Major Right Atrial Thrombus Related to Central Venous Catheter Positioning
Abstract
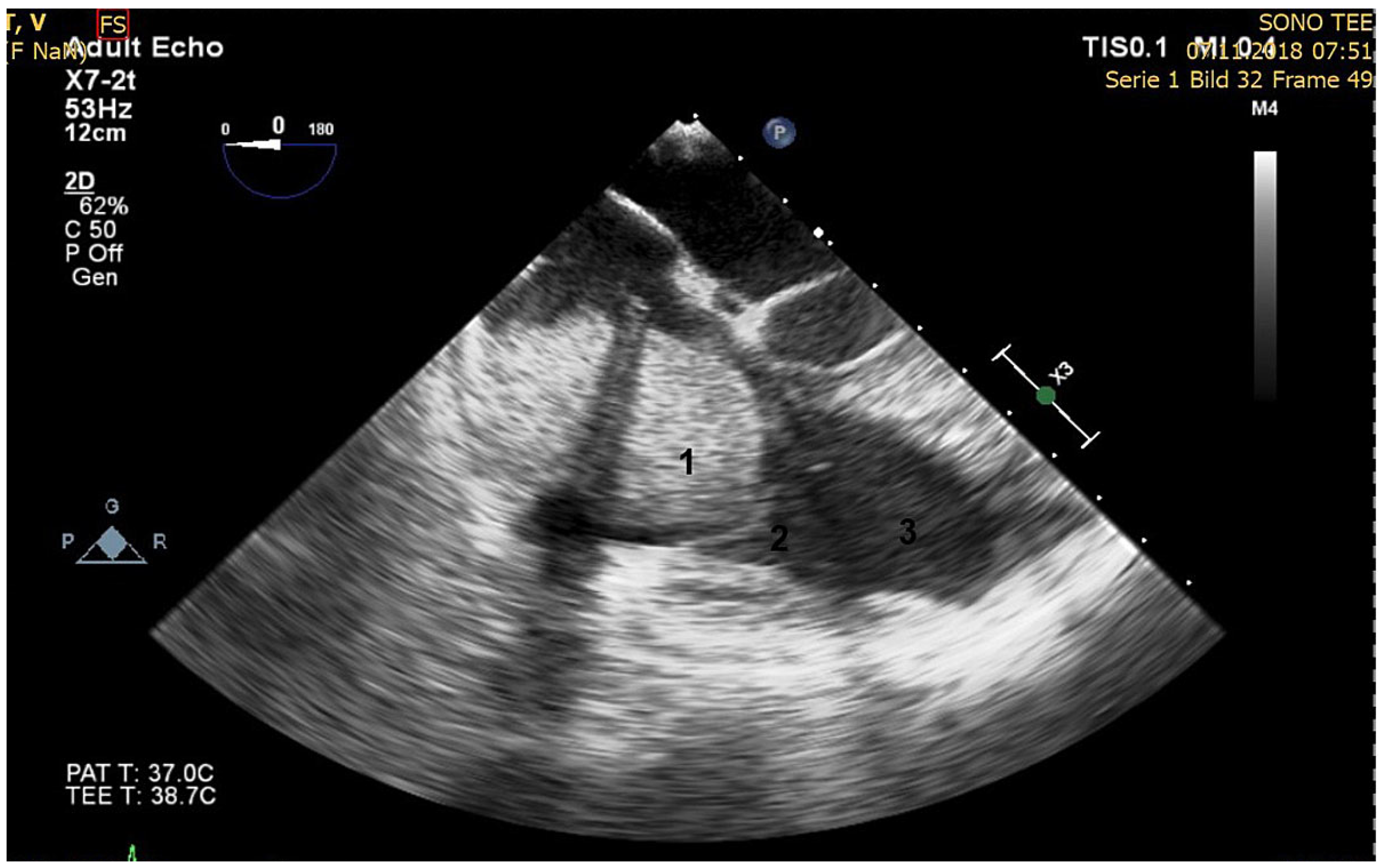
Case description
Discussion
Conflicts of Interest
References
- Forauer, A.R.; Theoharis, C. Histologic changes in the human vein wall adjacent to indwelling central venous catheters. J Vasc Interv Radiol. 2003, 14, 1163–1168. [Google Scholar] [CrossRef] [PubMed]
- Stavroulopoulos, A.; Aresti, V.; Zounis, C. Right atrial thrombi complicating haemodialysis catheters. A meta-analysis of reported cases and a proposal of a management algorithm. Nephrol Dial Transplant. 2012, 27, 2936–2944. [Google Scholar] [CrossRef] [PubMed]
- Parmar, M.S. (F)utility of “routine” postprocedural chest radiograph after hemodialysis catheter (central venous catheter) insertion. J Vasc Access. 2020, 2020. [Google Scholar] [CrossRef] [PubMed]
- Gilon, D.; Schechter, D.; Rein, A.J.; Gimmon, Z.; Or, R.; Rozenman, Y.; et al. Right atrial thrombi are related to indwelling central venous catheter position: insights into time course and possible mechanism of formation. Am Heart J. 1998, 135, 457–462. [Google Scholar] [CrossRef] [PubMed]
- Bayón, J.; Martín, M.; García-Ruíz, J.M.; Rodríguez, C. “We have a tenant” a right atrial thrombus related to a central catheter. Int J Cardiovasc Imaging. 2011, 27, 5–6. [Google Scholar] [CrossRef] [PubMed]
© 2020 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Blank, S.; Henzen, C.; Mueller, X.; Syburra, T. Major Right Atrial Thrombus Related to Central Venous Catheter Positioning. Cardiovasc. Med. 2020, 23, w02104. https://doi.org/10.4414/cvm.2020.02104
Blank S, Henzen C, Mueller X, Syburra T. Major Right Atrial Thrombus Related to Central Venous Catheter Positioning. Cardiovascular Medicine. 2020; 23(2):w02104. https://doi.org/10.4414/cvm.2020.02104
Chicago/Turabian StyleBlank, Sabine, Christoph Henzen, Xavier Mueller, and Thomas Syburra. 2020. "Major Right Atrial Thrombus Related to Central Venous Catheter Positioning" Cardiovascular Medicine 23, no. 2: w02104. https://doi.org/10.4414/cvm.2020.02104
APA StyleBlank, S., Henzen, C., Mueller, X., & Syburra, T. (2020). Major Right Atrial Thrombus Related to Central Venous Catheter Positioning. Cardiovascular Medicine, 23(2), w02104. https://doi.org/10.4414/cvm.2020.02104



