gender in recovery from soccer-related concussion. The American journal of sports medicine 37, 9: 1699–1704. [Google Scholar] [CrossRef]
- Corwin, D. J., M. R. Zonfrillo, C. L. Master, K. B. Arbogast, M. F. Grady, R. L. Robinson, A. M. Goodman, and D. J. Wiebe. 2014. Characteristics of prolonged concussion recovery in a pediatric subspecialty referral population. J Pediatr 165, 6: 1207–1215. [Google Scholar] [CrossRef]
- Covassin, T., R. Moran, and R. J. Elbin. 2016. Sex Differences in Reported Concussion Injury Rates and Time Loss From Participation: An Update of the National Collegiate Athletic Association Injury Surveillance Program From 2004-2005 Through 2008-2009. Journal of Athletic Training 51, 3: 189–194. [Google Scholar] [CrossRef]
- Covassin, T., C. B. Swanik, M. Sachs, Z. Kendrick, P. Schatz, E. Zillmer, and C. Kaminaris. 2006. Sex differences in baseline neuropsychological function and concussion symptoms of collegiate athletes. Br J Sports Med 40, 11: 923–927; discussion 927. [Google Scholar] [CrossRef]
- Deb, S., I. Lyons, and C. Koutzoukis. 1998. Neuropsychiatric sequelae one year after a minor head injury. J Neurol Neurosurg Psychiatry 65, 6: 899–902. [Google Scholar] [CrossRef]
- Dewan, M. C., A. Rattani, S. Gupta, R. E. Baticulon, Y. C. Hung, M. Punchak, A. Agrawal, A. O. Adeleye, M. G. Shrime, A. M. Rubiano, J. V. Rosenfeld, and K. B. Park. 2018. Estimating the global incidence of traumatic brain injury. J Neurosurg, 1–18. [Google Scholar] [CrossRef]
- Dick, R. W. 2009. Is there a gender difference in concussion incidence and outcomes? Br J Sports Med 43 Suppl 1: i46–50. [Google Scholar] [CrossRef] [PubMed]
- England, P. H. 2020. Falls: applying all our health. 1/11. Retrieved 1/11 from https://www.gov.uk/government/publications/falls-applying-all-our-health/falls-applying-all-ourhealth.
- Esposito, G., J. D. Van Horn, D. R. Weinberger, and K. F. Berman. 1996. Gender differences in cerebral blood flow as a function of cognitive state with PET. J Nucl Med 37, 4: 559–564. [Google Scholar] [PubMed]
- Feigin, V. L., A. Theadom, S. Barker-Collo, N. J. Starkey, K. McPherson, M. Kahan, A. Dowell, P. Brown, V. Parag, R. Kydd, K. Jones, A. Jones, and S. Ameratunga. 2013. Incidence of traumatic brain injury in New Zealand: a population-based study. Lancet Neurol 12, 1: 53–64. [Google Scholar] [CrossRef] [PubMed]
- Fox, D. D., P. R. Lees-haley, K. Earnest, and S. Dolezalwood. 1995. Post-Concussive symptoms: Base rates and etiology in psychiatric patients. The Clinical neuropsychologist 9, 1: 89–92. [Google Scholar] [CrossRef]
- Frost, R. B., T. J. Farrer, M. Primosch, and D. W. Hedges. 2013. Prevalence of Traumatic Brain Injury in the General Adult Population: A Meta-Analysis. Neuroepidemiology 40, 3: 154–159. [Google Scholar] [CrossRef]
- Gardner, A. J., K. L. Quarrie, and G. L. Iverson. 2019. The Epidemiology of Sport-Related Concussion: What the Rehabilitation Clinician Needs to Know. Journal of Orthopaedic & Sports Physical Therapy 49, 11: 768–778. [Google Scholar] [CrossRef]
- Gessel, L. M., S. K. Fields, C. L. Collins, R. W. Dick, and R. D. Comstock. 2007. Concussions among United States high school and collegiate athletes. Journal of Athletic Training 42, 4: 495–503. [Google Scholar] [PubMed] [PubMed Central]
- Gioia, G. A., M. Collins, and P. K. Isquith. 2008. Improving identification and diagnosis of mild traumatic brain injury with evidence.
- psychometric support for the acute concussion evaluation. J Head Trauma Rehabil 23, 4: 230–242. [CrossRef]
- Giza, C. C., and D. A. Hovda. 2001. The Neurometabolic Cascade of Concussion. Journal of Athletic Training 36, 3: 228–235. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC155411/. [CrossRef]
- Giza, C. C., and D. A. Hovda. 2014. The new neurometabolic cascade of concussion. Neurosurgery 75 Suppl 4: S24–33. [Google Scholar] [CrossRef]
- Goldstein, F. C., H. S. Levin, W. P. Goldman, A. D. Kalechstein, A. N. Clark, and T. Kenehan-Altonen. 1999. Cognitive and Behavioral Sequelae of Closed Head Injury in Older Adults According to Their Significant Others. The Journal of Neuropsychiatry and Clinical Neurosciences 11, 1: 38–44. [Google Scholar] [CrossRef] [PubMed]
- Group, T. C. I. S. 2017. Sport concussion assessment tool-5th edition. British Journal of Sports Medicine 51, 11: 851. [Google Scholar] [CrossRef]
- Hollander, K., S. Kluge, F. Glöer, H. Riepenhof, A. Zech, and A. Junge. 2020. Epidemiology of injuries during the Wheelchair Basketball World Championships 2018: A prospective cohort study. Scandinavian Journal of Medicine & Science in Sports 30, 1: 199–207. [Google Scholar] [CrossRef]
- Holmin, S., M. Schalling, B. Höjeberg, A.-C. S. Nordqvist, A.-K. Skeftruna, and T. Mathiesen. 1997. Delayed cytokine expression in rat brain following experimental contusion. Journal of Neurosurgery 86, 3: 493–504. [Google Scholar] [CrossRef]
- Hon, K. L., A. K. C. Leung, and A. R. Torres. 2019. Concussion: A Global Perspective. Seminars in Pediatric Neurology 30: 117–127. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine,, and Council, N. R. 2014. The National Academies Collection: Reports funded by National Institutes of Health. In Sports-Related Concussions in Youth: Improving the Science, Changing the Culture. Edited by R. Graham, F. P. Rivara, M. A. Ford and C. M. Spicer. National Academies Press (US). [Google Scholar] [CrossRef]
- Iverson, G. L. 2006. Misdiagnosis of the persistent postconcussion syndrome in patients with depression. Archives of Clinical Neuropsychology 21, 4: 303–310. [Google Scholar] [CrossRef]
- Iverson, G. L., A. J. Gardner, D. P. Terry, J. L. Ponsford, A. K. Sills, D. K. Broshek, and G. S. Solomon. 2017. Predictors of clinical recovery from concussion: a systematic review. Br J Sports Med 51, 12: 941–948. [Google Scholar] [CrossRef]
- Iverson, G. L., and L. M. McCracken. 1997. ‘Postconcussive’ symptoms in persons with chronic pain. Brain Injury 11, 11: 783–790. [Google Scholar] [CrossRef]
- Kabadi, S. V., B. A. Stoica, D. J. Loane, T. Luo, and A. I. Faden. 2014. CR8, a Novel Inhibitor of CDK, Limits Microglial Activation.
- Astrocytosis, Neuronal Loss, and Neurologic Dysfunction after Experimental Traumatic Brain Injury. Journal of Cerebral Blood Flow & Metabolism 34, 3: 502–513. [CrossRef]
- Kara, S., H. Crosswell, K. Forch, A. Cavadino, J. McGeown, and M. Fulcher. 2020. Less Than Half of Patients Recover Within 2 Weeks of Injury After a Sports-Related Mild Traumatic Brain Injury: A 2-Year Prospective Study. Clin J Sport Med 30, 2: 96–101. [Google Scholar] [CrossRef] [PubMed]
- Karlsen, R. H., C. Einarsen, H. K. Moe, A. K. Håberg, A. Vik, T. Skandsen, and L. Eikenes. 2019. Diffusion kurtosis imaging in mild traumatic brain injury and postconcussional syndrome. Journal of neuroscience research 97, 5: 568–581. [Google Scholar] [CrossRef]
- Katayama, Y., D. P. Becker, T. Tamura, and D. A. Hovda. 1990. Massive increases in extracellular potassium and the indiscriminate release of glutamate following concussive brain injury. J Neurosurg 73, 6: 889–900. [Google Scholar] [CrossRef] [PubMed]
- Kenzie, E. S., E. L. Parks, E. D. Bigler, D. W. Wright, M. M. Lim, J. C. Chesnutt, G. W. J. Hawryluk, W. Gordon, and W. Wakeland. 2018. The dynamics of concussion: Mapping pathophysiology, persistence, and recovery with causal-loop diagramming. Frontiers in neurology 9: 203–203. [Google Scholar] [CrossRef]
- King, D., C. Gissane, M. Brughelli, P. Hume, and J. Harawira. 2014. Sport-related concussion in New Zealand: A Review of 10 Years of Accident Compensation Corporation Moderate to Severe Claims and Costs. J Sci Med Sport 17, 3: 250–255. [Google Scholar] [CrossRef]
- Kontos, A. P., R. J. Elbin, 3rd, T. Covassin, and E. Larson. 2010. Exploring differences in computerized neurocognitive concussion testing between African American and White athletes. Arch Clin Neuropsychol 25, 8: 734–744. [Google Scholar] [CrossRef] [PubMed]
- La Fountaine, M. F., K. S. Heffernan, J. D. Gossett, W. A. Bauman, and R. E. De Meersman. 2009. Transient suppression of heart rate complexity in concussed athletes. Auton Neurosci 148, 1–2: 101–103. [Google Scholar] [CrossRef]
- Langdon, S., M. Königs, E. A. M. C. Adang, E. Goedhart, and J. Oosterlaan. 2020. Subtypes of Sport-Related Concussion: a Systematic Review and Meta-cluster Analysis. Sports Medicine 50, 10: 1829–1842. [Google Scholar] [CrossRef]
- Langlois, J. A., W. Rutland-Brown, and K. E. Thomas. 2005. The incidence of traumatic brain injury among children in the United States: differences by race. J Head Trauma Rehabil 20, 3: 229–238. [Google Scholar] [CrossRef]
- Leddy, J. J., H. Sandhu, V. Sodhi, J. G. Baker, and B. Willer. 2012. Rehabilitation of concussion and post-concussion syndrome. Sports Health 4, 2: 147–154. [Google Scholar] [CrossRef]
- Lees-Haley, P. R., and R. S. Brown. 1993. Neuropsychological complaint base rates of 170 personal injury claimants. Arch Clin Neuropsychol 8, 3: 203–209. [Google Scholar] [CrossRef]
- Lefevre-Dognin, C., M. Cogné, V. Perdrieau, A. Granger, C. Heslot, and P. Azouvi. 2021. Definition and epidemiology of mild traumatic brain injury. Neurochirurgie 67, 3: 218–221. [Google Scholar] [CrossRef]
- Leibson, C. L., A. W. Brown, J. E. Ransom, N. N. Diehl, P. K. Perkins, J. Mandrekar, and J. F. Malec. 2011. Incidence of traumatic brain injury across the full disease spectrum: a populationbased medical record review study. Epidemiology 22, 6: 836–844. [Google Scholar] [CrossRef] [PubMed]
- Lincoln, A. E., S. V. Caswell, J. L. Almquist, R. E. Dunn, J. B. Norris, and R. Y. Hinton. 2011. Trends in concussion incidence in high school sports: a prospective 11-year study. The American journal of sports medicine 39, 5: 958–963. [Google Scholar] [CrossRef] [PubMed]
- Lishman, W. A. 1988. Physiogenesis and psychogenesis in the ’post-concussional syndrome’. Br J Psychiatry 153: 460–469. [Google Scholar] [CrossRef]
- Lumba-Brown, A., M. Teramoto, O. J. Bloom, D. Brody, J. Chesnutt, J. R. Clugston, M. Collins, G. Gioia, A. Kontos, A. Lal, A. Sills, and J. Ghajar. 2019. Concussion Guidelines Step 2: Evidence for Subtype Classification. Neurosurgery. [Google Scholar] [CrossRef]
- Lumba-Brown, A., K. O. Yeates, K. Sarmiento, M. J. Breiding, T. M. Haegerich, G. A. Gioia, M. Turner, E. C. Benzel, S. J. Suskauer, C. C. Giza, M. Joseph, C. Broomand, B. Weissman, W. Gordon, D. W. Wright, R. S. Moser, K. McAvoy, L. Ewing-Cobbs, A.-C. Duhaime, M. Putukian, and et al. 2018. Centers for Disease Control and Prevention Guideline on the Diagnosis and Management of Mild Traumatic Brain Injury Among Children. JAMA Pediatrics 172, 11: e182853–e182853. [Google Scholar] [CrossRef] [PubMed]
- Maas, A. I. R., D. K. Menon, P. D. Adelson, N. Andelic, M. J. Bell, A. Belli, P. Bragge, A. Brazinova, A. Büki, R. M. Chesnut, G. Citerio, M. Coburn, D. J. Cooper, A. T. Crowder, E. Czeiter, M. Czosnyka, R. Diaz-Arrastia, J. P. Dreier, A. C. Duhaime, A. Ercole, and et al. 2017. Traumatic brain injury: integrated approaches to improve prevention, clinical care, and research. Lancet Neurol 16, 12: 987–1048. [Google Scholar] [CrossRef]
- Marar, M., N. M. McIlvain, S. K. Fields, and R. D. Comstock. 2012. Epidemiology of concussions among United States high school athletes in 20 sports. The American journal of sports medicine 40, 4: 747–755. [Google Scholar] [CrossRef]
- Maruta, J., M. Suh, S. N. Niogi, P. Mukherjee, and J. Ghajar. 2010. Visual tracking synchronization as a metric for concussion screening. J Head Trauma Rehabil 25, 4: 293–305. [Google Scholar] [CrossRef]
- Mauritz, W., A. Brazinova, M. Majdan, and J. Leitgeb. 2014. Epidemiology of traumatic brain injury in Austria. Wien Klin Wochenschr 126, 1–2: 42–52. [Google Scholar] [CrossRef]
- Mayer, A. R., D. K. Quinn, and C. L. Master. 2017. The spectrum of mild traumatic brain injury: A review. Neurology 89, 6: 623–632. [Google Scholar] [CrossRef] [PubMed]
- McCauley, S. R., C. Boake, C. Pedroza, S. A. Brown, H. S. Levin, H. S. Goodman, and S. G. Merritt. 2005. Postconcussional disorder: Are the DSM-IV criteria an improvement over the ICD10? J Nerv Ment Dis 193, 8: 540–550. [Google Scholar] [CrossRef]
- McCrory, P., W. H. Meeuwisse, M. Aubry, B. Cantu, J. Dvořák, R. J. Echemendia, L. Engebretsen, K. Johnston, J. S. Kutcher, M. Raftery, A. Sills, B. W. Benson, G. A. Davis, R. G. Ellenbogen, K. Guskiewicz, S. A. Herring, G. L. Iverson,, B. D. Jordan, J. Kissick, M. McCrea, A. S. McIntosh, D. Maddocks, M. Makdissi, L. Purcell, M. Putukian, K. Schneider, C. H. Tator, and M. Turner. 2013. Consensus statement on concussion in sport: the 4th International Conference on Concussion in Sport held in Zurich, November 2012. British Journal of Sports Medicine 47, 5: 250. [Google Scholar] [CrossRef] [PubMed]
- Meehan, W. P., 3rd, R. C. Mannix, M. J. O’Brien, and M. W. Collins. 2013. The prevalence of undiagnosed concussions in athletes. Clin J Sport Med 23, 5: 339–342. [Google Scholar] [CrossRef] [PubMed]
- Metting, Z., J. M. Spikman, L. A. Rödiger, and J. van der Naalt. 2014. Cerebral perfusion and neuropsychological follow up in mild traumatic brain injury: Acute versus chronic disturbances? Brain and Cognition 86: 24–31. [Google Scholar] [CrossRef]
- Mittl, R. L., R. I. Grossman, J. F. Hiehle, R. W. Hurst, D. R. Kauder, T. A. Gennarelli, and G. W. Alburger. 1994. Prevalence of MR evidence of diffuse axonal injury in patients with mild head injury and normal head CT findings. American Journal of Neuroradiology 15, 8: 1583. Available online: http://www.ajnr.org/content/15/8/1583.abstract.
- Moreland, B, R. K., and A. Henry. 2020. Trends in Nonfatal Falls and Fall-Related Injuries Among Adults Aged ≥65 Years—United States, 2012–2018. MMWR Morb Mortal Wkly Rep 2020 69: 875881. [Google Scholar] [CrossRef]
- Preiss-Farzanegan, S. J., B. Chapman, T. M. Wong, J. Wu, and J. J. Bazarian. 2009. The relationship between gender and postconcussion symptoms after sport-related mild traumatic brain injury. Pm r 1, 3: 245–253. [Google Scholar] [CrossRef]
- Prevention, C. F. D. C. a. 2019. Surveillance report of traumatic brain injury-related emergency department visits, hospitalizations, and deaths, United States, 2014. Retrieved September 3 from https://stacks.cdc.gov/view/cdc/78062.
- Price, L. W. C., and C Grant. 2016. Blood-Brain Barrier Pathophysiology following Traumatic Brain Injury. Edited by G. G. Laskowitz D. In Translational Research in Traumatic Brain Injury. CRC Press/Taylor and Francis Group: https://www.ncbi.nlm.nih.gov/books/NBK326726/.
- Prins, M. L., D. Alexander, C. C. Giza, and D. A. Hovda. 2013. Repeated mild traumatic brain injury: mechanisms of cerebral vulnerability. J Neurotrauma 30, 1: 30–38. [Google Scholar] [CrossRef]
- Prins, M. L., A. Hales, M. Reger, C. C. Giza, and D. A. Hovda. 2010. Repeat traumatic brain injury in the juvenile rat is associated with increased axonal injury and cognitive impairments. Dev Neurosci 32, 5–6: 510–518. [Google Scholar] [CrossRef] [PubMed]
- Rapoport, M. J., and A. Feinstein. 2000. Outcome following traumatic brain injury in the elderly: a critical review. Brain Injury 14, 8: 749–761. [Google Scholar] [CrossRef]
- Reeves, T. M., T. L. Smith, J. C. Williamson, and L. L. Phillips. 2012. Unmyelinated Axons Show Selective Rostrocaudal Pathology in the Corpus Callosum After Traumatic Brain Injury. Journal of Neuropathology & Experimental Neurology 71, 3: 198–210. [Google Scholar] [CrossRef]
- Romeu-Mejia, R., C. C. Giza, and J. T. Goldman. 2019. Concussion Pathophysiology and Injury Biomechanics. Current Reviews in Musculoskeletal Medicine. [Google Scholar] [CrossRef]
- Rugg-Gunn, F. J., M. R. Symms, G. J. Barker, R. Greenwood, and J. S. Duncan. 2001. Diffusion imaging shows abnormalities after blunt head trauma when conventional magnetic resonance imaging is normal. Journal of Neurology, Neurosurgery & Psychiatry 70, 4: 530. [Google Scholar] [CrossRef]
- Santhanam, P., T. Teslovich, S. H. Wilson, P. H. Yeh, T. R. Oakes, and L. K. Weaver. 2019. Decreases in White Matter Integrity of Ventro-Limbic Pathway Linked to Post-Traumatic Stress Disorder in Mild Traumatic Brain Injury. J Neurotrauma 36, 7: 1093–1098. [Google Scholar] [CrossRef]
- Selassie, A. W., D. A. Wilson, E. E. Pickelsimer, D. C. Voronca, N. R. Williams, and J. C. Edwards. 2013. Incidence of sport-related traumatic brain injury and risk factors of severity: a population-based epidemiologic study. Ann Epidemiol 23, 12: 750–756. [Google Scholar] [CrossRef]
- Sharp, D. J., and P. O. Jenkins. 2015. Concussion is confusing us all. Practical Neurology 15, 3: 172. [Google Scholar] [CrossRef] [PubMed]
- Slobounov, S., E. Slobounov, W. Sebastianelli, C. Cao, and K. Newell. 2007. Differential Rate of Recovery In Athletes After First and Second Concussion Episodes. Neurosurgery 61, 2: 338–344. [Google Scholar] [CrossRef]
- Sye, G., S. J. Sullivan, and P. McCrory. 2006. High school rugby players’ understanding of concussion and return to play guidelines. British Journal of Sports Medicine 40, 12: 1003–1005. [Google Scholar] [CrossRef]
- Taghdiri, F., J. Chung, S. Irwin, N. Multani, A. Tarazi, A. Ebraheem, M. Khodadadi, R. Goswami, R. Wennberg, D. Mikulis, R. Green, K. Davis, C. Tator, M. Eizenman, and M. C. Tartaglia. 2018. Decreased Number of Self-Paced Saccades in Post-Concussion Syndrome Associated with Higher Symptom Burden and Reduced White Matter Integrity. J Neurotrauma 35, 5: 719–729. [Google Scholar] [CrossRef] [PubMed]
- Theadom, A., S. Mahon, P. Hume, N. Starkey, S. Barker-Collo, K. Jones, M. Majdan, and V. L. Feigin. 2020. Incidence of Sports-Related Traumatic Brain Injury of All Severities: A Systematic Review. Neuroepidemiology. [Google Scholar] [CrossRef] [PubMed]
- Theadom, A., V. Parag, T. Dowell, K. McPherson, N. Starkey, S. Barker-Collo, K. Jones, S. Ameratunga, V. L. Feigin, and B. R. Group. 2016. Persistent problems 1 year after mild traumatic brain injury: a longitudinal population study in New Zealand. Br J Gen Pract 66, 642: e16–23. [Google Scholar] [CrossRef]
- Theadom, A., N. J. Starkey, T. Dowell, P. A. Hume, M. Kahan, K. McPherson, V. Feigin, and B. R. Group. 2014. Sports-related brain injury in the general population: an epidemiological study. J Sci Med Sport 17, 6: 591–596. [Google Scholar] [CrossRef] [PubMed]
- Tierney, R. T., M. R. Sitler, C. B. Swanik, K. A. Swanik, M. Higgins, and J. Torg. 2005. Gender differences in head-neck segment dynamic stabilization during head acceleration. Med Sci Sports Exerc 37, 2: 272–279. [Google Scholar] [CrossRef]
- Tyler, C. W., L. T. Likova, K. N. Mineff, and S. C. Nicholas. 2015. Deficits in the Activation of Human Oculomotor Nuclei in Chronic Traumatic Brain Injury. Frontiers in neurology 6: 173–173. [Google Scholar] [CrossRef]
- Vagnozzi, R., S. Signoretti, B. Tavazzi, R. Floris, A. Ludovici, S. Marziali, G. Tarascio, A. Amorini, V. Di Pietro, R. Delfini, and G. Lazzarino. 2008. Temporal window of metabolic brain vulnerability to concussion: A pilot 1H-magnetic resonance spectroscopic study in concussed athletes-Part III. Neurosurgery discussion 1295. 62: 1286–1295. [Google Scholar] [CrossRef]
- Ventura, R. E., J. M. Jancuska, L. J. Balcer, and S. L. Galetta. 2015. Diagnostic tests for concussion: is vision part of the puzzle? Journal of neuroophthalmology: the official journal of the North American Neuro-Ophthalmology Society 35, 1: 73–81. [Google Scholar] [CrossRef]
- Wallace, J. S., and R. C. Mannix. 2021. Racial Disparities in Diagnosis of Concussion and Minor Head Trauma and Mechanism of Injury in Pediatric Patients Visiting the Emergency Department. J Pediatr 233: 249–254.e241. [Google Scholar] [CrossRef]
- White, E. R., C. Pinar, C. A. Bostrom, A. Meconi, and B. R. Christie. 2017. Mild Traumatic Brain Injury Produces Long-Lasting Deficits in Synaptic Plasticity in the Female Juvenile Hippocampus. J Neurotrauma 34, 5: 1111–1123. [Google Scholar] [CrossRef]
- World Health Organization, and W. 1993. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines.
- Yeung, D., J. L. Manias, D. J. Stewart, and S. Nag. 2008. Decreased junctional adhesion molecule-A expression during blood-brain barrier breakdown. Acta Neuropathol 115, 6: 635–642. [Google Scholar] [CrossRef] [PubMed]
- Zhang, A. L., D. C. Sing, C. M. Rugg, B. T. Feeley, and C. Senter. 2016. The Rise of Concussions in the Adolescent Population. Orthopaedic journal of sports medicine 4, 8: 2325967116662458. [Google Scholar] [CrossRef] [PubMed]
| Subtype | Symptoms/ Risk Factors | Prevalence |
| Cognitive | Impairment in attention, reaction time, memory (storage, retrieval, and working), processing speed, thought organization, and behaviour. | 32% in a paediatric cohort and 40% in adults |
| Headache/ Migraine | Patients with a history of chronic headaches or migraine were considered high risk of exacerbation following mTBI | 52% in a paediatric cohort and 38% in adults. |
| Vestibular | Impairment of movement, proprioception, and balance, resulting in dizziness, ‘fogginess’, nausea, vertigo, and ‘lightheadedness’. A vestibuloocular subtype consists of abnormal vestibulo-ocular reflex, visual motion sensitivity, gait impairment, and balance issues. | 50% in a paediatric cohort and 25% in adults. |
| Anxiety/ Mood | Nervousness, experienced heightened emotions, ruminating, feeling overwhelmed, depression, hopelessness, fatigue, and anger/ irritability. | 30% in a paediatric cohort and 23% in adults. |
| Ocular motor | Asthenopia (‘eye strain’), ‘tired eyes’, difficulty with near or distance (from impaired vergence and accommodation), photophobia (sensitivity to light), frontal headaches, blurred vision, pressure around the eyes, and vision-related nausea. These issues arise from difficulties in obtaining and processing visual stimuli from impaired eye movements (saccades and smooth pursuits; see section below). | 34% in a paediatric cohort and 34% in adults (although this showed a large range). |
Copyright © 2022. This article is licensed under a Creative Commons Attribution 4.0 International License.
Share and Cite
McDonald, M.A.; Holdsworth, S.J.; Danesh-Meyer, H.V. Eye Movements in Mild Traumatic Brain Injury: Clinical Challenges. J. Eye Mov. Res. 2022, 15, 1-15. https://doi.org/10.16910/jemr.15.2.3
McDonald MA, Holdsworth SJ, Danesh-Meyer HV. Eye Movements in Mild Traumatic Brain Injury: Clinical Challenges. Journal of Eye Movement Research. 2022; 15(2):1-15. https://doi.org/10.16910/jemr.15.2.3
Chicago/Turabian StyleMcDonald, Matthew A., Samantha J. Holdsworth, and Helen V. Danesh-Meyer. 2022. "Eye Movements in Mild Traumatic Brain Injury: Clinical Challenges" Journal of Eye Movement Research 15, no. 2: 1-15. https://doi.org/10.16910/jemr.15.2.3
APA StyleMcDonald, M. A., Holdsworth, S. J., & Danesh-Meyer, H. V. (2022). Eye Movements in Mild Traumatic Brain Injury: Clinical Challenges. Journal of Eye Movement Research, 15(2), 1-15. https://doi.org/10.16910/jemr.15.2.3



