Expectations and Experiences of Participating in a Supervised and Home-Based Physical Exercise Intervention in Patients with Head and Neck Cancer during Chemoradiotherapy: A Qualitative Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethics
2.2. Setting, Eligibility and Recruitment
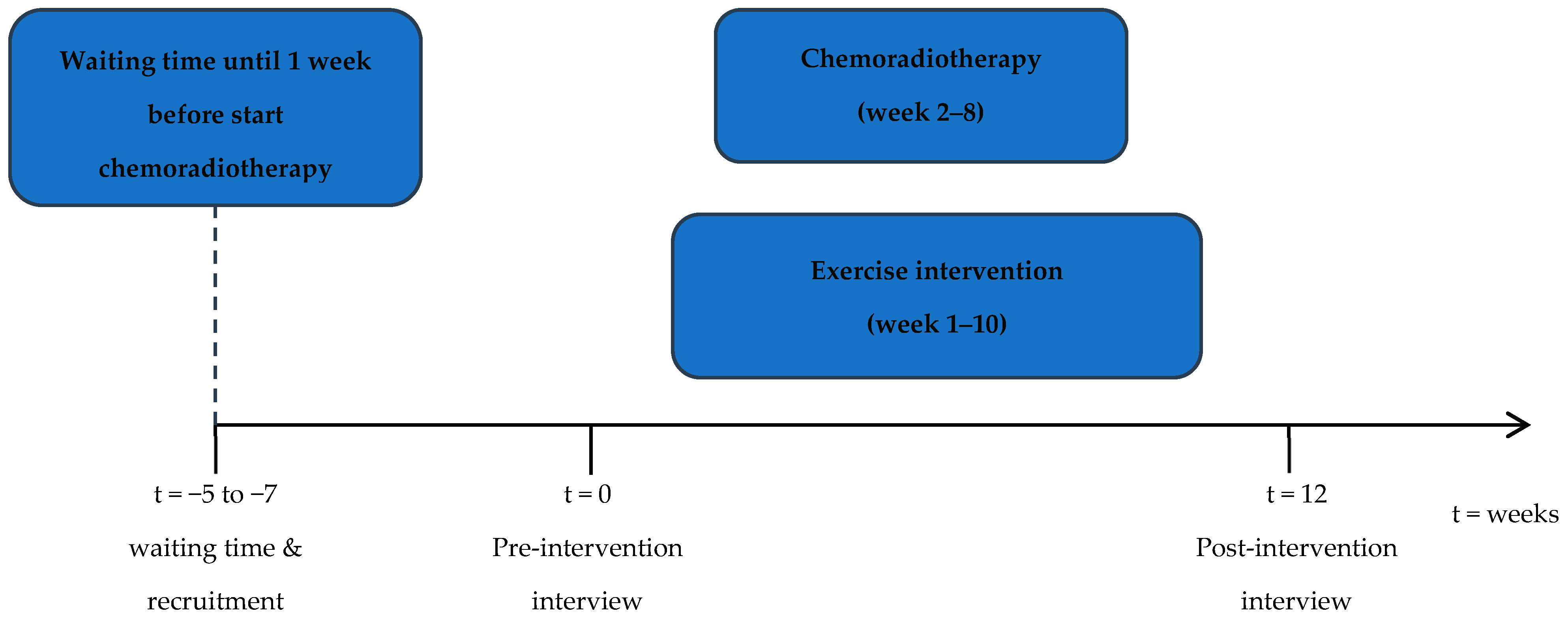
2.3. Exercise Intervention
2.4. Pre- and Post-Intervention Interviews
2.5. Data Analysis
3. Results
3.1. Participants
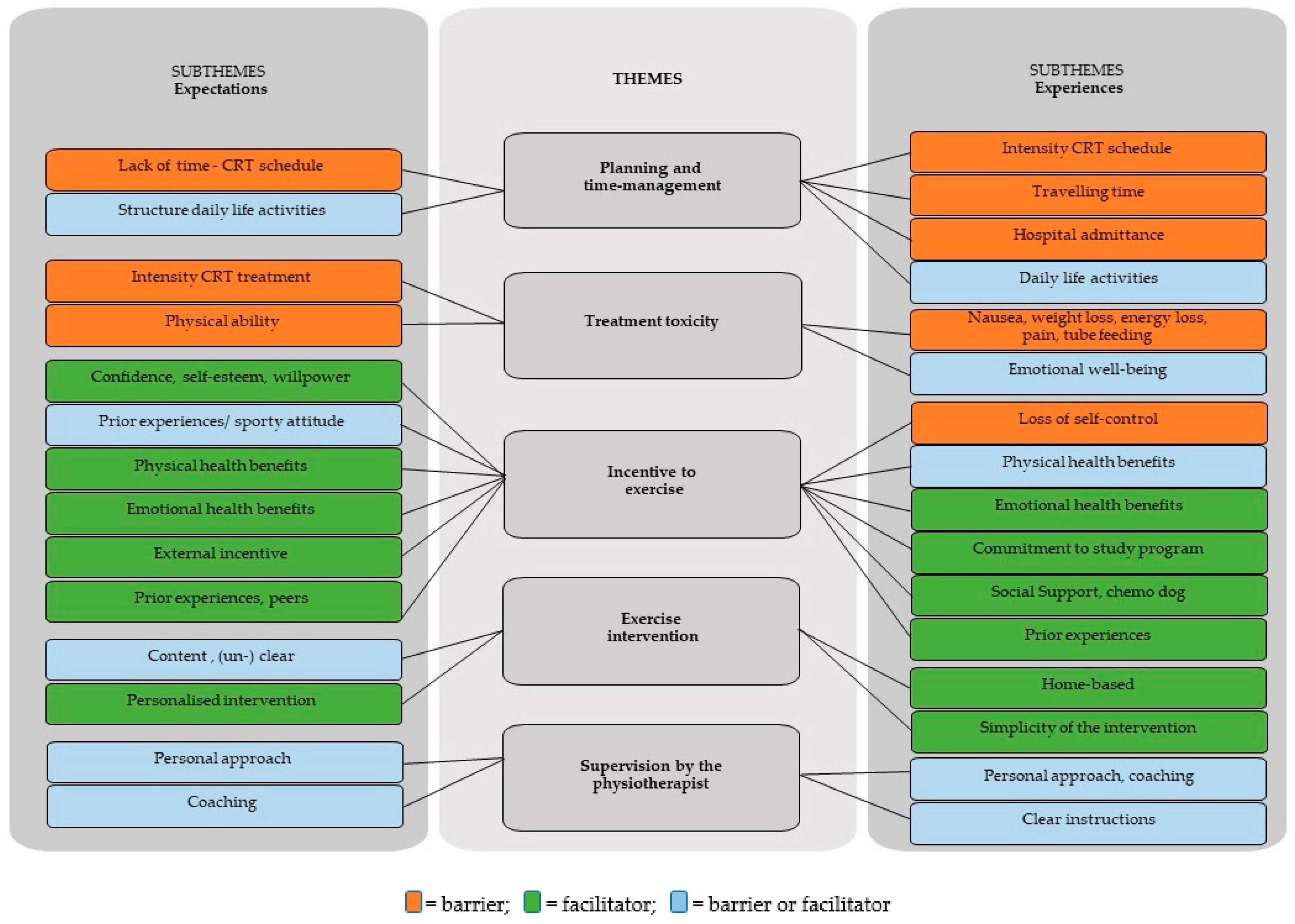
3.2. Overview of Findings
3.2.1. Theme (1) Planning and Time Management
3.2.2. Theme (2) Treatment Toxicity
3.2.3. Theme (3) Motivation to Exercise
3.2.4. Theme (4) Exercise Intervention
3.2.5. Theme (5) Supervision by the Physiotherapist
3.2.6. Suggestions for Improvement—Comments from Participants
4. Discussion
Clinical Implications and Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ameri, A.; Norouzi, S.; Sourati, A.; Azghandi, S.; Novin, K.; Taghizadeh-Hesary, F. Randomized trial on acute toxicities of weekly vs. three-weekly cisplatin-based chemoradiation in head and neck cancer. Cancer Rep. 2022, 5, e1425. [Google Scholar] [CrossRef]
- Szturz, P.; Wouters, K.; Kiyota, N.; Tahara, M.; Prabhash, K.; Noronha, V.; Castro, A.; Licitra, L.; Adelstein, D.; Vermorken, J.B. Weekly Low-Dose Versus Three-Weekly High-Dose Cisplatin for Concurrent Chemoradiation in Locoregionally Advanced Non-Nasopharyngeal Head and Neck Cancer: A Systematic Review and Meta-Analysis of Aggregate Data. Oncologist 2017, 22, 1056–1066. [Google Scholar] [CrossRef]
- Van den Bosch, L.; van der Laan, H.P.; van der Schaaf, A.; Oosting, S.F.; Halmos, G.B.; Witjes, M.J.H.; Oldehinkel, E.; Meijer, T.W.H.; van den Hoek, J.G.M.; Steenbakkers, R.J.H.M.; et al. Patient-Reported Toxicity and Quality-of-Life Profiles in Patients With Head and Neck Cancer Treated with Definitive Radiation Therapy or Chemoradiation. Int. J. Radiat. Oncol. Biol. Phys. 2021, 111, 456–467. [Google Scholar] [CrossRef] [PubMed]
- Silver, H.J.; Dietrich, M.S.; Murphy, B.A. Changes in body mass, energy balance, physical function, and inflammatory state in patients with locally advanced head and neck cancer treated with concurrent chemoradiation after low-dose induction chemotherapy. Head. Neck. 2007, 29, 893–900. [Google Scholar] [CrossRef]
- Rogers, L.Q.; Courneya, K.S.; Robbins, K.T.; Malone, J.; Seiz, A.; Koch, L.; Rao, K.; Nagarkar, M. Physical activity and quality of life in head and neck cancer survivors. Support. Care Cancer 2006, 14, 1012–1019. [Google Scholar] [CrossRef] [PubMed]
- Ligibel, J.A.; Bohlke, K.; May, A.M.; Clinton, S.K.; Demark-Wahnefried, W.; Gilchrist, S.C.; Irwin, M.L.; Late, M.; Mansfield, S.; Marshall, T.F.; et al. Exercise, Diet, and Weight Management During Cancer Treatment: ASCO Guideline. J. Clin. Oncol. 2022, 40, 2491–2507. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.V.; Friedenreich, C.M.; Moore, S.C.; Hayes, S.C.; Silver, J.K.; Campbell, K.L.; Winters-Stone, K.; Gerber, L.H.; George, S.M.; Fulton, J.E.; et al. American College of Sports Medicine roundtable report on physical activity, sedentary behavior, and cancer prevention and control. Med. Sci. Sports Exerc. 2019, 51, 2391–2402. [Google Scholar] [CrossRef]
- Campbell, K.L.; Winters-Stone, K.M.; Wiskemann, J.; May, A.M.; Schwartz, A.L.; Courneya, K.S.; Zucker, D.; Matthews, C.; Ligibel, J.; Gerber, L.; et al. Exercise Guidelines for Cancer Survivors: Consensus Statement from International Multidisciplinary Roundtable. Med. Sci. Sports Exerc. 2019, 51, 2375–2390. [Google Scholar] [CrossRef]
- Sealy, M.J.; Stuiver, M.M.; Midtgaard, J.; van der Schans, C.P.; Roodenburg, J.L.N.; Jager-Wittenaar, H. Perception and Performance of Physical Activity Behavior after Head and Neck Cancer Treatment: Exploration and Integration of Qualitative and Quantitative Findings. Int. J. Environ. Res. Public Health 2021, 19, 287. [Google Scholar] [CrossRef]
- D’Souza, M.; Samuel, S.R.; Saxena, P.P. Effects of Exercise Training during Concomitant Chemoradiation Therapy in Head-and-Neck Cancer Patients: A Systematic Review. Indian J. Palliat. Care. 2020, 26, 531–532. [Google Scholar]
- Lonkvist, C.K.; Lonbro, S.; Vinther, A.; Zerahn, B.; Rosenbom, E.; Primdahl, H.; Hojman, P.; Gehl, J. Progressive resistance training in head and neck cancer patients during concomitant chemoradiotherapy—Design of the DAHANCA 31 randomized trial. BMC Cancer 2017, 17, 400. [Google Scholar] [CrossRef]
- Samuel, S.R.; Maiya, A.G.; Fernandes, D.J.; Guddattu, V.; Saxena, P.U.P.; Kurian, J.R.; Lin, P.-J.; Mustian, K.M. Effectiveness of exercise-based rehabilitation on functional capacity and quality of life in head and neck cancer patients receiving chemo-radiotherapy. Support. Care Cancer 2019, 27, 3913–3920. [Google Scholar] [CrossRef]
- Kok, A.; Passchier, E.; May, A.M.; van den Brekel, M.W.; Jager-Wittenaar, H.; Veenhof, C.; de Bree, R.; Stuiver, M.M.; Speksnijder, C.M. Feasibility of a supervised and home-based tailored exercise intervention in head and neck cancer patients during chemoradiotherapy. Eur. J. Cancer Care 2022, 31, e13662. [Google Scholar] [CrossRef]
- Ning, Y.; Wang, Q.; Ding, Y.; Zhao, W.; Jia, Z.; Wang, B. Barriers and facilitators to physical activity participation in patients with head and neck cancer: A scoping review. Support. Care Cancer 2022, 30, 4591–4601. [Google Scholar] [CrossRef]
- Buffart, L.M.; de Bree, R.; Altena, M.; van der Werff, S.; Drossaert, C.H.C.; Speksnijder, C.M.; van Den Brekel, M.W.; Jager-Wittenaar, H.; Aaronson, N.K.; Stuiver, M.M. Demographic, clinical, lifestyle-related, and social-cognitive correlates of physical activity in head and neck cancer survivors. Support. Care Cancer 2018, 26, 1447–1456. [Google Scholar] [CrossRef]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef]
- Creswell, J.W.; Poth, C.N. Qualitative Inquiry and Research Design: Choosing among Five Approaches, 4th ed.; Sage Publications Inc.: Thousand Oaks, CA, USA, 2017. [Google Scholar]
- Guest, G.; Bunce, A.; Johnson, L. How Many Interviews Are Enough?:An Experiment with Data Saturation and Variability. Field Methods 2006, 18, 59–82. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Sandmael, J.A.; Bye, A.; Solheim, T.S.; Stene, G.B.; Thorsen, L.; Kaasa, S.; Lund, J.; Oldervoll, L.M. Feasibility and preliminary effects of resistance training and nutritional supplements during versus after radiotherapy in patients with head and neck cancer: A pilot randomized trial. Cancer 2017, 123, 4440–4448. [Google Scholar] [CrossRef] [PubMed]
- Felser, S.; Behrens, M.; Liese, J.; Strueder, D.F.; Rhode, K.; Junghanss, C.; Grosse-Thie, C. Feasibility and Effects of a Supervised Exercise Program Suitable for Independent Training at Home on Physical Function and Quality of Life in Head and Neck Cancer Patients: A Pilot Study. Integr. Cancer Ther. 2020, 19, 1534735420918935. [Google Scholar] [CrossRef] [PubMed]
- Jackson, C.; Dowd, A.J.; Capozzi, L.C.; Bridel, W.; Lau, H.Y.; Culos-Reed, S.N. A turning point: Head and neck cancer patients’ exercise preferences and barriers before and after participation in an exercise intervention. Eur. J. Cancer Care 2018, 27, e12826. [Google Scholar] [CrossRef]
- Capozzi, L.C.; McNeely, M.L.; Lau, H.Y.; Reimer, R.A.; Giese-Davis, J.; Fung, T.S.; Culos-Reed, S.N. Patient-reported outcomes, body composition, and nutrition status in patients with head and neck cancer: Results from an exploratory randomized controlled exercise trial. Cancer 2016, 122, 1185–1200. [Google Scholar] [CrossRef]
- Hammermuller, C.; Hinz, A.; Dietz, A.; Wichmann, G.; Pirlich, M.; Berger, T.; Zimmermann, K.; Neumuth, T.; Mehnert-Theuerkauf, A.; Wiegand, S.; et al. Depression, anxiety, fatigue, and quality of life in a large sample of patients suffering from head and neck cancer in comparison with the general population. BMC Cancer 2021, 21, 94. [Google Scholar] [CrossRef]
- Williams, C. Psychosocial Distress and Distress Screening in Multidisciplinary Head and Neck Cancer Treatment. Otolaryngol. Clin. N. Am. 2017, 50, 807–823. [Google Scholar] [CrossRef]
- Kampshoff, C.S.; van Mechelen, W.; Schep, G.; Nijziel, M.R.; Witlox, L.; Bosman, L.; Chinapaw, M.J.M.; Brug, J.; Buffart, L.M. Participation in and adherence to physical exercise after completion of primary cancer treatment. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 100. [Google Scholar] [CrossRef]
- Ghazali, N.; Roe, B.; Lowe, D.; Tandon, S.; Jones, T.; Brown, J.; Shaw, R.; Risk, J.; Rogers, S.N. Screening for distress using the distress thermometer and the University of Washington Quality of Life in post-treatment head and neck cancer survivors. Eur. Arch. Otorhinolaryngol. 2017, 274, 2253–2260. [Google Scholar] [CrossRef] [PubMed]
- Wijma, A.J.; Bletterman, A.N.; Clark, J.R.; Vervoort, S.; Beetsma, A.; Keizer, D.; Nijs, J.; Van Wilgen, C.P. Patient-centeredness in physiotherapy: What does it entail? A systematic review of qualitative studies. Physiother. Theory Pract. 2017, 33, 825–840. [Google Scholar] [CrossRef] [PubMed]
- Singh, B.; Olds, T.; Curtis, R.; Dumuid, D.; Virgara, R.; Watson, A.; Szeto, K.; O’Connor, E.; Ferguson, T.; Eglitis, E.; et al. Effectiveness of physical activity interventions for improving depression, anxiety and distress: An overview of systematic reviews. Br. J. Sports Med. 2023, 57, 1203–1209. [Google Scholar] [CrossRef] [PubMed]
- McDonough, M.H.; Beselt, L.J.; Kronlund, L.J.; Albinati, N.K.; Daun, J.T.; Trudeau, M.S.; Wong, J.B.; Culos-Reed, S.N.; Bridel, W. Social support and physical activity for cancer survivors: A qualitative review and meta-study. J. Cancer Surviv. 2021, 15, 713–728. [Google Scholar] [CrossRef] [PubMed]
- Wells, M.; King, E. Patient adherence to swallowing exercises in head and neck cancer. Curr. Opin. Otolaryngol. Head. Neck Surg. 2017, 25, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Rogers, S.N.; Lowe, D.; Midgley, A.W. Patients’ views of physical activity whilst living with and beyond head and neck cancer. Int. J. Oral. Maxillofac. Surg. 2022, 51, 323–331. [Google Scholar] [CrossRef]
- van Vulpen, J.K.; Witlox, L.; Methorst-de Haan, A.C.; Hiensch, A.E.; van Hillegersberg, R.; Ruurda, J.P.; Nieuwenhuijzen, G.A.P.; Kouwenhoven, E.A.; Siersema, P.D.; May, A.M. Perceived facilitators and barriers by esophageal cancer survivors participating in a post-treatment exercise program. Support. Care Cancer 2023, 31, 320. [Google Scholar] [CrossRef] [PubMed]
- Buffart, L.M.; Kalter, J.; Sweegers, M.G.; Courneya, K.S.; Newton, R.U.; Aaronson, N.K.; Jacobsen, P.B.; May, A.M.; Galvao, D.A.; Chinapaw, M.J.; et al. Effects and moderators of exercise on quality of life and physical function in patients with cancer: An individual patient data meta-analysis of 34 RCTs. Cancer Treat. Rev. 2017, 52, 91–104. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, S.A.; O’Connor, L.; McGee, A.; Kilcoyne, A.Q.; Connolly, A.; Mockler, D.; Guinan, E.; O’Neill, L. Recruitment rates and strategies in exercise trials in cancer survivorship: A systematic review. J. Cancer Surviv. 2023; Online ahead of print. Available online: https://pubmed.ncbi.nlm.nih.gov/37022641/ (accessed on 31 January 2024).
- van der Meer, H.A.; de Pijper, L.; van Bruxvoort, T.; Visscher, C.M.; Nijhuis-van der Sanden, M.W.G.; Engelbert, R.H.H.; Speksnijder, C.M. Using e-Health in the physical therapeutic care process for patients with temporomandibular disorders: A qualitative study on the perspective of physical therapists and patients. Disabil. Rehabil. 2022, 44, 617–624. [Google Scholar] [CrossRef] [PubMed]
- Toonders, S.A.J.; van der Meer, H.A.; van Bruxvoort, T.; Veenhof, C.; Speksnijder, C.M. Effectiveness of remote physiotherapeutic e-Health interventions on pain in patients with musculoskeletal disorders: A systematic review. Disabil. Rehabil. 2022, 45, 3620–3638. [Google Scholar] [CrossRef]
| Participant No. | Age (years) | Gender | Educational Level 1 | Disease Stage | Tumor Location | Number of Attended Supervised Sessions (out of 10) | Completed the Intervention | Interview before Intervention | Interview after Intervention | Rating Exercise Intervention 2 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 58 | M | Middle | IV | Oro- pharynx | 4 | yes | yes | yes | 8 |
| 2 | 56 | M | High | III | Oro- pharynx | 2 | no | yes | yes | missing |
| 3 | 35 | M | Middle | IV | Oral cavity | 9 | yes | yes | yes | 8 |
| 4 | 65 | F | Middle | IV | Oro- pharynx | 2 | no | yes | yes | 8 |
| 5 | 60 | M | Middle | V | Oro- pharynx | 9 | yes | yes | yes | 6 |
| 6 | 47 | M | Middle | III | Oro- pharynx | 2 | no | yes | yes | 8 |
| 7 | 63 | M | Middle | IV | Oral cavity | 7 | yes | yes | yes | 8 |
| 8 | 70 | M | Low | IV | Hypopharynx | 3 | no | yes | no | missing |
| 9 | 59 | F | High | IV | Oro- pharynx | 10 | yes | yes | yes | 8 |
| 10 | 58 | M | Middle | III | Oro- pharynx | 8 | yes | yes | yes | 5 |
| 11 | 53 | F | High | III | Oro- pharynx | 4 | no | yes | yes | 7.5 |
| 12 | 67 | M | High | IV | Oral cavity | 8 | yes | yes | yes | 10 |
| 13 | 54 | M | Middle | IV | Oral cavity | 4 | yes | yes | no | missing |
| 14 | 56 | M | High | IV | Oro- pharynx | 10 | yes | yes | yes | 7.5 |
| Themes | Subthemes | Quotes (Patient nr, Quote nr) |
|---|---|---|
| Planning and time management | Expectations | |
| Lack of time due to chemoradiotherapy schedule | “I hesitated because I already saw my agenda filling up completely with all sorts of different things.” (patient nr. 12, quote nr. 1) | |
| Structure of daily life activities | “My daily routine is completely thrown off, you are not in charge of your own calendar anymore, so it is a bit of a puzzle where to fit this in, but then again this number of exercises should not make this impossible.” (patient nr 2, quote nr. 2) | |
| Experiences | ||
| Intensity of chemoradiotherapy schedule | “You do not know what hits you. You must see the dental hygienist, the dietitian, the speech therapist… In the month of May, we had over 50 appointments scheduled at the hospital.” (patient nr. 4, quote nr. 3) | |
| Intensity of chemoradiotherapy schedule, travelling time | “And the reason for dropping out, that had to do with, like, there is so much you have to deal with when starting [therapy], you hardly realize what you agreed to. The intensity of the program and all that comes with it, not just the program, but having to travel more than three hours every day to get to and from the hospital. And then also having to comply to this program, in combination with all kinds of other appointments, that made it too hard.” (patient nr. 2, quote nr. 4) | |
| Treatment toxicity | Expectations | |
| Intensity of chemoradiotherapy treatment, physical ability | “I can imagine, that when you have just had your chemotherapy treatment, and you are extremely nauseated. Well, then, of course, it becomes difficult to motivate yourself and actually perform the exercises.” (patient nr. 10, quote nr. 5) | |
| Experiences | ||
| Nausea, weight loss, energy loss, pain, tube feeding | “At one point I could not stop throwing up… in a few days I became scrawny. It terrified me. Then I was admitted to the hospital. So, then you’re not like; okay, I should go ahead and do my exercises now.” (patient nr. 11, quote nr. 6) | |
| Emotional well-being | “You are happy after that last radiotherapy treatment; it’s over, you could just kiss everyone. But then you fall into a void, and then it is nice that there still is this exercise program, with its weekly appointments with the physiotherapist, so there was at least that, so this was especially helpful mentally. (patient nr. 4, quote nr. 7) | |
| Motivation to exercise | Expectations | |
| Physical health benefits | “Motivation to survive, and also a shorter rehabilitation period, but initially, strive to survive. So, everything I can do to support this treatment I will do. ” (patient nr. 3, quote nr. 8) | |
| Willpower | “There is no such thing as “I can’t do this anymore”, never ever, I can always take it a step further, at least at my level you can always take it a step further. The average top athlete will not be able to run much faster, but in my condition, there is always room for improvement” (patient nr. 3, quote nr. 9) | |
| Confidence | “Self-esteem, increasing confidence. I guess. Feeling less of a pitiful little creature… feeling better both physically and mentally being more confident. “ (patient nr 12, quote nr. 10) | |
| Sporty attitude | “Anyway, I already had the intention [to exercise] in advance. If you exercise on a regular basis during treatment, that’s just better. You pull through easier, you are fitter, you might have less drug side-effects and so on.” (patient nr. 10, quote nr. 11) | |
| Lack of sporty attitude | “Well, actually, I must confess I am a bit, ehm, this is anonymous right? I am actually very lazy.” (patient nr. 9, quote nr. 12) | |
| Peers, experiences of peers | “The experiences of someone I know, who has also had cancer, breast cancer, she told me she stayed as active as she could and this helped her a lot. And she is about my age, a few years younger, so I thought: that is a valuable piece of advice. And that’s how I selected tips and advice from people around me every now and then.” (patient nr. 9, quote nr. 13) | |
| Experiences | ||
| Physical health benefits | “I am convinced that, ehm, that for my recovery and maybe also to prevent deterioration, exercising is simply very beneficial. That is sort of what I think.” (patient nr. 10, quote nr. 14) | |
| Health beliefs, attitude | “You are also just tired of being ill, so the things that are not absolutely necessary for your health or to survive… well… they can wait until tomorrow.” (patient nr. 5, quote nr. 15) | |
| Loss of self-control | “at one point I was extremely nauseated, I just did not perform the exercises anymore, I just couldn’t. But I did take it up again, one week later. But it did give me a bit of a scare, because I often don’t know my own boundaries, so I became scared and then I dropped out”. (patient nr. 12, quote nr. 16) | |
| Self-control | “And everything I can do to feel less like a patient and to speed up my recovery I will do! So I was quite motivated not to be discouraged and not to become a passive patient, but instead keeping self-control during the treatment trajectory as well as during the rehabilitation phase.” (patient nr. 14, quote nr. 17) | |
| Physical health benefits | “Sitting is the new smoking”, they say, and not without reason, so considering that, and especially in these extreme circumstances, it is just good to do it [exercising].” (patient nr. 9, quote nr. 18) | |
| Commitment to the study program | “I already intended to exercise, even if I would not have participated in this study, as I had said before. Anyway, I still would have planned to do something, so that was my motivation. And then it is just discipline, especially when you are not feeling well.” (patient nr. 10, quote nr. 19) | |
| Chemo dog, social support | “I deliberately borrowed a dog during my treatment, to arrange my physical activity routine.” (patient nr. 14, quote nr. 20) | |
| “Fortunately, I have little experience with cancer. This is the first time, but you just have no clue… There is so much coming at you, it is very difficult to predict whether it will be feasible [exercising]”. (patient nr. 2, quote nr. 21) | ||
| Exercise intervention | Expectations | |
| Content, unclear expectations | “… I don’t know what to expect, so maybe… I don’t know what we are going to do yet.” (patient nr. 6, quote nr. 22) | |
| Personalized intervention | “Yes well, I would assume that, when developing the program, you gave it some consideration that one should be able to keep it up”. (patient nr. 9, quote nr. 23) | |
| Experiences | ||
| Simplicity of the intervention, home-based | “The simplicity, that is of course the strength of this program, anyone can do it, you don’t have to go to the gym. You can just do it at home whenever you want. It is simple, and that, of course, is the strength of this program. Because, if you’re aiming for feasibility you should not add the constraint that one must go to the gym.” (patient nr. 10, quote nr. 24) | |
| Home-based, social support | “It took me a while to get into it (home-based exercises), because I’m not used to that, but later on I did it together with my wife. She also got one of those (resistance) bands, and then we did it together, she is really good at it”. (patient nr. 12, quote nr. 25) | |
| Supervision physiotherapist | Expectations | |
| Coaching, motivating | “Well a strong external incentive, I definitely need that, because I think I am rather lazy by nature.” (patient nr. 9, quote nr. 26) | |
| Coaching, performance | “By correcting me when I didn’t perform the exercises properly. You know, of course I did them once and I have seen those pictures, but the correct posture… that is hard. You tend to make it as easy on yourself as possible with those exercises, but you have to adopt the right posture that truly makes you put in the effort.” (patient nr. 5, quote nr. 27) | |
| Coaching, personal approach | “In any case, it offers me (ehm) a custom-fit solution to stay sportive, or at least physically active”. (patient nr. 14, quote nr. 28) | |
| Experiences | ||
| Personal approach, coaching | “That physiotherapist, yeah, I think she put too much pressure on me… to go, (ehm)… to the extreme… for me that works counterproductive”. (patient nr. 11, quote nr. 29) | |
| Clear instructions | “You can do the exercises in many different ways, and there was actually only one good way. The physiotherapist was always very pleased that I remembered the exercises well and performed them in the correct way.”(patient nr. 5, quote nr. 30) | |
| Personal approach, coaching | “Yes, I found it very stimulating, really empowering, (ehm) the physiotherapist was really driven, and you become aware of what your limits are, and what you can still do…”. (patient nr. 12, quote nr. 31) | |
| “I think it is truly fantastic! Very well done, inspired, and the physiotherapist is of course a wonderful person, but also the way she presented it and made it attractive by stimulating me, yeah, that is really the way to get someone moving”. (patient nr. 12, quote nr. 32) |
| Suggestions for Improvement | Exemplary Quotes |
|---|---|
| Exercise videos | “What might be helpful,… you know, I had to do 6 different exercises… and if there were like 6 YouTube videos with exactly those exercises”. (patient nr. 5, quote nr. 33) |
| Supervised training near home | “I think, yeah, if a physiotherapist had visited me at home, I probably would have done those exercises”. (patient nr. 6, quote nr. 34) |
| Hospital-based training | “During hospital stay, I really liked it, but at home there was so much going on, too many distractions, and all the hassle with medication, tube feeding, that made it impossible to also do it (the exercises) on top of all that”. (patient nr. 5, quote nr. 35) |
| Exercise in peer group | “I think it is better (to exercise) in a group”. (patient nr. 4, quote nr. 36) |
| Personalized training program | “Consider each individuals’ own personal needs. I had a need for a more intensive program and with that, I would have liked the freedom to adjust the exercises when it’s not going well on occasion”. (patient nr. 10, quote nr. 37) |
| Health/exercise tracking apps | “To be honest, I didn’t find the fitbit very convenient,… I think it would be better to use your smartphone for tracking, because you always have it on you,… you know. I change my trousers before leaving the house and then the fitbit was still attached to the house pair…”. (patient nr. 5, quote nr. 38) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kok, A.; Passchier, E.; May, A.M.; Jager-Wittenaar, H.; Veenhof, C.; de Bree, R.; Stuiver, M.M.; Speksnijder, C.M. Expectations and Experiences of Participating in a Supervised and Home-Based Physical Exercise Intervention in Patients with Head and Neck Cancer during Chemoradiotherapy: A Qualitative Study. Curr. Oncol. 2024, 31, 885-899. https://doi.org/10.3390/curroncol31020066
Kok A, Passchier E, May AM, Jager-Wittenaar H, Veenhof C, de Bree R, Stuiver MM, Speksnijder CM. Expectations and Experiences of Participating in a Supervised and Home-Based Physical Exercise Intervention in Patients with Head and Neck Cancer during Chemoradiotherapy: A Qualitative Study. Current Oncology. 2024; 31(2):885-899. https://doi.org/10.3390/curroncol31020066
Chicago/Turabian StyleKok, Annemieke, Ellen Passchier, Anne M. May, Harriët Jager-Wittenaar, Cindy Veenhof, Remco de Bree, Martijn M. Stuiver, and Caroline M. Speksnijder. 2024. "Expectations and Experiences of Participating in a Supervised and Home-Based Physical Exercise Intervention in Patients with Head and Neck Cancer during Chemoradiotherapy: A Qualitative Study" Current Oncology 31, no. 2: 885-899. https://doi.org/10.3390/curroncol31020066
APA StyleKok, A., Passchier, E., May, A. M., Jager-Wittenaar, H., Veenhof, C., de Bree, R., Stuiver, M. M., & Speksnijder, C. M. (2024). Expectations and Experiences of Participating in a Supervised and Home-Based Physical Exercise Intervention in Patients with Head and Neck Cancer during Chemoradiotherapy: A Qualitative Study. Current Oncology, 31(2), 885-899. https://doi.org/10.3390/curroncol31020066






