Impact of the COVID-19 Pandemic on Medical Oncology Workload: A Provincial Review
Abstract
1. Introduction
2. Methods
3. Results
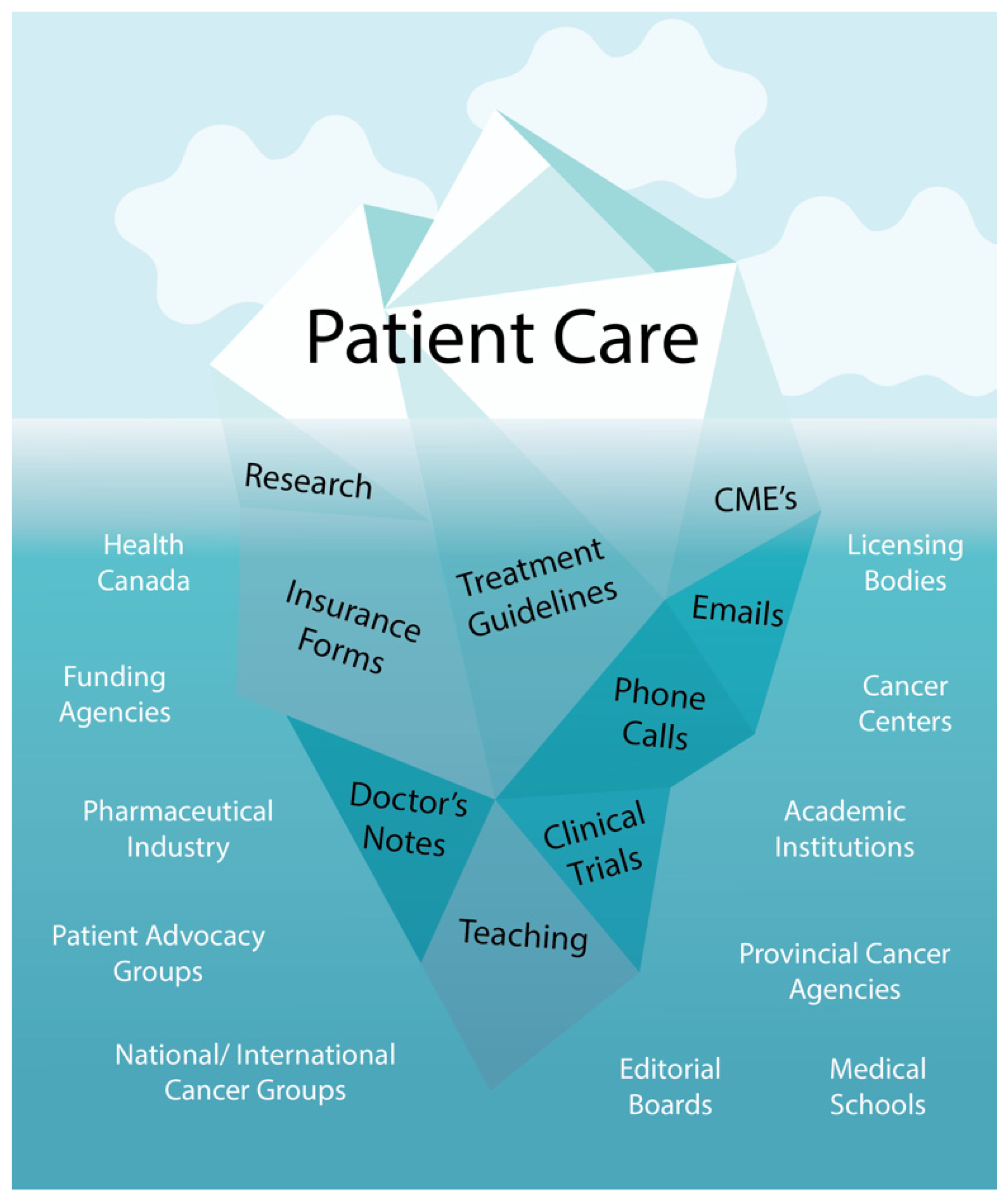
3.1. Overall Clinical Workload
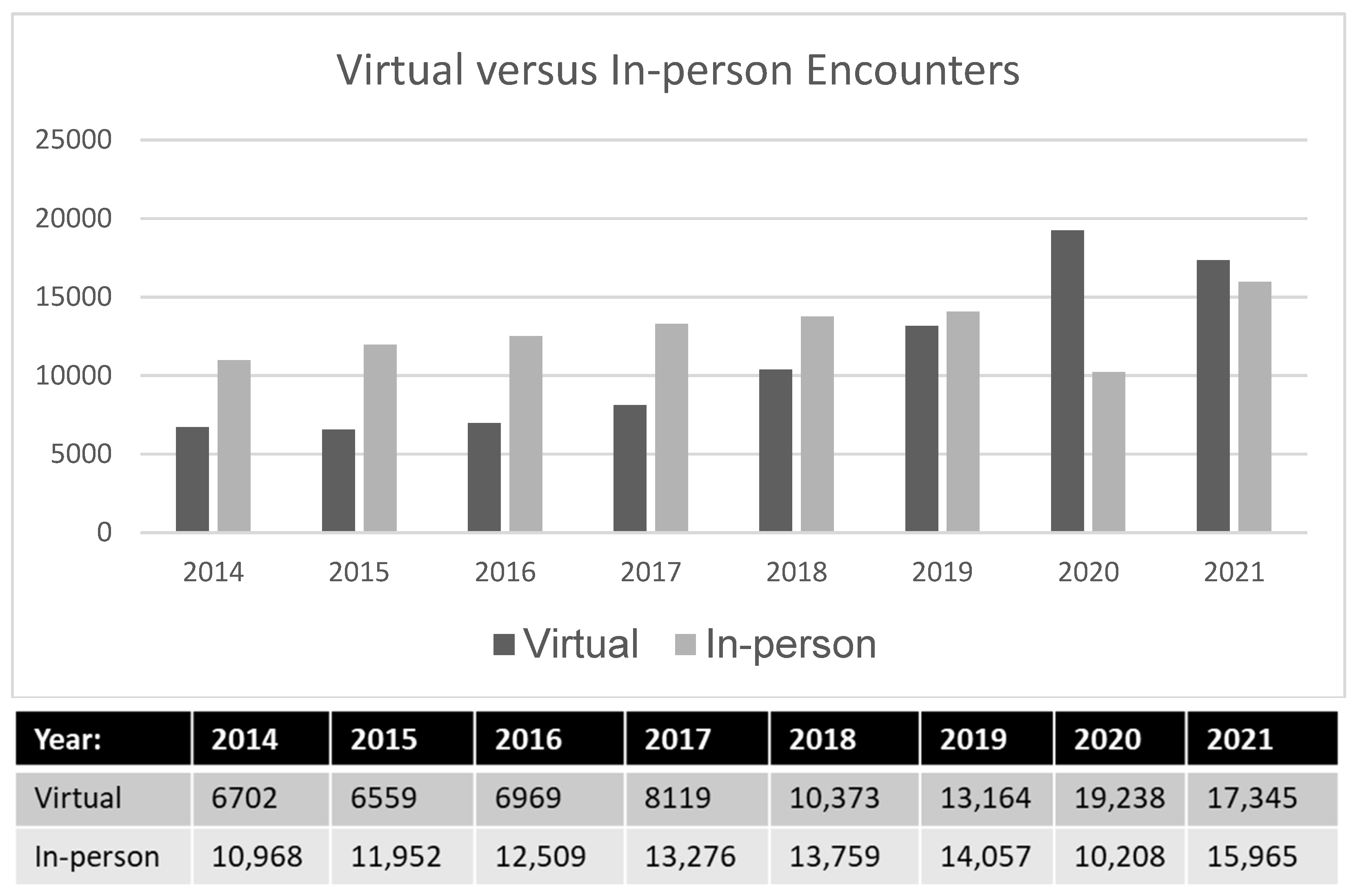
3.2. Clinical Workload during the COVID-19 Pandemic
3.3. Clinical Workload by Tumor Site
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Canadian Cancer Statistics Advisory Committee in Collaboration with the Canadian Cancer Society, Statistics Canada and Public Health Agency of Canada. Canadian Cancer Statistics 2021; Canadian Cancer Society: Toronto, ON, Canada, 2021.
- Statistics Canada Canadian Cancer Registry. Number and Rates of New Primary Cancer, by Cancer Type, Age Group, and Sex. Available online: https://www150.statcan.gc.ca/t1/tb11/en/tv.action?pid=1310011101 (accessed on 6 January 2022).
- Rittberg, R.; Mann, A.; Desautels, D.; Earle, C.; Navaratnam, S.; Pitz, M. Canadian Cancer Centre Response to COVID-19 Pandemic: A National and Provincial Response. Curr. Oncol. 2020, 28, 233–251. [Google Scholar] [CrossRef] [PubMed]
- Fundytus, A.; Hopman, W.; Hammad, N.; Biagi, J.; Sullivan, R.; Vanderpuye, V.; Seruga, B.; Lopes, G.; Sengar, M.; Brundage, M.; et al. Medical Oncology Workload in Canada: Infrastructure, Supports, and Delivery of Clinical Care. Curr. Oncol. 2018, 25, 206–212. [Google Scholar] [CrossRef] [PubMed]
- Fundytus, A.; Sullivan, R.; Vanderpuye, V.; Seruga, B.; Lopes, G.; Hammad, N.; Sengar, M.; Hopman, W.M.; Brundage, M.D.; Booth, C.M. Delivery of Global Cancer Care: An International Study of Medical Oncology Workload. J. Glob. Oncol. 2018, 4, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Yip, S.M.; Loewen, S.K.; Li, H.; Hao, D.; Easaw, J.C. Management of Medical Oncology Services in Canada: Redefined Workload with a Novel Supply-and-Demand Workforce Projection Model. J. Oncol. Pract. 2018, 14, e438–e445. [Google Scholar] [CrossRef] [PubMed]
- Cancer Care Ontario Systemic Therapy Task Force. The Systemic Therapy Task Force Report. 2000. Available online: https://www.cancercare.on.ca/common/pages/UserFile.aspx?fileId=14436 (accessed on 5 November 2020).
- Brenner, D.R.; Poirier, A.; Woods, R.R.; Ellison, L.F.; Billette, J.-M.; Demers, A.A.; Zhang, S.X.; Yao, C.; Finley, C.; Fitzgerald, N.; et al. Projected estimates of cancer in Canada in 2022. Can. Med. Assoc. J. 2022, 194, E601–E607. [Google Scholar] [CrossRef] [PubMed]
- Canadian Institute for Health Information. Wait Times for Priority Procedures in Canada, 2021: Focus on the First 6 Months of the COVID-19 Pandemic; Canadian Institute for Health Information: Ottawa, ON, Canada, 2021; Available online: https://www.cihi.ca/en/wait-times-for-priority-procedures-in-canada (accessed on 6 July 2022).
- Corvaja, C.; Targato, G.; Garattini, S.K.; Barazzutti, C.; Bin, A.; Donato, R.; Mansutti, M.; Riosa, C.; Rizzato, S.; Troiero, G.; et al. The impact of COVID-19 pandemic on oncology workload: The experience of an Italian reference cancer centre (Abstract). J. Clin. Oncol. 2021, 39, 15. [Google Scholar] [CrossRef]
- Tsang-Wright, F.; Tasoulis, M.-K.; Roche, N.; MacNeil, F. Breast cancer surgery after the COVID-19 pandemic. Future Oncol. 2020, 16, 33. [Google Scholar] [CrossRef] [PubMed]
- Nova Scotia Health—COVID Hub. Available online: https://covid19hub.nshealth.ca/workingin/ambulatorycare/resources#s-lg-box-wrapper-19169461 (accessed on 6 July 2022).
- Chiang, J.; Yang, V.; Han, S.; Zhuang, Q.; Zhou, S.; Mathur, S.; Kang, M.L.; Ngeow, J.; Yap, S.P.; Tham, C.K. Oncology workload in a tertiary hospital during the COVID-19 pandemic. Proc. Singap. Healthc. 2021. [Google Scholar] [CrossRef]
- Seruga, B.; Sullivan, R.; Fundytus, A.; Hopman, W.; Ocana, A.; Joffe, J.; Bodoky, G.; Le Tourneau, C.; Vanderpuye, V.; Lopes, G.; et al. Medical Oncology Workload in Europe: One Continent, Several Worlds. Clin. Oncol. 2020, 32, e19–e26. [Google Scholar] [CrossRef] [PubMed]
- Marhold, M.; Topakian, T.; Agis, H.; Bartsch, R.; Berghoff, A.S.; Brodowicz, T.; Fuereder, T.; Ilhan-Mutlu, A.; Kiesewetter, B.; Krainer, M.; et al. Thirteen-year analyses of medical oncology outpatient day clinic data: A changing field. ESMO Open 2020, 5, e000880. [Google Scholar] [CrossRef] [PubMed]
- Hadid, M.; Elomri, A.; El Mekkawy, T.; Jouini, O.; Kerbache, L.; Hamad, A. Operations management of outpatient chemotherapy process: An optimization-oriented comprehensive review. Oper. Res. Prospect. 2022, 9, 100214. [Google Scholar] [CrossRef]
- Ward, M.M.; Ullrich, F.; Matthews, K.; Rushton, G.; Tracy, R.; Bajorin, D.F. Access to chemotherapy services by availability of local and visiting oncologists. J. Oncol. Pract. 2014, 10, 26–31. [Google Scholar] [CrossRef] [PubMed]
- Grávalos, C.; Salvador, J.; Albanell, J.; Barnadas, A.; Borrega, P.; García-Mata, J.; Garrido, P.; González-Flores, E.; Isla, L.; Lomas, M.; et al. Functions and workload of medical oncologists in Spain. Clin. Transl. Oncol. 2012, 6, 423–429. [Google Scholar] [CrossRef] [PubMed]
- Moreira, A.; Heinzerling, L.; Bhardwaj, N.; Friedlander, P. Current Melanoma Treatments: Where do we stand? Cancers 2021, 13, 221. [Google Scholar] [CrossRef] [PubMed]
- Deb, D.; Moore, A.; Roy, U. The 2021 Global Lung Cancer Therapy Landscape. J. Thorac. Oncol. 2021, 17, 931–936. [Google Scholar] [CrossRef] [PubMed]
- Wong, K.; King, G.; Harris, W. The Treatment Landscape of Advanced Hepatocellular Carcinoma. Curr. Oncol. Rep. 2022, 24, 917–927. [Google Scholar] [CrossRef] [PubMed]
- Saung, M.; Zheng, L. Current Standards for Chemotherapy in Pancreatic Cancer. Clin. Ther. 2017, 39, 2125–2134. [Google Scholar] [CrossRef] [PubMed]
- Statistics Canada. Primary Health Care Providers, 2019. Available online: https://www150.statcan.gc.ca/n1/pub/82-625-x/2020001/article/00004-eng.htm (accessed on 21 September 2022).
- Nova Scotia Department of Health and Wellness. Virtual Care as a Protective Measure in Nova Scotia’s COVID-19 Response: A Shift of Physicians’ Services from Face-to-Face Care. 2021. Available online: https://novascotia.ca/dhw/publications/VC_evaluation_report.pdf (accessed on 21 September 2022).
- Canadian Cancer Society. Living at the Crossroads of COVID-19 and Cancer: A What We Heard Report by the Canadian Cancer Society. 2022. Available online: https://cdn.cancer.ca/-/media/files/get-involved/advocacy/what-we-are-doing/covid-19-response/living-at-the-crossroads-of-covid-19-and-cancer-a-what-we-heard-report-by-ccs.pdf?rev=19957a0df6a140c3811c2bdfd1f20c42&hash=D014BE2960F359974157287F44DDA24C&_gl=1*hefec9*_ga*MTg3ODgzMTk3MS4xNTQ5MjE5MTk5*_ga_23YMKBE2C3*MTY2NDIzODIyMy4zLjAuMTY2NDIzODIyMy42MC4wLjA (accessed on 19 September 2022).
- Malagon, T.; Yong, J.; Tope, P.; Miller, W.; Franco, E. Predicted long-term impact of COVID-19 pandemic-related care delays on cancer mortality in Canada. Int. J. Cancer 2022, 150, 1244–1254. [Google Scholar] [CrossRef] [PubMed]
- Stuckless, T.; Milosevic, M.; de Metz, C.; Parliament, M.; Tompkins, B.; Brundage, M. Managing a National Radiation Oncology Workforce: A workforce planning model. Radiother. Oncol. 2012, 103, 123–129. [Google Scholar] [CrossRef] [PubMed]


| Year | Consults | Follow-Up | Teletoxicities | Chart Review |
|---|---|---|---|---|
| 2014 | 2228 | 8902 | 915 | 5625 |
| 2015 | 2607 | 9380 | 623 | 5900 |
| 2016 | 2612 | 9951 | 648 | 6267 |
| 2017 | 2779 | 10,577 | 794 | 7244 |
| 2018 | 2708 | 11,096 | 1356 | 8971 |
| 2019 | 3003 | 11,203 | 2182 | 10,907 |
| 2020 | 2824 | 11,721 | 2006 | 12,896 |
| 2021 | 3254 | 13,485 | 2749 | 13,822 |
| % Change | 46.1% | 51.5% | 200.4% | 145.7% |
| # Visits/MO in 2014 | # Visits/MO in 2021 | # Encounters/Consult (2014) | # Encounters/ Consult (2021) | |
|---|---|---|---|---|
| GI | ||||
| Consults | 111.5 | 121.9 | ---- | ---- |
| Follow-up | 380.7 | 403.4 | 3.4 | 3.3 |
| Teletoxicities | 42.9 | 55.1 | 0.4 | 0.5 |
| Chart Review | 186.9 | 343.7 | 1.7 | 2.8 |
| BREAST | ||||
| Consults | 101.8 | 94.9 | ---- | ---- |
| Follow-up | 391.5 | 337.1 | 3.8 | 3.6 |
| Teletoxicities | 49.1 | 57.7 | 0.5 | 0.6 |
| Chart Review | 191.9 | 338.2 | 1.9 | 3.6 |
| GU | ||||
| Consults | 123.9 | 94.5 | ---- | ---- |
| Follow-up | 614.1 | 625.6 | 5.0 | 6.3 |
| Teletoxicities | 52 | 147.7 | 0.4 | 1.5 |
| Chart Review | 565 | 560.7 | 4.6 | 5.6 |
| LUNG | ||||
| Consults | 98.2 | 111.7 | ---- | ---- |
| Follow-up | 443.4 | 464.9 | 4.5 | 4.2 |
| Teletoxicities | 32.4 | 105.2 | 0.3 | 0.9 |
| Chart Review | 329 | 586.2 | 3.4 | 5.3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sheridan, M.; Colwell, B.; Lamond, N.W.D.; Macfarlane, R.; Rayson, D.; Snow, S.; Wood, L.A.; Ramjeesingh, R. Impact of the COVID-19 Pandemic on Medical Oncology Workload: A Provincial Review. Curr. Oncol. 2023, 30, 3149-3159. https://doi.org/10.3390/curroncol30030238
Sheridan M, Colwell B, Lamond NWD, Macfarlane R, Rayson D, Snow S, Wood LA, Ramjeesingh R. Impact of the COVID-19 Pandemic on Medical Oncology Workload: A Provincial Review. Current Oncology. 2023; 30(3):3149-3159. https://doi.org/10.3390/curroncol30030238
Chicago/Turabian StyleSheridan, Margaret, Bruce Colwell, Nathan W. D. Lamond, Robyn Macfarlane, Daniel Rayson, Stephanie Snow, Lori A. Wood, and Ravi Ramjeesingh. 2023. "Impact of the COVID-19 Pandemic on Medical Oncology Workload: A Provincial Review" Current Oncology 30, no. 3: 3149-3159. https://doi.org/10.3390/curroncol30030238
APA StyleSheridan, M., Colwell, B., Lamond, N. W. D., Macfarlane, R., Rayson, D., Snow, S., Wood, L. A., & Ramjeesingh, R. (2023). Impact of the COVID-19 Pandemic on Medical Oncology Workload: A Provincial Review. Current Oncology, 30(3), 3149-3159. https://doi.org/10.3390/curroncol30030238






