Combination of Immunotherapy and Radiation Therapy in Gastrointestinal Cancers: An Appraisal of the Current Literature and Ongoing Research
Abstract
1. Introduction
2. Mechanism of Radiation in Combination with Immune Checkpoint Inhibitors
3. Gastroesophageal Cancer
3.1. Phase I/II Studies
3.2. Retrospective Studies
3.3. Phase III Study
3.4. Ongoing Studies
4. Hepatocellular Carcinoma (HCC)
4.1. ICI alone Studies in HCC
4.2. RT with TKI in HCC
4.3. RT with ICI in HCC: Phase I Study
4.4. RT with ICI in HCC: Retrospective Data
4.5. RT with ICI in HCC: Ongoing Studies
4.6. TARE with ICI in HCC
5. Cholangiocarcinoma (CCA)
5.1. ICI in Advanced CCA
5.2. RT with ICI in CCA: Phase II Studies
6. Pancreatic Cancer
6.1. RT with ICI in RPC and BRPC
6.2. RT with ICI in LAPC
7. Colorectal Cancer
7.1. ICI alone in CRC: Phase II Studies
7.2. RT with ICI in CRC: Phase I/II Studies
7.3. RT with ICI in CRC: Ongoing Studies
8. Anal Cancer
9. Limitations
10. Conclusions
Author Contributions
Funding
Informed Consent Statement
Conflicts of Interest
References
- Lu, L.; Mullins, C.S.; Schafmayer, C.; Zeißig, S.; Linnebacher, M. A global assessment of recent trends in gastrointestinal cancer and lifestyle-associated risk factors. Cancer Commun. 2021, 41, 1137–1151. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics, 2022. CA Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef] [PubMed]
- Kraehenbuehl, L.; Weng, C.-H.; Eghbali, S.; Wolchok, J.D.; Merghoub, T. Enhancing immunotherapy in cancer by targeting emerging immunomodulatory pathways. Nat. Rev. Clin. Oncol. 2022, 19, 37–50. [Google Scholar] [CrossRef] [PubMed]
- Ribas, A.; Wolchok, J.D. Cancer immunotherapy using checkpoint blockade. Science 2018, 359, 1350–1355. [Google Scholar] [CrossRef] [PubMed]
- Seidel, J.A.; Otsuka, A.; Kabashima, K. Anti-PD-1 and Anti-CTLA-4 Therapies in Cancer: Mechanisms of Action, Efficacy, and Limitations. Front. Oncol. 2018, 8, 86. [Google Scholar] [CrossRef]
- Burnette, B.; Weichselbaum, R.R. Radiation as an immune modulator. Semin. Radiat. Oncol. 2013, 23, 273–280. [Google Scholar] [CrossRef]
- Park, B.; Yee, C.; Lee, K.-M. The effect of radiation on the immune response to cancers. Int. J. Mol. Sci. 2014, 15, 927–943. [Google Scholar] [CrossRef]
- Van Limbergen, E.J.; De Ruysscher, D.K.; Olivo Pimentel, V.; Marcus, D.; Berbee, M.; Hoeben, A.; Rekers, N.; Theys, J.; Yaromina, A.; Dubois, L.J.; et al. Combining radiotherapy with immunotherapy: The past, the present and the future. Br. J. Radiol. 2017, 90, 20170157. [Google Scholar] [CrossRef]
- Gupta, A.; Probst, H.C.; Vuong, V.; Landshammer, A.; Muth, S.; Yagita, H.; Schwendener, R.; Pruschy, M.; Knuth, A.; van den Broek, M. Radiotherapy promotes tumor-specific effector CD8+ T cells via dendritic cell activation. J. Immunol. 2012, 189, 558–566. [Google Scholar] [CrossRef]
- Wang, Y.; Deng, W.; Li, N.; Neri, S.; Sharma, A.; Jiang, W.; Lin, S.H. Combining Immunotherapy and Radiotherapy for Cancer Treatment: Current Challenges and Future Directions. Front. Pharmacol. 2018, 9, 185. [Google Scholar] [CrossRef]
- Sharabi, A.B.; Lim, M.; DeWeese, T.L.; Drake, C.G. Radiation and checkpoint blockade immunotherapy: Radiosensitisation and potential mechanisms of synergy. Lancet Oncol. 2015, 16, e498–e509. [Google Scholar] [CrossRef] [PubMed]
- Sharabi, A.B.; Nirschl, C.J.; Kochel, C.M.; Nirschl, T.R.; Francica, B.J.; Velarde, E.; Deweese, T.L.; Drake, C.G. Stereotactic Radiation Therapy Augments Antigen-Specific PD-1-Mediated Antitumor Immune Responses via Cross-Presentation of Tumor Antigen. Cancer Immunol. Res. 2015, 3, 345–355. [Google Scholar] [CrossRef] [PubMed]
- Germino, E.A.; Govindarajan, A.; Sedrak, M.S.; Li, D.; Amini, A. Multimodality Treatment with Radiotherapy and Immunotherapy in Older Adults: Rationale, Evolving Data, and Current Recommendations. Semin. Radiat. Oncol. 2022, 32, 142–154. [Google Scholar] [CrossRef] [PubMed]
- Pointer, K.B.; Pitroda, S.P.; Weichselbaum, R.R. Radiotherapy and immunotherapy: Open questions and future strategies. Trends Cancer 2022, 8, 9–20. [Google Scholar] [CrossRef]
- Badiyan, S.; Kaiser, A.; Eastman, B.; Forsthoefel, M.; Zeng, J.; Unger, K.; Chuong, M. Immunotherapy and radiation therapy for gastrointestinal malignancies: Hope or hype? Transl. Gastroenterol. Hepatol. 2020, 5, 21. [Google Scholar] [CrossRef]
- Oh, P.; Du, K.L.; Leichman, L.; Aifantis, I. PD-1 Blockade Enhances the Efficacy of Chemoradiation in a Mouse Model of Esophageal Cancer. Int. J. Radiat. Oncol. Biol. Phys. 2016, 96, S127–S128. [Google Scholar] [CrossRef]
- Hong, S.; Bi, M.; Yu, H.; Yan, Z.; Wang, H. Radiation therapy enhanced therapeutic efficacy of anti-PD1 against gastric cancer. J. Radiat. Res. 2020, 61, 851–859. [Google Scholar] [CrossRef]
- Zhang, W.; Yan, C.; Gao, X.; Li, X.; Cao, F.; Zhao, G.; Zhao, J.; Er, P.; Zhang, T.; Chen, X.; et al. Safety and Feasibility of Radiotherapy Plus Camrelizumab for Locally Advanced Esophageal Squamous Cell Carcinoma. Oncologist 2021, 26, e1110–e1124. [Google Scholar] [CrossRef]
- Uboha, N.V.; Eickhoff, J.C.; Maloney, J.D.; McCarthy, D.; DeCamp, M.; Deming, D.A.; LoConte, N.K.; Matkowskyj, K.A.; Patel, M.A.; Hurst, N.; et al. Phase I/II trial of perioperative avelumab in combination with chemoradiation (CRT) in the treatment of stage II/III resectable esophageal and gastroesophageal junction (E/GEJ) cancer. J. Clin. Oncol. 2022, 40, 4034. [Google Scholar] [CrossRef]
- Zhu, M.; Chen, C.; Foster, N.R.; Hartley, C.; Mounajjed, T.; Salomao, M.A.; Fruth, B.F.; Beamer, S.E.; Kim, Y.; Harrington, S.M.; et al. Pembrolizumab in Combination with Neoadjuvant Chemoradiotherapy for Patients with Resectable Adenocarcinoma of the Gastroesophageal Junction. Clin. Cancer Res. 2022, 28, 3021–3031. [Google Scholar] [CrossRef]
- van den Ende, T.; de Clercq, N.C.; van Berge Henegouwen, M.I.; Gisbertz, S.S.; Geijsen, E.D.; Verhoeven, R.H.A.; Meijer, S.L.; Schokker, S.; Dings, M.P.G.; Bergman, J.J.G.H.M.; et al. Neoadjuvant Chemoradiotherapy Combined with Atezolizumab for Resectable Esophageal Adenocarcinoma: A Single-arm Phase II Feasibility Trial (PERFECT). Clin. Cancer Res. 2021, 27, 3351–3359. [Google Scholar] [CrossRef]
- Wang, J.; Cheng, Y.; Wu, Y.; Cao, F.; Liu, Q.; Gao, G. Efficacy and safety of consolidative camrelizumab following definitive concurrent chemoradiotherapy in patients with locally advanced esophageal squamous cell cancer. Ann. Oncol. 2022, 33, S1124. [Google Scholar] [CrossRef]
- Wei, T.; Ti, W.; Song, Q.; Cheng, Y. Study of PD-1 Inhibitors in Combination with Chemoradiotherapy/Chemotherapy in Patients with Esophageal Squamous Carcinoma. Curr. Oncol. 2022, 29, 2920–2927. [Google Scholar] [CrossRef]
- Nie, Y.; Yao, G.; Li, L.; Feng, A.; Zhang, W.; Xu, X.; Li, Q.; Yang, Z. Effects of Radiotherapy on Survival of Esophageal Cancer Patients Receiving Immunotherapy: Propensity Score Analysis and Nomogram Construction. Cancer Manag. Res. 2022, 14, 2357–2371. [Google Scholar] [CrossRef]
- Peng, F.; Lian, H.M.; Niu, S.Q.; Liufu, W.J.; Yu, T.T.; Bao, Y. Induction Anti-PD-1 Immunotherapy plus Chemotherapy Followed by Definitive Chemoradiation Therapy in Locally Advanced Esophageal Squamous Cell Carcinoma: A Real-World Retrospective Study. Int. J. Radiat. Oncol. Biol. Phys. 2022, 114, e165. [Google Scholar] [CrossRef]
- Kelly, R.J.; Ajani, J.A.; Kuzdzal, J.; Zander, T.; Van Cutsem, E.; Piessen, G.; Mendez, G.; Feliciano, J.; Motoyama, S.; Lièvre, A.; et al. Adjuvant Nivolumab in Resected Esophageal or Gastroesophageal Junction Cancer. N. Engl. J. Med. 2021, 384, 1191–1203. [Google Scholar] [CrossRef]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Benson, A.B.; D’Angelica, M.I.; Abbott, D.E.; Anaya, D.A.; Anders, R.; Are, C.; Bachini, M.; Borad, M.; Brown, D.; Burgoyne, A.; et al. Hepatobiliary Cancers, Version 2.2021, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2021, 19, 541–565. [Google Scholar] [CrossRef] [PubMed]
- Sayan, M.; Yegya-Raman, N.; Greco, S.H.; Gui, B.; Zhang, A.; Chundury, A.; Grandhi, M.S.; Hochster, H.S.; Kennedy, T.J.; Langan, R.C.; et al. Rethinking the Role of Radiation Therapy in the Treatment of Unresectable Hepatocellular Carcinoma: A Data Driven Treatment Algorithm for Optimizing Outcomes. Front. Oncol. 2019, 9, 345. [Google Scholar] [CrossRef]
- Falette Puisieux, M.; Pellat, A.; Assaf, A.; Ginestet, C.; Brezault, C.; Dhooge, M.; Soyer, P.; Coriat, R. Therapeutic Management of Advanced Hepatocellular Carcinoma: An Updated Review. Cancers 2022, 14, 2357. [Google Scholar] [CrossRef]
- Finn, R.S.; Qin, S.; Ikeda, M.; Galle, P.R.; Ducreux, M.; Kim, T.-Y.; Kudo, M.; Breder, V.; Merle, P.; Kaseb, A.O.; et al. Atezolizumab plus Bevacizumab in Unresectable Hepatocellular Carcinoma. N. Engl. J. Med. 2020, 382, 1894–1905. [Google Scholar] [CrossRef] [PubMed]
- Abou-Alfa, G.K.; Lau, G.; Kudo, M.; Chan, S.L.; Kelley, R.K.; Furuse, J.; Sukeepaisarnjaroen, W.; Kang, Y.-K.; Van Dao, T.; De Toni, E.N.; et al. Tremelimumab plus Durvalumab in Unresectable Hepatocellular Carcinoma. NEJM Evid. 2022, 1, EVIDoa2100070. [Google Scholar] [CrossRef]
- Dawson, L.A.; Winter, K.; Knox, J.; Zhu, A.X.; Krishnan, S.; Guha, C.; Kachnic, L.A.; Gillin, M.T.; Hong, T.S.; Craig, T.; et al. NRG/RTOG 1112: Randomized Phase III Study of Sorafenib vs. Stereotactic Body Radiation Therapy (SBRT) Followed by Sorafenib in Hepatocellular Carcinoma (HCC) (NCT01730937). Int. J. Radiat. Oncol. Biol. Phys. 2022, 114, 1057. [Google Scholar] [CrossRef]
- Juloori, A.; Katipally, R.R.; Lemons, J.M.; Singh, A.K.; Iyer, R.; Robbins, J.R.; George, B.; Hall, W.A.; Pitroda, S.P.; Arif, F.; et al. Phase 1 Randomized Trial of Stereotactic Body Radiation Therapy Followed by Nivolumab plus Ipilimumab or Nivolumab Alone in Advanced/Unresectable Hepatocellular Carcinoma. Int. J. Radiat. Oncol. Biol. Phys. 2023, 115, 202–213. [Google Scholar] [CrossRef]
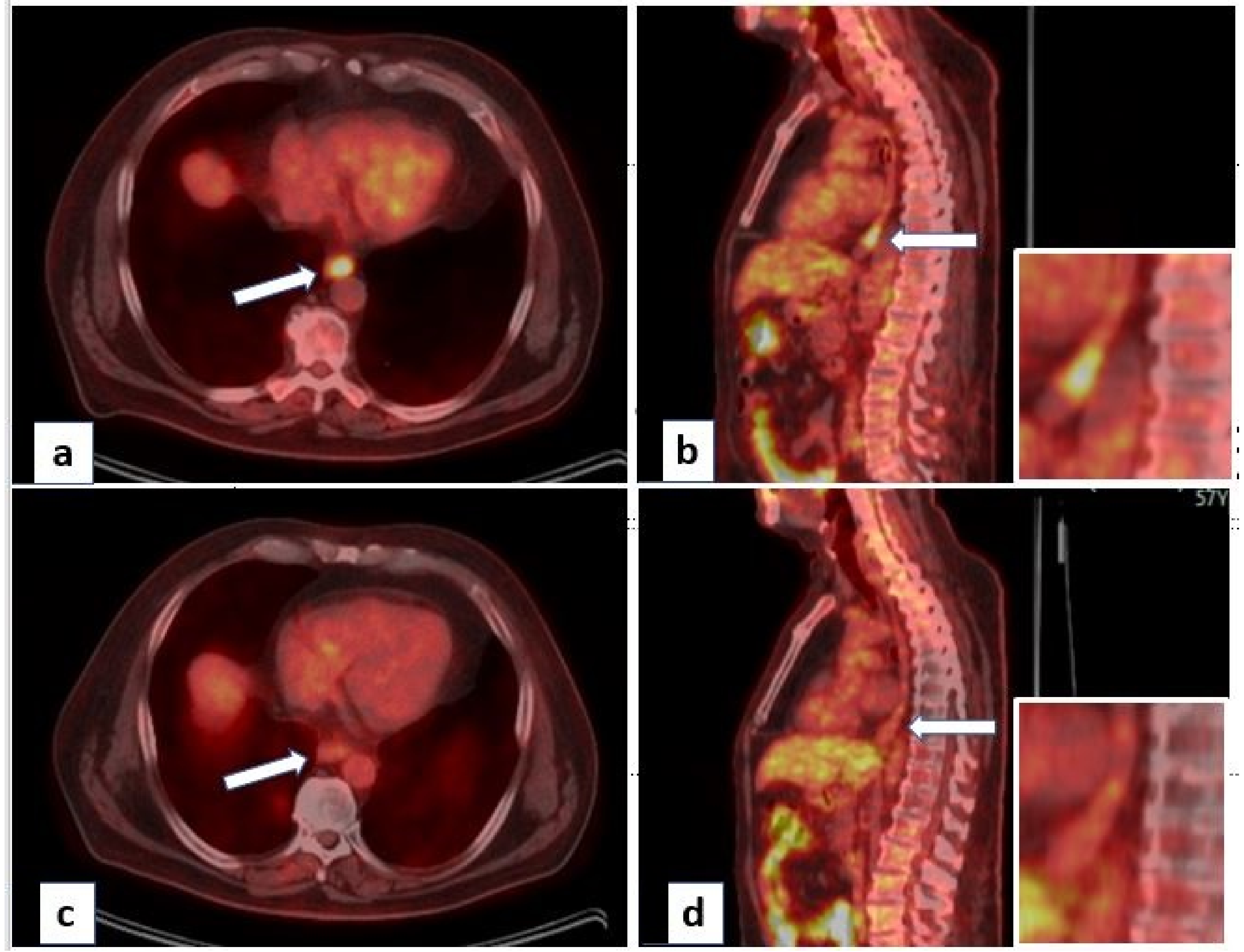
- Chiang, C.-L.; Chan, A.C.Y.; Chiu, K.W.H.; Kong, F.-M.S. Combined Stereotactic Body Radiotherapy and Checkpoint Inhibition in Unresectable Hepatocellular Carcinoma: A Potential Synergistic Treatment Strategy. Front. Oncol. 2019, 9, 1157. [Google Scholar] [CrossRef]
- Chiang, C.L.; Chan, A.C.Y.; Chiu, W.H.K.; Kong, F.M. Combined Stereotactic Body Radiotherapy and Immunotherapy (SBRT-IO) vs. TACE in Locally Advanced Hepatocellular Carcinoma (HCC): Propensity Score Matching Analysis. Int. J. Radiat. Oncol. Biol. Phys. 2021, 111, e35–e36. [Google Scholar] [CrossRef]
- Chew, V.; Lee, Y.H.; Pan, L.; Nasir, N.J.M.; Lim, C.J.; Chua, C.; Lai, L.; Hazirah, S.N.; Lim, T.K.H.; Goh, B.K.P.; et al. Immune activation underlies a sustained clinical response to Yttrium-90 radioembolisation in hepatocellular carcinoma. Gut 2019, 68, 335–346. [Google Scholar] [CrossRef]
- Rivoltini, L.; Bhoori, S.; Camisaschi, C.; Bergamaschi, L.; Lalli, L.; Frati, P.; Citterio, D.; Castelli, C.; Mazzaferro, V. Y90-radioembolisation in hepatocellular carcinoma induces immune responses calling for early treatment with multiple checkpoint blockers. Gut 2023, 72, 406–407. [Google Scholar] [CrossRef]
- de la Torre-Aláez, M.; Matilla, A.; Varela, M.; Iñarrairaegui, M.; Reig, M.; Lledó, J.L.; Arenas, J.I.; Lorente, S.; Testillano, M.; Márquez, L.; et al. Nivolumab after selective internal radiation therapy for the treatment of hepatocellular carcinoma: A phase 2, single-arm study. J. Immunother. Cancer 2022, 10, e005457. [Google Scholar] [CrossRef]
- Tai, D.; Loke, K.; Gogna, A.; Kaya, N.A.; Tan, S.H.; Hennedige, T.; Ng, D.; Irani, F.; Lee, J.; Lim, J.Q.; et al. Radioembolisation with Y90-resin microspheres followed by nivolumab for advanced hepatocellular carcinoma (CA 209-678): A single arm, single centre, phase 2 trial. Lancet Gastroenterol. Hepatol. 2021, 6, 1025–1035. [Google Scholar] [CrossRef]
- Gkika, E.; Hawkins, M.A.; Grosu, A.-L.; Brunner, T.B. The Evolving Role of Radiation Therapy in the Treatment of Biliary Tract Cancer. Front. Oncol. 2020, 10, 604387. [Google Scholar] [CrossRef]
- Ben-Josef, E.; Guthrie, K.A.; El-Khoueiry, A.B.; Corless, C.L.; Zalupski, M.M.; Lowy, A.M.; Thomas, C.R.; Alberts, S.R.; Dawson, L.A.; Micetich, K.C.; et al. SWOG S0809: A Phase II Intergroup Trial of Adjuvant Capecitabine and Gemcitabine Followed by Radiotherapy and Concurrent Capecitabine in Extrahepatic Cholangiocarcinoma and Gallbladder Carcinoma. J. Clin. Oncol. 2015, 33, 2617–2622. [Google Scholar] [CrossRef] [PubMed]
- Oh, D.-Y.; Ruth He, A.; Qin, S.; Chen, L.-T.; Okusaka, T.; Vogel, A.; Kim, J.W.; Suksombooncharoen, T.; Ah Lee, M.; Kitano, M.; et al. Durvalumab plus Gemcitabine and Cisplatin in Advanced Biliary Tract Cancer. NEJM Evid. 2022, 1, EVIDoa2200015. [Google Scholar] [CrossRef]
- Liu, X.; Yao, J.; Song, L.; Zhang, S.; Huang, T.; Li, Y. Local and abscopal responses in advanced intrahepatic cholangiocarcinoma with low TMB, MSS, pMMR and negative PD-L1 expression following combined therapy of SBRT with PD-1 blockade. J. Immunother. Cancer 2019, 7, 204. [Google Scholar] [CrossRef]
- Zhao, Q.; Chen, Y.; Du, S.; Yang, X.; Chen, Y.; Ji, Y.; Zeng, Z. Integration of radiotherapy with anti-PD-1 antibody for the treatment of intrahepatic or hilar cholangiocarcinoma: Reflection from four cases. Cancer Biol. Ther. 2021, 22, 175–183. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, S.A.; Duong, M.; Sohal, D.P.S.; Gandhi, N.S.; Beg, M.S.; Wang-Gillam, A.; Wade, J.L.; Chiorean, E.G.; Guthrie, K.A.; Lowy, A.M.; et al. Surgical Outcome Results from SWOG S1505: A Randomized Clinical Trial of mFOLFIRINOX Versus Gemcitabine/Nab-paclitaxel for Perioperative Treatment of Resectable Pancreatic Ductal Adenocarcinoma. Ann. Surg. 2020, 272, 481–486. [Google Scholar] [CrossRef] [PubMed]
- Versteijne, E.; Suker, M.; Groothuis, K.; Akkermans-Vogelaar, J.M.; Besselink, M.G.; Bonsing, B.A.; Buijsen, J.; Busch, O.R.; Creemers, G.-J.M.; van Dam, R.M.; et al. Preoperative Chemoradiotherapy Versus Immediate Surgery for Resectable and Borderline Resectable Pancreatic Cancer: Results of the Dutch Randomized Phase III PREOPANC Trial. J. Clin. Oncol. 2020, 38, 1763–1773. [Google Scholar] [CrossRef]
- Rahma, O.; Katz, M.; Bauer, T.; Wolpin, B.; Stucky, C.-C.; Bekaii-Saab, T.; Elias, R.; Dias-Costa, A.; Nowak, J.; Patrick, L.; et al. Randomized multicenter study of neoadjuvant chemoradiation therapy (CRT) alone or in combination with pembrolizumab in patients with resectable or borderline resectable pancreatic cancer. J. Immunother. Cancer 2021, 9, A1010. [Google Scholar] [CrossRef]
- Zhu, X.; Cao, Y.; Liu, W.; Ju, X.; Zhao, X.; Jiang, L.; Ye, Y.; Jin, G.; Zhang, H. Stereotactic body radiotherapy plus pembrolizumab and trametinib versus stereotactic body radiotherapy plus gemcitabine for locally recurrent pancreatic cancer after surgical resection: An open-label, randomised, controlled, phase 2 trial. Lancet Oncol. 2022, 23, e105–e115. [Google Scholar] [CrossRef]
- Koopman, M.; Kortman, G.a.M.; Mekenkamp, L.; Ligtenberg, M.J.L.; Hoogerbrugge, N.; Antonini, N.F.; Punt, C.J.A.; van Krieken, J.H.J.M. Deficient mismatch repair system in patients with sporadic advanced colorectal cancer. Br. J. Cancer 2009, 100, 266–273. [Google Scholar] [CrossRef]
- Lumish, M.A.; Cercek, A. Immunotherapy for the treatment of colorectal cancer. J. Surg. Oncol. 2021, 123, 760–774. [Google Scholar] [CrossRef]
- Lenz, H.-J.; Van Cutsem, E.; Luisa Limon, M.; Wong, K.Y.M.; Hendlisz, A.; Aglietta, M.; García-Alfonso, P.; Neyns, B.; Luppi, G.; Cardin, D.B.; et al. First-Line Nivolumab Plus Low-Dose Ipilimumab for Microsatellite Instability-High/Mismatch Repair-Deficient Metastatic Colorectal Cancer: The Phase II CheckMate 142 Study. J. Clin. Oncol. 2022, 40, 161–170. [Google Scholar] [CrossRef]
- Diaz, L.A.; Shiu, K.-K.; Kim, T.-W.; Jensen, B.V.; Jensen, L.H.; Punt, C.; Smith, D.; Garcia-Carbonero, R.; Benavides, M.; Gibbs, P.; et al. Pembrolizumab versus chemotherapy for microsatellite instability-high or mismatch repair-deficient metastatic colorectal cancer (KEYNOTE-177): Final analysis of a randomised, open-label, phase 3 study. Lancet Oncol. 2022, 23, 659–670. [Google Scholar] [CrossRef] [PubMed]
- Chalabi, M.; Fanchi, L.F.; Dijkstra, K.K.; Van den Berg, J.G.; Aalbers, A.G.; Sikorska, K.; Lopez-Yurda, M.; Grootscholten, C.; Beets, G.L.; Snaebjornsson, P.; et al. Neoadjuvant immunotherapy leads to pathological responses in MMR-proficient and MMR-deficient early-stage colon cancers. Nat. Med. 2020, 26, 566–576. [Google Scholar] [CrossRef]
- Chalabi, M.; Verschoor, Y.L.; van den Berg, J.; Sikorska, K.; Beets, G.; Lent, A.V.; Grootscholten, M.C.; Aalbers, A.; Buller, N.; Marsman, H.; et al. LBA7 Neoadjuvant immune checkpoint inhibition in locally advanced MMR-deficient colon cancer: The NICHE-2 study. Ann. Oncol. 2022, 33, S1389. [Google Scholar] [CrossRef]
- Cercek, A.; Lumish, M.; Sinopoli, J.; Weiss, J.; Shia, J.; Lamendola-Essel, M.; El Dika, I.H.; Segal, N.; Shcherba, M.; Sugarman, R.; et al. PD-1 Blockade in Mismatch Repair-Deficient, Locally Advanced Rectal Cancer. N. Engl. J. Med. 2022, 386, 2363–2376. [Google Scholar] [CrossRef]
- Deng, L.; Liang, H.; Burnette, B.; Beckett, M.; Darga, T.; Weichselbaum, R.R.; Fu, Y.-X. Irradiation and anti-PD-L1 treatment synergistically promote antitumor immunity in mice. J. Clin. Investig. 2014, 124, 687–695. [Google Scholar] [CrossRef] [PubMed]
- Dovedi, S.J.; Adlard, A.L.; Lipowska-Bhalla, G.; McKenna, C.; Jones, S.; Cheadle, E.J.; Stratford, I.J.; Poon, E.; Morrow, M.; Stewart, R.; et al. Acquired resistance to fractionated radiotherapy can be overcome by concurrent PD-L1 blockade. Cancer Res. 2014, 74, 5458–5468. [Google Scholar] [CrossRef]
- Yoshino, T.; Bando, H.; Tsukada, Y.; Inamori, K.; Yuki, S.; Komatsu, Y.; Homma, S.; Uemura, M.; Kato, T.; Kotani, D.; et al. Voltage: Investigator-initiated clinical trial of nivolumab monotherapy and subsequent radical surgery following preoperative chemoradiotherapy in patients with microsatellite stable locally advanced rectal cancer. J. Clin. Oncol. 2019, 37, 3606. [Google Scholar] [CrossRef]
- George, T.J.; Yothers, G.; Rahma, O.E.; Hong, T.S.; Russell, M.M.; You, Y.N.; Parker, W.; Jacobs, S.A.; Lucas, P.C.; Colangelo, L.H.; et al. Long-term results from NRG-GI002: A phase II clinical trial platform using total neoadjuvant therapy (TNT) in locally advanced rectal cancer (LARC). J. Clin. Oncol. 2023, 41, 7. [Google Scholar] [CrossRef]
- Eng, C.; Ciombor, K.K.; Cho, M.; Dorth, J.A.; Rajdev, L.N.; Horowitz, D.P.; Gollub, M.J.; Jácome, A.A.; Lockney, N.A.; Muldoon, R.L.; et al. Anal Cancer: Emerging Standards in a Rare Disease. J. Clin. Oncol. 2022, 40, 2774–2788. [Google Scholar] [CrossRef] [PubMed]
- Morris, V.K.; Salem, M.E.; Nimeiri, H.; Iqbal, S.; Singh, P.; Ciombor, K.; Polite, B.; Deming, D.; Chan, E.; Wade, J.L.; et al. Nivolumab for previously treated unresectable metastatic anal cancer (NCI9673): A multicentre, single-arm, phase 2 study. Lancet Oncol. 2017, 18, 446–453. [Google Scholar] [CrossRef] [PubMed]
- Marabelle, A.; Cassier, P.A.; Fakih, M.; Kao, S.; Nielsen, D.; Italiano, A.; Guren, T.K.; van Dongen, M.G.J.; Spencer, K.; Bariani, G.M.; et al. Pembrolizumab for previously treated advanced anal squamous cell carcinoma: Results from the non-randomised, multicohort, multicentre, phase 2 KEYNOTE-158 study. Lancet Gastroenterol. Hepatol. 2022, 7, 446–454. [Google Scholar] [CrossRef] [PubMed]
| Author/Study | Type of Study | Number (n) | Disease Status | ICI | Intervention | Results |
|---|---|---|---|---|---|---|
| Zhang [18] | Phase 1b | 19 | Locally advanced | Camrelizumab | RT-ICI f/b ICI | PFS 11.7 months OS 16.7 months |
| Zhu [20] | Phase 1/2 | 31 | Resectable (Stage II/III) | Pembrolizumab | CRT-ICI f/b Surgery f/b adjuvant ICI | pCR in 22.6% |
| PERFECT [21] | Phase 2 | 40 | Resectable | Atezolizumab | CRT-ICI f/b Surgery | pCR in 25% |
| Wang [22] | Phase 2 | 12 | Locally advanced | Camrelizumab | Definitive CRT f/b consolidative ICI (n = 12) | 11/12 patients had SD |
| Wie [23] | Retrospective | 55 | Inoperable | Camrelizumab Tislelizumab Sintilimab | CRT-ICI (n = 26) CRT alone (n = 29) | Improved OS with CRT-ICI |
| Nie [24] | Retrospective | 134 | Locally advanced | Carmelizumab Pembrolizumab | CHT-ICI f/b RT (n = 55) CHT-ICI (n = 79) | PFS (15.7 vs. 5.7 m) OS (15.7 vs. 12 m) |
| Peng [25] | Retrospective | 62 | Locally advanced | ---- | CHT-ICI f/b definitive CRT | PFS 28.8 months |
| CheckMate 577 [26] | Phase 3 | 794 | Resectable | Nivolumab | NA-CRT f/b Surgery +/−adjuvant ICI (n = 532 vs. 262) | DFS 24.4 vs. 11 months |
| NCT Number | Interventions | Primary Outcome | Phase |
|---|---|---|---|
| NCT05650216 | Camrelizumab + CRT | Safety, pCR | 2 |
| NCT05043688 | Camrelizumab + CRT | pCR | 2 |
| NCT04229459 | Nivolumab + CRT | pCR | 2 |
| NCT03777813 | Durvalumab +CRT vs. CRT | PFS | 2 |
| NCT05520619 | Tislelizumab + CRT | PFS | 2 |
| NCT05387681 | Envafolimab + CRT | pCR | 2 |
| NCT04929392 | Pembrolizumab + CRT | pCR | 2 |
| NCT04888403 | Toripalimab + CRT | pCR | 2 |
| NCT03257163 | Pembrolizumab → Surgery → adj CHT and CRT with Pembrolizumab | DFS | 2 |
| NCT04973306 | Tislelizumab + CRT vs. CRT | pCR, OS | 2, 3 |
| NCT03604991 | Pre-op Nivolumab + CRT vs. Pre-op CRT with post-surgery adjuvant (Nivo vs. Nivo/Ipi) | pCR, DFS, OS | 3 |
| NCT04404491 | Camrelizumab + RT vs. RT + CHT | AE, PFS | 3 |
| NCT04821843 | Nimotuzumab + CRT vs. Nimotuzumab + CHT | OS | 3 |
| NCT04821778 | Nimotuzumab + CRT vs. CRT | OS | 3 |
| NCT05244798 | Sintilimab + CHT vs. Sintilimab + CRT vs. CRT | pCR | 3 |
| NCT04807673 | Pembrolizumab + CRT | Event-Free Survival (EFS) | 3 |
| Author | Type of Study | Patient Characteristics | Intervention | Results |
|---|---|---|---|---|
| Chiang [35] | Case series | N = 5 Unresectable HCC | SBRT + Nivolumab | CR: 2/5 PR: 3/5 |
| Chiang [36] | Retrospective | N = 16 | SBRT + Nivolumab | CR: 50% PR: 37.5% |
| Juloori [34] | Prospective Phase 1 RCT | N = 14 | SBRT + Nivolumab (n = 6) | PR—12.5% SD—37.5% PD—50% |
| SBRT + Ipilimumab + nivolumab (n = 8) | PR—50% SD—37.5% PD—12.5% |
| NCT Number | Interventions | Outcome Measures | Phase |
|---|---|---|---|
| NCT05488522 | SBRT + atezolizumab and bevacizumab | PFS | 1 |
| NCT03817736 | TACE followed by SBRT followed by Avelumab | Response Rate/Amenable to surgery | 2 |
| NCT04913480 | SBRT + Durvalumab (1 yr) | PFS | 2 |
| NCT04988945 | TACE followed by SBRT followed by Durvalumab + Tremelimumab | Response Rate/Amenable to surgery | 2 |
| NCT04611165 | Hypofractionated radiation (10 fractions) + Nivolumab | PFS | 2 |
| NCT04430452 | Hypofractionated radiation + Durvalumab +/− Tremelimumab | Response Rate | 2 |
| NCT03316872 | SBRT + Pembrolizumab | Response Rate | 2 |
| NCT05366829 | RT + Tislelizumab | PFS | 2 |
| NCT04167293 | SBRT + Sintilimab | PFS | 2/3 |
| NCT Number | Interventions | Outcome Measures | Phase |
|---|---|---|---|
| NCT04708067 | RT + Bintrafusp Alfa | Response | 1 |
| NCT04866836 | RT + Tislelizumab | Response | 2 |
| NCT03898895 (CORRECT) | RT + Camrelizumab | PFS | 2 |
| NCT Number | Disease Status | Interventions | Outcome Measures | Phase |
|---|---|---|---|---|
| NCT04098432 | Locally Advanced Unresectable Pancreatic Adenocarcinoma | SBRT + Nivolumab | Safety | 1/2 |
| NCT04247165 | Pancreatic Cancer | SBRT + Ipilimumab + Nivolumab | PFS | 1/2 |
| NCT04390399 | Locally Advanced or Metastatic Pancreatic Cancer | SBRT + Chemo +/− IT | PFS/ORR | 2 |
| NCT04361162 | MSS Pancreatic Cancer | RT + Nivolumab + Ipilimumab | ORR | 2 |
| NCT03563248 | Localized Pancreatic Cancer | FOLFIRINOX + SBRT + Surgery +/− Nivolumab +/− Losartan | R0 Resection | 2 |
| NCT05116917 | Pancreatic Cancer | SBRT + Nivolumab + Influenza Vaccine | ORR | 2 |
| NCT03161379 | Borderline Resectable Pancreatic Cancer | SBRT + Nivolumab + GVAX Pancreas Vaccine | ORR | 2 |
| NCT Number | Phase | Stage | ARM | Interventions | Outcome Measures |
|---|---|---|---|---|---|
| NCT03127007 (R-IMMUNE) | Phase 1/2 | LARC | A | LC CRT + Atezolizumab → TME | AE, pCR |
| B | LC CRT → TME | ||||
| NCT02948348 | Phase 1/2 | LARC | -- | LC CRT + Nivo → TME | pCR |
| NCT05245474 | Phase 2 | LARC | A | LC CRT + Concurrent Tislelizumab → TME | pCR |
| B | LC CRT + Sequential Tislelizumab → TME | ||||
| C | LC CRT → TME | ||||
| NCT05576480 | Phase 2 | LARC | -- | SCRT → Penpulimab + CAPEOX → TME | pCR |
| NCT05086627 | Phase 2 | LARC | A | SCRT → Tislelizumab + CAPEOX → TME → CAPEOX | pCR |
| B | SCRT → CAPEOX → TME → CAPEOX | ||||
| NCT04621370 (PRIME-RT) | Phase 2 | LARC | A | SCRT + Durvalumab → FOLFOX | pCR, cCR |
| B | LCRT + Durvalumab → FOLFOX | ||||
| NCT05507112 | Phase 2 | LARC | A | LC CRT + Concurrent Tislelizumab → TME | pCR |
| B | LC CRT → TME | ||||
| NCT04503694 | Phase 2 | LARC | -- | Regorafenib + Nivolumab → SCRT → Regorafenib + Nivolumab → TME → +/− adjuvant Chemo | pCR |
| NCT04751370 | Phase 2 | LARC | -- | Nivo/Ipi → SCRT → Nivo/Ipi → TME | pCR |
| NCT03921684 | Phase 2 | LARC | -- | LC CRT → FOLFOX + Nivolumab → TME | pCR |
| NCT04124601 | Phase 2 | LARC | A | LC CRT | AE, Response |
| B | LC CRT → Nivo/Ipi | ||||
| NCT03299660 | Phase 2 | LARC | -- | LC CRT → Avelumab → TME | pCR |
| NCT03854799 | Phase 2 | LARC | -- | LC CRT → Avelumab → TME | pCR |
| NCT03503630 | Phase 2 | LARC | -- | SCRT → Avelumab + FOLFOX → TME | pCR |
| NCT04293419 (DUREC) | Phase 2 | LARC | -- | FOLFOX + Durvalumab → LCCRT → TME | pCR |
| NCT05009069 | Phase 2 | LARC | A | LC CRT + Atezolizumab + Tiragolumab → TME | pCR |
| NCT05484024 | Phase 2/3 | LARC | A | SCRT → NACT + Sintilimab → W/W or TME | pCR, DFS |
| B | SCRT → NACT → W/W or TME |
| NCT Number | Phases | Stage | Interventions | Outcome Measures |
|---|---|---|---|---|
| NCT04046133 (CORINTH) | Phase 1 | LA III A/B | CRT + Pembrolizumab | AE, Response |
| NCT04230759 (RADIANCE) | Phase 2 | LA IIB-IIIC | CRT (with 5FU/MMC) | DFS |
| CRT (with 5FU/MMC/Durvalumab) | ||||
| NCT04929028 | Phase 2 | Low Risk HIV | CRT (with 5FU/MMC) | AE, DFS |
| High Risk HIV | CRT (with 5FU/MMC/Nivolumab) | |||
| NCT05661188 (TIRANUS) | Phase 2 | I-IIIB | CRT (with 5FU/MMC/Tiraglolumab/Atezolizumab) | cCR |
| NCT03233711 | Phase 3 | LA II-IIIB | CRT | DFS |
| CRT → Nivolumab | ||||
| NCT05374252 | Phase 3 | LA III | CRT (with 5FU/MMC) | PFS, OS, cCR |
| CRT (with 5FU/MMC/Sintilimab) → Adjuvant Sintilimab |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kumar, R.; Kim, J.; Deek, M.P.; Eskander, M.F.; Gulhati, P.; In, H.; Kennedy, T.; Shah, M.M.; Grandhi, M.S.; Berim, L.; et al. Combination of Immunotherapy and Radiation Therapy in Gastrointestinal Cancers: An Appraisal of the Current Literature and Ongoing Research. Curr. Oncol. 2023, 30, 6432-6446. https://doi.org/10.3390/curroncol30070473
Kumar R, Kim J, Deek MP, Eskander MF, Gulhati P, In H, Kennedy T, Shah MM, Grandhi MS, Berim L, et al. Combination of Immunotherapy and Radiation Therapy in Gastrointestinal Cancers: An Appraisal of the Current Literature and Ongoing Research. Current Oncology. 2023; 30(7):6432-6446. https://doi.org/10.3390/curroncol30070473
Chicago/Turabian StyleKumar, Ritesh, Jongmyung Kim, Matthew P. Deek, Mariam F. Eskander, Prateek Gulhati, Haejin In, Timothy Kennedy, Mihir M. Shah, Miral S. Grandhi, Lyudmyla Berim, and et al. 2023. "Combination of Immunotherapy and Radiation Therapy in Gastrointestinal Cancers: An Appraisal of the Current Literature and Ongoing Research" Current Oncology 30, no. 7: 6432-6446. https://doi.org/10.3390/curroncol30070473
APA StyleKumar, R., Kim, J., Deek, M. P., Eskander, M. F., Gulhati, P., In, H., Kennedy, T., Shah, M. M., Grandhi, M. S., Berim, L., Spencer, K. R., Langan, R. C., Hochster, H. S., Boland, P. M., & Jabbour, S. K. (2023). Combination of Immunotherapy and Radiation Therapy in Gastrointestinal Cancers: An Appraisal of the Current Literature and Ongoing Research. Current Oncology, 30(7), 6432-6446. https://doi.org/10.3390/curroncol30070473







