Soft Tissue Sarcomas of the Head and Neck Region with Skull Base/Intracranial Invasion: Review of Surgical Outcomes and Multimodal Treatment Strategies: A Retrospective Case Series
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Cohort Characteristics
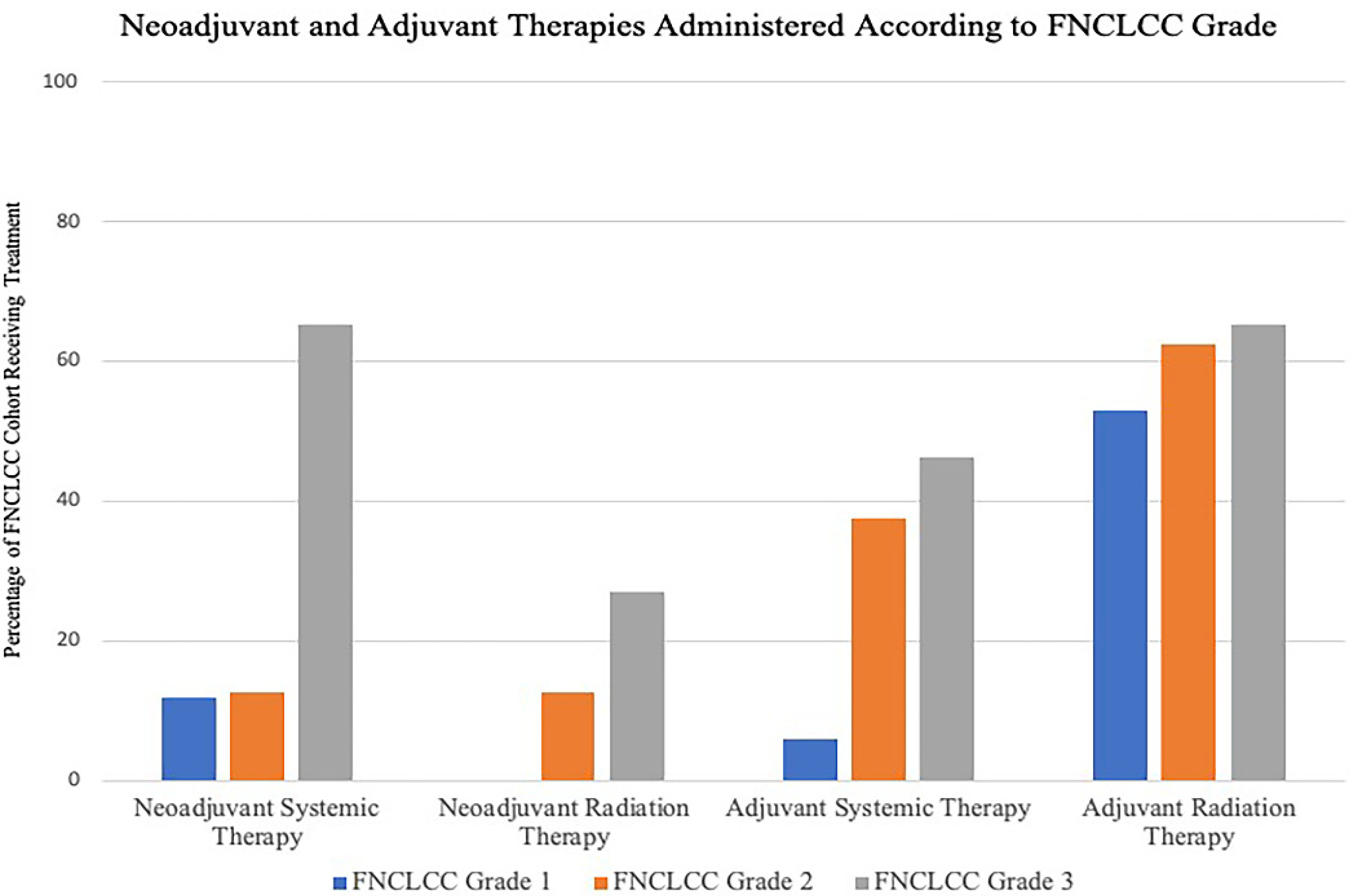
3.2. Histological Breakdown and Multimodality Treatment Strategies
3.3. Tumor Extent and Surgical Strategies
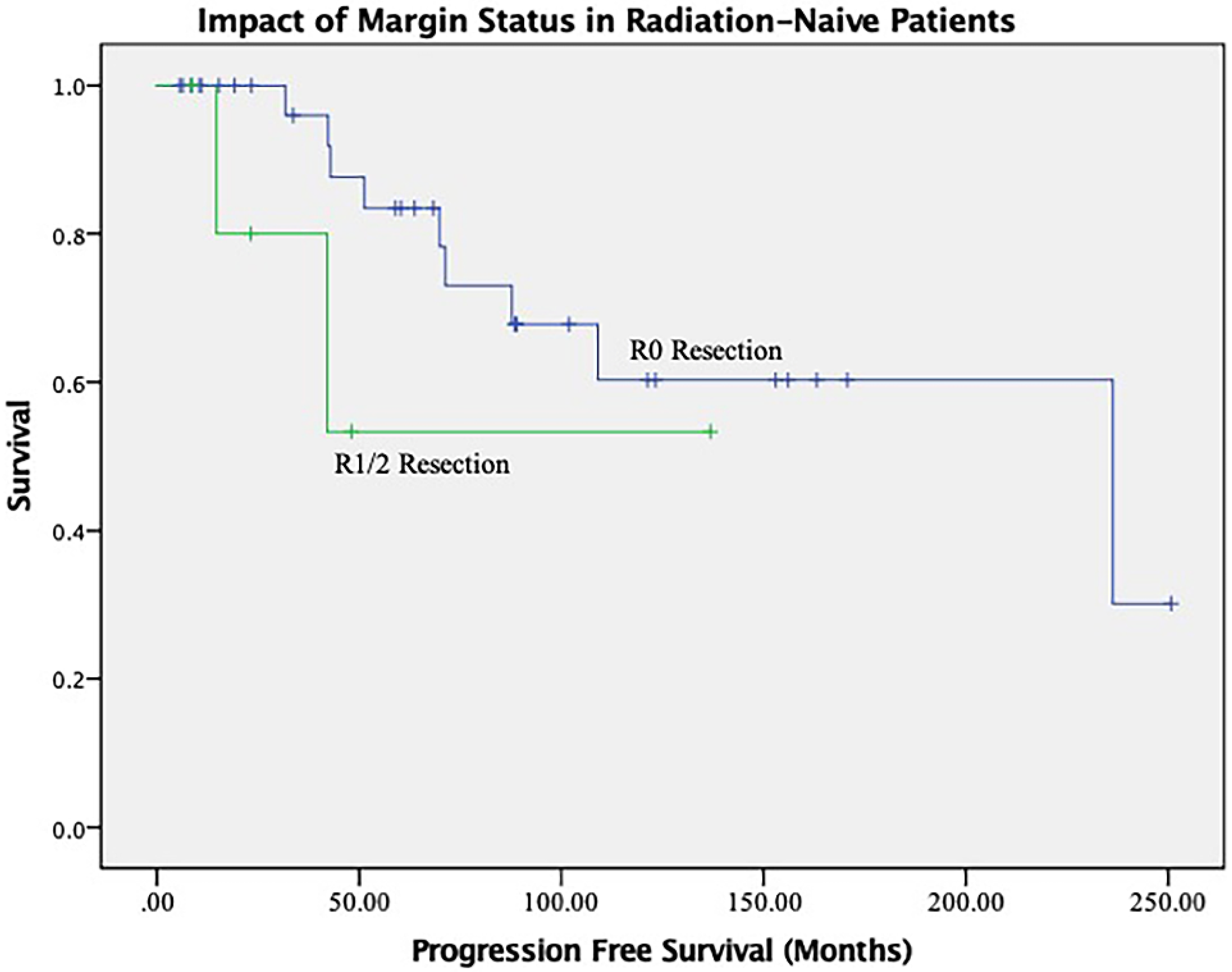
3.4. Recurrence Patterns and Predictors of Long-Term Outcomes
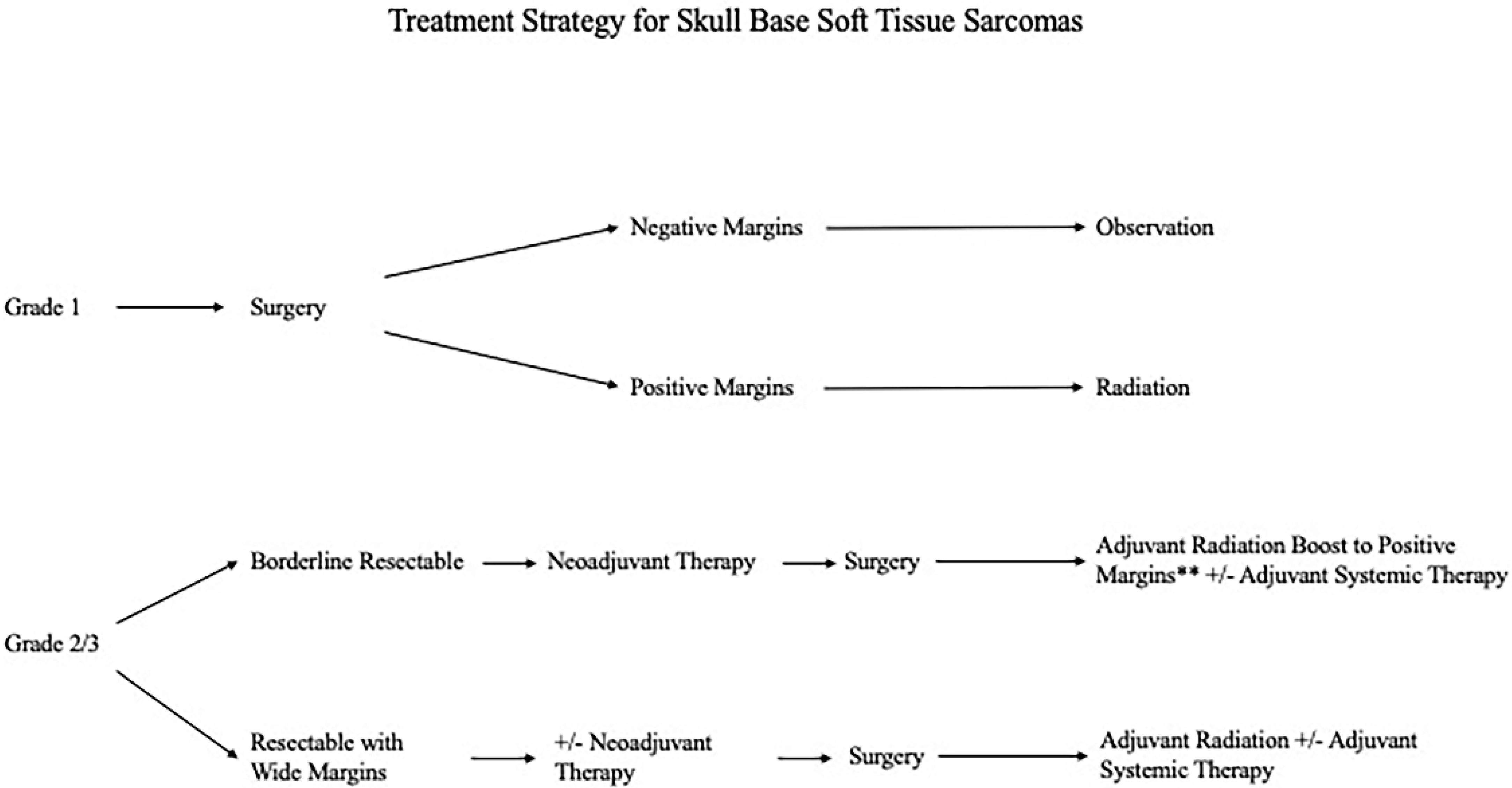
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Oniscu, A.; Salter, D.M. Pathology of soft tissue tumours. Surgery 2011, 29, 51–54. [Google Scholar]
- Bentz, B.G.; Singh, B.; Woodruff, J.; Brennan, M.; Shah, J.P.; Kraus, D. Head and neck soft tissue sarcomas: A multivariate analysis of outcomes. Ann. Surg. Oncol. 2004, 11, 619–628. [Google Scholar] [CrossRef] [PubMed]
- Gullane, P.; Kraus, D.; Weber, R. Soft tissue sarcoma. Head Neck 2002, 24, 296–300. [Google Scholar] [CrossRef] [PubMed]
- Kraus, D.H.; Dubner, S.; Harrison, L.B.; Strong, E.W.; Hajdu, S.I.; Kher, U.; Begg, C.; Brennan, M.F. Prognostic factors for recurrence and survival in head and neck soft tissue sarcomas. Cancer 1994, 74, 697–702. [Google Scholar] [CrossRef]
- Edge, S.; Byrd, D.; Compton, C. American Joint Committee on Cancer Staging Manual; Springer: New York, NY, USA, 2010. [Google Scholar]
- Akagündüz, B.; Telli, T.A.; Goksu, S.S.; Yildirim, H.C.; Ozer, M.; Aydin, S.G.; Ozyurt, N.; Karacin, C.; Paydas, S.; Dogan, M. Assessment of Prognostic Factors and Adjuvant Treatment Modalities in Adult Head and Neck Soft Tissue Sarcoma Patients Treated With Upfront Surgery. Cureus 2021, 13, e13324. [Google Scholar] [CrossRef] [PubMed]
- Lee, N.C.J.; Eskander, A.; Miccio, J.A.; Park, H.S.; Shah, C.; Rutenberg, M.; Hosni, A.; Husain, Z.A. Evaluation of head and neck soft tissue sarcoma 8th edition pathologic staging system and proposal of a novel stage grouping system. Oral Oncol. 2021, 114, 105137. [Google Scholar] [CrossRef] [PubMed]
- Dangoor, A.; Seddon, B.; Gerrand, C.; Grimer, R.; Whelan, J.; Judson, I. UK guidelines for the management of soft tissue sarcomas. Clin. Sarcoma Res. 2016, 6, 20. [Google Scholar] [CrossRef] [PubMed]
- Gil, Z.; Patel, S.G.; Singh, B.; Cantu, G.; Fliss, D.M.; Kowalski, L.P.; Kraus, D.H.; Snyderman, C.; Shah, J.P.; International Collaborative Study Group. Analysis of prognostic factors in 146 patients with anterior skull base sarcoma: An international collaborative study. Cancer 2007, 110, 1033–1041. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, K.; Matsumoto, F.; Miyakita, Y.; Mori, T.; Shimoi, T.; Murakami, N.; Yoshida, A.; Arakawa, A.; Omura, G.; Fukasawa, M.; et al. Impact of Surgical Margin in Skull Base Surgery for Head and Neck Sarcomas. J. Neurol. Surg. B Skull Base 2018, 79, 437–444. [Google Scholar] [PubMed]
- Agha, R.A.; Sohrabi, C.; Mathew, G.; Franchi, T.; Kerwan, A.; O’Neill, N.; PROCESS Group. The PROCESS 2020 Guideline: Updating Consensus Preferred Reporting Of CasESeries in Surgery (PROCESS) Guidelines. Int. J. Surg. 2020, 84, 231–235. [Google Scholar] [CrossRef] [PubMed]
- Guillou, L.; Coindre, J.M.; Bonichon, F.; Nguyen, B.B.; Terrier, P.; Collin, F.; O Vilain, M.; Mandard, A.M.; Le Doussal, V.; Leroux, A.; et al. Comparative study of the National Cancer Institute and French Federation of Cancer Centers Sarcoma Group grading systems in a population of 410 adult patients with soft tissue sarcoma. J. Clin. Oncol. 1997, 15, 350–362. [Google Scholar] [CrossRef] [PubMed]
- de Bree, R.; van der Waal, I.; de Bree, E.; Leemans, C.R. Management of adult soft tissue sarcomas of the head and neck. Oral Oncol. 2010, 46, 786–790. [Google Scholar] [CrossRef] [PubMed]
- Mattavelli, D.; Miceli, R.; Radaelli, S.; Cantu, G.; Barisella, M.; Quattrone, P.; Stacchiotti, S.; Sangalli, C.; Casali, P.G.; Gronchi, A.; et al. Head and neck soft tissue sarcomas: Prognostic factors and outcome in a series of patients treated at a single institution. Ann. Oncol. 2013, 24, 2181–2189. [Google Scholar] [CrossRef] [PubMed]
- NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines): Soft Tissue Sarcomas (Version 4.2019); National Comprehensive Cancer Network September 2019; National Comprehensive Cancer Network: Jenkintown, PA, USA, 2019.
- Jebsen, N.L.; Trovik, C.S.; Bauer, H.C.; Rydholm, A.; Monge, O.R.; Hall, K.S.; Alvegård, T.; Bruland, O.S. Radiotherapy to improve local control regardless of surgical margin and malignancy grade in extremity and trunk wall soft tissue sarcoma: A Scandinavian sarcoma group study. Int. J. Radiat. Oncol. Biol. Phys. 2008, 71, 1196–1203. [Google Scholar] [CrossRef] [PubMed]
- Karasek, K.; Constine, L.S.; Rosier, R. Sarcoma therapy: Functional outcome and relationship to treatment parameters. Int. J. Radiat. Oncol. Biol. Phys. 1992, 24, 651–656. [Google Scholar] [CrossRef]
- Nielsen, O.S.; Cummings, B.; O’Sullivan, B.; Catton, C.; Bell, R.S.; Fornasier, V.L. Preoperative and postoperative irradiation of soft tissue sarcomas: Effect of radiation field size. Int. J. Radiat. Oncol. Biol. Phys. 1991, 21, 1595–1599. [Google Scholar] [CrossRef]
- Sadoski, C.; Suit, H.D.; Rosenberg, A.; Mankin, H.; Efird, J. Preoperative radiation, surgical margins, and local control of extremity sarcomas of soft tissues. J. Surg. Oncol. 1993, 52, 223–230. [Google Scholar] [CrossRef] [PubMed]
- Wilson, A.N.; Davis, A.; Bell, R.S.; O’Sullivan, B.; Catton, C.; Madadi, F.; Kandel, R.; Fornasier, V.L. Local control of soft tissue sarcoma of the extremity: The experience of a multidisciplinary sarcoma group with definitive surgery and radiotherapy. Eur. J. Cancer 1994, 30A, 746–751. [Google Scholar] [CrossRef]
- O’Sullivan, B.; Davis, A.M.; Turcotte, R.; Bell, R.; Catton, C.; Chabot, P.; Wunder, J.; Kandel, R.; Goddard, K.; Sadura, A.; et al. Preoperative versus postoperative radiotherapy in soft-tissue sarcoma of the limbs: A randomised trial. Lancet 2002, 359, 2235–2241. [Google Scholar] [CrossRef]
- Gronchi, A.; Ferrari, S.; Quagliuolo, V.; Martin-Broto, J.M.; Pousa, A.L.; Grignani, G.; Basso, U.; Blay, J.-Y.; Tendero, O.; Beveridge, R.D.; et al. Histotype-tailored neoadjuvant chemotherapy versus standard chemotherapy in patients with high-risk soft-tissue sarcomas (ISG-STS 1001): An international, open-label, randomised, controlled, phase 3, multicentre trial. Lancet Oncol. 2017, 18, 812–822. [Google Scholar] [CrossRef]
| Variable | Univariate PFS Analysis | ||||
|---|---|---|---|---|---|
| Kaplan Meier | Cox Regression | ||||
| Mean | p-Value | HR (95% CI) | p-Value | ||
| Gender | Female | 72.885 | 0.343 | 1.639 (0.585–4.596) | 0.348 |
| Male | 42.610 | ||||
| FNCLCC Grade | FNCLCC (1) | 74.911 | 0.741 | 1.166 (0.664–2.046) | 0.593 |
| FNCLCC (2) | 42.066 | ||||
| FNCLCC (3) | 47.243 | ||||
| Prior Surgery | No | 43.958 | 0.548 | 0.729 (0.259–2.050) | 0.549 |
| Yes | 62.859 | ||||
| Outcome Prior Surgery | STR | 69.377 | 0.970 | 0.954 (0.418–2.176) | 0.912 |
| GTR | 51.137 | ||||
| Unknown | 69.377 | ||||
| Prior Radiation Treatment | No | 76.770 | 0.002 | 6.359 (1.751–23.087) | 0.005 |
| Yes | 24.084 | ||||
| Prior Chemotherapy | No | 67.296 | 0.000 | 15.437 (2.694–88.454) | 0.002 |
| Yes | 15.361 | ||||
| Anterior Fossa | No | 63.233 | 0.545 | 1.360 (0.501–3.691) | 0.547 |
| Yes | 43.424 | ||||
| Middle Fossa | No | 92.800 | 0.086 | 3.040 (0.812–11.374) | 0.099 |
| Yes | 39.358 | ||||
| Posterior Fossa | No | 55.076 | -- | -- | -- |
| Yes | -- | ||||
| Dural Involvement | No | 84.354 | 0.260 | 2.083 (0.567–7.643) | 0.269 |
| Yes | 42.877 | ||||
| Brain Invasion | No | 66.085 | 0.249 | 1.898 (0.628–5.737) | 0.256 |
| Yes | 39.349 | ||||
| Cavernous Sinus Involvement | No | 97.967 | 0.052 | 3.346 (0.924–12.120) | 0.066 |
| Yes | 37.205 | ||||
| Cranial Nerve Involvement | No | 57.392 | 0.849 | 0.905 (0.322–2.543) | 0.850 |
| Yes | 52.471 | ||||
| Resection Status | R2 | 42.066 | 0.610 | 0.663 (0.271–1.622) | 0.368 |
| R1 | 31.361 | ||||
| R0 | 59.393 | ||||
| FNCLCC Tumor Grade | ||||
|---|---|---|---|---|
| Tumor Histology by Differentiation | FNCLCC (1) | FNCLCC (2) | FNCLCC (3) | Total |
| Skeletal muscle tumors | ||||
| Rhabdomyosarcoma | 0 | 0 | 10 | 10 |
| Fibroblastic or myofibroblastic tumors | ||||
| Fibrosarcoma | 3 | 1 | 0 | 4 |
| Hemangiopericytoma | 8 | 5 | 3 | 13 |
| Dermatofibrosarcoma Protuberans | 0 | 1 | 0 | 1 |
| Malignant Fibrous Histiocytoma | 0 | 1 | 4 | 5 |
| Vascular tumors | ||||
| Angiosarcoma | 0 | 0 | 1 | 1 |
| Adipocytic tumors | ||||
| Liposarcoma | 1 | 0 | 5 | 6 |
| Pleomorphic Liposarcoma | 0 | 0 | 0 | 0 |
| Synovial tissue tumors | ||||
| Synovial Sarcoma | 1 | 0 | 2 | 3 |
| Nerve sheath tumors | ||||
| Neurofibrosarcoma | 2 | 0 | 3 | 5 |
| Smooth muscle tumors | ||||
| Leiomyosarcoma | 1 | 0 | 0 | 1 |
| Tumors of Uncertain Differentiation | ||||
| Sarcoma [NOS] | 1 | 0 | 0 | 1 |
| Alveolar Soft Part Sarcoma | 0 | 0 | 1 | 1 |
| Total | 17 | 8 | 26 | 51 |
| Characteristic | Subcategory | Total, n = 51 (% of Cohort) |
|---|---|---|
| Skull base involvement | Anterior fossa | 16 (30.8) |
| Middle fossa | 35 (67.3) | |
| Posterior fossa | 5 (9.8) | |
| Subcranial involvement | Nasal cavity | 6 (11.5) |
| Frontal sinus | 3 (5.8) | |
| Ethmoid sinus | 9 (17.3) | |
| Maxillary sinus | 14 (26.9) | |
| Orbit | 13 (25) | |
| Sphenoid sinus | 9 (17.3) | |
| Infratemporal fossa | 24 (46.2) | |
| Pterygopalatine fossa | 23 (44.2) | |
| Temporal bone | 25 (48.1) | |
| Clivus | 6 (11.5) | |
| Craniocervical junction | 3 (5.8) | |
| Extent of intracranial invasion | Bone | 47 (92.2) |
| Dura | 33 (63.5) | |
| Brain | 16 (30.8) | |
| Cavernous sinus | 19 (36.5) | |
| Cranial nerves | 27 (53) | |
| Arterial | 8 (15.4) | |
| Venous | 23 (45) | |
| Surgical Strategies | ||
| Subtotal resection (STR) | 7 (13.5) | |
| Gross total resection (GTR) with positive margins | 3 (5.8) | |
| Gross total resection (GTR) with negative margins | 41 (80.3) | |
| Surgical Reconstruction | ||
| Primary closure | 37 (71.2) | |
| Rotational Flap | 1 (1.9) | |
| Free Flap Reconstruction | 13 (25.5) | |
| Surgery Complications | ||
| Short Term | Airway compromise, epidural hematoma, post-op pneumocephalus with CSF leak | 3 (5.8) |
| Long Term | Ethmoid defect causing enophthalmos | 2 (3.8) |
| Overall Cohort | FNCLCC Grade 1 | FNCLCC Grade 2 | FNCLCC Grade 3 | |
|---|---|---|---|---|
| N = 51 Patients | ||||
| Mean PFS (months) | 153.788 | 181.320 | 117.895 | 91.885 |
| Recurrence | 17 | 5 | 1 | 11 |
| Local | 10 | 5 | 1 | 4 |
| Distant | 4 | 0 | 0 | 4 |
| Local and distant | 3 | 0 | 0 | 3 |
| Median disease specific survival (DSS) (months) | 94.5 | 170.7 | 89.2 | 73.2 |
| Status at Last Follow-Up | ||||
| Alive | 22 | 13 | 3 | 6 |
| Dead | 29 | 4 | 5 | 20 |
| Variable | Univariate PFS Analysis | ||||
|---|---|---|---|---|---|
| Kaplan Meier | Cox Regression | ||||
| Mean | p-Value | HR (95% CI) | p-Value | ||
| Gender | Female | 162.406 | 0.723 | 1.201 (0.434–3.32) | 0.724 |
| Male | 112.584 | ||||
| FNCLCC Grade | FNCLCC (1) | 181.320 | 0.258 | 1.516 (0.832–2.760) | 0.174 |
| FNCLCC (2) | 117.895 | ||||
| FNCLCC (3) | 91.885 | ||||
| Prior Surgery | No | 108.337 | 0.532 | 0.730 (0.271–1.967) | 0.533 |
| Yes | 161.593 | ||||
| Outcome Prior Surgery | STR | 181.861 | 0.704 | 1.085 (0.503–2.340) | 0.836 |
| GTR | 85.798 | ||||
| Unknown | 121.491 | ||||
| Prior Radiation Treatment | No | 172.890 | 0.014 | 3.645 (1.213–10.953) | 0.021 |
| Yes | 49.991 | ||||
| Prior Chemotherapy | No | 159.495 | 0.174 | 2.166 (0.692–6.748) | 0.184 |
| Yes | 93.530 | ||||
| Anterior Fossa | No | 159.342 | 0.621 | 1.278 (0.482–3.386) | 0.622 |
| Yes | 138.744 | ||||
| Middle Fossa | No | 165.214 | 0.442 | 1.505 (0.527–4.298) | 0.445 |
| Yes | 147.249 | ||||
| Posterior Fossa | No | -- | 0.176 | 0.042 (0.0–50.757) | 0.382 |
| Yes | -- | ||||
| Dural Involvement | No | 174.260 | 0.361 | 1.703 (0.538–5.393) | 0.366 |
| Yes | 106.761 | ||||
| Brain Invasion | No | 169.577 | 0.132 | 2.135 (0.779–5.855) | 0.141 |
| Yes | 80.300 | ||||
| Cavernous Sinus Involvement | No | 204.512 | 0.000 | 11.393 (3.159–41.095) | 0.000 |
| Yes | 49.515 | ||||
| Cranial Nerve Involvement | No | 155.029 | 0.774 | 0.866 (0.324–2.316) | 0.774 |
| Yes | 111.816 | ||||
| Resection Status | R2 | 117.895 | 0.105 | 1.050 (0.483–2.283) | 0.902 |
| R1 | 36.896 | ||||
| R0 | 155.741 | ||||
| Variable | Multivariate OS Analysis | Multivariate PFS Analysis | |||
|---|---|---|---|---|---|
| Cox Regression | Cox Regression | ||||
| HR (95% CI) | p-Value | HR (95% CI) | p-Value | ||
| Prior Radiation Treatment | No | 2.477 (1.066–5.759) | 0.035 | 5.734 | |
| Yes | (0.774–19.530) | 0.005 | |||
| Prior Chemotherapy | No | 2.181 (0.736–6.459) | 0.159 | 2.686 | |
| Yes | (0.766–9.419) | 0.123 | |||
| Yes | |||||
| Posterior Fossa | No | 0.742 (0.134–4.108) | 0.732 | 0.000 | |
| Yes | 0.985 | ||||
| Yes | |||||
| Brain Invasion | No | 2.981 (1.130–7.861) | 0.027 | 0.778 | 0.658 |
| Yes | (0.256–2.364) | ||||
| Cavernous Sinus Involvement | No | 1.872 (0.780–4.494) | 0.161 | 18.712 | |
| Yes | (3.960–88.412) | 0.000 | |||
| Resection Status | R2 | 0.804 (0.465–1.390) | 0.434 | 0.774 | |
| R1 | (0.316–1.891) | 0.574 | |||
| R0 | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Habib, A.; Edem, I.; Bell, D.; Su, S.Y.; Hanna, E.Y.; Kupferman, M.E.; DeMonte, F.; Raza, S.M. Soft Tissue Sarcomas of the Head and Neck Region with Skull Base/Intracranial Invasion: Review of Surgical Outcomes and Multimodal Treatment Strategies: A Retrospective Case Series. Curr. Oncol. 2022, 29, 6540-6550. https://doi.org/10.3390/curroncol29090514
Habib A, Edem I, Bell D, Su SY, Hanna EY, Kupferman ME, DeMonte F, Raza SM. Soft Tissue Sarcomas of the Head and Neck Region with Skull Base/Intracranial Invasion: Review of Surgical Outcomes and Multimodal Treatment Strategies: A Retrospective Case Series. Current Oncology. 2022; 29(9):6540-6550. https://doi.org/10.3390/curroncol29090514
Chicago/Turabian StyleHabib, Ahmed, Idara Edem, Diana Bell, Shirley Y. Su, Ehab Y. Hanna, Michael E. Kupferman, Franco DeMonte, and Shaan M. Raza. 2022. "Soft Tissue Sarcomas of the Head and Neck Region with Skull Base/Intracranial Invasion: Review of Surgical Outcomes and Multimodal Treatment Strategies: A Retrospective Case Series" Current Oncology 29, no. 9: 6540-6550. https://doi.org/10.3390/curroncol29090514
APA StyleHabib, A., Edem, I., Bell, D., Su, S. Y., Hanna, E. Y., Kupferman, M. E., DeMonte, F., & Raza, S. M. (2022). Soft Tissue Sarcomas of the Head and Neck Region with Skull Base/Intracranial Invasion: Review of Surgical Outcomes and Multimodal Treatment Strategies: A Retrospective Case Series. Current Oncology, 29(9), 6540-6550. https://doi.org/10.3390/curroncol29090514





