Oral Assessment and Preventive Actions within the Swedish Quality Register Senior Alert: Impact on Frail Older Adults’ Oral Health in a Longitudinal Perspective
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design and Sample
- lived in nursing homes, including special housing for people with neurocognitive disorders;
- had at least two ROAG-J assessments registered in SA with one-year interval, between the years 2011 and 2016.
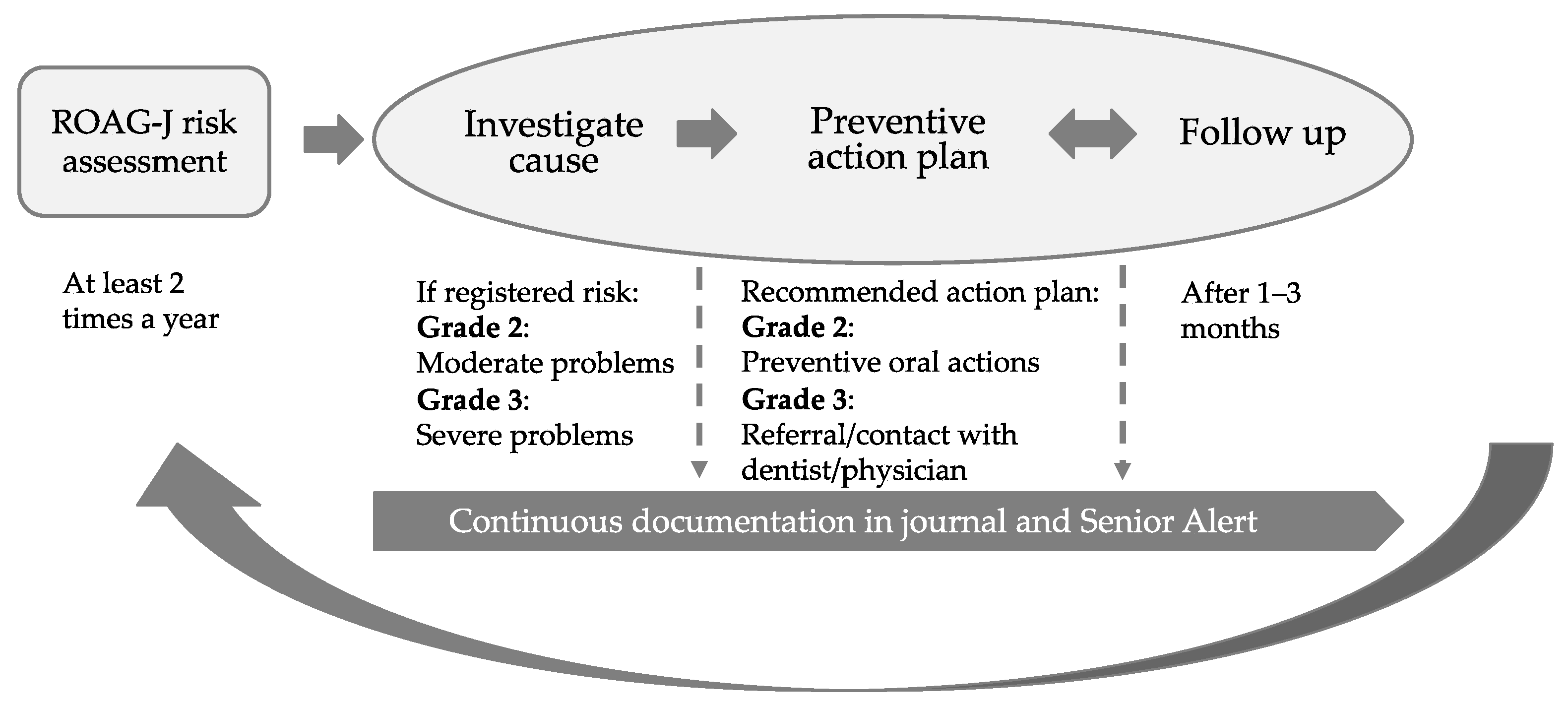
2.2. Data Collection
- Contact or referral to a dentist/physician when at least one grade 3 is registered;
- Assistance with cleaning teeth;
- Assistance with cleaning mucous membranes, tongue and dentures;
- Extra fluoride in addition to ordinary toothpaste;
- Pain relief for lips and/or oral cavity;
- Saliva substitute or moisturising/lubrication of mucous membranes and/or lips;
- Information, instruction and motivation regarding oral health and/or oral hygiene;
- Other oral care measures, such as facilitating practical measures influencing diet and/or swallowing.
2.3. Statistical Methods
2.4. Ethical Consideration
3. Results
3.1. Sample
3.2. Planned Registered Actions
3.3. Difference between the First and the Subsequent Assessments
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- United Nations. World Population Ageing 2019; UN Department of Economic and Social Affairs, Population Division: New York, NY, USA, 2019. [Google Scholar]
- Statistics Sweden. The Future Population of Sweden 2020–2070. Available online: https://www.scb.se/contentassets/9c8e50dfe0484fda8fed2be33e374f46/be0401_2020i70_sm_be18sm2001.pdf (accessed on 6 December 2021). (In Swedish, a Summary in English).
- Norderyd, O.; Koch, G.; Papias, A.; Köhler, A.A.; Helkimo, A.N.; Brahm, C.O.; Lindmark, U.; Lindfors, N.; Mattsson, A.; Rolander, B.; et al. Oral health of individuals aged 3–80 years in Jönkoping, Sweden during 40 years (1973–2013): II. Review of clinical and radiographic findings. Swed. Dent. J. 2015, 39, 69–86. [Google Scholar] [PubMed]
- Petersen, P.E.; Kandelman, D.; Arpin, S.; Ogawa, H. Global oral health of older people—Call for public health action. Community Dent. Health 2010, 27, 257–267. [Google Scholar] [PubMed]
- Tôrres, L.H.; Tellez, M.; Hilgert, J.B.; Hugo, F.N.; de Sousa, M.D.; Ismail, A.I. Frailty, frailty components, and oral health: A systematic review. J. Am. Geriatr. Soc. 2015, 63, 2555–2562. [Google Scholar] [CrossRef] [PubMed]
- Hakeem, F.F.; Bernabé, E.; Sabbah, W. Association between oral health and frailty: A systematic review of longitudinal studies. Gerodontology 2019, 36, 205–215. [Google Scholar] [CrossRef] [PubMed]
- Andersson, P.; Renvert, S.; Sjögren, P.; Zimmerman, M. Dental status in nursing home residents with domiciliary dental care in Sweden. Community Dent Health 2017, 34, 203–207. [Google Scholar] [PubMed]
- SKaPa. Results—Annual Report 2020. Available online: http://www.skapareg.se/resultat/ (accessed on 6 December 2021). (In Swedish).
- Kassebaum, N.J.; Bernabé, E.; Dahiya, M.; Bhandari, B.; Murray, C.J.; Marcenes, W. Global burden of untreated caries: A systematic review and metaregression. J. Dent. Res. 2015, 94, 650–658. [Google Scholar] [CrossRef] [PubMed]
- Pina, G.M.S.; Mota Carvalho, R.; Silva, B.S.F.; Almeida, F.T. Prevalence of hyposalivation in older people: A systematic review and meta-analysis. Gerodontology 2020, 37, 317–331. [Google Scholar] [CrossRef]
- Cassolato, S.F.; Turnbull, R.S. Xerostomia: Clinical aspects and treatment. Gerodontology 2003, 20, 64–77. [Google Scholar] [CrossRef]
- Risheim, H.; Arneberg, P.; Birkhed, D. Oral sugar clearance and root caries prevalence in rheumatic patients with dry mouth symptoms. Caries Res. 1992, 26, 439–444. [Google Scholar] [CrossRef] [PubMed]
- Wong, F.M.F.; Ng, Y.T.Y.; Leung, W.K. Oral health and its associated factors among older institutionalized residents—A systematic review. Int. J. Environ. Res. Public Health 2019, 16, 4132. [Google Scholar] [CrossRef] [Green Version]
- Koistinen, S.; Olai, L.; Ståhlnacke, K.; Fält, A.; Ehrenberg, A. Oral health-related quality of life and associated factors among older people in short-term care. Int. J. Dent. Hyg. 2020, 18, 163–172. [Google Scholar] [CrossRef]
- Porter, J.; Ntouva, A.; Read, A.; Murdoch, M.; Ola, D.; Tsakos, G. The impact of oral health on the quality of life of nursing home residents. Health Qual. Life Outcomes 2015, 13, 102. [Google Scholar] [CrossRef] [Green Version]
- Lertpimonchai, A.; Rattanasiri, S.; Arj-Ong Vallibhakara, S.; Attia, J.; Thakkinstian, A. The association between oral hygiene and periodontitis: A systematic review and meta-analysis. Int. Dent. J. 2017, 67, 332–343. [Google Scholar] [CrossRef] [Green Version]
- Muzurovic, S.; Babajic, E.; Masic, T.; Smajic, R.; Selmanagic, A. The relationship between oral hygiene and oral colonisation with Candida species. Med. Arch. 2012, 66, 415–417. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coll, P.P.; Lindsay, A.; Meng, J.; Gopalakrishna, A.; Raghavendra, S.; Bysani, P.; O’Brien, D. The prevention of infections in older adults: Oral health. J. Am. Geriatr. Soc. 2020, 68, 411–416. [Google Scholar] [CrossRef] [PubMed]
- Khadka, S.; Khan, S.; King, A.; Goldberg, L.R.; Crocombe, L.; Bettiol, S. Poor oral hygiene, oral microorganisms and aspiration pneumonia risk in older people in residential aged care: A systematic review. Age Ageing 2020, 50, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.Z.; Yuan, Y.H.; Liu, H.H.; Li, S.S.; Zhang, B.W.; Chen, W.; An, Z.J.; Chen, S.Y.; Wu, Y.Z.; Han, B.; et al. Epidemiologic relationship between periodontitis and type 2 diabetes mellitus. BMC Oral Health 2020, 20, 204. [Google Scholar] [CrossRef]
- DiBardino, D.M.; Wunderink, R.G. Aspiration pneumonia: A review of modern trends. J. Crit. Care 2015, 30, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Ortega, O.; Sakwinska, O.; Combremont, S.; Berger, B.; Sauser, J.; Parra, C.; Zarcero, S.; Nart, J.; Carrión, S.; Clavé, P. High prevalence of colonization of oral cavity by respiratory pathogens in frail older patients with oropharyngeal dysphagia. Neurogastroenterol. Motil. 2015, 27, 1804–1816. [Google Scholar] [CrossRef] [PubMed]
- Hägglund, P.; Koistinen, S.; Olai, L.; Ståhlnacke, K.; Wester, P.; Levring Jäghagen, E. Older people with swallowing dysfunction and poor oral health are at greater risk of early death. Community Dent. Oral Epidemiol. 2019, 47, 494–501. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Edman, K.; Holmlund, A.; Norderyd, O. Caries disease among an elderly population—A 10-year longitudinal study. Int. J. Dent. Hyg. 2021, 19, 166–175. [Google Scholar] [CrossRef] [PubMed]
- Haag, D.G.; Peres, K.G.; Balasubramanian, M.; Brennan, D.S. Oral conditions and health-related quality of life: A systematic review. J. Dent. Res. 2017, 96, 864–874. [Google Scholar] [CrossRef] [PubMed]
- Kandelman, D.; Petersen, P.E.; Ueda, H. Oral health, general health, and quality of life in older people. Spec. Care Dentist. 2008, 28, 224–236. [Google Scholar] [CrossRef] [PubMed]
- Willumsen, T.; Karlsen, L.; Næss, R.; Bjørntvedt, S. Are the barriers to good oral hygiene in nursing homes within the nurses or the patients? Gerodontology 2012, 29, e748–e755. [Google Scholar] [CrossRef]
- Grönbeck Linden, I.; Hägglin, C.; Gahnberg, L.; Andersson, P. Factors affecting older persons’ ability to manage oral hygiene: A qualitative study. JDR Clin. Trans. Res. 2017, 2, 223–232. [Google Scholar] [CrossRef] [PubMed]
- McNally, M.E.; Matthews, D.C.; Clovis, J.B.; Brillant, M.; Filiaggi, M.J. The oral health of ageing baby boomers: A comparison of adults aged 45–64 and those 65 years and older. Gerodontology 2014, 31, 123–135. [Google Scholar] [CrossRef] [PubMed]
- Forsell, M.; Sjögren, P.; Johansson, O. Need of assistance with daily oral hygiene measures among nursing home resident elderly versus the actual assistance received from the staff. Open Dent. J. 2009, 3, 241–244. [Google Scholar] [CrossRef] [Green Version]
- Forsell, M.; Sjögren, P.; Kullberg, E.; Johansson, O.; Wedel, P.; Herbst, B.; Hoogstraate, J. Attitudes and perceptions towards oral hygiene tasks among geriatric nursing home staff. Int. J. Dent. Hyg. 2011, 9, 199–203. [Google Scholar] [CrossRef] [PubMed]
- Wårdh, I.; Jonsson, M.; Wikström, M. Attitudes to and knowledge about oral health care among nursing home personnel—An area in need of improvement. Gerodontology 2012, 29, e787–e792. [Google Scholar] [CrossRef] [PubMed]
- Jablonski, R.A.; Munro, C.L.; Grap, M.J.; Schubert, C.M.; Ligon, M.; Spigelmyer, P. Mouth care in nursing homes: Knowledge, beliefs, and practices of nursing assistants. Geriatr. Nurs. 2009, 30, 99–107. [Google Scholar] [CrossRef] [Green Version]
- Grönbeck-Linden, I.; Hägglin, C.; Petersson, A.; Linander, P.O.; Gahnberg, L. Discontinued dental attendance among elderly people in Sweden. J. Int. Soc. Prev. Community Dent. 2016, 6, 224–229. [Google Scholar]
- Andersson, P.; Hallberg, I.R.; Renvert, S. Inter-rater reliability of an oral assessment guide for elderly patients residing in a rehabilitation ward. Spec. Care Dentist. 2002, 22, 181–186. [Google Scholar] [CrossRef]
- Eilers, J.; Berger, A.M.; Petersen, M.C. Development, testing, and application of the oral assessment guide. Oncol. Nurs. Forum 1988, 15, 325–330. [Google Scholar]
- Senior Alert. Senior Alert—More than Just a Quality Register. Available online: https://www.senioralert.se/english/ (accessed on 6 December 2021).
- Ribeiro, M.T.; Ferreira, R.C.; Vargas, A.M.; e Ferreira, E.F. Validity and reproducibility of the revised oral assessment guide applied by community health workers. Gerodontology 2014, 31, 101–110. [Google Scholar] [CrossRef]
- Everaars, B.; Weening-Verbree, L.F.; Jerković-Ćosić, K.; Schoonmade, L.; Bleijenberg, N.; de Wit, N.J.; van der Heijden, G. Measurement properties of oral health assessments for non-dental healthcare professionals in older people: A systematic review. BMC Geriatr. 2020, 20, 4. [Google Scholar] [CrossRef] [PubMed]
- National Board of Health and Welfare. Quality Register in Municipal Health and Medical Care—Coverage Rate Comparisons and Results of Co-Operations with the National Board of Health and Welfare’s Register. Available online: https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/ovrigt/2018-2-17.pdf (accessed on 6 December 2021). (In Swedish).
- Bellander, L.; Andersson, P.; Nordvall, D.; Hägglin, C. Oral health among older adults in nursing homes: A survey in a national quality register, the Senior Alert. Nurs. Open 2021, 8, 1262–1274. [Google Scholar] [CrossRef]
- Ek, A.C. Prediction of pressure sore development. Scand. J. Caring Sci. 1987, 1, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Rubenstein, L.Z.; Harker, J.O.; Salvà, A.; Guigoz, Y.; Vellas, B. Screening for undernutrition in geriatric practice: Developing the short-form mini-nutritional assessment (MNA-SF). J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M366–M372. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Backlund, A.; Holmbeck, O.; Kumlien, C.; Axelsson, M. A registry study of nursing assessments, interventions and evaluations according to nutrition for persons living in municipal residential care homes. Nurs. Open 2018, 5, 341–350. [Google Scholar] [CrossRef] [Green Version]
- Gabre, P.; Moberg Sköld, U.; Birkhed, D. Simplified methods of topical fluoride administration: Effects in individuals with hyposalivation. Spec. Care Dentist. 2013, 33, 111–117. [Google Scholar] [CrossRef]
- Marinho, V.C.; Chong, L.Y.; Worthington, H.V.; Walsh, T. Fluoride mouthrinses for preventing dental caries in children and adolescents. Cochrane Database Syst. Rev. 2016, 7, Cd002284. [Google Scholar] [PubMed]
- Ekstrand, K.R.; Poulsen, J.E.; Hede, B.; Twetman, S.; Qvist, V.; Ellwood, R.P. A randomized clinical trial of the anti-caries efficacy of 5000 compared to 1450 ppm fluoridated toothpaste on root caries lesions in elderly disabled nursing home residents. Caries Res. 2013, 47, 391–398. [Google Scholar] [CrossRef]
- Petersen, P.E.; Ogawa, H. Promoting oral health and quality of life of older people—The need for public health action. Oral Health Prev. Dent. 2018, 16, 113–124. [Google Scholar] [PubMed]
- Sonde, L.; Emami, A.; Kiljunen, H.; Nordenram, G. Care providers’ perceptions of the importance of oral care and its performance within everyday caregiving for nursing home residents with dementia. Scand. J. Caring Sci. 2011, 25, 92–99. [Google Scholar] [CrossRef] [PubMed]
- Villarosa, A.R.; Clark, S.; Villarosa, A.C.; Patterson Norrie, T.; Macdonald, S.; Anlezark, J.; Srinivas, R.; George, A. Promoting oral health care among people living in residential aged care facilities: Perceptions of care staff. Gerodontology 2018, 35, 177–184. [Google Scholar] [CrossRef]
- Lindqvist, L.; Seleskog, B.; Wårdh, I.; von Bültzingslöwen, I. Oral care perspectives of professionals in nursing homes for the elderly. Int. J. Dent. Hyg. 2013, 11, 298–305. [Google Scholar] [CrossRef]
- National Board of Health and Welfare. Mapping of Obstacles to Collaboration between Dental Care and Health Care. Available online: https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/ovrigt/2019-10-6428.pdf (accessed on 6 December 2021). (In Swedish).
- Chalmers, J.M. Behavior management and communication strategies for dental professionals when caring for patients with dementia. Spec. Care Dentist. 2000, 20, 147–154. [Google Scholar] [CrossRef] [PubMed]
- Ástvaldsdóttir, A.; Boström, A.M.; Davidson, T.; Gabre, P.; Gahnberg, L.; Sandborgh Englund, G.; Skott, P.; Ståhlnacke, K.; Tranaeus, S.; Wilhelmsson, H.; et al. Oral health and dental care of older persons—A systematic map of systematic reviews. Gerodontology 2018, 35, 290–304. [Google Scholar] [CrossRef]
- Miegel, K.; Wachtel, T. Improving the oral health of older people in long-term residential care: A review of the literature. Int. J. Older People Nurs. 2009, 4, 97–113. [Google Scholar] [CrossRef]

| Item | Grade 0 | Grade 1 | Grade 2 | Grade 3 |
|---|---|---|---|---|
| VOICE | Not applicable to judge | Normal | Dry, hoarse, smacking | Difficulty speaking |
| LIPS | - | Smooth, bright red, moist | Dry, cracked, sore corners of the mouth | Ulcerated, bleeding |
| MUCOUS MEMBRANES | - | Bright red, moist | Red, dry, or areas of discolouration, coating | Wounds with or without bleeding, blisters |
| TONGUE | - | Pink, moist with papillae | No papillae, red, dry, coating | Ulcers with or without bleeding, blistering |
| GUMS | No gums, only mucous membranes | Light red and solid | Swollen, reddened | Spontaneous bleeding |
| TEETH | No natural teeth | Clean, no visible coating or food debris | Coating or food debris locally | Coating or food debris generally, broken teeth |
| DENTURES | No prosthetics | Clean, functioning | Coating or food debris | Not used or malfunctioning |
| SALIVA | - | Runs freely | Runs sluggishly | Does not run at all |
| SWALLOWING | Not applicable to judge | Unimpeded swallowing | Minor swallowing problems | Pronounced swallowing problems |
| n | % | |
|---|---|---|
| Age | ||
| 65–74 | 5485 | 10.4 |
| 75–84 | 17,610 | 33.4 |
| 85–94 | 26,020 | 49.3 |
| ≥95 | 3625 | 6.9 |
| Gender | ||
| Female | 36,030 | 68.3 |
| Male | 16,710 | 31.7 |
| Physical condition 1 | ||
| Good | 26,504 | 53.3 |
| Fair | 20,939 | 42.1 |
| Poor | 2062 | 4.1 |
| Very bad | 234 | 0.5 |
| Neuropsychological problems 2 | ||
| No problems | 15,308 | 30.0 |
| Mild dementia/depression | 24,978 | 49.0 |
| Severe dementia/depression | 10,689 | 21.0 |
| ROAG Item | Risk (Grade 2 and/or 3) n 21,394 | Severe Risk (Grade 3) n 6147 | ||
|---|---|---|---|---|
| n | % | n | % | |
| Voice | 4053 | 7.7 | 1230 | 2.3 |
| Lips | 3178 | 6.0 | 37 | 0.1 |
| Mucous membranes | 3269 | 6.2 | 257 | 0.5 |
| Tongue | 3372 | 6.4 | 86 | 0.2 |
| Teeth 1 | 10,770 | 26.9 | 2568 | 6.4 |
| Gums 2 | 4079 | 8.5 | 519 | 1.1 |
| Dentures 3 | 3427 | 15.2 | 1376 | 6.1 |
| Saliva | 4133 | 7.8 | 172 | 0.3 |
| Swallowing | 5412 | 10.3 | 1237 | 2.3 |
| Gender | Age | |||||||
|---|---|---|---|---|---|---|---|---|
| Men n 7145 | Women n 14,249 | 65–74 n 2575 | 75–84 n 7332 | 85–94 n 10,109 | >95 n 1378 | |||
| Registered Actions When Detected Risk | % | % | p | % | % | % | % | p 1 |
| Assistance with cleaning teeth 2 | 45.5 | 43.0 | 0.002 | 46.9 | 47.0 | 41.1 | 39.8 | <0.001 |
| Assistance with cleaning mucous membranes, tongue, dentures | 18.8 | 19.0 | 0.725 | 16.3 | 18.4 | 19.4 | 22.4 | <0.001 |
| Extra fluoride | 6.0 | 5.9 | 0.736 | 6.8 | 6.6 | 5.3 | 4.9 | <0.001 |
| Pain relief lips and/or oral cavity | 0.3 | 0.4 | 0.186 | 0.4 | 0.8 | 0.7 | 0.6 | 0.884 |
| Saliva substitute or moisturizing/lubrication | 25.3 | 31.8 | <0.001 | 27.7 | 28.8 | 30.3 | 31.8 | <0.001 |
| Information, instruction and motivation | 8.6 | 7.6 | 0.018 | 8.9 | 7.5 | 8.1 | 7.7 | 0.382 |
| Other oral care measures | 6.2 | 6.6 | 0.274 | 6.1 | 6.4 | 6.6 | 6.0 | 0.693 |
| Contact or referral to a dentist/physician 3 | 15.2 | 11.1 | <0.001 | 13.4 | 13.2 | 11.5 | 13.5 | 0.103 |
| Individuals n (%) | Assessments 1 | Risk (Grade 2 and/or 3) | Severe Risk (Grade 3) | ||||
|---|---|---|---|---|---|---|---|
| n | % | p | n | % | p | ||
| 52,740 (100) | 1 | 21,394 | 40.6 | 6147 | 11.7 | ||
| 2 | 22,440 | 42.5 | <0.001 | 6733 | 12.8 | <0.001 | |
| 23,443 (44.5) | 1 | 9380 | 40.0 | 2652 | 11.3 | ||
| 2 | 9639 | 41.1 | 2793 | 11.9 | |||
| 3 | 10,255 | 43.7 | <0.001 | 3223 | 13.7 | <0.001 | |
| 7703 (14.6) | 1 | 3126 | 40.6 | 880 | 11.4 | ||
| 2 | 3145 | 40.8 | 897 | 11.6 | |||
| 3 | 3218 | 41.8 | 994 | 12.9 | |||
| 4 | 3492 | 45.3 | <0.001 | 1178 | 15.3 | <0.001 | |
| 999 (1.9) | 1 | 364 | 36.4 | 100 | 10.0 | ||
| 2 | 376 | 37.6 | 108 | 10.8 | |||
| 3 | 403 | 40.3 | 135 | 13.5 | |||
| 4 | 416 | 41.6 | 137 | 13.7 | |||
| 5 | 429 | 42.9 | <0.001 | 141 | 14.1 | <0.001 | |
| ROAG-J Risk (Grade 2 and/or 3) | ROAG-J Severe Risk (Grade 3) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Individuals n | Assessments 1 | Risk n | No Risk n | Risk n | No Risk n | ||||
| Still Risk “Unchanged” n (%) | No Risk “Better” n (%) | Still No Risk “Unchanged” n (%) | Risk “Worse” n (%) | Still Risk “Unchanged” n (%) | No Risk “Better” n (%) | Still No Risk “Unchanged” n (%) | Risk “Worse” n (%) | ||
| 52,740 | 1 2 | 21,394 | 31,346 | 6147 | 46,593 | ||||
| 16,706 (78.1) | 4688 (21.9) | 25,612 (81.7) | 5734 (18.3) | 4009 (65.2) | 2138 (34.8) | 43,869 (94.2) | 2724 (5.8) | ||
| 23,443 | 1 3 | 9380 | 14,063 | 2652 | 20,791 | ||||
| 6548 (69.8) | 2832 (30.2) | 10,356 (73.6) | 3707 (26.4) | 1398 (52.7) | 1254 (47.3) | 18,966 (91.2) | 1825 (8.8) | ||
| 7703 | 1 4 | 3126 | 4577 | 880 | 6823 | ||||
| 2039 (65.2) | 1087 (34.8) | 3124 (68.3) | 1453 (31.7) | 405 (46.0) | 475 (54.0) | 6050 (88.7) | 773 (11.3) | ||
| 999 | 1 5 | 364 | 635 | 100 | 899 | ||||
| 217 (59.6) | 147 (40.4) | 423 (66.6) | 212 (33.4) | 38 (38.0) | 62 (62.0) | 796 (88.5) | 103 (11.5) | ||
| ROAG-J Risk in the First Assessment | No ROAG-J Risk in the Subsequent Assessment | |||||
|---|---|---|---|---|---|---|
| n | Registered Actions n | “Better” % | No Registered Actions n | “Better” % | p | |
| Risk | 21,394 | 13,285 | 22.0 | 8109 | 21.7 | 0.645 |
| Voice | 4053 | 2511 | 39.0 | 1542 | 36.0 | 0.057 |
| Lips | 3178 | 2068 | 49.0 | 1110 | 44.7 | 0.021 |
| Mucous membranes | 3269 | 2104 | 43.2 | 1165 | 42.3 | 0.658 |
| Tongue | 3372 | 2172 | 45.2 | 1200 | 40.8 | 0.014 |
| Teeth | 10,770 | 6909 | 26.9 | 3861 | 26.5 | 0.617 |
| Gums | 4079 | 2695 | 36.3 | 1384 | 36.4 | 0.918 |
| Dentures | 3427 | 2111 | 41.0 | 1316 | 36.8 | 0.015 |
| Saliva | 4133 | 2674 | 40.1 | 1459 | 38.2 | 0.244 |
| Swallowing | 5412 | 3269 | 28.1 | 2143 | 28.7 | 0.579 |
| Severe risk 1 | 6147 | 3707 | 35.5 | 2440 | 33.7 | 0.147 |
| Contact or referral 2 | 6147 | 772 | 41.7 | 5375 | 33.8 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bellander, L.; Andersson, P.; Wijk, H.; Hägglin, C. Oral Assessment and Preventive Actions within the Swedish Quality Register Senior Alert: Impact on Frail Older Adults’ Oral Health in a Longitudinal Perspective. Int. J. Environ. Res. Public Health 2021, 18, 13075. https://doi.org/10.3390/ijerph182413075
Bellander L, Andersson P, Wijk H, Hägglin C. Oral Assessment and Preventive Actions within the Swedish Quality Register Senior Alert: Impact on Frail Older Adults’ Oral Health in a Longitudinal Perspective. International Journal of Environmental Research and Public Health. 2021; 18(24):13075. https://doi.org/10.3390/ijerph182413075
Chicago/Turabian StyleBellander, Lisa, Pia Andersson, Helle Wijk, and Catharina Hägglin. 2021. "Oral Assessment and Preventive Actions within the Swedish Quality Register Senior Alert: Impact on Frail Older Adults’ Oral Health in a Longitudinal Perspective" International Journal of Environmental Research and Public Health 18, no. 24: 13075. https://doi.org/10.3390/ijerph182413075
APA StyleBellander, L., Andersson, P., Wijk, H., & Hägglin, C. (2021). Oral Assessment and Preventive Actions within the Swedish Quality Register Senior Alert: Impact on Frail Older Adults’ Oral Health in a Longitudinal Perspective. International Journal of Environmental Research and Public Health, 18(24), 13075. https://doi.org/10.3390/ijerph182413075






