The Relation between Masticatory Function and Nutrition in Older Individuals, Dependent on Supportive Care for Daily Living
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Process
2.2. The Study Group Participants
2.2.1. Inclusion Criteria
2.2.2. Exclusion Criteria
2.3. Ethical Considerations
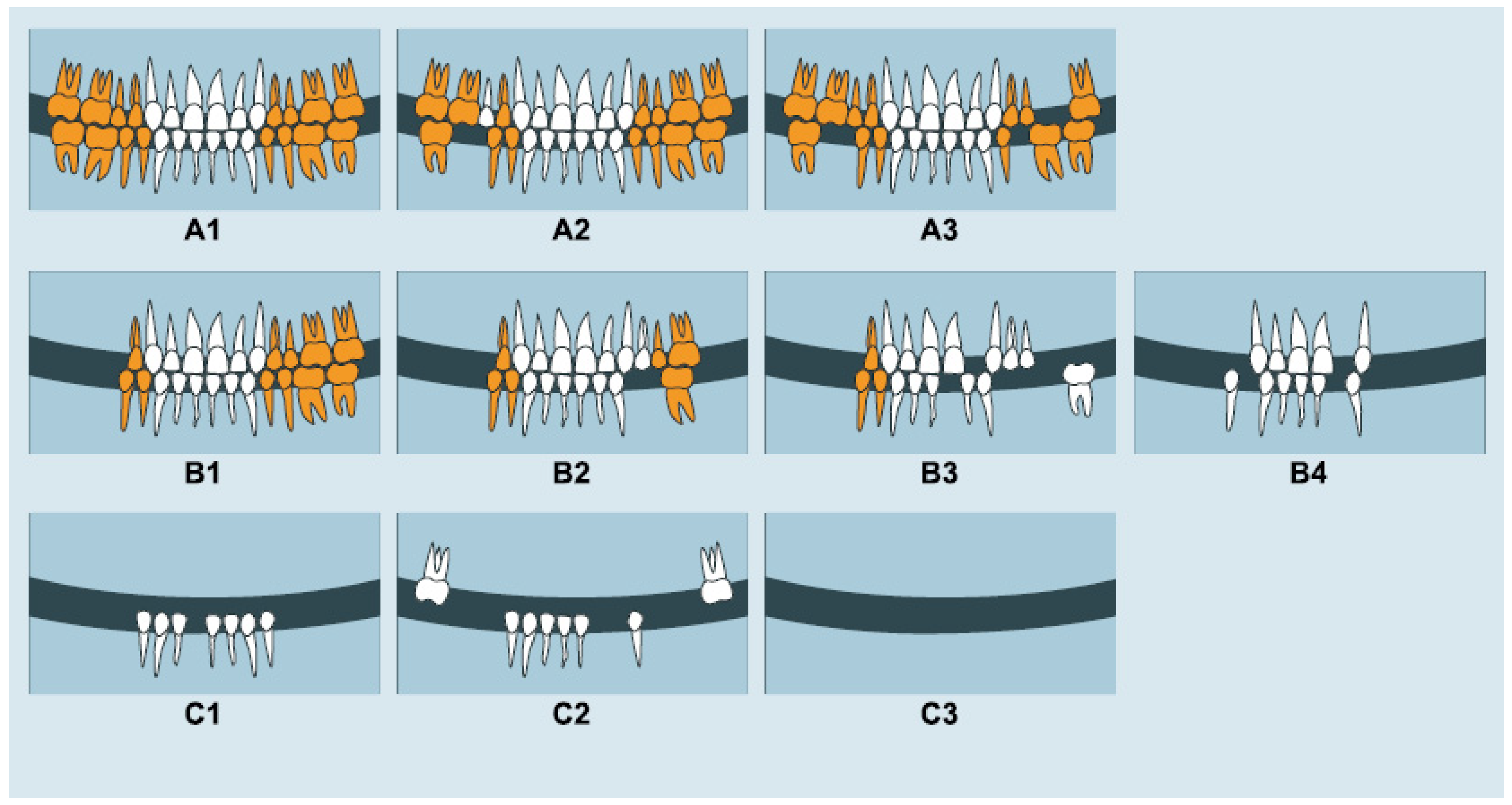
2.4. Masticatory Performance
2.5. Masticatory Ability
2.5.1. Items from OHaBF
2.5.2. Items from GOHAI
2.6. Nutritional Status
2.7. Statistical Methods
3. Results
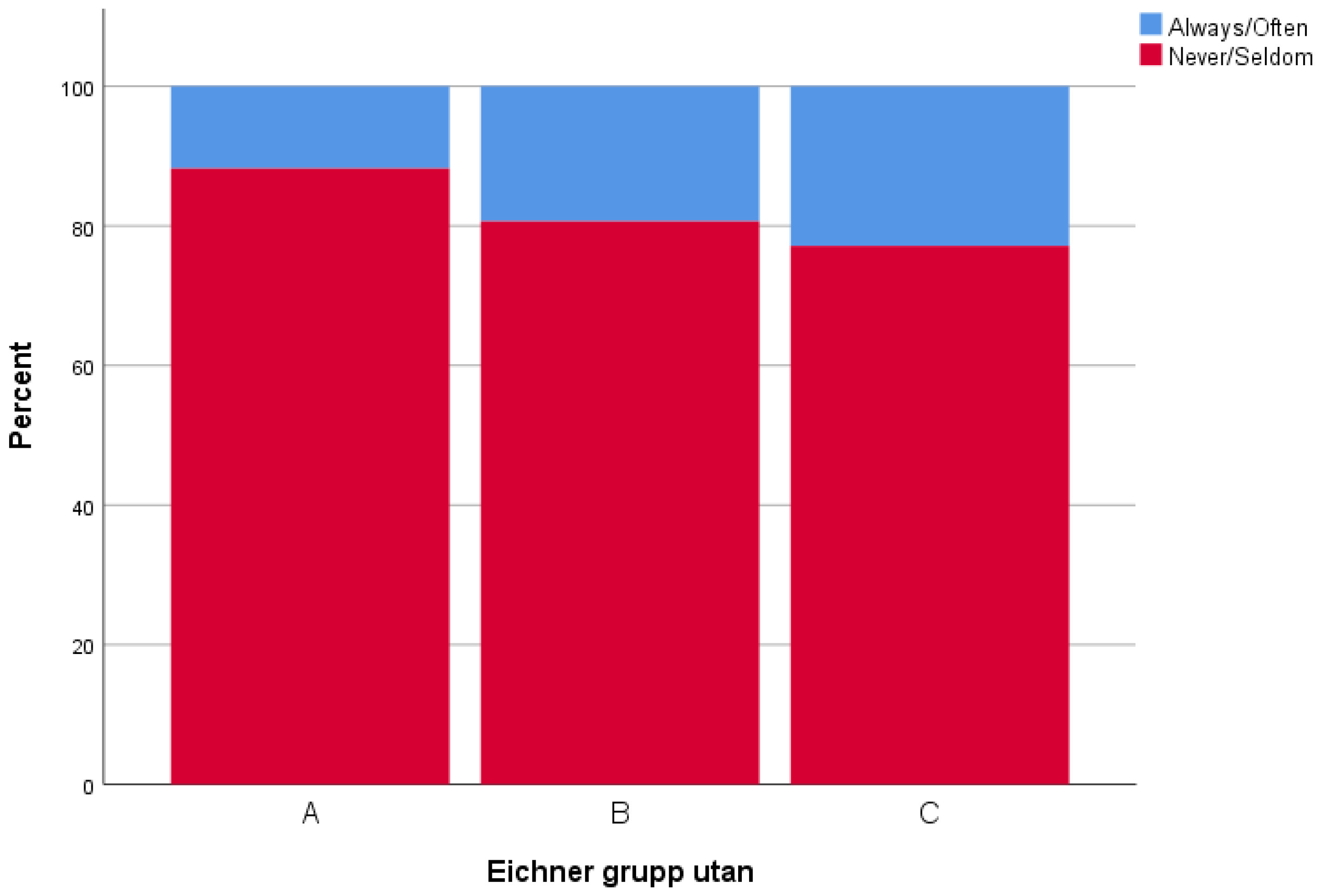
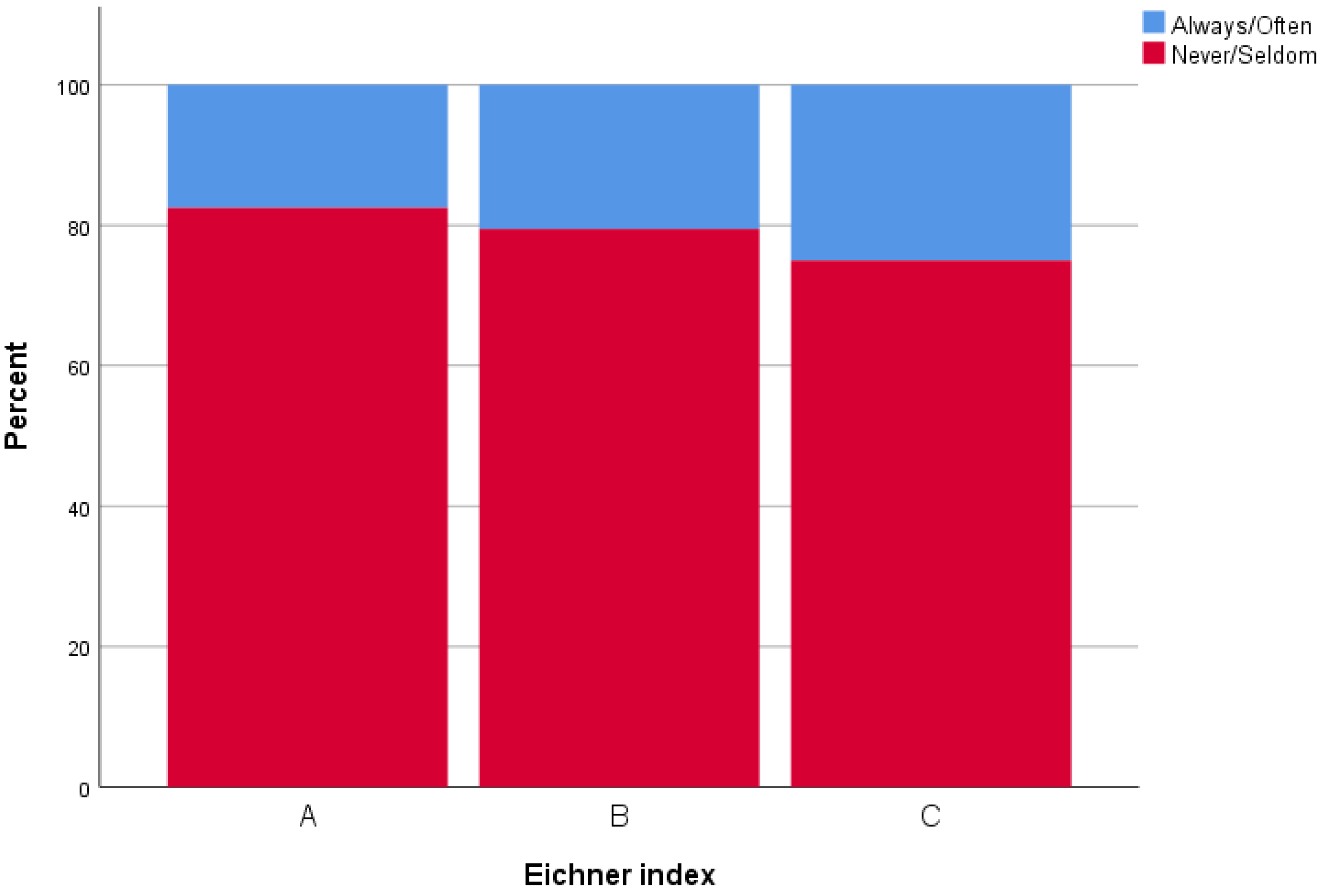
3.1. Masticatory Performance and Masticatory Ability
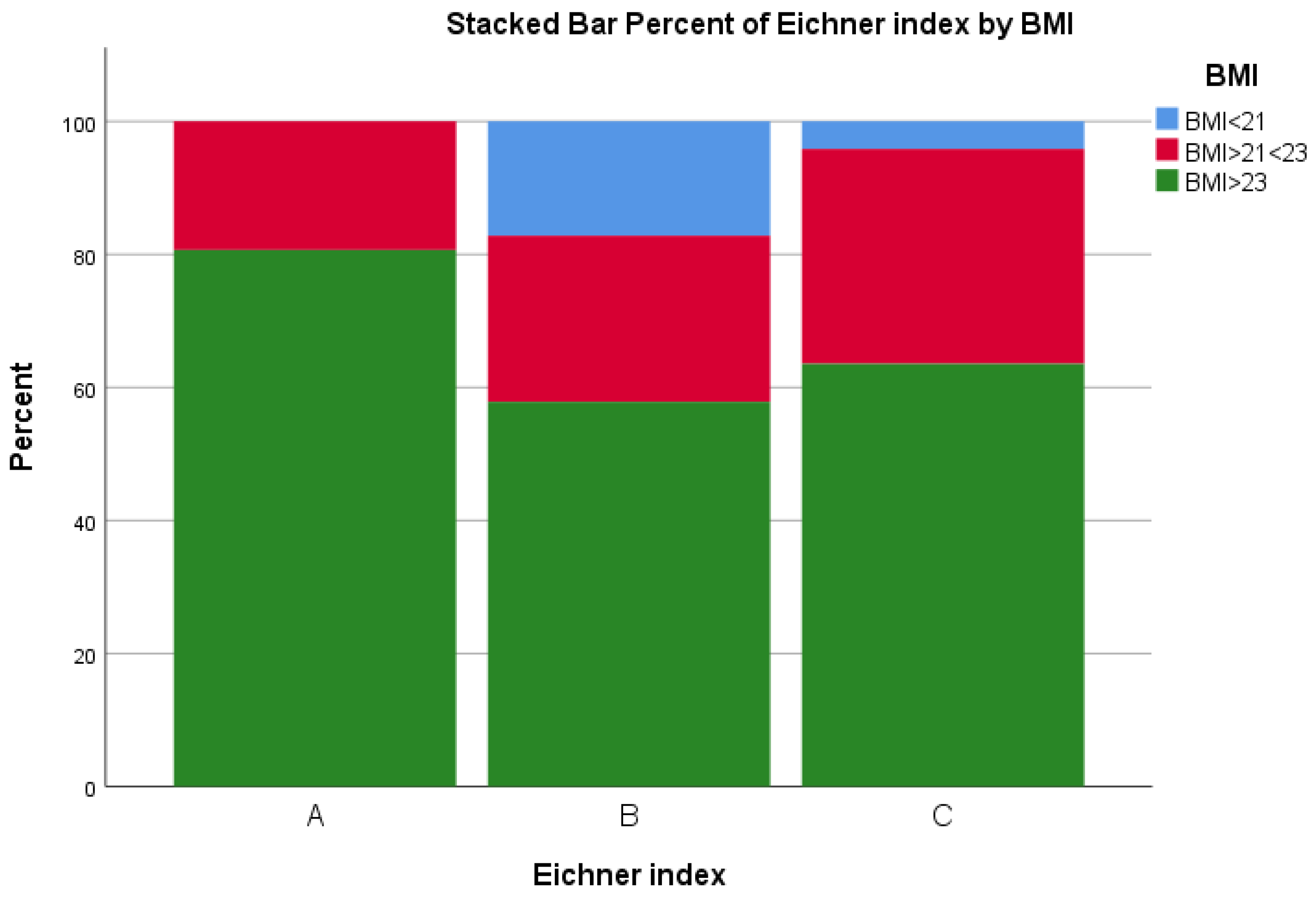
3.2. Masticatory Performance and Nutritional Variables
3.3. Masticatory Ability and Nutritional Variables
4. Discussion
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Strömberg, E.; Holmèn, A.; Hagman-Gustafsson, M.-L.; Gabre, P.; Wårdh, I. Oral health-related quality-of-life in homebound elderly dependent on moderate and substantial supportive care for daily living. Acta Odontol. Scand. 2013, 71, 771–777. [Google Scholar] [CrossRef] [PubMed]
- Volkert, D.; Beck, A.M.; Cederholm, T.; Cruz-Jentoft, A.; Goisser, S.; Hooper, L.; Bischoff, S.C. ESPEN guideline on clinical nutrition and hydration in geriatrics. Clin. Nutr. 2019, 38, 10–47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agarwal, E.; Miller, M.; Yaxley, A.; Isenring, E. Malnutrition in the elderly: A narrative review. Maturitas 2013, 76, 296–302. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cruz-Jentoft, A.J.; Baeyens, J.P.; Bauer, J.M.; Boirie, Y.; Cederholm, T.; Landi, F.; Zamboni, M. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 2010, 39, 412–423. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clegg, A.; Young, J.; Iliffe, S.; Rikkert, M.O.; Rockwood, K. Frailty in elderly people. Lancet 2013, 381, 752–762. [Google Scholar] [CrossRef] [Green Version]
- Castrejon-Perez, R.C.; Borges-Yanez, S.A.; Gutierrez-Robledo, L.M.; Avila-Funes, J.A. Oral health conditions and frailty in Mexican community-dwelling elderly: A cross sectional analysis. BMC Public Health 2012, 12, 773. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- de Andrade, F.B.; Lebrao, M.L.; Santos, J.L.; Duarte, Y.A. Relationship between oral health and frailty in community-dwelling elderly individuals in Brazil. J. Am. Geriatr. Soc. 2013, 61, 809–814. [Google Scholar] [CrossRef]
- Kamdem, B.; Seematter-Bagnoud, L.; Botrugno, F.; Santos-Eggimann, B. Relationship between oral health and Fried’s frailty criteria in community-dwelling older persons. BMC Geriatr. 2017, 17, 174. [Google Scholar] [CrossRef] [Green Version]
- Lin, C.S. Revisiting the link between cognitive decline and masticatory dysfunction. BMC Geriatr. 2018, 18, 5. [Google Scholar] [CrossRef]
- Tada, A.; Miura, H. Systematic review of the association of mastication with food and nutrient intake in the independent elderly. Arch. Gerontol. Geriatr. 2014, 59, 497–505. [Google Scholar] [CrossRef]
- Sheiham, A.; Steele, J.G.; Marcenes, W.; Lowe, C.; Finch, S.; Bates, C.J.; Walls, A.W.G. The relationship among dental status, nutrient intake, and nutritional status in older people. J. Dent. Res. 2001, 80, 408–413. [Google Scholar] [CrossRef] [PubMed]
- do Nascimento TL, H.; Liberalesso, N.A.; Balbinot, H.J.; Neves, H.F. Association between underweight and overweight/obesity with oral health among independently living Brazilian elderly. Nutrition 2013, 29, 152–157. [Google Scholar] [CrossRef] [PubMed]
- N’Gom, P.I.; Woda, A. Influence of impaired mastication on nutrition. J. Prosthet. Dent. 2002, 87, 667–673. [Google Scholar] [CrossRef]
- Semba, R.D.; Blaum, C.S.; Bartali, B.; Xue, Q.L. Denture use, malnutrition, frailty, and mortality among older women living in the community. J. Nutr. Health Aging 2006, 10, 161–167. [Google Scholar] [PubMed]
- Tsai, A.C.; Chang, T.L. Association of dental prosthetic condition with food consumption and the risk of malnutrition and follow-up 4-year mortality risk in elderly Taiwanese. J. Nutr. Health Aging 2011, 15, 265–270. [Google Scholar] [CrossRef] [PubMed]
- Huppertz, V.A.L.; van der Putten, G.J.; Halfens, R.J.G.; Schols, J.; de Groot, L. Association between Malnutrition and Oral Health in Dutch Nursing Home Residents: Results of the LPZ Study. J. Am. Med. Dir. Assoc. 2017, 18, 948–954. [Google Scholar] [CrossRef]
- Astvaldsdottir, A.; Bostrom, A.M.; Davidson, T.; Gabre, P.; Gahnberg, L.; Sandborgh Englund, G.; Nilsson, M. Oral health and dental care of older persons—A systematic map of systematic reviews. Gerodontology 2018, 35, 290–304. [Google Scholar] [CrossRef]
- van der Bilt, A. Assessment of mastication with implications for oral rehabilitation: A review. J. Oral Rehabil. 2011, 38, 754–780. [Google Scholar] [CrossRef]
- Pedroni-Pereira, A.; Marquezin, M.C.S.; Araujo, D.S.; Pereira, L.J.; Bommarito, S.; Castelo, P.M. Lack of agreement between objective and subjective measures in the evaluation of masticatory function: A preliminary study. Physiol. Behav. 2018, 184, 220–225. [Google Scholar] [CrossRef]
- Takagi, D.; Watanabe, Y.; Edahiro, A.; Ohara, Y.; Murakami, M.; Murakami, K.; Hirano, H. Factors affecting masticatory function of community-dwelling older people: Investigation of the differences in the relevant factors for subjective and objective assessment. Gerodontology 2017, 34, 357–364. [Google Scholar] [CrossRef]
- van der Bilt, A.; Olthoff, L.W.; Bosman, F.; Oosterhaven, S.P. Chewing performance before and after rehabilitation of post-canine teeth in man. J. Dent. Res. 1994, 73, 1677–1683. [Google Scholar] [CrossRef] [PubMed]
- Pfeiffer, E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J. Am. Geriatr. Soc. 1975, 23, 433–441. [Google Scholar] [CrossRef] [PubMed]
- Eichner, K. Über eine Gruppeneinteilung der Lückengebissefür die Prothetik. Dtsch. Zahnarztl. Z. 1955, 10, 1831–1834. [Google Scholar]
- Lantto, A.; Lundqvist, R.; Wårdh, I. Oral Status and Prosthetic Treatment Needs in Functionally Impaired and Elderly Individuals. Int. J. Prosthodont. 2018, 31, 494–501. [Google Scholar] [CrossRef] [Green Version]
- Atchison, K.A.; Dolan, T.A. Development of the Geriatric Oral Health Assessment Index. J. Dent. Educ. 1990, 54, 680–687. [Google Scholar] [CrossRef]
- Vellas, B.; Guigoz, Y.; Garry, P.J.; Nourhashemi, F.; Bennahum, D.; Lauque, S.; Albarede, J.L. The Mini Nutritional Assessment (MNA) and its use in grading the nutritional state of elderly patients. Nutrition 1999, 15, 116–122. [Google Scholar] [CrossRef]
- Elgestad Stjernfeldt, P.; Faxén-Irving, G.; Wårdh, I. Masticatory ability in older individuals: A qualitative interview study. Gerodontology 2021, 38, 199–208. [Google Scholar] [CrossRef]
- Carlsson, G.E. Masticatory efficiency: The effect of age, the loss of teeth and prosthetic rehabilitation. Int. Dent. J. 1984, 34, 93–97. [Google Scholar]
- Feine, J.S.; Lund, J.P. Measuring chewing ability in randomized controlled trials with edentulous populations wearing implant prostheses. J. Oral Rehabil. 2006, 33, 301–308. [Google Scholar] [CrossRef]
- Aquilanti, L.; Alia, S.; Pugnaloni, S.; Coccia, E.; Mascitti, M.; Santarelli, A.; Rappelli, G. Impact of Elderly Masticatory Performance on Nutritional Status: An Observational Study. Medicina 2020, 56, 130. [Google Scholar] [CrossRef] [Green Version]
- de Medeiros, M.M.D.; Pinheiro, M.A.; de Figueredo, O.M.C.; de Oliveira, L.F.S.; Wanderley, R.L.; Cavalcanti, Y.W.; Rodrigues Garcia, R.C.M. Masticatory function in nursing home residents: Correlation with the nutritional status and oral health-related quality of life. J. Oral Rehabil. 2020, 47, 1511–1520. [Google Scholar] [CrossRef] [PubMed]
- Lantto, A.; Lundqvist, R.; Wårdh, I. Quality of life related to tooth loss and prosthetic replacements among persons with dependency and functional limitations. Acta Odontol. Scand. 2020, 78, 173–180. [Google Scholar] [CrossRef] [Green Version]
- Ueno, M.; Yanagisawa, T.; Shinada, K.; Ohara, S.; Kawaguchi, Y. Masticatory ability and functional tooth units in Japanese adults. J. Oral Rehabil. 2008, 35, 337–344. [Google Scholar] [CrossRef] [PubMed]
- Sarita, P.T.N.; Witter, D.J.; Kreulen, C.M.; Van’t Hof, M.A.; Creugers, N.H.J. Chewing ability of subjects with shortened dental arches. Community Dent. Oral Epidemiol. 2003, 31, 328–334. [Google Scholar] [CrossRef] [PubMed]
- De Vet, H.C.; Terwee, C.B.; Mokkink, L.B.; Knol, D.L. Measurement in Medicine: A Practical Guide; Cambridge University Press: Cambridge, UK; New York, NY, USA, 2011. [Google Scholar]
- Johansson, A.; Unell, L.; Johansson, A.K.; Carlsson, G.E. A 10-year longitudinal study of self-assessed chewing ability and dental status in 50-year-old subjects. Int. J. Prosthodont. 2007, 20, 643–645. [Google Scholar] [PubMed]
- Osterberg, T.; Carlsson, G.E. Dental state, prosthodontic treatment and chewing ability—A study of five cohorts of 70-year-old subjects. J. Oral Rehabil. 2007, 34, 553–559. [Google Scholar] [CrossRef]
- Ikebe, K.; Matsuda, K.; Morii, K.; Furuya-Yoshinaka, M.; Nokubi, T.; Renner, R.P. Association of masticatory performance with age, posterior occlusal contacts, occlusal force, and salivary flow in older adults. Int. J. Prosthodont. 2006, 19, 475–481. [Google Scholar]
- Hatch, J.P.; Shinkai, R.S.A.; Sakai, S.; Rugh, J.D.; Paunovich, E.D. Determinants of masticatory performance in dentate adults. Arch Oral Biol. 2001, 46, 641–648. [Google Scholar] [CrossRef]
- Elgestad Stjernfeldt, P.; Sjogren, P.; Wardh, I.; Bostrom, A.M. Systematic review of measurement properties of methods for objectively assessing masticatory performance. Clin. Exp. Dent. Res. 2019, 5, 76–104. [Google Scholar] [CrossRef]
- Kaiser, M.J.; Bauer, J.M.; Ramsch, C.; Uter, W.; Guigoz, Y.; Cederholm, T.; Sieber, C.C. Validation of the Mini Nutritional Assessment short-form (MNA-SF): A practical tool for identification of nutritional status. J. Nutr. Health Aging 2009, 13, 782–788. [Google Scholar] [CrossRef]
- Ng, W.L.; Collins, P.F.; Hickling, D.F.; Bell, J.J. Evaluating the concurrent validity of body mass index (BMI) in the identification of malnutrition in older hospital inpatients. Clin. Nutr. 2019, 38, 2417–2422. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Study’s Participant Characteristics | Total Included n = 196 | Answered Questions n = 86 Group Q1 | Not Answered Questions n = 110 Group Q0 |
|---|---|---|---|
| Age (yrs) mean ± SD | 79.7 ± 10.8 | 76.7 ± 11.4 | 81.7 ± 9.8 |
| Female/male, n (%) | 119/77 (61/39) | 51/35 (59/41) | 68/42 (62/38) |
| Dentures, n (%) | 88 (45) | 37 (42) | 51 (63) |
| a Eichner index group | |||
| A, n | 32 | 20 | 22 |
| B, n | 66 | 31 | 35 |
| C, n | 98 | 35 | 63 |
| b MNA (0–30 p) median, range | 23, 14.5 | 24, 14 | 21.6, 13.5 |
| Normal 24–30 p, n (%) | 87 (45) | 47 (55) | 40 (37) |
| At risk 17–23.5 p, n (%) | 88 (45) | 34 (40) | 54 (49) |
| Malnourished < 17 p, n (%) | 19 (10) | 4 (5) | 15 (14) |
| BMI < 21 n (%) | 15 (9) | 2 (2) | 13 (12) |
| BMI > 21 n (%) | 176 (91) | 79 (98) | 97 (88) |
| CC < 31 cm, n (%) | 35 (18) | 8 (9) | 27 (25) |
| CC ≥ 31 cm, n (%) | 159 (82) | 78 (91) | 81 (75) |
| MAC < 21 cm, n (%) | 1 (1) | 1 (1) | 0 (0) |
| MAC = 21–22 cm, n (%) | 7 (4) | 1 (1) | 6 (5) |
| MAC > 22 cm, n (%) | 187 (95) | 84 (98) | 103 (95) |
| Mode of feeding: | |||
| Need assistance/self-fed with difficulty/self-fed | 16/23/157 | 2/3/83 | 14/20/74 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stjernfeldt, P.E.; Faxén Irving, G.; Wårdh, I.; Lundqvist, R.; Lantto, A. The Relation between Masticatory Function and Nutrition in Older Individuals, Dependent on Supportive Care for Daily Living. Int. J. Environ. Res. Public Health 2022, 19, 5801. https://doi.org/10.3390/ijerph19105801
Stjernfeldt PE, Faxén Irving G, Wårdh I, Lundqvist R, Lantto A. The Relation between Masticatory Function and Nutrition in Older Individuals, Dependent on Supportive Care for Daily Living. International Journal of Environmental Research and Public Health. 2022; 19(10):5801. https://doi.org/10.3390/ijerph19105801
Chicago/Turabian StyleStjernfeldt, Per Elgestad, Gerd Faxén Irving, Inger Wårdh, Robert Lundqvist, and Angelika Lantto. 2022. "The Relation between Masticatory Function and Nutrition in Older Individuals, Dependent on Supportive Care for Daily Living" International Journal of Environmental Research and Public Health 19, no. 10: 5801. https://doi.org/10.3390/ijerph19105801
APA StyleStjernfeldt, P. E., Faxén Irving, G., Wårdh, I., Lundqvist, R., & Lantto, A. (2022). The Relation between Masticatory Function and Nutrition in Older Individuals, Dependent on Supportive Care for Daily Living. International Journal of Environmental Research and Public Health, 19(10), 5801. https://doi.org/10.3390/ijerph19105801






