Pedicled Functional Latissimus Flaps for Reconstruction of the Upper Extremity following Resection of Soft-Tissue Sarcomas
Abstract
1. Introduction
2. Materials and Methods
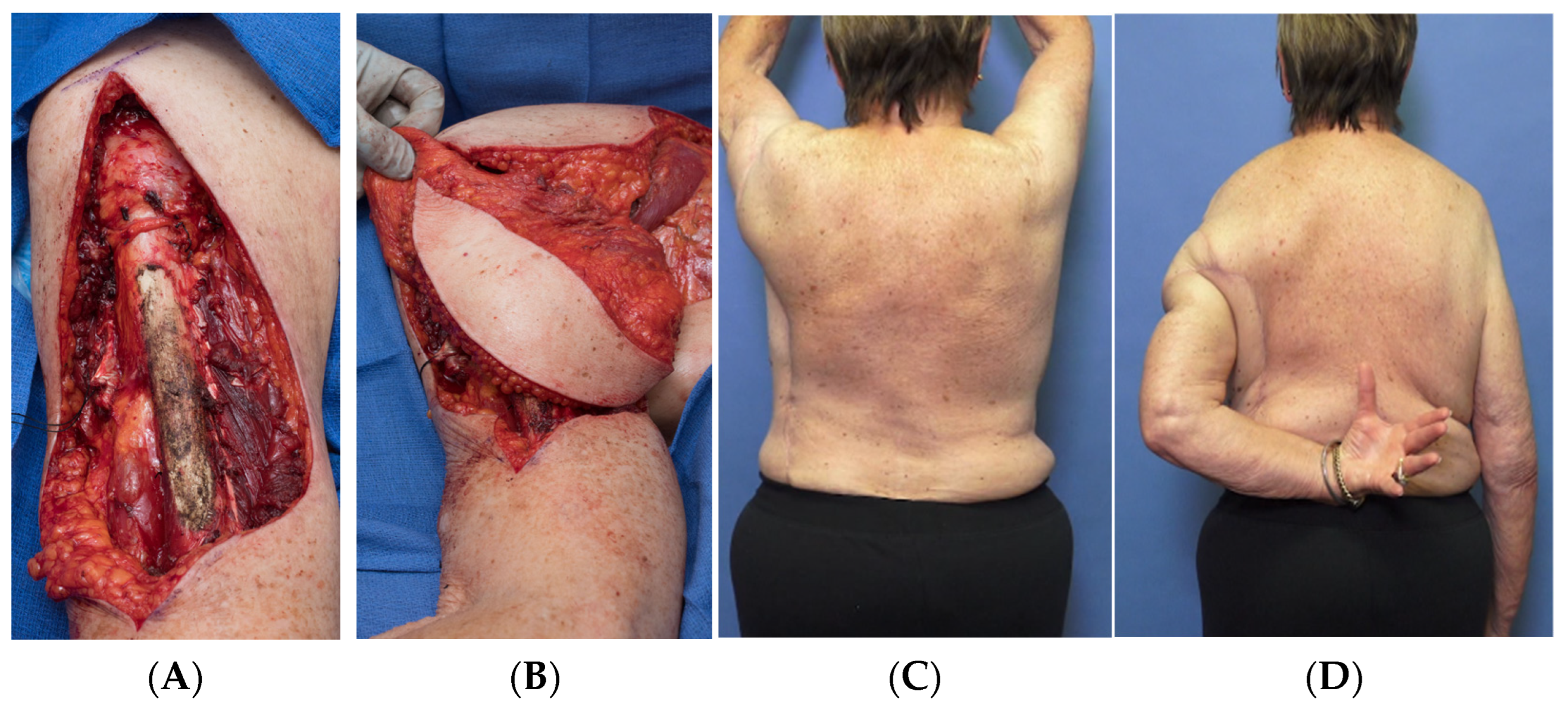
Surgical Technique
3. Results
3.1. Functional Outcomes
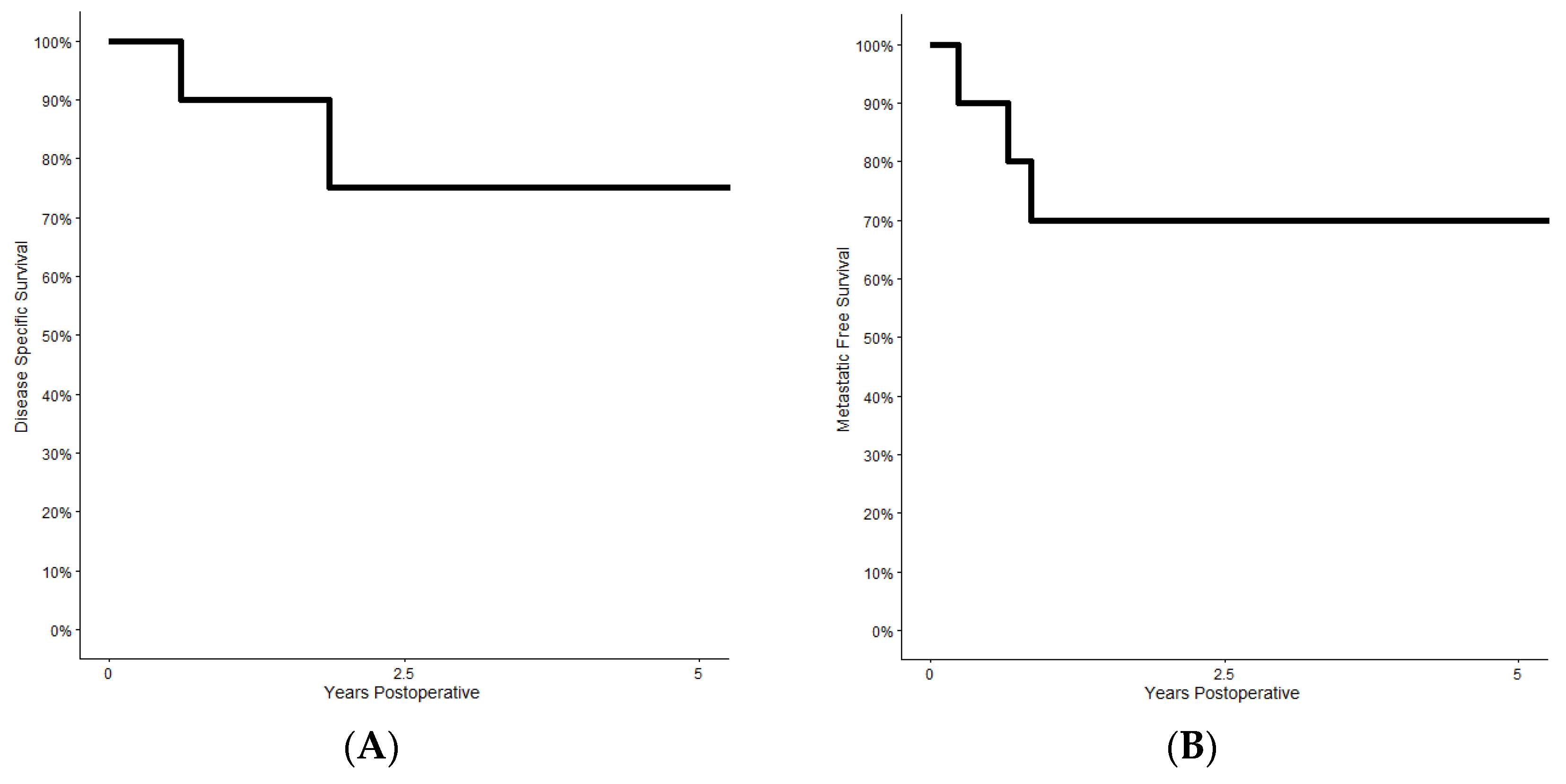
3.2. Oncologic Outcomes
3.3. Complications
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Brennan, M.F.; Casper, E.S.; Harrison, L.B.; Shiu, M.H.; Gaynor, J.; Hajdu, S.I. The role of multimodality therapy in soft-tissue sarcoma. Ann. Surg. 1991, 214, 328–336; discussion 36–38. [Google Scholar] [CrossRef] [PubMed]
- Davidge, K.M.; Wunder, J.; Tomlinson, G.; Wong, R.; Lipa, J.; Davis, A.M. Function and health status outcomes following soft tissue reconstruction for limb preservation in extremity soft tissue sarcoma. Ann. Surg. Oncol. 2010, 17, 1052–1062. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, N.F.; Cannon, C.P.; Lin, P.P.; Lewis, V.O. Soft-tissue sarcoma. J. Am. Acad. Orthop. Surg. 2009, 17, 40–47. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, B.; Davis, A.M.; Turcotte, R.; Bell, R.; Catton, C.; Chabot, P.; Wunder, J.; Kandel, R.; Goddard, K.; Sadura, A.; et al. Preoperative versus postoperative radiotherapy in soft-tissue sarcoma of the limbs: A randomised trial. Lancet 2002, 359, 2235–2241. [Google Scholar] [CrossRef]
- Baysal, Ö.; Toprak, C.; Günar, B.; Erol, B. Soft tissue sarcoma of the upper extremity: Oncological and functional results after surgery. J. Hand Surg. Eur. Vol. 2021, 46, 659–664. [Google Scholar] [CrossRef]
- Grinsell, D.; Di Bella, C.; Choong, P.F. Functional reconstruction of sarcoma defects utilising innervated free flaps. Sarcoma 2012, 2012, 315190. [Google Scholar] [CrossRef]
- Lucattelli, E.; Lusetti, I.L.; Cipriani, F.; Innocenti, A.; De Santis, G.; Innocenti, M. Reconstruction of upper limb soft-tissue defects after sarcoma resection with free flaps: A systematic review. J. Plast. Reconstr. Aesthetic Surg. 2021, 74, 755–767. [Google Scholar] [CrossRef]
- Chao, A.H.; Mayerson, J.L.; Chandawarkar, R.; Scharschmidt, T.J. Surgical management of soft tissue sarcomas: Extremity sarcomas. J. Surg. Oncol. 2015, 111, 540–545. [Google Scholar] [CrossRef]
- Kapoor, T.; Banuelos, J.; Adabi, K.; Moran, S.L.; Manrique, O.J. Analysis of clinical outcomes of upper and lower extremity reconstructions in patients with soft-tissue sarcoma. J. Surg. Oncol. 2018, 118, 614–620. [Google Scholar] [CrossRef]
- Popov, P.; Tukiainen, E.; Asko-Seljavaara, S.; Huuhtanen, R.; Virolainen, M.; Virkkunen, P.; Blomqvist, C. Soft-tissue sarcomas of the upper extremity: Surgical treatment and outcome. Plast. Reconstr. Surg. 2004, 113, 222–230; discussion 31–32. [Google Scholar] [CrossRef]
- Morelli Coppola, M.; Brunetti, B.; Ciarrocchi, S.; Tenna, S.; Persichetti, P. Reconstruction of the Posterior Compartment of the Leg With Functional Free Latissimus Dorsi Flap to the Medial Sural Neurovascular Pedicle. Ann. Plast. Surg. 2021, 86, 731–733. [Google Scholar] [CrossRef]
- Rednam, R.S.; Rinker, B.D. Reconstruction of posterior compartment of lower extremity using a functional latissimus dorsi free flap: A case report. Microsurgery 2016, 36, 77–80. [Google Scholar] [CrossRef] [PubMed]
- Willcox, T.M.; Smith, A.A.; Beauchamp, C.; Meland, N.B. Functional free latissimus dorsi muscle flap to the proximal lower extremity. Clin. Orthop. Relat. Res. 2003, 410, 285–288. [Google Scholar] [CrossRef] [PubMed]
- Athey, A.G.; Wyles, C.C.; Carlsen, B.T.; Perry, K.I.; Houdek, M.T.; Moran, S.L. Free Flap Coverage for Complex Primary and Revision Total Knee Arthroplasty. Plast. Reconstr. Surg. 2021, 148, 804e–810e. [Google Scholar] [CrossRef] [PubMed]
- Houdek, M.T.; Wellings, E.P.; Mallett, K.E.; Honig, R.L.; Rose, P.S.; Moran, S.L. Free Functional Latissimus Dorsi Reconstruction of the Quadriceps and Hamstrings following Oncologic Resection of Soft Tissue Sarcomas of the Thigh. Sarcoma 2021, 2021, 8480737. [Google Scholar] [CrossRef]
- Pierce, T.D.; Tomaino, M.M. Use of the Pedicled Latissimus Muscle Flap for Upper-Extremity Reconstruction. JAAOS—J. Am. Acad. Orthop. Surg. 2000, 8, 324–331. [Google Scholar] [CrossRef]
- Enneking, W.F.; Dunham, W.; Gebhardt, M.C.; Malawar, M.; Pritchard, D.J. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin. Orthop. Relat. Res. 1993, 286, 241–246. [Google Scholar] [CrossRef]
- Chan, L.W.M.; Imanishi, J.; Grinsell, D.G.; Choong, P. Preoperative Radiotherapy and Wide Resection for Soft Tissue Sarcomas: Achieving a Low Rate of Major Wound Complications with the Use of Flaps. Results of a Single Surgical Team. Front. Surg. 2017, 4, 79. [Google Scholar] [CrossRef]
- Payne, C.E.; Hofer, S.O.; Zhong, T.; Griffin, A.C.; Ferguson, P.C.; Wunder, J.S. Functional outcome following upper limb soft tissue sarcoma resection with flap reconstruction. J. Plast. Reconstr. Aesthetic Surg. 2013, 66, 601–607. [Google Scholar] [CrossRef]
- Muramatsu, K.; Ihara, K.; Tominaga, Y.; Hashimoto, T.; Taguchi, T. Functional reconstruction of the deltoid muscle following complete resection of musculoskeletal sarcoma. J. Plast. Reconstr. Aesthetic Surg. 2014, 67, 916–920. [Google Scholar] [CrossRef]
- Ozaniak, A.; Hladik, P.; Lischke, R. Successful Restoration of Elbow Extension Using the Latissimus Dorsi Flap: Case Report. Plast. Reconstr. Surg. Glob. Open 2022, 10, e4121. [Google Scholar] [PubMed]
- Luis Á, M.; Aguilar, D.P.; Martín, J.A. Multidisciplinary management of soft tissue sarcomas. Clin. Transl. Oncol. 2010, 12, 543–553. [Google Scholar] [CrossRef] [PubMed]
- Nakayama, R.; Mori, T.; Okita, Y.; Shiraishi, Y.; Endo, M. A multidisciplinary approach to soft-tissue sarcoma of the extremities. Expert Rev. Anticancer Ther. 2020, 20, 893–900. [Google Scholar] [CrossRef] [PubMed]
- Chuang, D.C.; Strauch, R.J.; Wei, F.C. Technical considerations in two-stage functioning free muscle transplantation reconstruction of both flexor and extensor functions of the forearm. Microsurgery 1994, 15, 338–343. [Google Scholar] [CrossRef]
- Giordano, S.; Kääriäinen, K.; Alavaikko, J.; Kaistila, T.; Kuokkanen, H. Latissimus dorsi free flap harvesting may affect the shoulder joint in long run. Scand. J. Surg. 2011, 100, 202–207. [Google Scholar] [CrossRef]
- Lee, K.T.; Mun, G.H. A systematic review of functional donor-site morbidity after latissimus dorsi muscle transfer. Plast. Reconstr. Surg. 2014, 134, 303–314. [Google Scholar] [CrossRef]
- Spear, S.L.; Hess, C.L. A review of the biomechanical and functional changes in the shoulder following transfer of the latissimus dorsi muscles. Plast. Reconstr. Surg. 2005, 115, 2070–2073. [Google Scholar] [CrossRef]
- Khruekarnchana, P.; Suzuki, K.; Fukuda, H. Shoulder function after subtotal excision of the deltoid muscle and of the deltoid and infraspinatus muscles in extra-abdominal desmoid tumor: A long-term follow-up in two cases. J. Shoulder Elb. Surg. 2004, 13, 119–122. [Google Scholar] [CrossRef]
- Markhede, G.; Monastyrski, J.; Stener, B. Shoulder function after deltoid muscle removal. Acta Orthop. Scand. 1985, 56, 242–244. [Google Scholar] [CrossRef]
- Sanchez-Sotelo, J.; Morrey, B.F. Surgical techniques for reconstruction of chronic insufficiency of the triceps. Rotation flap using anconeus and tendo achillis allograft. J. Bone Jt. Surg. Br. 2002, 84, 1116–1120. [Google Scholar] [CrossRef]
- Clancy, R.; Lim, Z.; Ravinsky, R.A.; O’Neill, A.; Ferguson, P.; Wunder, J. Use of a Fascia Lata Autograft to Reconstruct a Large Triceps Tendon Defect After En-Bloc Resection of a Soft-Tissue Sarcoma: A Case Report. JBJS Case Connect. 2020, 10, e0390. [Google Scholar] [CrossRef] [PubMed]
- Albertsmeier, M.; Rauch, A.; Roeder, F.; Hasenhütl, S.; Pratschke, S.; Kirschneck, M.; Gronchi, A.; Jebsen, N.L.; Cassier, P.A.; Sargos, P.; et al. External Beam Radiation Therapy for Resectable Soft Tissue Sarcoma: A Systematic Review and Meta-Analysis. Ann. Surg. Oncol. 2018, 25, 754–767. [Google Scholar] [CrossRef] [PubMed]
- Bartelstein, M.K.; Yerramilli, D.; Christ, A.B.; Kenan, S.; Ogura, K.; Fujiwara, T.; Fabbri, N.; Healey, J.H. Postradiation Fractures after Combined Modality Treatment in Extremity Soft Tissue Sarcomas. Sarcoma 2021, 2021, 8877567. [Google Scholar] [CrossRef] [PubMed]
- Holt, G.E.; Griffin, A.M.; Pintilie, M.; Wunder, J.S.; Catton, C.; O’Sullivan, B.; Bell, R.S. Fractures following radiotherapy and limb-salvage surgery for lower extremity soft-tissue sarcomas. A comparison of high-dose and low-dose radiotherapy. J. Bone Jt. Surg. Am. 2005, 87, 315–319. [Google Scholar] [CrossRef]
- Leibel, S.A.; Tranbaugh, R.F.; Wara, W.M.; Beckstead, J.H.; Bovill, E.G.; Phillips, T.L. Soft tissue sarcomas of the extremities: Survival and patterns of failure with conservative surgery and postoperative irradiation compared to surgery alone. Cancer 1982, 50, 1076–1083. [Google Scholar] [CrossRef] [PubMed]
- Davis, A.M.; O’Sullivan, B.; Turcotte, R.; Bell, R.; Catton, C.; Chabot, P.; Wunder, J.; Hammond, A.; Benk, V.; Kandel, R.; et al. Late radiation morbidity following randomization to preoperative versus postoperative radiotherapy in extremity soft tissue sarcoma. Radiother. Oncol. 2005, 75, 48–53. [Google Scholar] [CrossRef]
- Davis, A.; O’Sullivan, B.; Bell, R.; Turcotte, R.; Catton, C.; Wunder, J.; Chabot, P.; Hammond, A.; Benk, V.; Isler, M.; et al. Function and health status outcomes in a randomized trial comparing preoperative and postoperative radiotherapy in extremity soft tissue sarcoma. J. Clin. Oncol. 2002, 20, 4472–4477. [Google Scholar] [CrossRef]
- O’Donnell, P.W.; Griffin, A.M.; Eward, W.C.; Sternheim, A.; Catton, C.N.; Chung, P.W.; O’Sullivan, B.; Ferguson, P.C.; Wunder, J.S. The effect of the setting of a positive surgical margin in soft tissue sarcoma. Cancer 2014, 120, 2866–2875. [Google Scholar] [CrossRef]
- Clarkson, P.W.; Griffin, A.; Catton, C.N.; O’Sullivan, B.; Ferguson, P.C.; Wunder, J.S.; Bell, R.S. Epineural dissection is a safe technique that facilitates limb salvage surgery. Clin. Orthop. Relat. Res. 2005, 438, 92–96. [Google Scholar] [CrossRef]
- Jones, K.B.; Ferguson, P.C.; Deheshi, B.; Riad, S.; Griffin, A.; Bell, R.S.; Wunder, J.S. Complete femoral nerve resection with soft tissue sarcoma: Functional outcomes. Ann. Surg. Oncol. 2010, 17, 401–406. [Google Scholar] [CrossRef]
- Ghert, M.A.; Davis, A.; Griffin, A.M.; Alyami, A.; White, L.; Kandel, R.A.; Ferguson, P.; O’Sullivan, B.; Catton, C.N.; Lindsay, T.; et al. The surgical and functional outcome of limb-salvage surgery with vascular reconstruction for soft tissue sarcoma of the extremity. Ann. Surg. Oncol. 2005, 12, 1102–1110. [Google Scholar] [CrossRef] [PubMed]
- Gundle, K.; Kafchinski, L.; Gupta, S.; Griffin, A.; Dickson, B.C.; Chung, P.; Catton, C.N.; O’Sullivan, B.; Wunder, J.S.; Ferguson, P.C. Analysis of Margin Classification Systems for Assessing the Risk of Local Recurrence after Soft Tissue Sarcoma Resection. J. Clin. Oncol. 2018, 36, 704–709. [Google Scholar] [CrossRef] [PubMed]
- Gundle, K.R.; Kafchinski, L.; Dickson, B.C.; Chung, P.W.; Catton, C.N.; O’Sullivan, B.; Ferguson, P.C.; Wunder, J.S.; Gupta, S.; Griffin, A.; et al. An Analysis of Tumor- and Surgery-Related Factors that Contribute to Inadvertent Positive Margins Following Soft Tissue Sarcoma Resection. Ann. Surg. Oncol. 2017, 24, 2137–2144. [Google Scholar] [CrossRef] [PubMed]

| Patient | Age | Gender | Location | Neurovascular Resection | Tumor Size | Tumor Depth | Histology | Additional Treatments |
|---|---|---|---|---|---|---|---|---|
| 1 | 61 | Female | Long Head Triceps Lateral Triceps Medial Triceps | None | 5.6 cm | Deep | UPS | Preop RT (50 Gy) |
| 2 | 76 | Female | Middle Deltoid Posterior Deltoid | Middle and Anterior Axillary Nerve | 5.1 cm | Deep | UPS | Preop RT (50 Gy) |
| 3 | 56 | Male | Long Head Biceps Short Head Biceps Brachialis | MSC Nerve | Re-Excision | Superficial | Myxofibro | Preop RT (50 Gy) |
| 4 | 60 | Female | Long Head Biceps Short Head Biceps Brachialis | MSC Nerve | Re-Excision | Deep | Extraskeletal Osteosarcoma | Preop RT (50 Gy) |
| 5 | 26 | Male | Long Head Triceps Lateral Triceps Medial Triceps | None | 11.8 cm | Deep | NTRK Sarcoma | Preop RT (50 Gy) |
| 6 | 77 | Male | Long Head Triceps Lateral Triceps Medial Triceps | None | 10.8 cm | Deep | Pleomorphic Liposarcoma | Preop RT (50 Gy) |
| 7 | 66 | Male | Long Head Biceps Short Head Biceps Brachialis Anterior Deltoid Coracobrachialis Pectoralis Major | MSC Nerve | 4 nodules 1.5–7.5 cm | Deep | Pleomorphic Spindle Cell Sarcoma | Preop RT (50 Gy) |
| 8 | 68 | Male | Anterior Deltoid Middle Deltoid Posterior Deltoid | Middle and Anterior Axillary Nerve | 10.3 cm | Deep | Myxofibro | Preop RT (50 Gy) |
| 9 | 63 | Male | Long Head Biceps Short Head Biceps Brachialis Anterior Deltoid Coracobrachialis Brachioradialis | MSC Nerve | 24 cm | Deep | UPS | Preop RT (50 Gy) |
| 10 | 77 | Male | Long Head Triceps Lateral Triceps Medial Triceps | None | 12.6 cm | Deep | UPS | Preop RT (50 Gy) Intraop RT (11 Gy) |
| Patient | Elbow ROM | Shoulder ROM | Strength | MSTS93 | Complication | Tumor Recurrence | Clinical Status |
|---|---|---|---|---|---|---|---|
| 1 | 10–120° | 0–170° | 4/5 | 93% | - | - | ANED 4 Years |
| 2 | 0–130° | 0–180° | 5/5 | 97% | Delayed Healing | - | ANED 4 Years |
| 3 | 10–120° | 0–160° | 5/5 | 100% | Delayed Healing Needed STSG | - | ANED 1 Year |
| 4 | 10–110° | 0–170° | 4/5 | 93% | Delayed Healing Needed STSG | - | ANED 2.5 Years |
| 5 | 0–130° | 0–180° | 4/5 | 90% | - | - | ANED 2 Years |
| 6 | 0–120° | 0–170° | 4/5 | 97% | - | - | ANED 11 years |
| 7 | 10–115° | 0–170° | 5/5 | 97% | Delayed Healing | Metastatic Disease Lymph nodes, Lungs | AWED 1 year |
| 8 | 0–130° | 0–150° | 4/5 | 93% | Donor Site Seroma Needed I and D | Metastatic Disease Lungs | DOD 2 years |
| 9 | 0° | 0° | 0/5 | 37% | Radiation Associated Humerus Fracture | Metastatic Disease Lungs | DOD 8 Years |
| 10 | 25–120° | 0–160° | 3/5 | 80% | - | Metastatic Disease Soft Tissue, Lungs | DOD 7 Months |
| Citation | Patients | Tumor Location | Surgical Technique Data | Outcomes |
|---|---|---|---|---|
| Grinsell et al. [6] |
|
|
|
|
| Lucattelli et al. [7] |
| - |
|
|
| Kapoor et al. [9] |
|
|
|
|
| Rednam et al. [12] |
| - |
|
|
| Houdek et al. [15] |
|
|
|
|
| Chan et al. [18] |
|
|
|
|
| Payne et al. [19] |
|
|
|
|
| Muramatus et al. [20] |
|
|
|
|
| Ozaniak et al. [21] |
|
|
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arguello, A.M.; Sullivan, M.H.; Mills, G.L.; Moran, S.L.; Houdek, M.T. Pedicled Functional Latissimus Flaps for Reconstruction of the Upper Extremity following Resection of Soft-Tissue Sarcomas. Curr. Oncol. 2023, 30, 3138-3148. https://doi.org/10.3390/curroncol30030237
Arguello AM, Sullivan MH, Mills GL, Moran SL, Houdek MT. Pedicled Functional Latissimus Flaps for Reconstruction of the Upper Extremity following Resection of Soft-Tissue Sarcomas. Current Oncology. 2023; 30(3):3138-3148. https://doi.org/10.3390/curroncol30030237
Chicago/Turabian StyleArguello, Alexandra M., Mikaela H. Sullivan, Gavin L. Mills, Steven L. Moran, and Matthew T. Houdek. 2023. "Pedicled Functional Latissimus Flaps for Reconstruction of the Upper Extremity following Resection of Soft-Tissue Sarcomas" Current Oncology 30, no. 3: 3138-3148. https://doi.org/10.3390/curroncol30030237
APA StyleArguello, A. M., Sullivan, M. H., Mills, G. L., Moran, S. L., & Houdek, M. T. (2023). Pedicled Functional Latissimus Flaps for Reconstruction of the Upper Extremity following Resection of Soft-Tissue Sarcomas. Current Oncology, 30(3), 3138-3148. https://doi.org/10.3390/curroncol30030237






