Novel Approach to Improving Specialist Access in Underserved Populations with Suspicious Oral Lesions
Abstract
1. Introduction
2. Materials and Methods
2.1. Overview
2.2. Subjects
2.3. Protocol
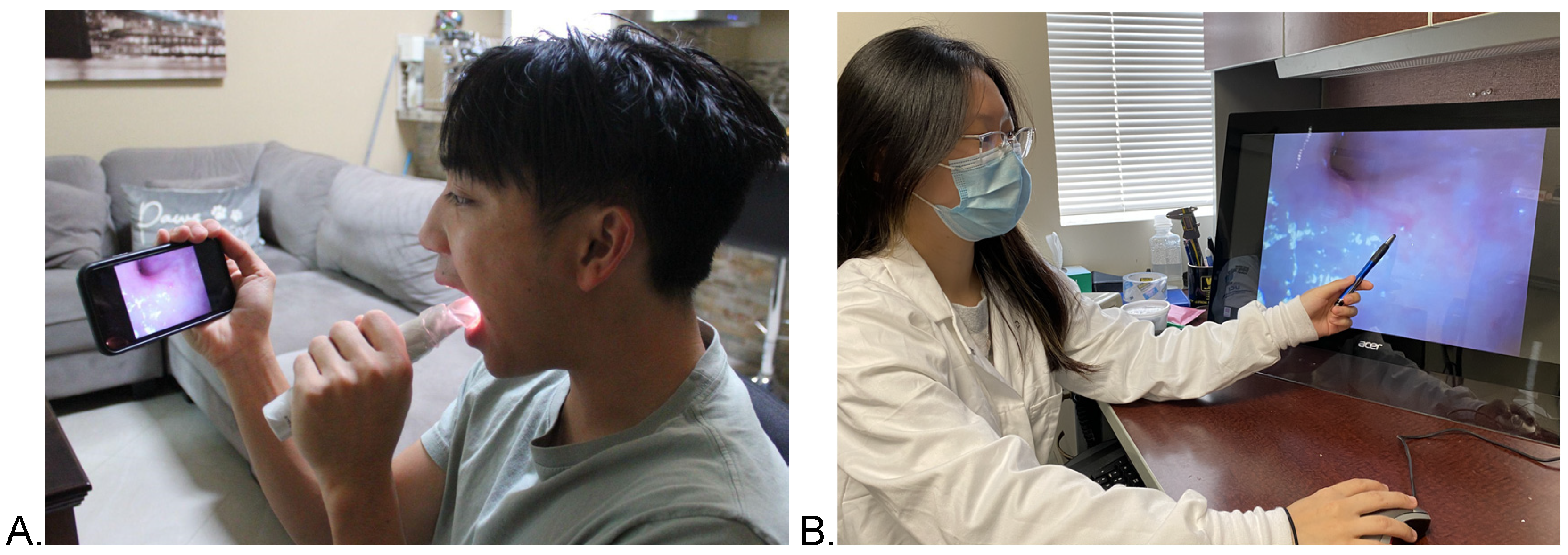
2.4. Intraoral Camera Platform
2.5. Statistical Analysis
3. Results
3.1. Subjects
3.2. Diagnostic Accuracy vs. Histopathology
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ferlay, J.; Shin, H.-R.; Bray, F.; Forman, D.; Mathers, C.; Parkin, D.M. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int. J. Cancer 2010, 127, 2893–2917. [Google Scholar] [CrossRef] [PubMed]
- Westra, W.H. The Changing Face of Head and Neck Cancer in the 21st Century: The Impact of HPV on the Epidemiology and Pathology of Oral Cancer. Head Neck Pathol. 2009, 3, 78–81. [Google Scholar] [CrossRef] [PubMed]
- Lingen, M.W.; Kalmar, J.R.; Karrison, T.; Speight, P.M. Critical evaluation of diagnostic aids for the detection of oral cancer. Oral Oncol. 2008, 44, 10–22. [Google Scholar] [CrossRef] [PubMed]
- Jamal, A.; Agaku, I.T.; O’Connor, E.; King, B.A.; Kenemer, J.B.; Neff, L. Current Cigarette Smoking among Adults-United States, 2005–2013. Morb. Mortal. Wkly. Rep. 2014, 63, 1108–1112. [Google Scholar]
- Gupta, P.C.; Mehta, F.S.; Daftary, D.K.; Pindborg, J.J.; Bhonsle, R.B.; Jalnawalla, P.N.; Sinor, P.N.; Pitkar, V.K.; Murti, P.R.; Irani, R.R.; et al. Incidence rates of oral cancer and natural history of oral precancerous lesions in a 10-year follow-up study of Indian villagers. Community Dent. Oral Epidemiol. 1980, 8, 287–333. [Google Scholar] [CrossRef]
- Silverman, S.; Gorsky, M.; Lozada, F. Oral Leukoplakia and Malignant Transformation. A Follow-up Study of 257 Patients. Cancer 1984, 53, 563–568. [Google Scholar]
- Silverman, S.; Bhargava, K.; Mani, N.J.; Smith, L.W.; Malaowalla, A.M. Malignant transformation and natural history of oral leukoplakia in 57,518 industrial workers of gujarat, india. Cancer 1976, 38, 1790–1795. [Google Scholar] [CrossRef]
- Silverman, S. Early Diagnosis of Oral Cancer. Cancer 1988, 62, 1796–1799. [Google Scholar] [CrossRef]
- Speight, P.M.; Khurram, S.A.; Kujan, O. Oral potentially malignant disorders: Risk of progression to malignancy. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2018, 125, 612–627. [Google Scholar] [CrossRef]
- Warnakulasuriya, S. Oral potentially malignant disorders: A comprehensive review on clinical aspects and management. Oral Oncol. 2020, 102, 104550. [Google Scholar] [CrossRef]
- Iocca, O.; Sollecito, T.P.; Alawi, F.; Weinstein, G.S.; Newman, J.G.; De Virgilio, A.; Di Maio, P.; Spriano, G.; López, S.P.; Shanti, R.M. Potentially malignant disorders of the oral cavity and oral dysplasia: A systematic review and meta-analysis of malignant transformation rate by subtype. Head Neck 2019, 42, 539–555. [Google Scholar] [CrossRef] [PubMed]
- Murphy, C.T.; Galloway, T.J.; Handorf, E.A.; Egleston, B.; Wang, L.S.; Mehra, R.; Flieder, D.B.; Ridge, J.A. Survival Impact of Increasing Time to Treatment Initiation for Patients With Head and Neck Cancer in the United States. J. Clin. Oncol. 2016, 34, 169–178. [Google Scholar] [CrossRef]
- Villa, A.; Bin Woo, S. Leukoplakia—A Diagnostic and Management Algorithm. J. Oral Maxillofac. Surg. 2017, 75, 723–734. [Google Scholar] [CrossRef]
- Vernham, G.A.; Crowther, J.A. Head and neck carcinoma ? stage at presentation. Clin. Otolaryngol. 1994, 19, 120–124. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, A.K.; Sethi, A.; Sareen, D.; Dhingra, S. Treatment Delay in Oral and Oropharyngeal Cancer in Our Population: The Role of Socio-Economic Factors and Health-Seeking Behaviour. Indian J. Otolaryngol. Head Neck Surg. 2011, 63, 145–150. [Google Scholar] [CrossRef] [PubMed]
- McGurk, M.; Chan, C.; Jones, J.; O’Regan, E.; Sherriff, M. Delay in diagnosis and its effect on outcome in head and neck cancer. Br. J. Oral Maxillofac. Surg. 2005, 43, 281–284. [Google Scholar] [CrossRef] [PubMed]
- Alston, P.A.; Knapp, J.; Luomanen, J.C. Who Will Tend the Dental Safety Net? J. Calif. Dent. Assoc. 2014, 42, 112–118. [Google Scholar]
- Available online: http://ocf.org.in/mainconfig.aspx?Moduleid=107&isexpandable=True&categoryid=162 (accessed on 9 October 2017).
- Ries, L.G.; Eisner, M.P.; Kosary, C.L.; Hankey, B.F.; Miller, B.A.; Clegg, L.; Mariotto, A.; Feuer, E.J.; Edwards, B.K. SEER Cancer Statistics Review; National Cancer Institute: Rockville, MD, USA, 2005; pp. 1975–2002.
- Graboyes, E.; Cramer, J.; Balakrishnan, K.; Cognetti, D.M.; López-Cevallos, D.; De Almeida, J.R.; Megwalu, U.C.; Moore, C.E.; Nathan, C.; Spector, M.E.; et al. COVID-19 pandemic and health care disparities in head and neck cancer: Scanning the horizon. Head Neck 2020, 42, 1555–1559. [Google Scholar] [CrossRef] [PubMed]
- Goshtasbi, A. (CCDH, London, UK; Washington, DC, USA). Personal communication, 2020.
- Alberson, R. Is TeleMedicine Here to Stay? NYT. August 2020. Available online: https://www.nytimes.com/2020/08/03/health/covid-telemedicine-congress.html (accessed on 10 April 2022).
- Hincapié, M.A.; Gallego, J.C.; Gempeler, A.; Piñeros, J.A.; Nasner, D.; Escobar, M.F. Implementation and Usefulness of Telemedicine During the COVID-19 Pandemic: A Scoping Review. J. Prim. Care Community Health 2020, 11. [Google Scholar] [CrossRef]
- Ibrahim, A.E.; Magdy, M.; Khalaf, E.M.; Mostafa, A.; Arafa, A. Teledermatology in the time of COVID-19. Int. J. Clin. Pract. 2021, 75, e15000. [Google Scholar] [CrossRef]
- Kane-Gill, S.L.; Rincon, F. Expansion of Telemedicine Services. Crit. Care Clin. 2019, 35, 519–533. [Google Scholar] [CrossRef]
- Sud, E.; Anjankar, A. Applications of Telemedicine in Dermatology. Cureus 2022, 14, e27740. [Google Scholar] [CrossRef] [PubMed]
- Augusterfer, E.F.; O’Neal, C.R.; Martin, S.W.; Sheikh, T.L.; Mollica, R.F. The Role of Telemental Health, Tele-consultation, and Tele-supervision in Post-disaster and Low-resource Settings. Curr. Psychiatry Rep. 2020, 22, 1–10. [Google Scholar] [CrossRef]
- Wilder-Smith, P.; Beckman Laser Institute and Medical Clinic, Irvine, California, US. Unpublished data. 2021.
- Wilder-Smith, P.; Beckman Laser Institute and Medical Clinic, Irvine, California, US. Unpublished data. 2022.
- Riju, J.; Tirkey, A.J.; Mathew, M.; Chamania, G.; Babu, M.; Patil, S.; Anto, R.; Agarwal, M.; Vidya, K. Analysis of Early Impact of COVID-19 on Presentation and Management of Oral Cancers – an Experience from a Tertiary Care Hospital in South India. Indian J. Surg. Oncol. 2021, 12, 242–249. [Google Scholar] [CrossRef]
- Stennett, M.; Tsakos, G. The impact of the COVID-19 pandemic on oral health inequalities and access to oral healthcare in England. Br. Dent. J. 2022, 232, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Popovic, M.; Fiano, V.; Moirano, G.; Chiusa, L.; Conway, D.I.; Demo, P.G.; Gilardetti, M.; Iorio, G.C.; Moccia, C.; Ostellino, O.; et al. The Impact of the COVID-19 Pandemic on Head and Neck Cancer Diagnosis in the Piedmont Region, Italy: Interrupted Time-Series Analysis. Front. Public Health 2022, 10, 225. [Google Scholar] [CrossRef] [PubMed]
- Ms, R.A.S.; Gao, W.; Bs, C.R.W.; Kurachi, C.; Lee, J.J.; El-Naggar, A.K.; Richards-Kortum, R.; Gillenwater, A. Noninvasive evaluation of oral lesions using depth-sensitive optical spectroscopy. Cancer 2009, 115, 1669–1679. [Google Scholar] [CrossRef]
- Jafari, A.; Najafi, S.; Moradi, F.; Kharazifard, M.; Khami, M.R. Delay in the Diagnosis and Treatment of Oral Cancer. J. Dent. (Shiraz, Iran) 2013, 14, 146–150. [Google Scholar]
- Shepperd, J.A.; Howell, J.L.; Logan, H. A survey of barriers to screening for oral cancer among rural Black Americans. Psycho-Oncology 2013, 23, 276–282. [Google Scholar] [CrossRef] [PubMed]
- Edwards, P.; Subramanian, S.; Hoover, S.; Ramesh, C.; Ramadas, K. Financial barriers to oral cancer treatment in India. J. Cancer Policy 2016, 7, 28–31. [Google Scholar] [CrossRef]
- Villa, A.; Stock, S.; Aboalela, A.; Lerman, M.A.; Woo, S.-B.; Sonis, S.T.; Treister, N.S. Oral Medicine referrals at a hospital-based practice in the United States. Oral Surgery, Oral Med. Oral Pathol. Oral Radiol. 2015, 119, 423–429. [Google Scholar] [CrossRef] [PubMed]
- Shetty, S.; Shaik, M.; Babu, S. Oral medicine and radiology- the Indian scenario. J. Contemp. Med Educ. 2013, 1, 59–61. [Google Scholar] [CrossRef]
- Janakiram, C.; Rajeev, B.; Taha, F.; Venkitachalam, R.; Akalgud, H.; Kadanakuppe, S. Equity in Oral Healthcare in In-dia A Review on Health System Analysis. Econ. Political Wkly. 2017, 52, 82–89. [Google Scholar]
- Gambhir, R.; Gupta, T. Need for Oral Health Policy in India. Ann. Med Heal. Sci. Res. 2016, 6, 50–55. [Google Scholar] [CrossRef] [PubMed]
- The Dentist Workforce. Available online: https://www.ada.org/-/media/project/ada-organization/ada/ada-org/files/resources/research/hpi/hpidata_supply_of_dentists_2021.xlsx?rev=5a77b55be401470483e65011fbca7c18&hash=791602EB2E5A91F065BBC975ACBCBDC2 (accessed on 20 July 2022).
- Ng, S.W.; Sobri, S.N.S.S.M.; Zain, R.B.; Kallarakkal, T.G.; Amtha, R.; Wong, F.A.W.; Rimal, J.; Durward, C.; Chea, C.; Jayasinghe, R.D.; et al. Barriers to early detection and management of oral cancer in the Asia Pacific region. J. Health Serv. Res. Policy 2022, 27, 133–140. [Google Scholar] [CrossRef]
- Pinto, A.; Khalaf, M.; Miller, C.S. The practice of oral medicine in the United States in the twenty-first century: An update. Oral Surgery, Oral Med. Oral Pathol. Oral Radiol. 2015, 119, 408–415. [Google Scholar] [CrossRef] [PubMed]
- Haberland, C.M.; Allen, C.M.; Beck, F. Referral patterns, lesion prevalence, and patient care parameters in a clinical oral pathology practice. Oral Surgery, Oral Med. Oral Pathol. Oral Radiol. Endodontology 1999, 87, 583–588. [Google Scholar] [CrossRef]
- Carrard, V.C.; Gonçalves, M.; Strey, J.R.; Pilz, C.; Martins, M.A.T.; Schmitz, C.A.A.; Moro, R.G.D.; D’Avila, O.; Rados, D.; Harzheim, E. Telediagnosis of oral lesions in primary care: The EstomatoNet Program. Oral Dis. 2018, 24, 1012–1019. [Google Scholar] [CrossRef]
- Khan, S.A.; Omar, H. Teledentistry in Practice: Literature Review. Telemed. e-Health 2013, 19, 565–567. [Google Scholar] [CrossRef]
- Tiwari, T.; Diep, V.; Tranby, E.; Thakkar-Samtani, M.; Frantsve-Hawley, J. Dentist perceptions about the value of teledentistry. BMC Oral Health 2022, 22, 1–9. [Google Scholar] [CrossRef]
- Estai, M.; Kanagasingam, Y.; Tennant, M.; Bunt, S. A systematic review of the research evidence for the benefits of teledentistry. J. Telemed. Telecare 2017, 24, 147–156. [Google Scholar] [CrossRef] [PubMed]
- Ghai, S. Teledentistry during COVID-19 pandemic. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 933–935. [Google Scholar] [CrossRef] [PubMed]
| Gender | Race | Age |
|---|---|---|
| 78 Female | 52 Hispanic | 42–89 years old |
| 111 Male | 48 White | Mean of 68 years old |
| 41 Asian | ||
| 27 more than one race | ||
| 19 African American | ||
| 2 Pacific Islander |
| Category | Cases |
|---|---|
| Vascular | 2 |
| Pigmented | 3 |
| Traumatic | 4 |
| Infectious | 5 |
| Periodontal or Dental | 6 |
| Anatomic | 2 |
| Candida | 4 |
| Keratotic | 17 |
| Lichen Planus | 11 |
| Hyperplastic | 19 |
| Nicotinic | 33 |
| OPML | 64 |
| OSCC | 19 |
| Value | SE | Lower CI | Upper CI | ||
|---|---|---|---|---|---|
| In-Person | Sensitivity | 0.949 | 0.017 | 0.916 | 0.981 |
| Specificity | 0.692 | 0.128 | 0.443 | 0.942 | |
| False Positive Rate | 0.308 | 0.128 | 0.058 | 0.557 | |
| False Negative Rate | 0.057 | 0.017 | 0.023 | 0.091 | |
| Agreement with Histopathology | 0.926 | 0.019 | 0.889 | 0.963 | |
| Remote | Sensitivity | 0.948 | 0.017 | 0.915 | 0.981 |
| Specificity | 0.625 | 0.121 | 0.389 | 0.861 | |
| False Positive Rate | 0.375 | 0.121 | 0.139 | 0.611 | |
| False Negative Rate | 0.052 | 0.017 | 0.019 | 0.085 | |
| Agreement with Histopathology | 0.921 | 0.020 | 0.882 | 0.959 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nguyen, J.; Yang, S.; Melnikova, A.; Abouakl, M.; Lin, K.; Takesh, T.; Wink, C.; Le, A.; Messadi, D.; Osann, K.; et al. Novel Approach to Improving Specialist Access in Underserved Populations with Suspicious Oral Lesions. Curr. Oncol. 2023, 30, 1046-1053. https://doi.org/10.3390/curroncol30010080
Nguyen J, Yang S, Melnikova A, Abouakl M, Lin K, Takesh T, Wink C, Le A, Messadi D, Osann K, et al. Novel Approach to Improving Specialist Access in Underserved Populations with Suspicious Oral Lesions. Current Oncology. 2023; 30(1):1046-1053. https://doi.org/10.3390/curroncol30010080
Chicago/Turabian StyleNguyen, James, Susan Yang, Anastasya Melnikova, Mary Abouakl, Kairong Lin, Thair Takesh, Cherie Wink, Anh Le, Diana Messadi, Kathryn Osann, and et al. 2023. "Novel Approach to Improving Specialist Access in Underserved Populations with Suspicious Oral Lesions" Current Oncology 30, no. 1: 1046-1053. https://doi.org/10.3390/curroncol30010080
APA StyleNguyen, J., Yang, S., Melnikova, A., Abouakl, M., Lin, K., Takesh, T., Wink, C., Le, A., Messadi, D., Osann, K., & Wilder-Smith, P. (2023). Novel Approach to Improving Specialist Access in Underserved Populations with Suspicious Oral Lesions. Current Oncology, 30(1), 1046-1053. https://doi.org/10.3390/curroncol30010080






