Fractional-Order Control Strategy for Anesthesia–Hemodynamic Stabilization in Patients Undergoing Surgical Procedures
Abstract
:1. Introduction
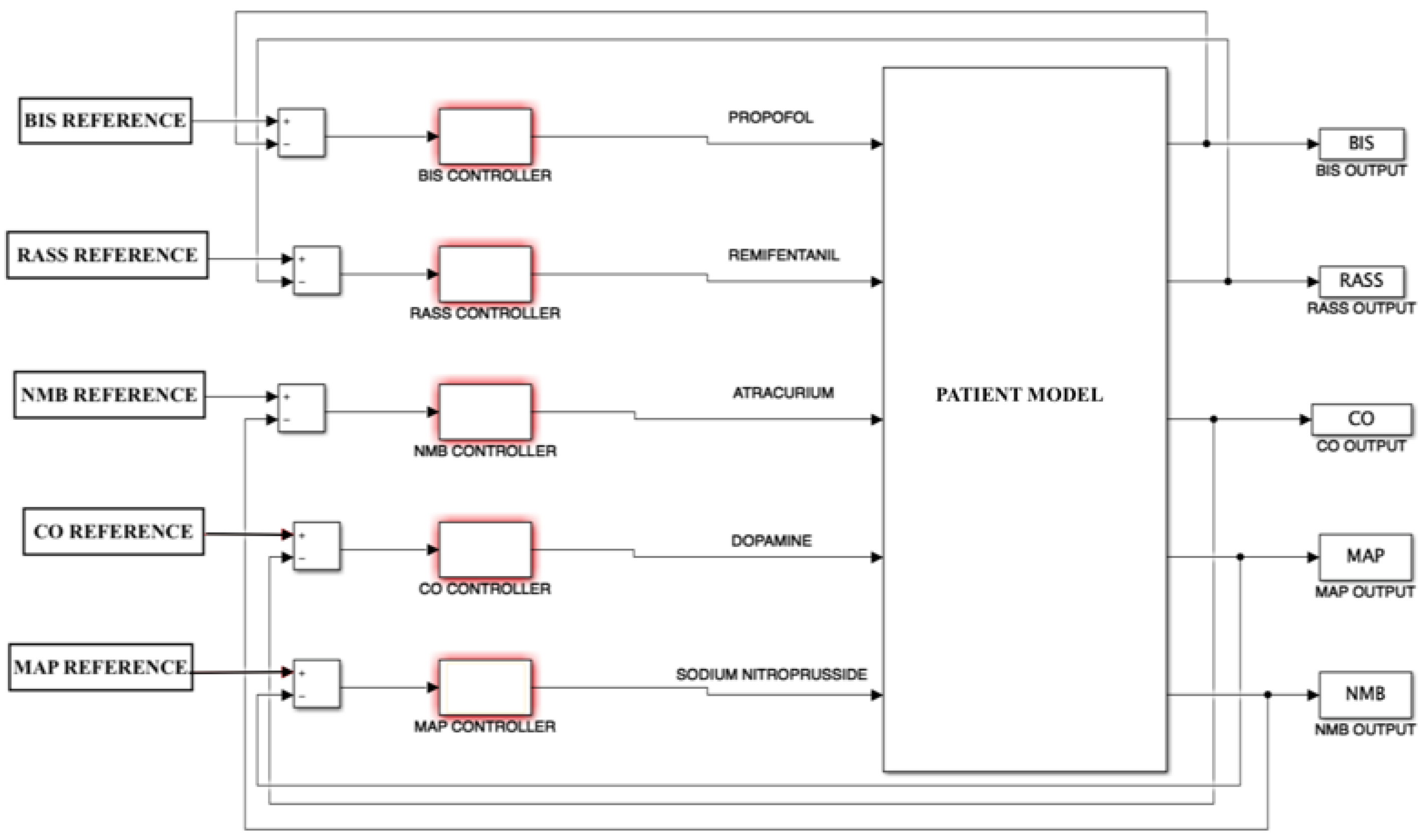
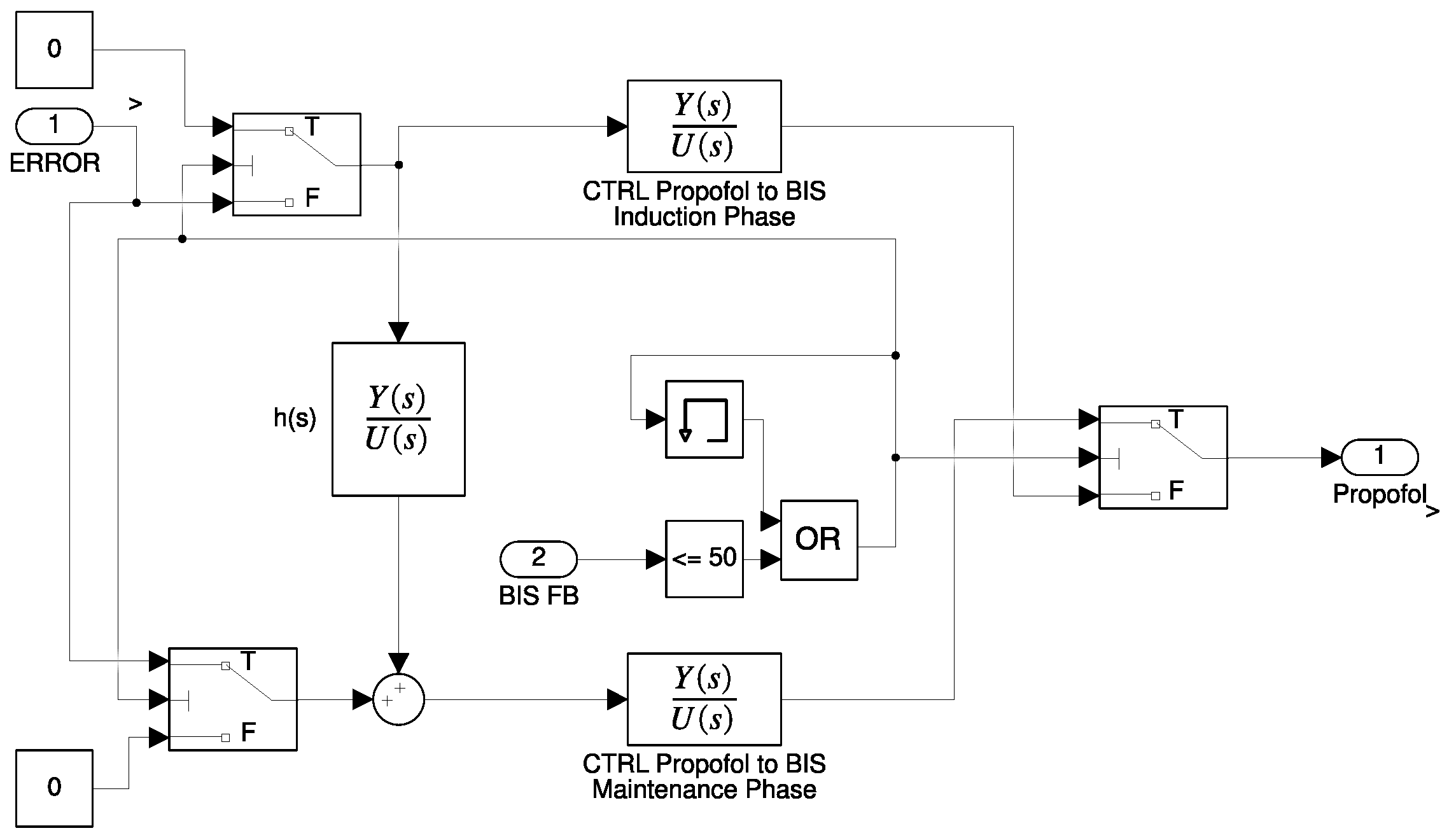
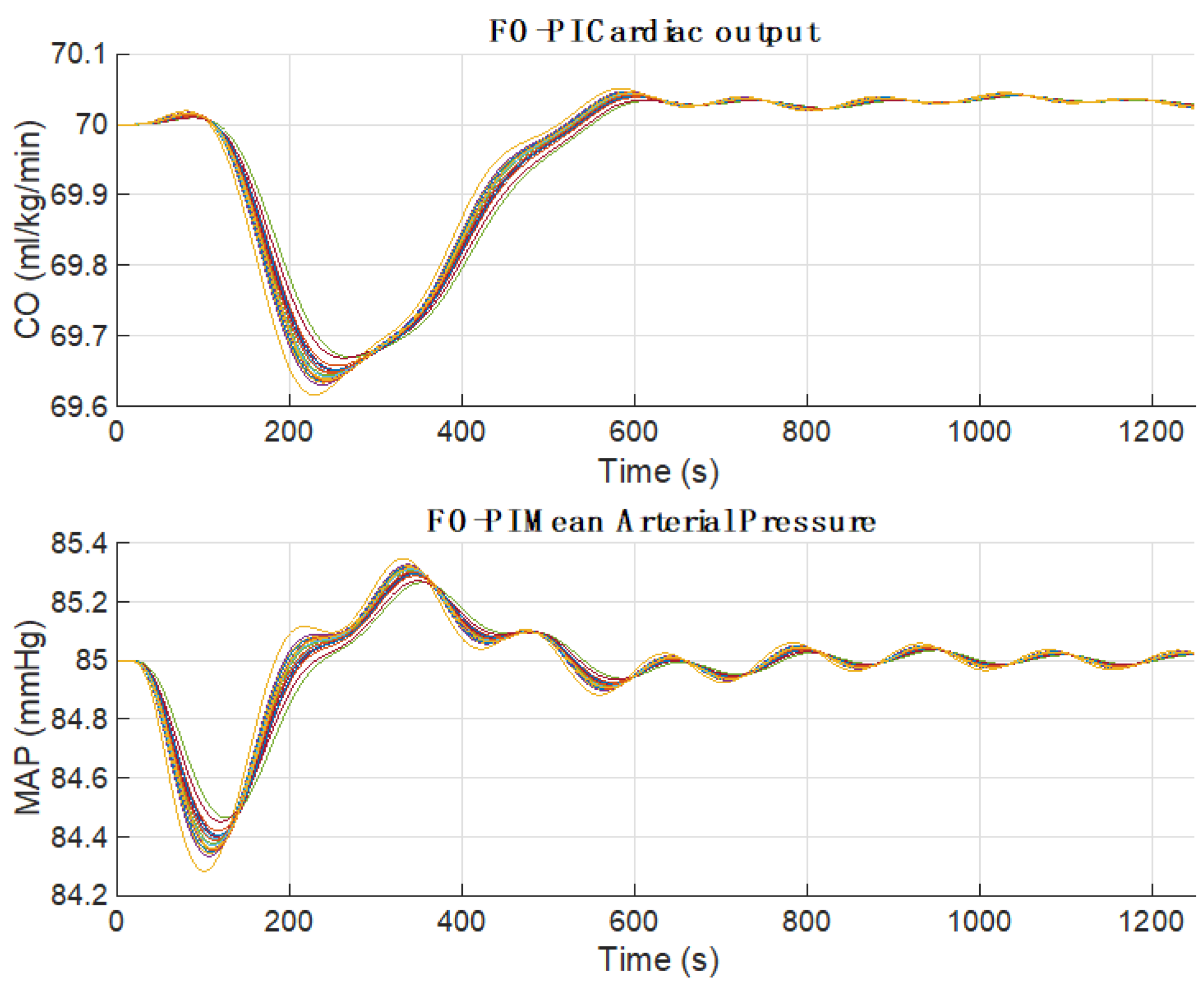
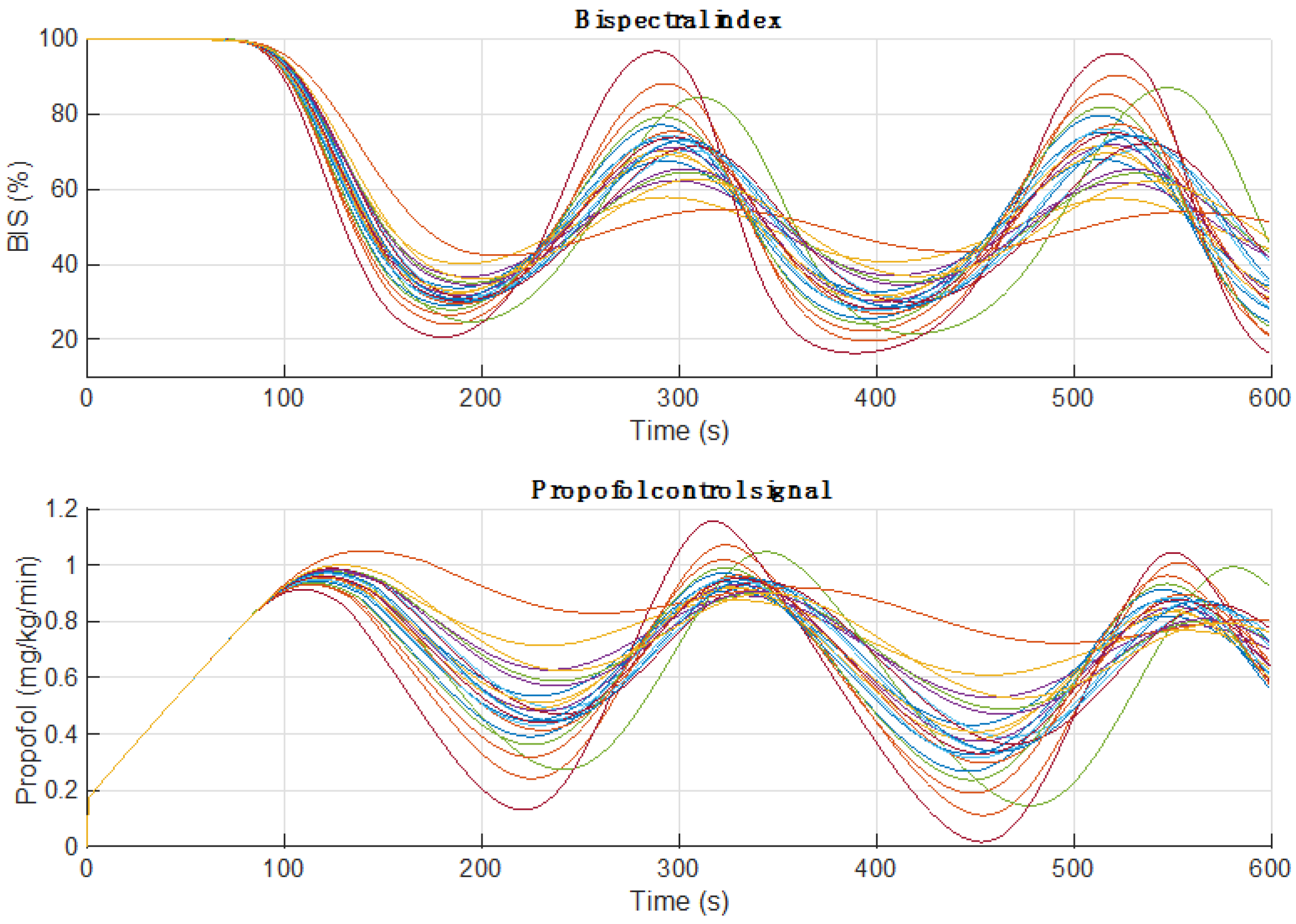
2. A Dedicated Double-FOPID Control System with Bumpless Transfer for Controlling the Depth of Hypnosis
- (a)
- The intra- and inter-patient variability must be minimized;
- (b)
- The time to target must respect the four-minute mark;
- (c)
- Excessive undershoot and significant oscillations must be avoided;
- (d)
- Disturbances acting on the depth of anesthesia such as nociceptor stimuli must be rejected, keeping BIS in the range of 40% to 60%.
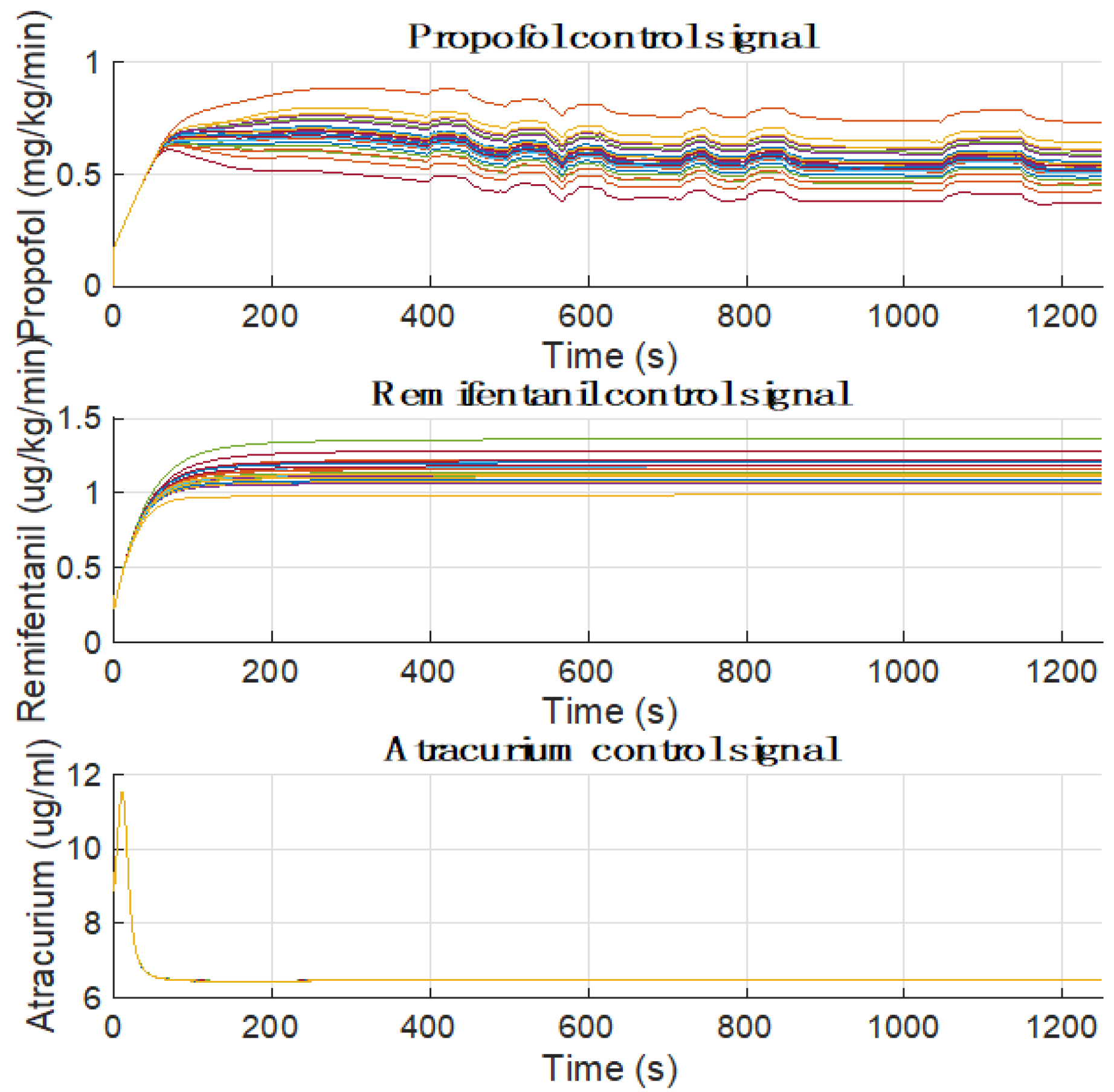
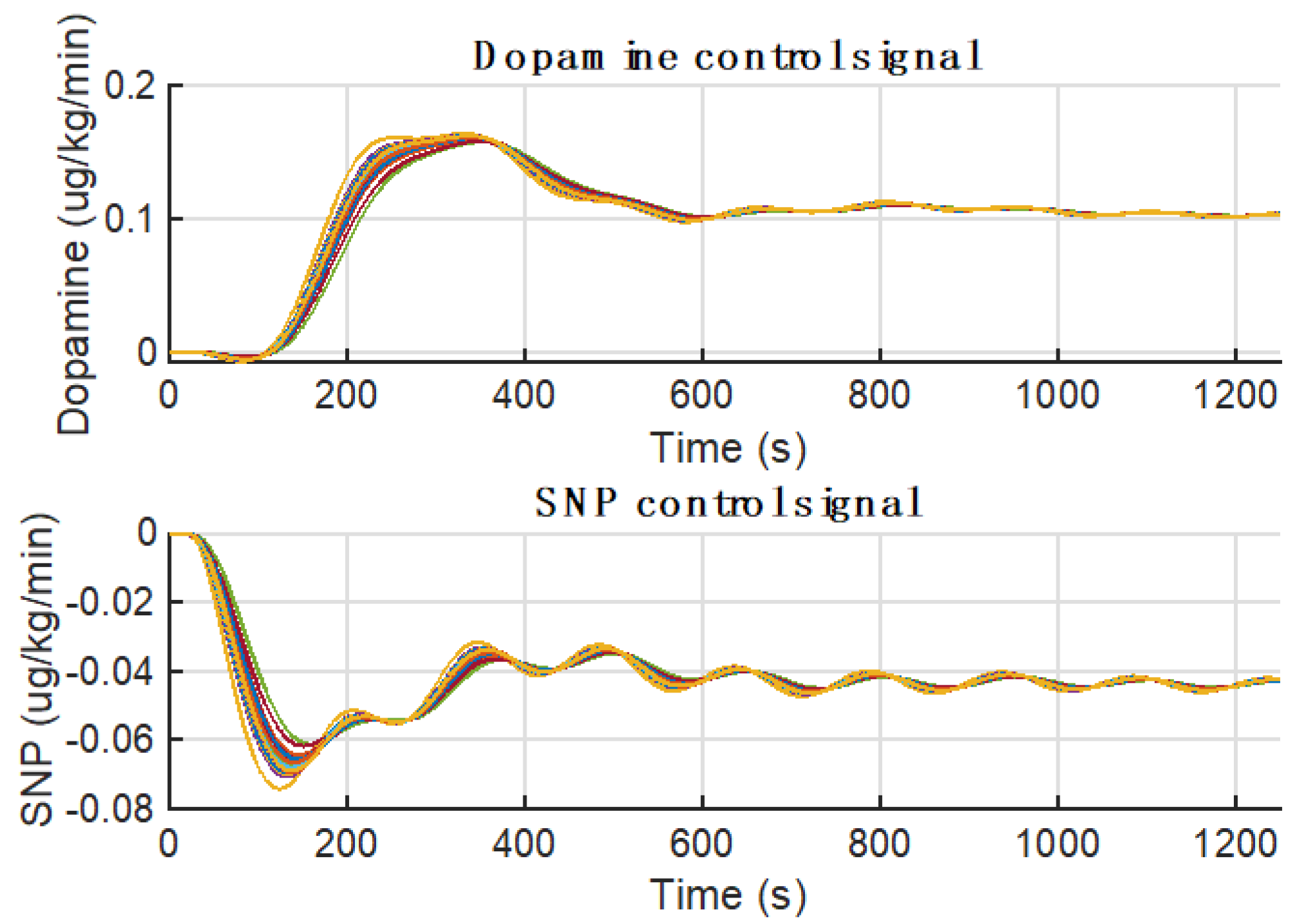
3. Results
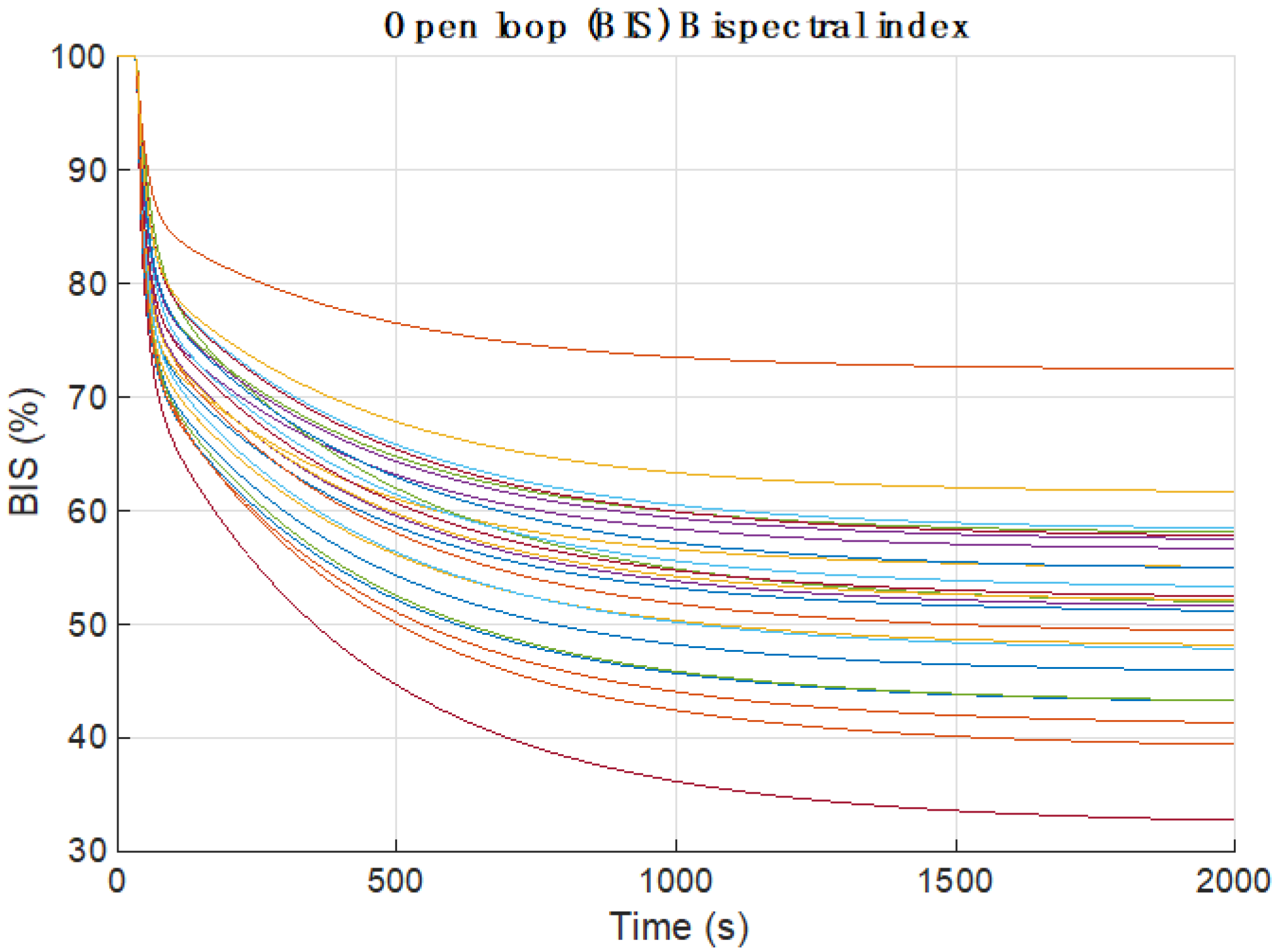
3.1. Design of the FOPIDs for the Induction Phase
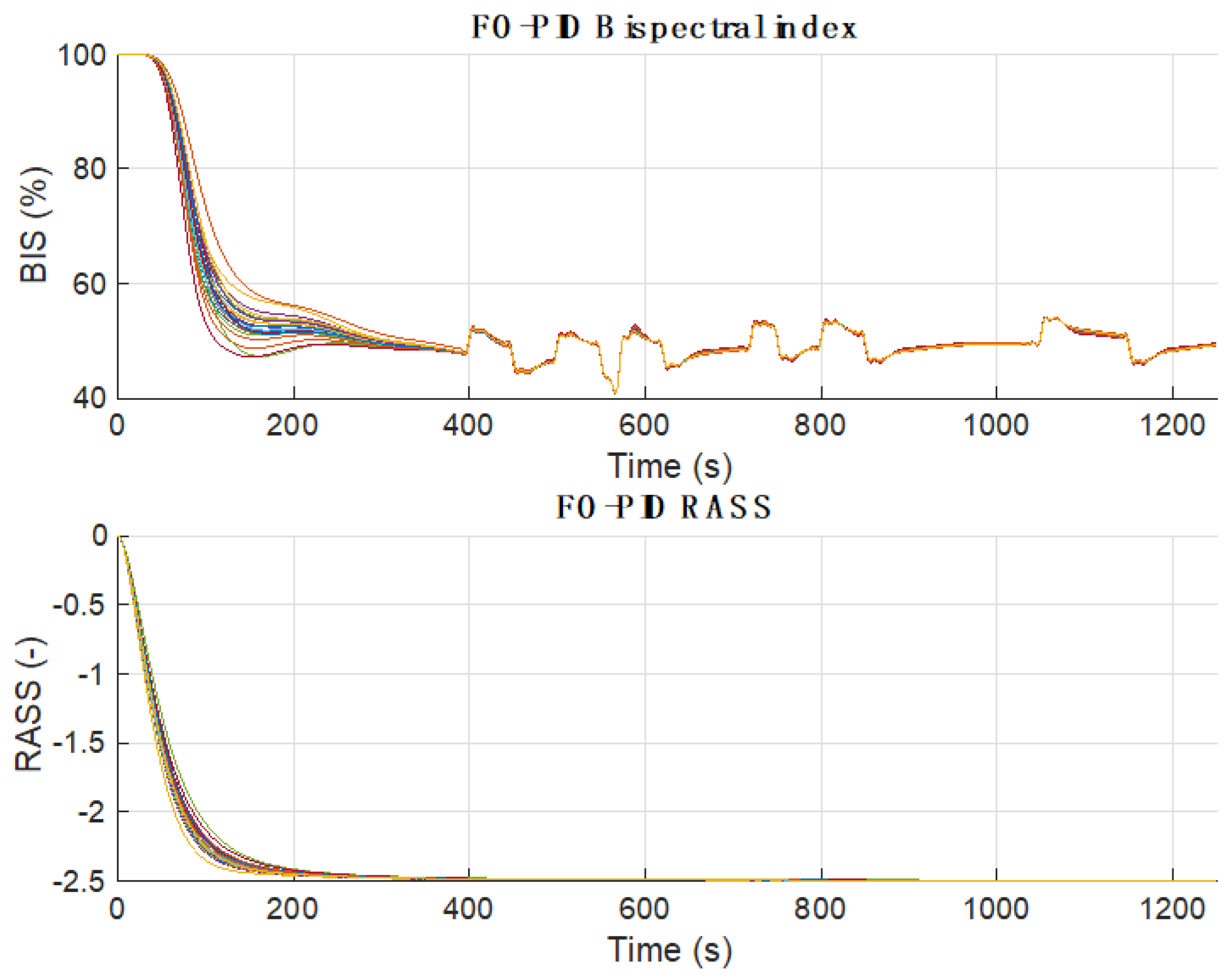
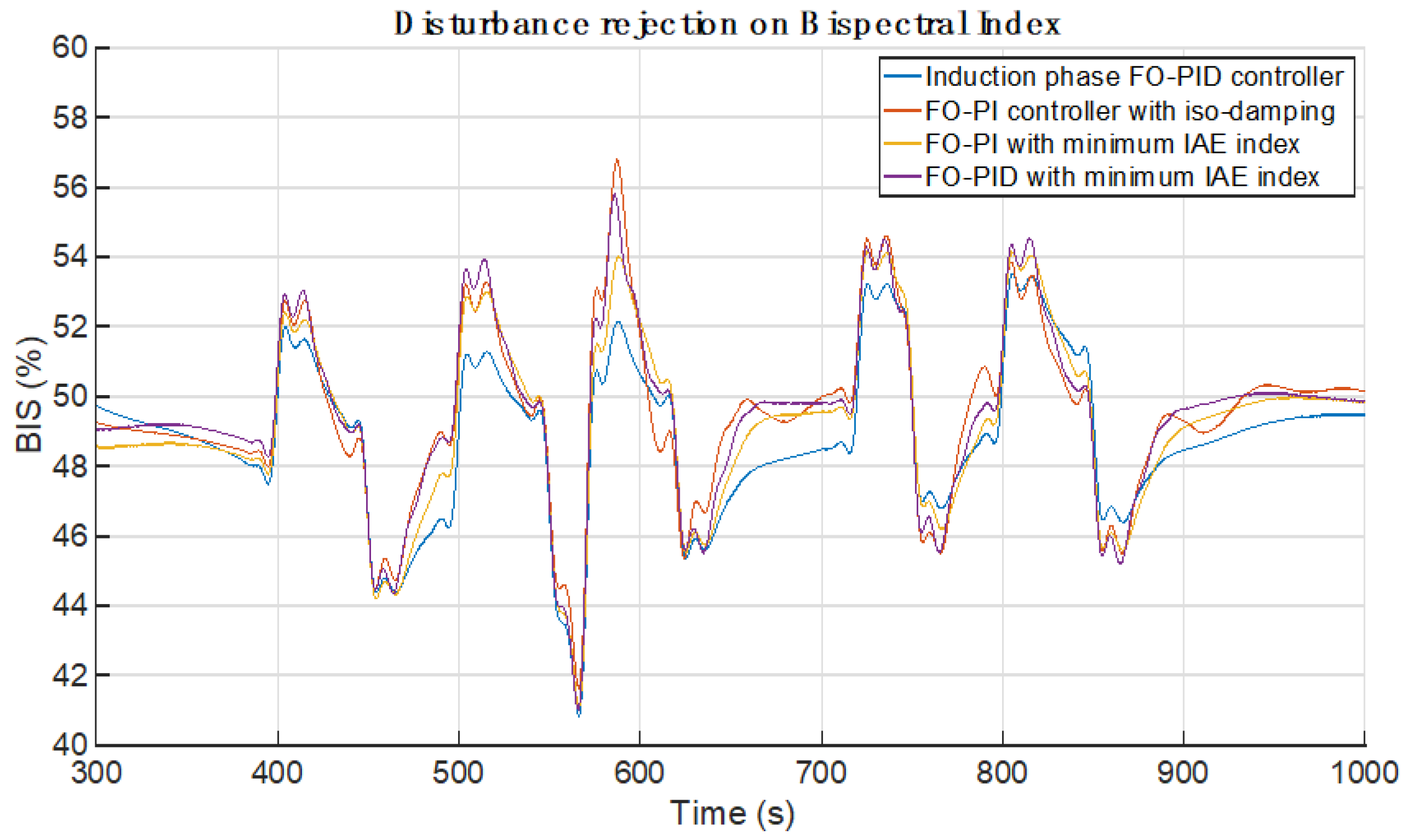
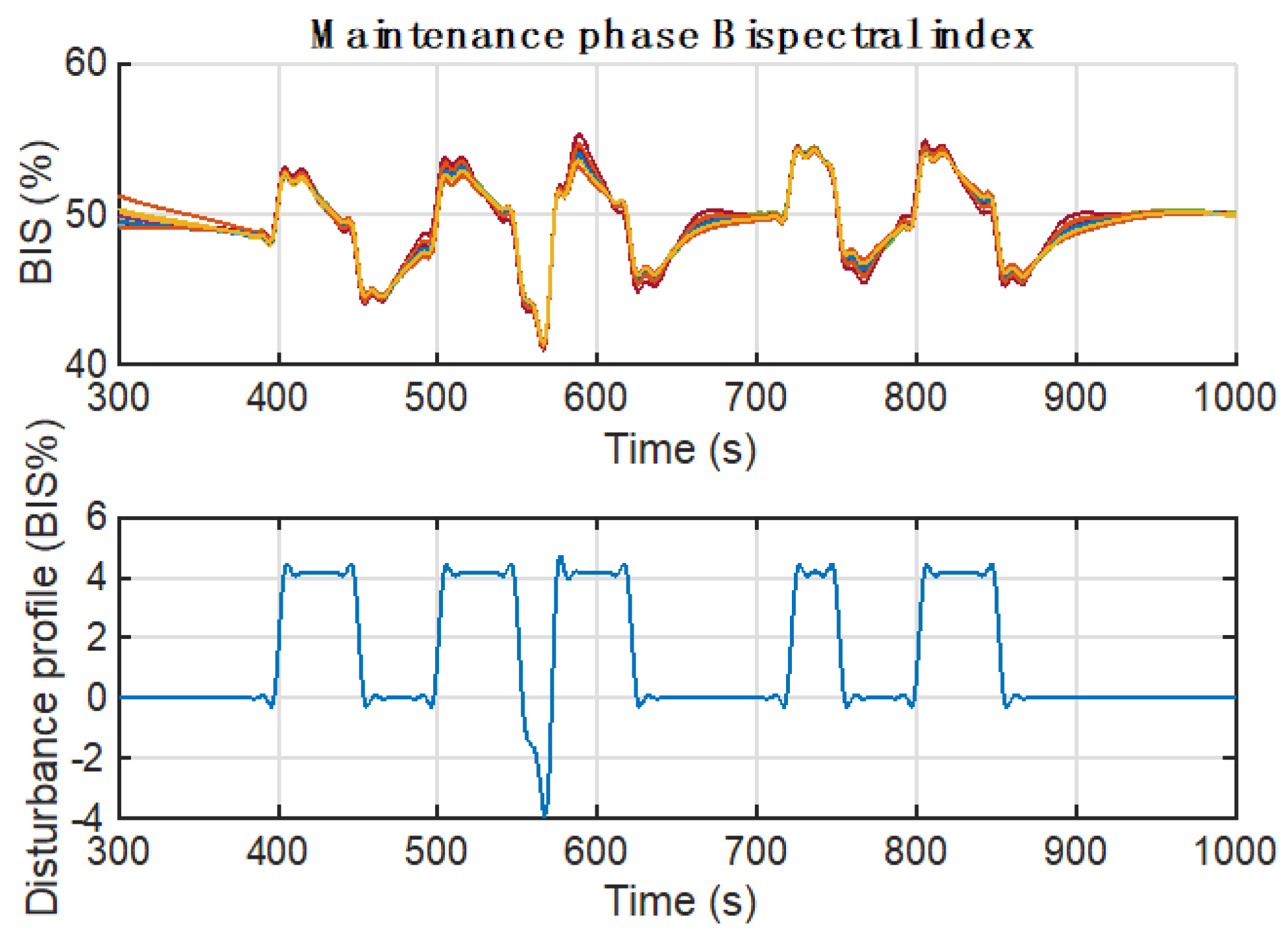
3.2. Design of the FOPIDs for the Maintenance Phase
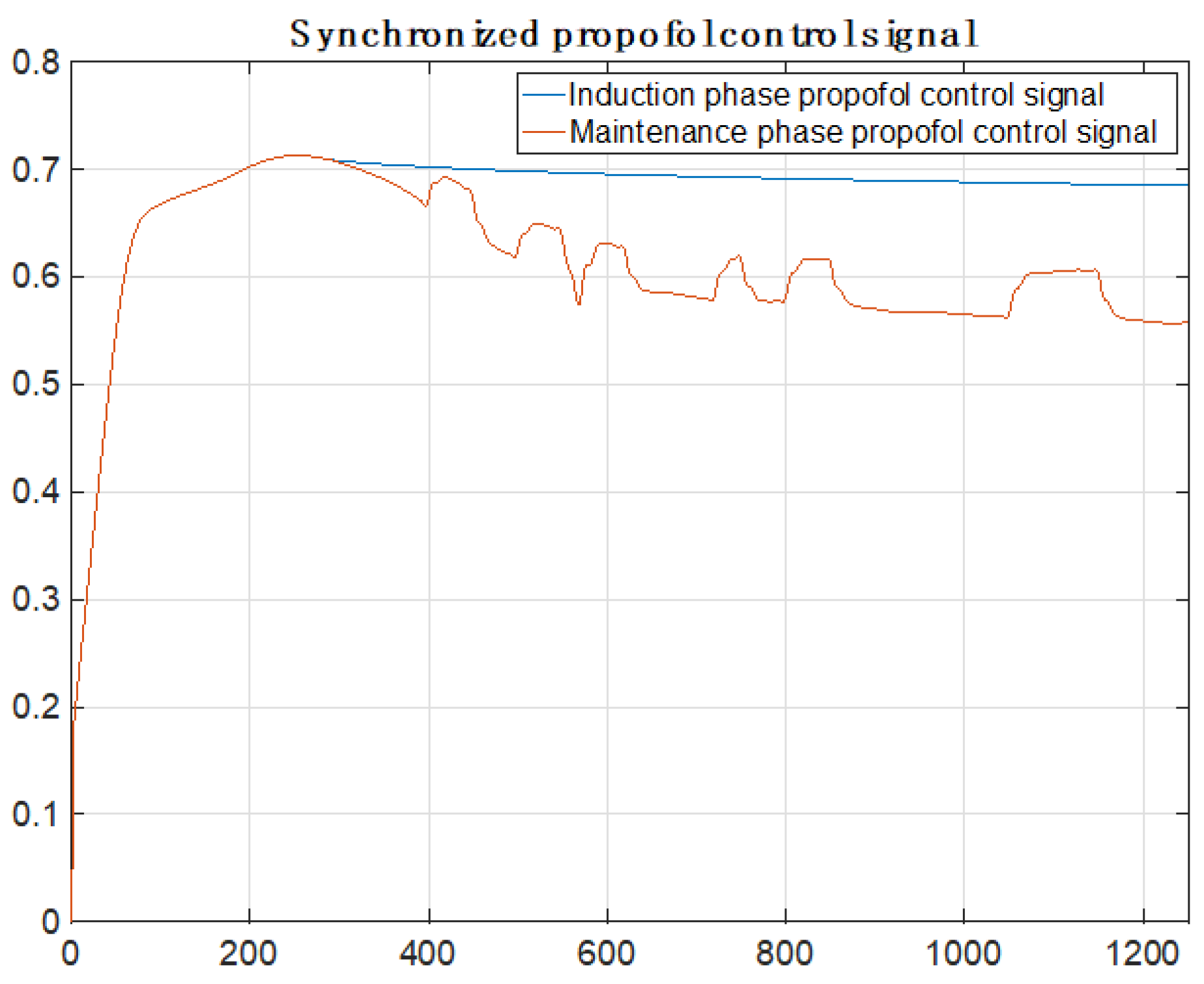
3.3. Design of the Synchronization Function for Bumpless Transfer between the Induction- and Maintenance-Phase Controllers
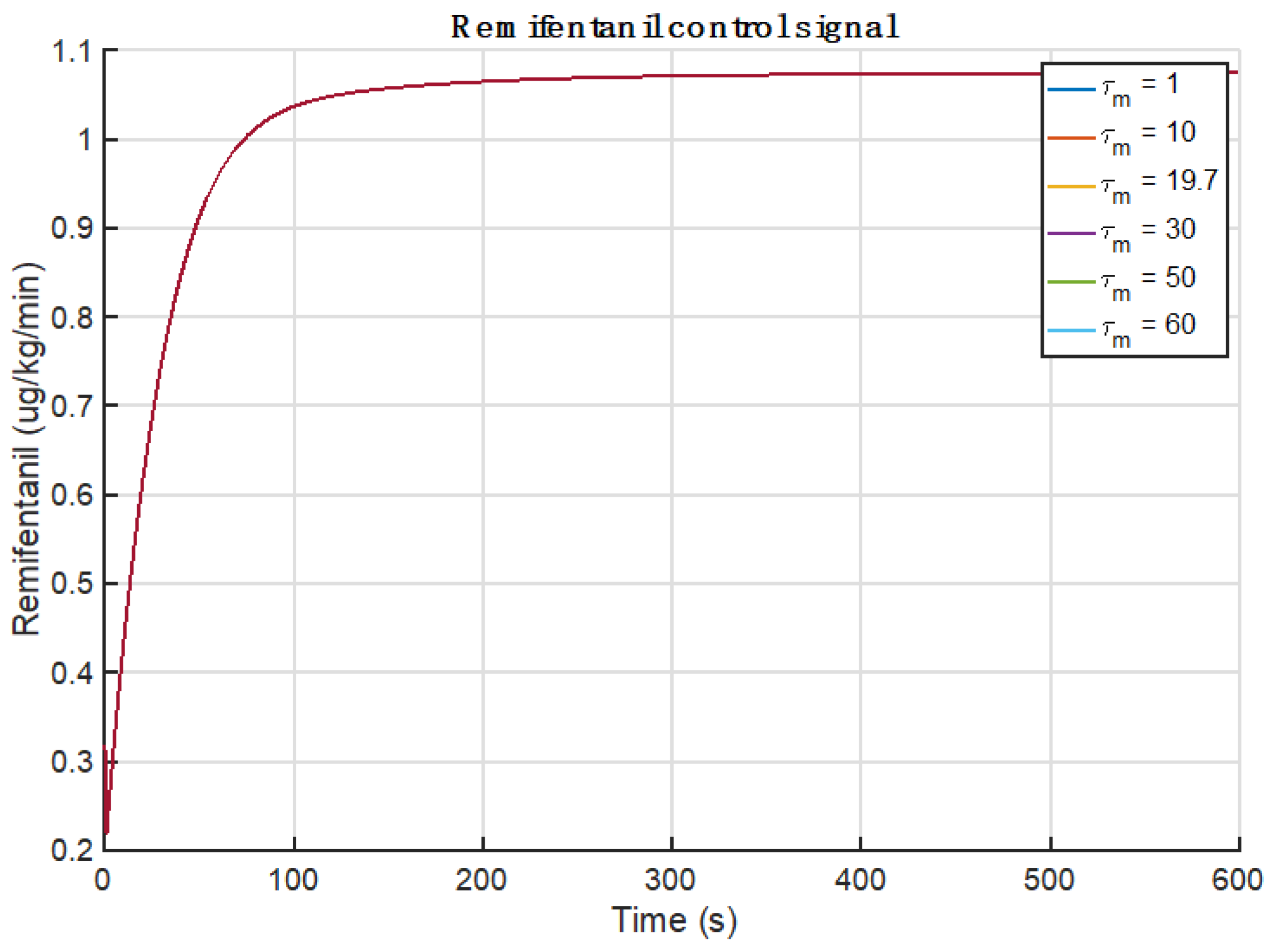
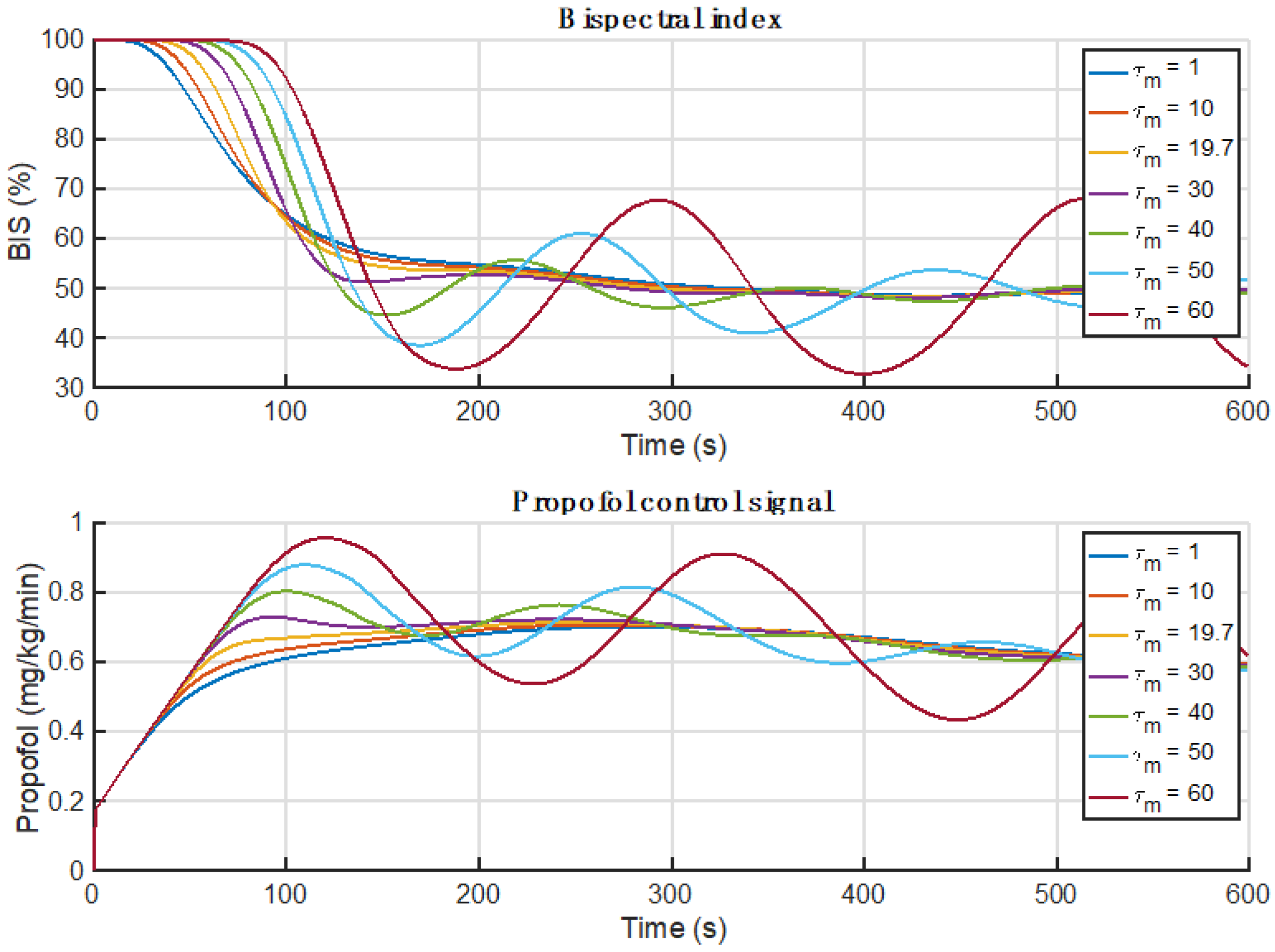
4. Overdose Analysis and Controller Validation for Variable Measurement Delays
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Machado, J.T. Fractional Calculus: Application in Modeling and Control. In Integral Methods in Science and Engineering; Constanda, C., Bodmann, B., Velho, H., Eds.; Birkhäuser: New York, NY, USA, 2013. [Google Scholar] [CrossRef] [Green Version]
- Bachmann, F.; Koch, G.; Pfister, M.; Szinnai, G.; Schropp, J. OptiDose: Computing the Individualized Optimal Drug Dosing Regimen Using Optimal Control. J. Optim. Theory Appl. 2021, 189, 46–65. [Google Scholar] [CrossRef] [PubMed]
- Padmanabhan, R.; Meskin, N.; Haddad, W.M. Optimal adaptive control of drug dosing using integral reinforcement learning. Math. Biosci. 2019, 309, 131–142. [Google Scholar] [CrossRef] [PubMed]
- Ai, Y.; Pan, B.; Fu, Y.; Wang, S. Control system design for a novel minimally invasive surgical robot. Comput. Assist. Surg. 2016, 21, 45–53. [Google Scholar] [CrossRef] [Green Version]
- Birs, I.; Muresan, C.; Ionescu, C. An event based implementation of a fractional order controller on a scalable nanorobot. In Proceedings of the European Control Conference (ECC), St. Petersburg, Russia, 12–15 May 2020; pp. 1436–1441. [Google Scholar] [CrossRef]
- Chongthavonsatit, N.; Kovavinthaweewat, C.; Yuksen, C.; Sittichanbuncha, Y.; Angkoontassaneeyarat, C.; Atiksawedparit, P.; Phattharapornjaroen, P. Comparison of Accuracy and Speed in Computer-Assisted Versus Conventional Methods for Pediatric Drug Dose Calculation: A Scenario-Based Randomized Controlled Trial. Glob. Pediatr. Health 2021, 8, 2333794X21999144. [Google Scholar] [CrossRef] [PubMed]
- Jayaraman, P.P.; Forkan, A.R.M.; Morshed, A.; Haghighi, P.D.; Kang, Y.-B. Healthcare 4.0: A review of frontiers in digital health. WIREs Data Min. Knowl. Discov. 2020, 10, 1–23. [Google Scholar] [CrossRef]
- Ghita, M.; Neckebroek, M.; Muresan, C.; Copot, D. Closed-Loop Control of Anesthesia: Survey on Actual Trends, Challenges and Perspectives. IEEE Access 2020, 8, 206264–206279. [Google Scholar] [CrossRef]
- Copot, D.; Muresan, C.; Birs, I.; Kovacs, L. Robust Hemodynamic Control Under General Anesthesia Conditions. IFAC-Pap. 2020, 53, 16179–16184. [Google Scholar] [CrossRef]
- Fellahi, J.L.; Futier, E.; Vaisse, C.; Collange, O.; Huet, O.; Loriau, J.; Gayat, E.; Tavernier, B.; Biais, M.; Asehnoune, K.; et al. Perioperative hemodynamic optimization: From guidelines to implementation—An experts’ opinion paper. Ann. Intensiv. Care 2021, 11, 58. [Google Scholar] [CrossRef]
- Copot, D.; Ionescu, C. Models for Nociception Stimulation and Memory Effects in Awake and Aware Healthy Individuals. IEEE Trans. Biomed. Eng. 2019, 66, 718–726. [Google Scholar] [CrossRef]
- Gentilini, A.; Rossoni-Gerosa, M.; Frei, C.; Wymann, R.; Morari, M.; Zbinden, A.; Schnider, T. Modeling and closed-loop control of hypnosis by means of bispectral index (BIS) with isoflurane. IEEE Trans. Biomed. Eng. 2001, 48, 874–889. [Google Scholar] [CrossRef]
- Copot, D.; Ionescu, C. Tailored Pharmacokinetic model to predict drug trapping in long-term anesthesia. J. Adv. Res. 2021, 32, 27–36. [Google Scholar] [CrossRef] [PubMed]
- Merigo, L.; Beschi, M.; Padula, F.; Latronico, N.; Paltenghi, M.; Visioli, A. Event-Based control of depth of hypnosis in anesthesia. Comput. Methods Programs Biomed. 2017, 147, 63–83. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Padula, F.; Ionescu, C.; Latronico, N.; Paltenghi, M.; Visioli, A.; Vivacqua, G. Optimized PID control of depth of hypnosis in anesthesia. Comput. Methods Programs Biomed. 2017, 144, 21–35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ionescu, C.M.; de Keyser, R.; Torrico, B.C.; de Smet, T.; Struys, M.M.R.F.; Normey-Rico, J.E. Robust predicitve control strategy applied for propofol dosing using BIS as a controlled variable during anesthesia. IEEE Trans. Biomed. Eng. 2008, 55, 2161–2170. [Google Scholar] [CrossRef]
- Merigo, L.; Padula, F.; Latronico, N.; Paltenghi, M.; Visioli, A. Event-based control tuning of propofol and remifentanil coadministration for general anaesthesia. IET Control. Theory Appl. 2020, 14, 2995–3008. [Google Scholar] [CrossRef]
- Araujo, H.; Xiao, B.; Liu, C.; Zhao, Y.; Lam, H.K. Design of type- 1 and interval type-2 fuzzy PID control for anesthesia using genetic algorithms. J. Intell. Learn. Syst. Appl. 2014, 4, 70–93. [Google Scholar] [CrossRef] [Green Version]
- Ionescu, C.; Neckebroek, M.; Ghita Mi Copot, D. An Open Source Patient Simulator for Design and Evaluation of Computer Based Multiple Drug Dosing Control for Anesthetic and Hemodynamic Variables. IEEE Access 2021, 9, 8680–8694. [Google Scholar] [CrossRef]
- Absalom, A.; Struys, M. An Overview of TCI and TIVA; Academia Press: Ghent, Belgium, 2007. [Google Scholar]
- Tao, Y.; Fang, M.; Wang, Y. A fault tolerant closed-loop anesthesia system based on internal model control and extended state observer. In Proceedings of the 25th Chinese Control and Decision Conference (CCDC ′13), Guiyang, China, 25–27 May 2013; pp. 4910–4914. [Google Scholar]
- Ilyas, M.; Butt, M.F.U.; Bilal, M.; Mahmood, K.; Khaqan, A.; Riaz, R.A. A Review of Modern Control Strategies for Clinical Evaluation of Propofol Anesthesia Administration Employing Hypnosis Level Regulation. BioMed Res. Int. 2017, 2017, 1–12. [Google Scholar] [CrossRef]
- Guy, A. Dumont, Closed-Loop Control of Anesthesia-A Review. IFAC Proc. Vol. 2012, 45, 373–378. [Google Scholar] [CrossRef]
- Medvedev, A.; Zhusubaliyev, Z.T.; Rosén, O.; Silva, M.M. Oscillations-free PID control of anesthetic drug delivery in neuromuscular blockade. Comput. Methods Programs Biomed. 2019, 171, 119–131. [Google Scholar] [CrossRef]
- da Silva, M.M.; Mendonça, T.; Wigren, T. Nonlinear adaptive control of the NeuroMuscular Blockade in anesthesia. In Proceedings of the 50th IEEE Conference on Decision and Control and European Control Conference, Orlando, FL, USA, 12–15 December 2011; pp. 41–46. [Google Scholar] [CrossRef]
- Mendonça, T.; Rocha, P.; Silva, J. 6-Modeling and control of neuromuscular blockade level in general anesthesia: The neuromuscular blockade case. In Automated Drug Delivery in Anesthesia; Copot, D., Ed.; Academic Press: Cambridge, MA, USA, 2020; pp. 167–195. [Google Scholar] [CrossRef]
- Janda, M.; Simanski, O.; Bajorat, J.; Pohl, B.; Noeldge-Schomburg, G.; Hofmockel, R. Clinical evaluation of a simultaneous closed-loop system for depth of anaesthesia and neuromuscular blockade. Anaesthesia 2011, 66, 1112–1120. [Google Scholar] [CrossRef] [PubMed]
- Zaouter, C.; Hemmerling, T.M.; Lanchon, R.; Valoti, E.; Remy, A.; Leuillet, S.; Ouattara, A. The feasibility of a completely automated total IV anesthesia drug delivery system for cardiac surgery. Anesth. Analg. 2016, 123, 885–893. [Google Scholar] [CrossRef] [PubMed]
- Isaka, S.; Sebald, A.V. Control strategies for arterial blood pressure regulation. IEEE Trans. Biomed. Eng. 1993, 40, 353–363. [Google Scholar] [CrossRef] [PubMed]
- Voss, G.I.; Katona, P.G.; Chizeck, H.J. Adaptive multivarable drug delivery: Control of artenal pressure and cardiac output in anesthetized dogs. IEEE Trans. Biomed. Eng. 1987, 34, 617–623. [Google Scholar] [CrossRef] [PubMed]
- de Moura Oliveira, P.B.; Durães, J.; Pires, E.J.S. Mean Arterial Pressure PID Control Using a PSO-BOIDS Algorithm. In Advances in Intelligent Systems and Computing, Proceedings of the International Joint Conference SOCO’13-CISIS’13-ICEUTE’13, Salamanca, Spain, 11–13 September 2013; Herrero, Á., Baruque, B., Klett, F., Abraham, A., Snášel, V., Carvalho, A.C.P.L.F., Bringas, P.G., Zelinka, I., Quintián, H., Corchado, E., Eds.; Springer: Cham, Switzerland, 2014; Volume 239. [Google Scholar] [CrossRef]
- Enbiya, S.; Mahieddine, F.; Hossain, A. Model Reference Adaptive Scheme for Multi-drug Infusion for Blood Pressure Control. J. Integr. Bioinform. 2011, 8, 43–56. [Google Scholar] [CrossRef]
- Padmanabhan, R.; Meskin, N.; Haddad, W.M. Closed-loop control of anesthesia and mean arterial pressure using reinforcement learning. Biomed. Signal Process. Control 2015, 22, 54–64. [Google Scholar] [CrossRef]
- Rao, R.; Palerm, C.; Aufderheide, B.; Bequette, W. Experimental studies on automated regulation of hemodynamic variables. IEEE Eng. Med. Biol. Mag. 2000, 20, 24–38. [Google Scholar]
- Rao, R.R.; Aufderheide, B.; Bequette, B.W. Experimental studies on multiple-model predictive control for automated regulation of hemodynamic variables. IEEE Trans. Biomed. Eng. 2003, 50, 277–288. [Google Scholar] [CrossRef]
- Kumar, A.; Raj, R. Design of a fractional order two layer fuzzy logic controller for drug delivery to regulate blood pressure. Biomed. Signal Process. Control 2022, 78, 104024. [Google Scholar] [CrossRef]
- Coronel-Escamilla, A.; Gomez-Aguilar, J.F.; Stamova, I.; Santamaria, F. Fractional order controllers increase the robustness of closed-loop deep brain stimulation systems. Chaos Solitons Fractals 2020, 140, 110149. [Google Scholar] [CrossRef]
- Balasaheb, W.V.; Chaskar, U.M. Arterial Blood Pressure Regulation using a Novel Fractional Order Based Sliding Mode Elephant Herd Controller. In Proceedings of the 5th International Conference on Intelligent Computing and Control Systems (ICICCS), Madurai, India, 6–8 May 2021; pp. 496–502. [Google Scholar]
- Navarro-Guerrero, G.; Tang, Y. Fractional-Order Closed-Loop Model Reference Adaptive Control for Anesthesia. Algorithms 2018, 11, 106. [Google Scholar] [CrossRef] [Green Version]
- Patel, B.J.; Patel, H.G. Design of CRONE-Based Fractional-Order Control Scheme for BIS Regulation in Intravenous Anesthesia. In Advances in Control Instrumentation Systems. Lecture Notes in Electrical Engineering; George, V., Roy, B., Eds.; Springer: Singapore, 2020; Volume 660. [Google Scholar]
- Copot, D.; Muresan, C.; de Keyser, R.; Ionescu, C. Patient specific model based induction of hypnosis using fractional order control. IFAC-PapersOnLine 2017, 50, 15097–15102. [Google Scholar] [CrossRef]
- Liu, N.; Chazot, T.; Hamada, S.; Landais, A.; Boichut, N.; Dussaussoy, C.; Trillat, B.; Beydon, L.; Samain, E.; Sessler, D.I.; et al. Closed-loop coadministration of propofol and remifentanil guided by bispectral index: A randomized multicenter study. Anesth. Analg. 2011, 112, 546–557. [Google Scholar] [CrossRef] [PubMed]
- Orliaguet, G.A.; Lambert, F.B.; Chazot, T.; Glasman, P.; Fischler, M.; Liu, N. Feasibility of Closed-loop Titration of Propofol and Remifentanil Guided by the Bispectral Monitor in Pediatric and Adolescent Patients: A Prospective Randomized Study. Anesthesiology 2015, 122, 759–767. [Google Scholar] [CrossRef] [Green Version]
- Urooj, S.; Singh, B. Fractional-order PID control for postoperative mean arterial blood pressure control scheme. Procedia Comput. Sci. 2019, 152, 380–389. [Google Scholar] [CrossRef]
- Nagarsheth, S.H.; Sharma, S.N. The Impact of Fractional-Order Control on Blood Pressure Regulation. Int. J. E-Health Med. Commun. 2021, 12, 38–54. [Google Scholar] [CrossRef]
- Birs, I.; Copot, D.; Muresan, C.I.; de Keyser, R.; Ionescu, C.M. Robust Fractional Order PI Control for Cardiac Output Stabilisation. IFAC-PapersOnLine 2019, 52, 994–999. [Google Scholar] [CrossRef]
- Hegedus, E.; Birs, I.; Muresan, C. Fractional Order Control of the Combined Anaesthesia-Hemodynamic System: A Preliminary Study. IFAC-PapersOnLine 2021, 54, 19–24. [Google Scholar] [CrossRef]
- Oustaloup, A.; Levron, F.; Mathieu, B.; Nanot, F.M. Frequency-band complex noninteger differentiator: Characterization and synthesis. In IEEE Transactions on Circuits and Systems I: Fundamental Theory and Application; IEEE: New York, NY, USA, 2000; Volume 47, pp. 25–39. [Google Scholar] [CrossRef]
- Monje, C.A.; Chen, Y.; Vinagre, B.M.; Xue, D.; Feliu-Batlle, V.; Feliu, V. Fractional-Order Systems and Controls. Fundamentals and Applications; Springer: London, UK, 2010. [Google Scholar]
- Muresan, C.I.; De Keyser, R. Revisiting Ziegler–Nichols. A fractional order approach. ISA Trans. 2022, 129, 287–296. [Google Scholar] [CrossRef]
- Neckebroek, M.; Ionescu, C.-M.; van Amsterdam, K.; de Smet, T.; de Baets, P.; Decruyenaere, J.; de Keyser, R.; Struys, M. A comparison of propofol-to-BIS post-operative intensive care sedation by means of target controlled infusion, Bayesian-based and predictive control methods: An observational, open-label pilot study. J. Clin. Monit. Comput. 2019, 33, 675–686. [Google Scholar] [CrossRef] [Green Version]
- Copot, D.; de Keyser, R.; Ionescu, C. Drug Interaction Between Propofol and Remifentanil in Individualised Drug Delivery Systems. 9th IFAC Symposium on Biological and Medical Systems. IFAC-PapersOnLine 2015, 48, 64–69. [Google Scholar] [CrossRef] [Green Version]
- Struys, M.M.; Coppens, M.J.; de Neve, N.; Mortier, E.P.; Doufas, A.G.; van Bocxlaer, J.F.; Shafer, S.L. Influence of administration rate on propofol plasma-effect site equilibration. Anesthesiology 2007, 107, 386–396. [Google Scholar] [CrossRef] [PubMed]








| Index | Age (yrs) | Height (cm) | Weight (kg) | C50 (mg/ml) | γ (-) |
|---|---|---|---|---|---|
| 1 | 74 | 164 | 88 | 2.5 | 3 |
| 2 | 67 | 161 | 69 | 4.6 | 2 |
| 3 | 75 | 176 | 101 | 5 | 1.6 |
| 4 | 69 | 173 | 97 | 1.8 | 2.5 |
| 5 | 45 | 171 | 64 | 6.8 | 1.78 |
| 6 | 57 | 182 | 80 | 2.7 | 2.8 |
| 7 | 74 | 155 | 55 | 1.7 | 3.5 |
| 8 | 71 | 172 | 78 | 7.8 | 2.9 |
| 9 | 65 | 176 | 77 | 2.9 | 1.88 |
| 10 | 72 | 192 | 73 | 3.9 | 3.1 |
| 11 | 69 | 168 | 84 | 2.3 | 3.1 |
| 12 | 60 | 190 | 92 | 4.8 | 2.1 |
| 13 | 61 | 177 | 81 | 2.5 | 3 |
| 14 | 54 | 173 | 86 | 2.5 | 3 |
| 15 | 71 | 172 | 83 | 4.3 | 1.9 |
| 16 | 53 | 186 | 114 | 2.7 | 1.6 |
| 17 | 72 | 162 | 87 | 4.5 | 2.9 |
| 18 | 61 | 182 | 93 | 2.7 | 1.78 |
| 19 | 70 | 167 | 77 | 6.8 | 3.1 |
| 20 | 69 | 168 | 82 | 9.8 | 1.6 |
| 21 | 69 | 158 | 81 | 3.2 | 2.1 |
| 22 | 60 | 165 | 85 | 5.1 | 2.51 |
| 23 | 70 | 173 | 69 | 3.67 | 3.1 |
| 24 | 56 | 186 | 99 | 5.8 | 2.3 |
| Patient | TT (s) | Undershoot (%) | BIS-NADIR |
|---|---|---|---|
| 1 | 140.56 | 1.78 | 40.82 |
| 2 | 104.41 | 1.93 | 40.77 |
| 3 | 219.36 | 1.63 | 40.86 |
| 4 | 166.37 | 1.64 | 40.85 |
| 5 | 112.25 | 2.68 | 40.83 |
| 6 | 129.51 | 1.66 | 40.83 |
| 7 | 96.73 | 2.83 | 40.74 |
| 8 | 117.32 | 1.95 | 40.79 |
| 9 | 120.20 | 1.83 | 40.81 |
| 10 | 131.79 | 1.86 | 40.81 |
| 11 | 129.36 | 1.78 | 40.81 |
| 12 | 145.74 | 1.66 | 40.85 |
| 13 | 124.43 | 1.77 | 40.82 |
| 14 | 126.91 | 1.69 | 40.83 |
| 15 | 124.84 | 1.91 | 40.80 |
| 16 | 230.84 | 1.03 | 40.95 |
| 17 | 134.84 | 1.76 | 40.82 |
| 18 | 142.40 | 1.67 | 40.84 |
| 19 | 114.15 | 1.93 | 40.79 |
| 20 | 122.36 | 1.86 | 40.80 |
| 21 | 124.04 | 1.75 | 40.81 |
| 22 | 124.34 | 1.73 | 40.82 |
| 23 | 109.79 | 1.94 | 40.78 |
| 24 | 152.03 | 1.56 | 40.86 |
| Mean | 135.19 | 1.83 | 40.82 |
| Std. Dev. | 31.65 | 0.34 | 0.04 |
| Min | 96.73 | 1.03 | 40.74 |
| Max | 230.84 | 2.83 | 40.95 |
| Controller Type | Iso-Damping | Phase Margin PM (deg) | Gain Crossover Frequency (rad/s) | Nominal Sensitivity Peak (dB) | T Function Value at | Integral of Absolute Error (IAE) (-) |
|---|---|---|---|---|---|---|
| Induction FOPID | YES | 84 | 0.017 | +3.28 | −75.0 | 66.31 |
| FO-PI with iso-damping | YES | 60 | 0.0305 | +9.06 | −65.5 | 45.38 |
| FO-PI with minimum IAE | NO | 61.39 | 0.0308 | +2.7 | −101.1 | 33.23 |
| FOPID with minimum IAE | NO | 55.73 | 0.0400 | +5.23 | −56.2 | 30.58 |
| Patient | TTn (seconds) | BIS-NADIRn (%) | TTp (seconds) | BIS-NADIRp (%) |
|---|---|---|---|---|
| 1 | 35.11 | 41.21 | 0 | 54.46 |
| 2 | 36.95 | 41.02 | 0 | 54.67 |
| 3 | 32.05 | 41.28 | 0 | 54.46 |
| 4 | 34.69 | 41.27 | 0 | 54.44 |
| 5 | 36.79 | 41.20 | 0 | 54.57 |
| 6 | 35.69 | 41.26 | 0 | 54.43 |
| 7 | 40.24 | 40.93 | 4.56 | 55.30 |
| 8 | 35.95 | 41.12 | 0 | 54.46 |
| 9 | 35.99 | 41.17 | 0 | 54.44 |
| 10 | 35.36 | 41.18 | 0 | 54.46 |
| 11 | 35.55 | 41.19 | 0 | 54.45 |
| 12 | 35.11 | 41.29 | 0 | 54.43 |
| 13 | 35.86 | 41.21 | 0 | 54.44 |
| 14 | 35.83 | 41.27 | 0 | 54.43 |
| 15 | 35.61 | 41.15 | 0 | 54.46 |
| 16 | 31.08 | 41.43 | 0 | 54.41 |
| 17 | 35.32 | 41.20 | 0 | 54.45 |
| 18 | 35.19 | 41.28 | 0 | 54.43 |
| 19 | 36.17 | 41.10 | 0 | 54.49 |
| 20 | 35.81 | 41.16 | 0 | 54.45 |
| 21 | 35.81 | 41.17 | 0 | 54.44 |
| 22 | 35.90 | 41.22 | 0 | 54.43 |
| 23 | 36.44 | 41.07 | 0 | 54.59 |
| 24 | 34.98 | 41.33 | 0 | 54.43 |
| Mean | 35.56 | 41.20 | 0.19 | 54.50 |
| Std. Dev. | 1.63 | 0.10 | 0.93 | 0.18 |
| Min | 31.08 | 40.93 | 0 | 54.41 |
| Max | 40.24 | 41.43 | 4.56 | 55.30 |
| Patient | TT (s) | Undershoot (%) | BIS-NADIR |
|---|---|---|---|
| 1 | 140.56 | 1.37 | 41.21 |
| 2 | 104.41 | 1.26 | 41.02 |
| 3 | 219.36 | 1.41 | 41.28 |
| 4 | 166.37 | 1.35 | 41.27 |
| 5 | 112.25 | 2.53 | 41.20 |
| 6 | 129.51 | 1.24 | 41.26 |
| 7 | 96.73 | 2.57 | 40.93 |
| 8 | 117.32 | 1.35 | 41.12 |
| 9 | 120.20 | 1.29 | 41.17 |
| 10 | 131.79 | 1.38 | 41.18 |
| 11 | 129.36 | 1.32 | 41.19 |
| 12 | 145.74 | 1.33 | 41.29 |
| 13 | 124.43 | 1.28 | 41.21 |
| 14 | 126.91 | 1.24 | 41.27 |
| 15 | 124.84 | 1.37 | 41.15 |
| 16 | 230.84 | 1.00 | 41.43 |
| 17 | 134.84 | 1.33 | 41.20 |
| 18 | 142.40 | 1.32 | 41.28 |
| 19 | 114.15 | 1.31 | 41.10 |
| 20 | 122.36 | 1.33 | 41.16 |
| 21 | 124.04 | 1.26 | 41.17 |
| 22 | 124.34 | 1.25 | 41.22 |
| 23 | 109.79 | 1.28 | 41.07 |
| 24 | 152.03 | 1.29 | 41.33 |
| Mean | 135.19 | 1.40 | 41.20 |
| Std. Dev. | 31.65 | 0.36 | 0.10 |
| Min | 96.73 | 1.00 | 40.93 |
| Max | 230.84 | 2.57 | 41.43 |
| Patient | TTn (s) | BIS-NADIRn (%) | TTp (s) | BIS-NADIRp (%) |
|---|---|---|---|---|
| 1 | 35.11 | 41.21 | 0 | 54.46 |
| 2 | 36.95 | 41.02 | 0 | 54.67 |
| 3 | 32.05 | 41.28 | 0 | 54.46 |
| 4 | 34.69 | 41.27 | 0 | 54.44 |
| 5 | 36.79 | 41.20 | 0 | 54.57 |
| 6 | 35.69 | 41.26 | 0 | 54.43 |
| 7 | 40.24 | 40.93 | 4.56 | 55.30 |
| 8 | 35.95 | 41.12 | 0 | 54.46 |
| 9 | 35.99 | 41.17 | 0 | 54.44 |
| 10 | 35.36 | 41.18 | 0 | 54.46 |
| 11 | 35.55 | 41.19 | 0 | 54.45 |
| 12 | 35.11 | 41.29 | 0 | 54.43 |
| 13 | 35.86 | 41.21 | 0 | 54.44 |
| 14 | 35.83 | 41.27 | 0 | 54.43 |
| 15 | 35.61 | 41.15 | 0 | 54.46 |
| 16 | 31.08 | 41.43 | 0 | 54.41 |
| 17 | 35.32 | 41.20 | 0 | 54.45 |
| 18 | 35.19 | 41.28 | 0 | 54.43 |
| 19 | 36.17 | 41.10 | 0 | 54.49 |
| 20 | 35.81 | 41.16 | 0 | 54.45 |
| 21 | 35.81 | 41.17 | 0 | 54.44 |
| 22 | 35.90 | 41.22 | 0 | 54.43 |
| 23 | 36.44 | 41.07 | 0 | 54.59 |
| 24 | 34.98 | 41.33 | 0 | 54.43 |
| Mean | 35.56 | 41.20 | 0.19 | 54.50 |
| Std. Dev. | 1.63 | 0.10 | 0.93 | 0.18 |
| Min | 31.08 | 40.93 | 0 | 54.41 |
| Max | 40.24 | 41.43 | 4.56 | 55.30 |
| Substance | Maximum Allowed Dosage for Adult Patients up to 55 Years Old | |
|---|---|---|
| Induction | Maintenance | |
| Propofol | 2.5 mg/kg IV titrated to 40 mg every 10 seconds until onset of induction | 150 to 200 ug/kg/min IV for the first 10 to 15 min, then decreased by 30% to 50% during the first 30 min of maintenance |
| Remifentanil | 1 ug/kg/min for 30 to 60 seconds | 0.4 ug/kg/min (range 0.1 to 2 micrograms/kg/min) |
| Dopamine | 10 ug/kg/min | 50 ug/kg/min |
| SNP | 0.3 ug/kg/min, but the dose can be adjusted up to 10 ug/kg/min in major cases | 0.3 ug/kg/min, but the dose can be adjusted up to 10 ug/kg/min in major cases |
| Atracurium | 0.6 mg/kg (bolus injection) | 13 ug/kg/min (can be adjusted up to 29.5 ug/kg/min if patient does not respond to initial dose—major cases only) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hegedus, E.T.; Birs, I.R.; Ghita, M.; Muresan, C.I. Fractional-Order Control Strategy for Anesthesia–Hemodynamic Stabilization in Patients Undergoing Surgical Procedures. Fractal Fract. 2022, 6, 614. https://doi.org/10.3390/fractalfract6100614
Hegedus ET, Birs IR, Ghita M, Muresan CI. Fractional-Order Control Strategy for Anesthesia–Hemodynamic Stabilization in Patients Undergoing Surgical Procedures. Fractal and Fractional. 2022; 6(10):614. https://doi.org/10.3390/fractalfract6100614
Chicago/Turabian StyleHegedus, Erwin T., Isabela R. Birs, Mihaela Ghita, and Cristina I. Muresan. 2022. "Fractional-Order Control Strategy for Anesthesia–Hemodynamic Stabilization in Patients Undergoing Surgical Procedures" Fractal and Fractional 6, no. 10: 614. https://doi.org/10.3390/fractalfract6100614






