Mind–Body Physical Activity Interventions and Stress-Related Physiological Markers in Educational Settings: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
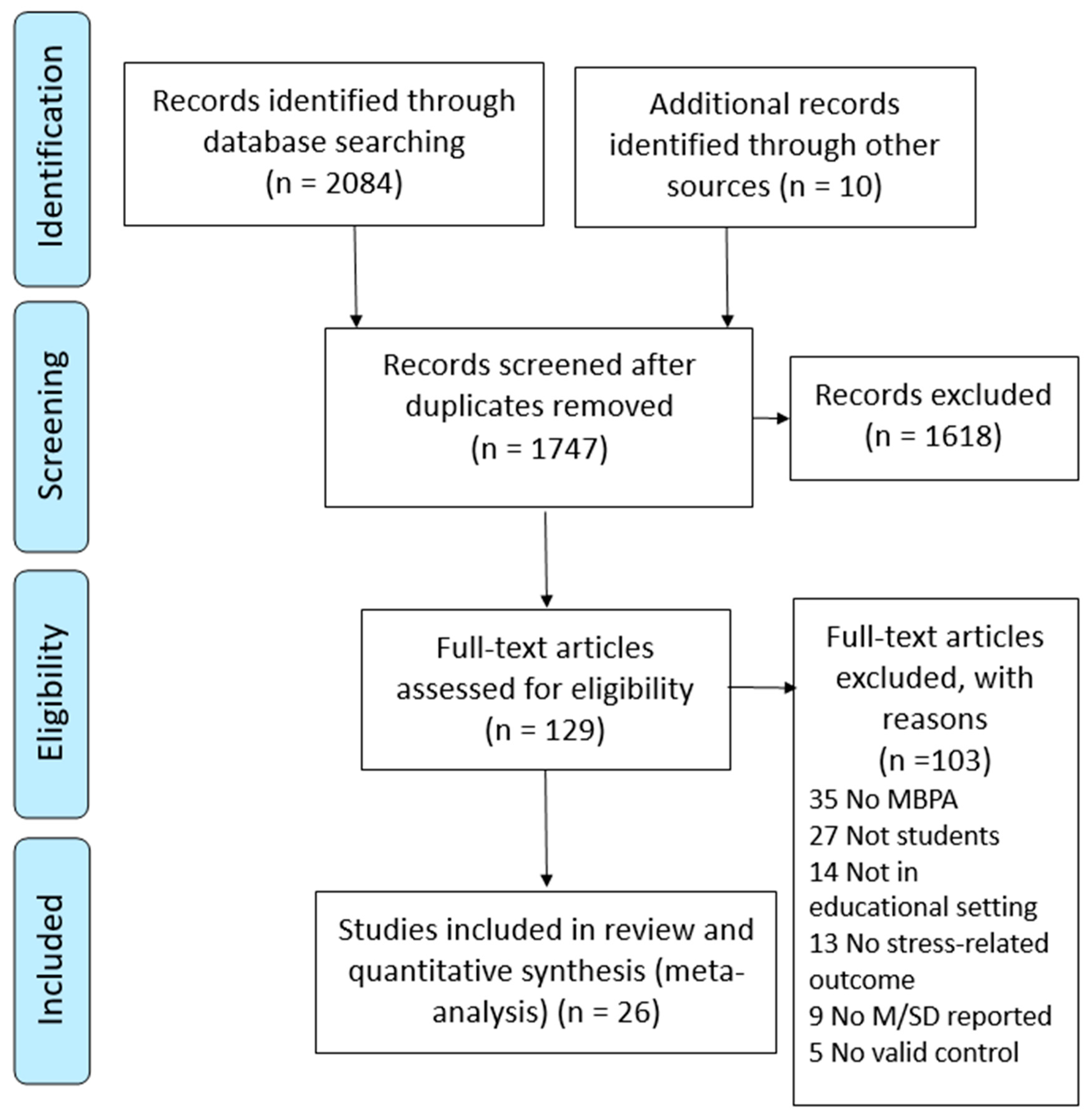
2. Materials and Methods
2.1. Search Procedures
2.2. Study Inclusion Criteria
2.3. Study Quality
2.4. Statistical Analysis
3. Results
3.1. Characteristics of the Included Studies
3.2. MBPA Interventions
3.3. Meta-Analyses
3.4. Heart Rate
3.5. Glucose
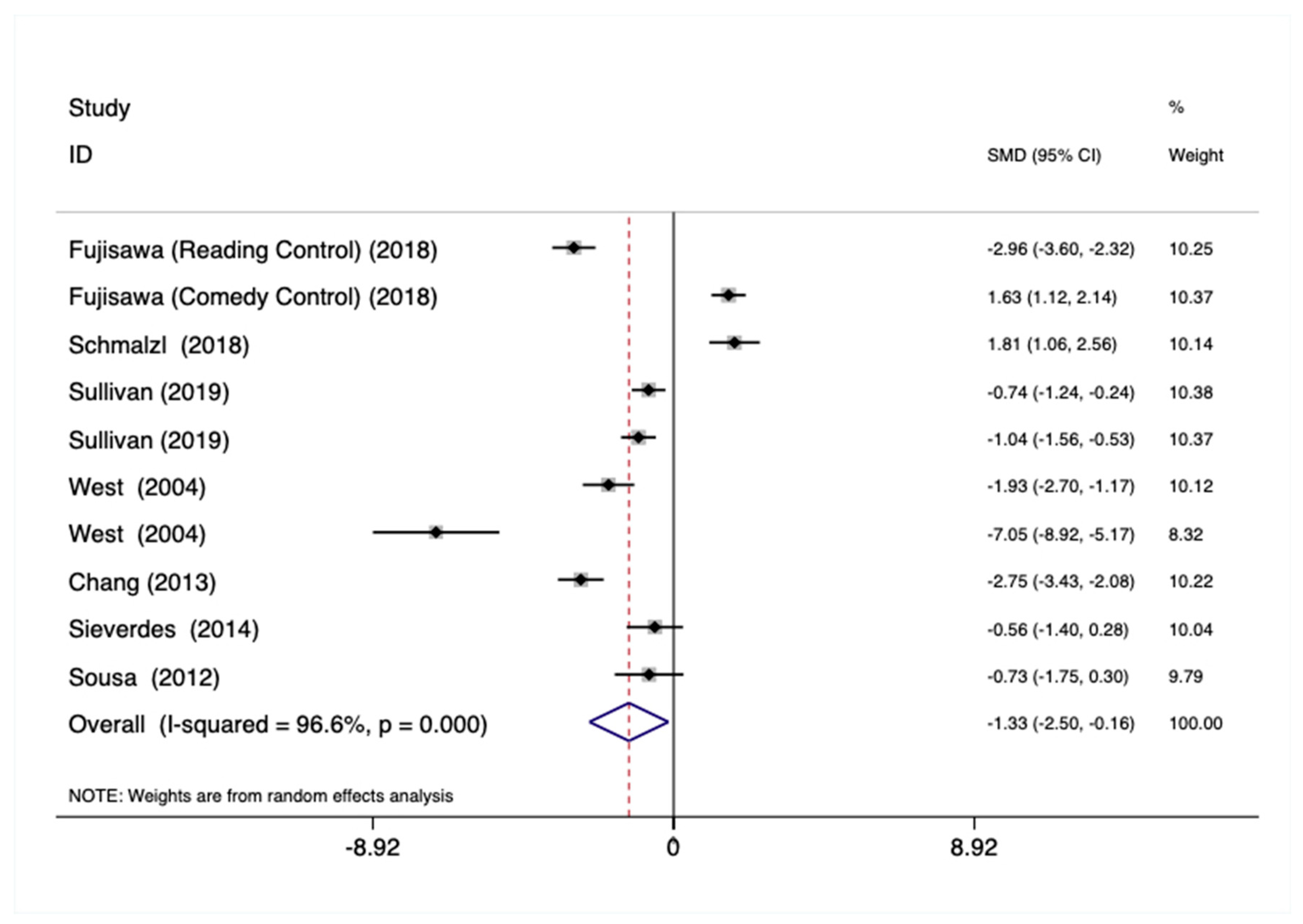
3.6. Cortisol
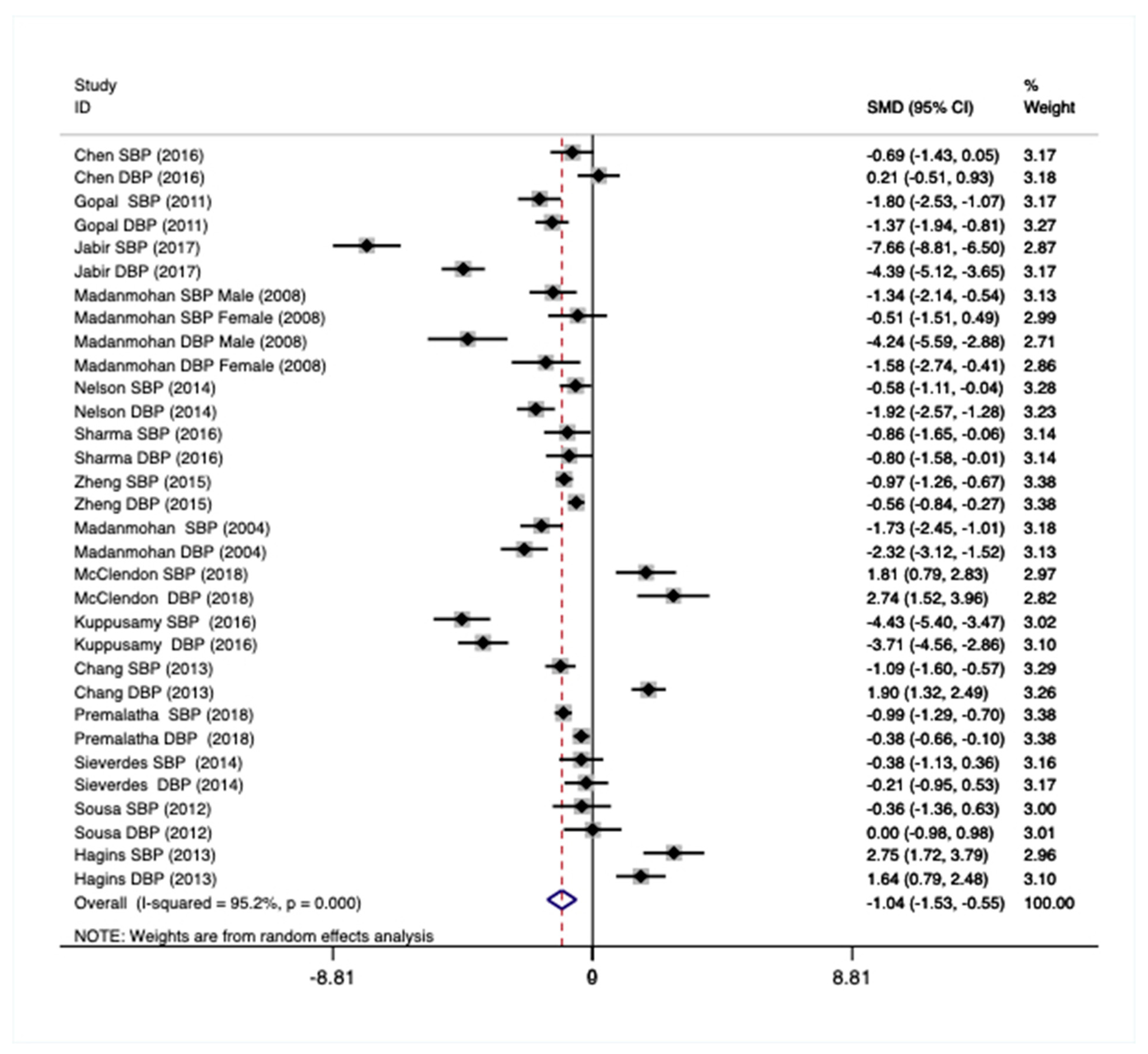
3.7. Blood Pressure
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kabat-Zinn, J. Coming to Our Senses: Healing Ourselves and the World Through Mindfulness; Hachette Books: Paris, France, 2005. [Google Scholar]
- Kabat-Zinn, J. Wherever You Go, There You Are: Mindfulness Meditation in Everyday Life; Hachette Books: Paris, France, 2009. [Google Scholar]
- Kabat-Zinn, J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness, 15th Anniversary Ed; Delta Trade Paperback/Bantam Dell: New York, NY, USA, 2005. [Google Scholar]
- Turner, A.I.; Smyth, N.; Hall, S.J.; Torres, S.J.; Hussein, M.; Jayasinghe, S.U.; Ball, K.; Clow, A. Psychological stress reactivity and future health and disease outcomes: A systematic review of prospective evidence. Psychoneuroendocrinology 2020, 114, 104599. [Google Scholar] [CrossRef] [PubMed]
- Smyth, N.; Rossi, E.; Wood, C. Effectiveness of stress-relieving strategies in regulating patterns of cortisol secretion and promoting brain health. Int. Rev. Neurobiol. 2020, 150, 219–246. [Google Scholar] [CrossRef]
- Powell, K.E.; King, A.C.; Buchner, D.M.; Campbell, W.W.; DiPietro, L.; Erickson, K.I.; Hillman, C.H.; Jakicic, J.M.; Janz, K.F.; Katzmarzyk, P.T.; et al. The Scientific Foundation for the Physical Activity Guidelines for Americans, 2nd Edition. J. Phys. Act. Health 2018, 1–11. [Google Scholar] [CrossRef]
- Jakicic, J.M.; Kraus, W.E.; Powell, K.E.; Campbell, W.W.; Janz, K.F.; Troiano, R.P.; Sprow, K.; Torres, A.; Piercy, K.L. Association between Bout Duration of Physical Activity and Health: Systematic Review. Med. Sci. Sports Exerc. 2019, 51, 1213–1219. [Google Scholar] [CrossRef] [PubMed]
- Katzmarzyk, P.T.; Powell, K.E.; Jakicic, J.M.; Troiano, R.P.; Piercy, K.; Tennant, B. Sedentary Behavior and Health: Update from the 2018 Physical Activity Guidelines Advisory Committee. Med. Sci. Sports Exerc. 2019, 51, 1227–1241. [Google Scholar] [CrossRef] [PubMed]
- Königstein, K.; Klenk, C.; Appenzeller-Herzog, C.; Hinrichs, T.; Schmidt-Trucksäss, A. Impact of sedentary behavior on large artery structure and function in children and adolescents: A systematic review. Eur. J. Pediatr. 2020, 179, 17–27. [Google Scholar] [CrossRef] [PubMed]
- King, A.C.; Whitt-Glover, M.C.; Marquez, D.X.; Buman, M.P.; Napolitano, M.A.; Jakicic, J.; Fulton, J.E.; Tennant, B.L. Physical Activity Promotion: Highlights from the 2018 Physical Activity Guidelines Advisory Committee Systematic Review. Med. Sci. Sports Exerc. 2019, 51, 1340–1353. [Google Scholar] [CrossRef]
- Barranco-Ruiz, Y.; Etxabe, B.E.; Ramirez-Velez, R.; Villa-Gonzalez, E. Interventions Based on Mind-Body Therapies for the Improvement of Attention-Deficit/Hyperactivity Disorder Symptoms in Youth: A Systematic Review. Medicina 2019, 55, 325. [Google Scholar] [CrossRef]
- Im, H.-J.; Kim, Y.-J.; Kim, H.-G.; Kim, H.-S.; Son, C.-G. Kouksundo, a traditional Korean mind–body practice, regulates oxidative stress profiles and stress hormones. Physiol. Behav. 2015, 141, 9–16. [Google Scholar] [CrossRef]
- Ideno, Y.; Hayashi, K.; Abe, Y.; Ueda, K.; Iso, H.; Noda, M.; Lee, J.-S.; Suzuki, S. Blood pressure-lowering effect of Shinrin-yoku (Forest bathing): A systematic review and meta-analysis. BMC Complement. Altern. Med. 2017, 17. [Google Scholar] [CrossRef]
- Wang, C.; Preisser, J.; Chung, Y.; Li, K. Complementary and alternative medicine use among children with mental health issues: Results from the National Health Interview Survey. BMC Complement. Altern. Med. 2018, 18, 241. [Google Scholar] [CrossRef] [PubMed]
- Seo, D.Y.; Lee, S.; Figueroa, A.; Kim, H.K.; Baek, Y.H.; Kwak, Y.S.; Kim, N.; Choi, T.H.; Rhee, B.D.; Ko, K.S.; et al. Yoga training improves metabolic parameters in obese boys. Korean J. Physiol. Pharmacol. 2012, 16, 175–180. [Google Scholar] [CrossRef] [PubMed]
- Sharma, B.; Misra, R.; Singh, K.; Sharma, R. Archana Comparative study of effect of anuloma-viloma (pranayam) and yogic asanas in premenstrual syndrome. Indian J. Physiol. Pharmacol. 2013, 57, 384–389. [Google Scholar] [PubMed]
- Sharma, V.K.; Trakroo, M.; Subramaniam, V.; Rajajeyakumar, M.; Bhavanani, A.B.; Sahai, A. Effect of fast and slow pranayama on perceived stress and cardiovascular parameters in young health-care students. Int. J. Yoga 2013, 6, 104–110. [Google Scholar] [CrossRef]
- Vasanthan, S.; Madanmohan, T.; Bhavanani, A.B.; Hanifah, M.; Jaiganesh, K. Comparative study on the effect of yogic relaxing asanas and pranayamas on cardiovascular response in healthy young volunteers. Natl. J. Physiol. Pharm. Pharmacol. 2017, 7, 127–130. [Google Scholar] [CrossRef]
- Fujisawa, A.; Ota, A.; Matsunaga, M.; Li, Y.; Kakizaki, M.; Naito, H.; Yatsuya, H. Effect of laughter yoga on salivary cortisol and dehydroepiandrosterone among healthy university students: A randomized controlled trial. Complement. Ther. Clin. Pract. 2018, 32, 6–11. [Google Scholar] [CrossRef]
- Pascoe, M.C.; Bauer, I.E. A systematic review of randomised control trials on the effects of yoga on stress measures and mood. J. Psychiatr. Res. 2015, 68, 270–282. [Google Scholar] [CrossRef]
- Pascoe, M.C.; Thompson, D.R.; Ski, C.F. Yoga, mindfulness-based stress reduction and stress-related physiological measures: A meta-analysis. Psychoneuroendocrinology 2017, 86, 152–168. [Google Scholar] [CrossRef]
- Bazzano, A.N.; Anderson, C.E.; Hylton, C.; Gustat, J. Effect of mindfulness and yoga on quality of life for elementary school students and teachers: Results of a randomized controlled school-based study. Psychol. Res. Behav. Manag. 2018, 11, 81–89. [Google Scholar] [CrossRef]
- Bhadane, M.; Kanojia, A. A Systematic Review of Yoga for Mental and Physical Health in College Students. Int. J. Yoga Allied Sci. 2018, 7. Available online: http://indianyoga.org/wp-content/uploads/2018/03/v7-issue2-article13.pdf (accessed on 28 February 2020).
- Breedvelt, J.J.F.; Amanvermez, Y.; Harrer, M.; Karyotaki, E.; Gilbody, S.; Bockting, C.L.H.; Cuijpers, P.; Ebert, D.D. The Effects of Meditation, Yoga, and Mindfulness on Depression, Anxiety, and Stress in Tertiary Education Students: A Meta-Analysis. Front. Psychiatry 2019, 10, 193. [Google Scholar] [CrossRef] [PubMed]
- Chimiklis, A.L.; Dahl, V.; Spears, A.P.; Goss, K.; Fogarty, K.; Chacko, A. Yoga, Mindfulness, and Meditation Interventions for Youth with ADHD: Systematic Review and Meta-Analysis. J. Child Fam. Stud. 2018, 27, 3155–3168. [Google Scholar] [CrossRef]
- Gopal, A.; Mondal, S.; Gandhi, A.; Arora, S.; Bhattacharjee, J. Effect of integrated yoga practices on immune responses in examination stress—A preliminary study. Int. J. Yoga 2011, 4, 26–32. [Google Scholar] [PubMed]
- Jabir, P.K.; Sadananda, B.; Das, K.S. Effect of Balasana on cardiac parameters among healthy medical students. Natl. J. Physiol. Pharm. Pharmacol. 2017, 7, 1342–1346. [Google Scholar]
- Kanojia, S.; Sharma, V.K.; Gandhi, A.; Kapoor, R.; Kukreja, A.; Subramanian, S.K. Effect of yoga on autonomic functions and psychological status during both phases of menstrual cycle in young healthy females. J. Clin. Diagn. Res. 2013, 7, 2133–2139. [Google Scholar] [CrossRef]
- Kim, S.D. Effects of yogic exercises on life stress and blood glucose levels in nursing students. J. Phys. Ther. Sci. 2014, 26, 2003–2006. [Google Scholar] [CrossRef]
- Kuppusamy, M.; Kamaldeen, D.; Pitani, R.; Amaldas, J. Immediate effects of Bhramari pranayama on resting cardiovascular parameters in healthy adolescents. J. Clin. Diagn. Res. 2016, 10, CC17–CC19. [Google Scholar] [CrossRef]
- Mahadevan, S.K.M.; Balakrishnan, S.; Gopalakrishnan, M.; Prakash, E.S. Effect of six weeks yoga training on weight loss following step test, respiratory pressures, handgrip strength and handgrip endurance in young healthy subjects. Indian J. Physiol. Pharmacol. 2008, 52, 164–170. [Google Scholar]
- Madanmohan; Udupa, K.; Bhavanani, A.B.; Shatapathy, C.C.; Sahai, A. Modulation of cardiovascular response to exercise by yoga training. Indian J. Physiol. Pharmacol. 2004, 48, 461–465. [Google Scholar]
- Parshad, O.; Richards, A.; Asnani, M. Impact of yoga on haemodynamic function in healthy medical students. West Indian Med. J. 2012, 60, 148–152. [Google Scholar]
- Premalatha, P.; Kanniammal, C.; Valli, G.; Mahendra, J. Effect of physical exercise and yoga on blood pressure among school children. Asian J. Pharm. Clin. Res. 2018, 11, 399–403. [Google Scholar]
- Priya, S.A. Effect of shavasana training on basal heart rate and blood pressure in young healthy volunteers. Biomedicine 2012, 32, 25–28. [Google Scholar]
- Khalsa, S.B.S.; Butzer, B. Yoga in school settings: A research review. Ann. N. Y. Acad. Sci. 2016, 1373, 45–55. [Google Scholar] [CrossRef] [PubMed]
- Sieverdes, J.C.; Mueller, M.; Gregoski, M.J.; Brunner-Jackson, B.; McQuade, L.; Matthews, C.; Treiber, F.A. Effects of Hatha yoga on blood pressure, salivary alpha-amylase, and cortisol function among normotensive and prehypertensive youth. J. Altern. Complement. Med. 2014, 20, 241–250. [Google Scholar] [CrossRef] [PubMed]
- West, J.; Otte, C.; Geher, K.; Johnson, J.; Mohr, D.C. Effects of Hatha yoga and African dance on perceived stress, affect, and salivary cortisol. Ann. Behav. Med. 2004, 28, 114–118. [Google Scholar] [CrossRef] [PubMed]
- Iuliano, B.; Grahn, D.; Cao, V.; Zhao, B.; Rose, J. Physiologic correlates of T’ai chi chuan. J. Altern. Complement. Med. 2011, 17, 77–81. [Google Scholar] [CrossRef]
- Sharma, M.; Haider, T. Tai chi as an alternative and complimentary therapy for anxiety: A systematic review. J. Evid. Based Complement. Altern. Med. 2015, 20, 143–153. [Google Scholar] [CrossRef]
- Zhang, S.; Zou, L.; Chen, L.Z.; Yao, Y.; Loprinzi, P.D.; Siu, P.M.; Wei, G. The Effect of Tai Chi Chuan on Negative Emotions in Non-Clinical Populations: A Meta-Analysis and Systematic Review. Int. J. Environ. Res. Public Health 2019, 16, 3033. [Google Scholar] [CrossRef]
- Zheng, G.; Lan, X.; Li, M.; Ling, K.; Lin, H.; Chen, L.; Tao, J.; Li, J.; Zheng, X.; Chen, B.; et al. Effectiveness of Tai Chi on physical and psychological health of college students: Results of a randomized controlled trial. PLoS ONE 2015, 10, e0132605. [Google Scholar] [CrossRef]
- Chan, E.S.; Koh, D.; Teo, Y.C.; Hj Tamin, R.; Lim, A.; Fredericks, S. Biochemical and psychometric evaluation of Self-Healing Qigong as a stress reduction tool among first year nursing and midwifery students. Complement. Ther. Clin. Pract. 2013, 19, 179–183. [Google Scholar] [CrossRef]
- Chang, C.; Tsai, G.; Hsieh, C.J. Psychological, immunological and physiological effects of a Laughing Qigong Program (LQP) on adolescents. Complement. Ther. Med. 2013, 21, 660–668. [Google Scholar] [CrossRef]
- Butzer, B.; Bury, D.; Telles, S.; Khalsa, S.B.S. Implementing yoga within the school curriculum: A scientific rationale for improving social-emotional learning and positive student outcomes. J. Child. Serv. 2016, 11, 3–24. [Google Scholar] [CrossRef]
- Butzer, B.; Day, D.; Potts, A.; Ryan, C.; Coulombe, S.; Davies, B.; Weidknecht, K.; Ebert, M.; Flynn, L.; Khalsa, S.B.S. Effects of a classroom-based yoga intervention on cortisol and behavior in second- and third-grade students: A pilot study. J. Evid. Based Complement. Altern. Med. 2015, 20, 41–49. [Google Scholar] [CrossRef]
- Butzer, B.; Ebert, M.; Telles, S.; Khalsa, S.B. School-based Yoga Programs in the United States: A Survey. Adv. Mind Body Med. 2015, 29, 18–26. [Google Scholar] [PubMed]
- Aberg, M.A.; Nyberg, J.; Toren, K.; Sorberg, A.; Kuhn, H.G.; Waern, M. Cardiovascular fitness in early adulthood and future suicidal behaviour in men followed for up to 42 years. Psychol. Med. 2014, 44, 779–788. [Google Scholar] [CrossRef] [PubMed]
- Åberg, M.; Waern, M.; Nyberg, J.; Pedersen, N.L.; Bergh, Y.; Åberg, N.D.; Nilsson, M.; Kuhn, H.G.; Torén, K. Cardiovascular fitness in males at age 18 and risk of serious depression in adulthood: Swedish prospective population-based study. Br. J. Psychiatry 2012, 201, 352–359. [Google Scholar] [CrossRef] [PubMed]
- Nyberg, J.; Henriksson, M.; Aberg, M.A.I.; Rosengren, A.; Soderberg, M.; Aberg, N.D.; Kuhn, H.G.; Waern, M. Cardiovascular fitness in late adolescent males and later risk of serious non-affective mental disorders: A prospective, population-based study. Psychol. Med. 2018, 48, 416–425. [Google Scholar] [CrossRef] [PubMed]
- Brusseau, T.A.; Hannon, J.; Burns, R. The Effect of a Comprehensive School Physical Activity Program on Physical Activity and Health-Related Fitness in Children from Low-Income Families. J. Phys. Act. Health 2016, 13, 888–894. [Google Scholar] [CrossRef]
- Burns, R.D.; Brusseau, T.A.; Fang, Y.; Fu, Y.; Hannon, J.C. Waist-to-Height Ratio, Aerobic Fitness, and Cardiometabolic Risk in Hispanic Children from Low-Income, U.S. Schools. Pediatric Exerc. Sci. 2016, 28, 388–396. [Google Scholar] [CrossRef]
- Burns, R.D.; Brusseau, T.A.; Fu, Y.; Hannon, J.C. Gross Motor Skills and Cardiometabolic Risk in Children: A Mediation Analysis. Med. Sci. Sports Exerc. 2017, 49, 746–751. [Google Scholar] [CrossRef]
- Burns, R.D.; Brusseau, T.A.; Hannon, J.C. Effect of Comprehensive School Physical Activity Programming on Cardiometabolic Health Markers in Children from Low-Income Schools. J. Phys. Act. Health 2017, 14, 671–676. [Google Scholar] [CrossRef] [PubMed]
- Vazou, S.; Pesce, C.; Lakes, K.; Smiley-Oyen, A. More than one road leads to Rome: A narrative review and meta-analysis of physical activity intervention effects on cognition in youth. Int. J. Sport Exerc. Psychol. 2019, 17, 153–178. [Google Scholar] [CrossRef] [PubMed]
- Elwy, A.R.; Groessl, E.J.; Eisen, S.V.; Riley, K.E.; Maiya, M.; Lee, J.P.; Sarkin, A.; Park, C.L. A systematic scoping review of yoga intervention components and study quality. Am. J. Prev. Med. 2014, 47, 220–232. [Google Scholar] [CrossRef] [PubMed]
- Kabat-Zinn, J. Foreword: Seeds of a necessary global renaissance in the making: The refining of psychology’s understanding of the nature of mind, self, and embodiment through the lens of mindfulness and its origins at a key inflection point for the species. Curr. Opin. Psychol. 2019, 28. [Google Scholar] [CrossRef] [PubMed]
- Kee, Y.H.; Li, C.; Kong, L.C.; Tang, C.J.; Chuang, K.L. Scoping Review of Mindfulness Research: A Topic Modelling Approach. Mindfulness 2019, 10, 1474–1488. [Google Scholar] [CrossRef]
- Soulakova, B.; Kasal, A.; Butzer, B.; Winkler, P. Meta-Review on the Effectiveness of Classroom-Based Psychological Interventions Aimed at Improving Student Mental Health and Well-Being, and Preventing Mental Illness. J. Prim. Prev. 2019, 40, 255–278. [Google Scholar] [CrossRef]
- Burgdorf, V.; Szabo, M.; Abbott, M.J. The Effect of Mindfulness Interventions for Parents on Parenting Stress and Youth Psychological Outcomes: A Systematic Review and Meta-Analysis. Front. Psychol. 2019, 10, 1336. [Google Scholar] [CrossRef]
- Calvete, E.; Fernández-González, L.; Echezarraga, A.; Orue, I. Dispositional mindfulness profiles in adolescents and their associations with psychological functioning and hypothalamic–pituitary–adrenal axis hormones. J. Youth Adolesc. 2019, 49, 1406–1419. [Google Scholar] [CrossRef]
- Chi, X.; Bo, A.; Liu, T.; Zhang, P.; Chi, I. Effects of Mindfulness-Based Stress Reduction on Depression in Adolescents and Young Adults: A Systematic Review and Meta-Analysis. Front. Psychol. 2018, 9, 1034. [Google Scholar] [CrossRef]
- Chiesa, A.; Serretti, A. A systematic review of neurobiological and clinical features of mindfulness meditations. Psychol. Med. 2010, 40, 1239–1252. [Google Scholar] [CrossRef]
- Chiesa, A.; Serretti, A. Mindfulness-based stress reduction for stress management in healthy people: A review and meta-analysis. J. Altern. Complement. Med. 2009, 15, 593–600. [Google Scholar] [CrossRef] [PubMed]
- Dunning, D.L.; Griffiths, K.; Kuyken, W.; Crane, C.; Foulkes, L.; Parker, J.; Dalgleish, T. Research Review: The effects of mindfulness-based interventions on cognition and mental health in children and adolescents—A meta-analysis of randomized controlled trials. J. Child. Psychol. Psychiatry 2019, 60, 244–258. [Google Scholar] [CrossRef] [PubMed]
- Khoury, B.; Sharma, M.; Rush, S.E.; Fournier, C. Mindfulness-based stress reduction for healthy individuals: A meta-analysis. J. Psychosom. Res. 2015, 78, 519–528. [Google Scholar] [CrossRef] [PubMed]
- Zimmaro, L.A.; Salmon, P.; Naidu, H.; Rowe, J.; Phillips, K.; Rebholz, W.N.; Giese-Davis, J.; Cash, E.; Dreeben, S.J.; Bayley-Veloso, R.; et al. Association of dispositional mindfulness with stress, cortisol, and well-being among university undergraduate students. Mindfulness 2016, 7, 874–885. [Google Scholar] [CrossRef]
- Li, C.; Kee, Y.H.; Kong, L.C.; Zou, L.; Ng, K.L.; Li, H. Autonomy-supportive teaching and basic psychological need satisfaction among school students: The role of mindfulness. Int. J. Environ. Res. Public Health 2019, 16, 2599. [Google Scholar] [CrossRef]
- Zenner, C.; Herrnleben-Kurz, S.; Walach, H. Mindfulness-based interventions in schools-a systematic review and meta-analysis. Front. Psychol. 2014, 5, 603. [Google Scholar] [CrossRef]
- Lin, J.; Chadi, N.; Shrier, L. Mindfulness-based interventions for adolescent health. Curr. Opin. Pediatr. 2019, 31, 469–475. [Google Scholar] [CrossRef]
- Virgili, M. Mindfulness-Based Interventions Reduce Psychological Distress in Working Adults: A Meta-Analysis of Intervention Studies. Mindfulness 2015, 6, 326–337. [Google Scholar] [CrossRef]
- Pascoe, M.C.; Thompson, D.R.; Jenkins, Z.M.; Ski, C.F. Mindfulness mediates the physiological markers of stress: Systematic review and meta-analysis. J. Psychiatr. Res. 2017, 95, 156–178. [Google Scholar] [CrossRef]
- Barr, D.A. The Childhood Roots of Cardiovascular Disease Disparities. Mayo Clin. Proc. 2017, 92, 1415–1421. [Google Scholar] [CrossRef]
- Benjamin, E.J.; Blaha, M.J.; Chiuve, S.E.; Cushman, M.; Das, S.R.; de Ferranti, S.D.; Floyd, J.; Fornage, M.; Gillespie, C.; Isasi, C.R.; et al. Heart Disease and Stroke Statistics-2017 Update: A Report from the American Heart Association. Circulation 2017, 135, e146–e603. [Google Scholar] [CrossRef] [PubMed]
- Kenney, W.L. Physiology of Sport and Exercise; Wilmore, J.H., Costill, D.L., Eds.; Human Kinetics: Champaign, IL, USA, 2015. [Google Scholar]
- Chadi, N.; McMahon, A.; Vadnais, M.; Malboeuf-Hurtubise, C.; Djemli, A.; Dobkin, P.L.; Lacroix, J.; Luu, T.M.; Haley, N. Mindfulness-based intervention for female adolescents with chronic pain: A pilot randomized trial. J. Can. Acad. Child Adolesc. Psychiatry 2016, 25, 159–168. [Google Scholar] [PubMed]
- Chadi, N.; Weisbaum, E.; Malboeuf-Hurtubise, C.; Kohut, S.A.; Viner, C.; Kaufman, M.; Locke, J.; Vo, D. Can the Mindful Awareness and Resilience Skills for Adolescents (MARS-A) Program Be Provided Online? Voices from the Youth. Children 2018, 5, 115. [Google Scholar]
- Chadi, N.; Weisbaum, E.; Vo, D.X.; Kohut, S.A. Mindfulness-Based Interventions for Adolescents: Time to Consider Telehealth. J. Altern. Complement. Med. 2020, 26, 172–175. [Google Scholar] [CrossRef] [PubMed]
- Chadi, N.; Weisbaum, E.; Malboeuf-Hurtubise, C.; Kohut, S.A.; Viner, C.; Palaniyar, N.; Kaufman, M.; Locke, J.; Vo, D.X. In-person vs. eHealth Mindfulness-based Intervention for Adolescents with Chronic Illnesses: A Pilot Randomized Trial. Adolesc. Psychiatry 2019, 9, 11–23. [Google Scholar] [CrossRef]
- Dariotis, J.K.; Cluxton-Keller, F.; Mirabal-Beltran, R.; Gould, L.F.; Greenberg, M.T.; Mendelson, T. “The Program Affects Me Cause it Gives Away Stress”: Urban Students’ Qualitative Perspectives on Stress and a School-Based Mindful Yoga Intervention. Explore 2016, 12, 443–450. [Google Scholar] [CrossRef]
- Dawson, A.F.; Brown, W.W.; Anderson, J.; Datta, B.; Donald, J.N.; Hong, K.; Allan, S.; Mole, T.B.; Jones, P.B.; Galante, J. Mindfulness-Based Interventions for University Students: A Systematic Review and Meta-Analysis of Randomised Controlled Trials. Appl. Psychol. Health Well-Being 2019, 12, 384–410. [Google Scholar] [CrossRef]
- Gouda, S.; Luong, M.T.; Schmidt, S.; Bauer, J. Students and Teachers Benefit from Mindfulness-Based Stress Reduction in a School-Embedded Pilot Study. Front. Psychol. 2016, 7, 590. [Google Scholar] [CrossRef]
- Langer, Á.I.; Ulloa, V.G.; Cangas, A.J.; Rojas, G.; Krause, M. Mindfulness-based interventions in secondary education: A qualitative systematic review. Estudios Psicología 2015, 36, 533–570. [Google Scholar] [CrossRef]
- Mussey, S. Mindfulness in the Classroom: Mindful Principles for Social and Emotional Learning; Prufrock Press Inc.: Waco, TX, USA, 2019. [Google Scholar]
- Stillwell, S.B.; Vermeesch, A.L.; Scott, J.G. Interventions to Reduce Perceived Stress Among Graduate Students: A Systematic Review with Implications for Evidence-Based Practice. Worldviews Evid. Based Nurs. 2017, 14, 507–513. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef] [PubMed]
- NIH: National Heart L, and Blood Institute. 2018. Available online: https://www.nhlbi.nih.gov/ (accessed on 10 January 2020).
- Thabane, L.; Mbuagbaw, L.; Zhang, S.; Samaan, Z.; Marcucci, M.; Ye, C.; Debono, V.B. A tutorial on sensitivity analyses in clinical trials: The what, why, when and how. BMC Med. Res. Methodol. 2013, 13, 92. [Google Scholar] [CrossRef] [PubMed]
- StataCorp. Stata Statistical Software: Release 15; StataCorp LLC: College Station, TX, USA, 2017.
- Albracht-Schulte, K.; Robert-McComb, J. The effects of yoga and quiet rest on subjective levels of anxiety and physiological correlates: A 2-way crossover randomized trial. BMC Complement. Altern. Med. 2018, 18, 280. [Google Scholar] [CrossRef] [PubMed]
- Edwards, M.K.; Rosenbaum, S.; Loprinzi, P.D. Differential experimental effects of a short bout of walking, meditation, or combination of walking and meditation on state anxiety among young adults. Am. J. Health Promot. 2018, 32, 949–958. [Google Scholar] [CrossRef]
- Qiu, Y.; Wang, Y.; Qin, C. Effects of different kinds of health-maintaining Qigong on the cardiovascular functions of martial arts majors. Int. J. Simul. Syst. Sci. Technol. 2015, 16, 8.1–8.4. [Google Scholar]
- Sharma, P.; Anand, S.; Kumar, P.; Malhotra, V.; Itagappa, M.; Tripathi, Y.; Ps, D.; Pughazhendhi, H.R.; Biswas, S. Yoga practice and biochemical and physiological alterations in normal subjects. Asian J. Pharm. Clin. Res. 2016, 9, 186–188. [Google Scholar]
- Madanmohan; Bhavanani, A.B.; Prakash, E.S.; Kamath, M.G.; Amudhan, J. Effect of six weeks of shavasan training on spectral measures of short-term heart rate variability in young healthy volunteers. Indian J. Physiol. Pharmacol. 2004, 48, 370–373. [Google Scholar]
- McClendon, B.D.; Scott, J. Namaste to Wellbeing? The Effect of Yoga on the Health of African American High School Students. J. Emerg. Investig. 2018. Available online: https://www.theneighborhoodacademy.org/editoruploads/files/yoga_final1.pdf (accessed on 28 February 2020).
- Sousa, C.M.; Goncalves, M.; Machado, J. Effects of qigong on performance-related anxiety and physiological stress functions in transverse flute music schoolchildren: A feasibility study. J. Chin. Integr. Med. 2012, 10, 858–865. [Google Scholar] [CrossRef]
- Hagins, M.; Haden, S.C.; Daly, L.A. A randomized controlled trial on the effects of yoga on stress reactivity in 6th grade students. Evid. Based Complement. Altern. Med. 2013, 2013, 607134. [Google Scholar] [CrossRef]
- Chen, N.; Xia, X.; Qin, L.-Q.; Luo, L.; Han, S.; Wang, G.; Zhang, R.; Wan, Z. Effects of 8-Week Hatha Yoga training on metabolic and inflammatory markers in healthy, female Chinese subjects: A randomized clinical trial. BioMed Res. Int. 2016, 2016. [Google Scholar] [CrossRef] [PubMed]
- Schmalzl, L.; Powers, C.; Zanesco, A.P.; Yetz, N.; Groessl, E.J.; Saron, C.D. The effect of movement-focused and breath-focused yoga practice on stress parameters and sustained attention: A randomized controlled pilot study. Conscious. Cogn. 2018, 65, 109–125. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, M.; Carberry, A.; Evans, E.S.; Hall, E.E.; Nepocatych, S. The effects of power and stretch yoga on affect and salivary cortisol in women. J. Health Psychol. 2019, 24, 1658–1667. [Google Scholar] [CrossRef] [PubMed]
- Nelson, D.; Reed, J.; Buck, S.M. Effect of a 16-week yoga program on blood pressure in healthy college students. Phys. Educ. 2014, 71, 533. [Google Scholar]
- Park, C.L.; Finkelstein-Fox, L.; Groessl, E.J.; Elwy, A.R.; Lee, S.Y. Exploring how different types of yoga change psychological resources and emotional well-being across a single session. Complement. Ther. Med. 2020, 49, 102354. [Google Scholar] [CrossRef]
- Aldwin, C.M. Stress, Coping, and Development: An Integrative Perspective; Guilford Press: New York, NY, USA, 2007. [Google Scholar]
- Riley, K.E.; Park, C.L. How does yoga reduce stress? A systematic review of mechanisms of change and guide to future inquiry. Health Psychol. Rev. 2015, 9, 379–396. [Google Scholar] [CrossRef]
- Smyth, N.; Hucklebridge, F.; Thorn, L.; Evans, P.; Clow, A. Salivary cortisol as a biomarker in social science research. Soc. Personal. Psychol. Compass 2013, 7, 605–625. [Google Scholar] [CrossRef]
- Brusseau, T.; Fairclough, S.; Lubans, D. The Routledge Handbook of Youth Physical Activity; Routledge, Taylor & Francis Group: New York, NY, USA; London, UK, 2020. [Google Scholar]
- Billman, G.E.; Sacha, J.; Werner, B.; Jelen, P.J.; Gasior, J.S. Editorial: Heart Rate Variability and Other Autonomic Markers in Children and Adolescents. Front. Physiol. 2019, 10, 1265. [Google Scholar] [CrossRef]
- Field, T. Yoga research review. Complement. Ther. Clin. Pract. 2016, 24, 145–161. [Google Scholar] [CrossRef]
- Kong, J.; Wilson, G.; Park, J.; Pereira, K.; Walpole, C.; Yeung, A. Treating Depression with Tai Chi: State of the Art and Future Perspectives. Front. Psychiatry 2019, 10, 237. [Google Scholar] [CrossRef]
- Miller, S.; Mendelson, T.; Lee-Winn, A.; Dyer, N.L.; Khalsa, S.B.S. Systematic Review of Randomized Controlled Trials Testing the Effects of Yoga with Youth. Mindfulness 2020, 11, 1336–1353. [Google Scholar] [CrossRef]
- Neumark-Sztainer, D.; Wall, M.M.; Choi, J.; Barr-Anderson, D.J.; Telke, S.; Mason, S.M. Exposure to Adverse Events and Associations with Stress Levels and the Practice of Yoga: Survey Findings from a Population-Based Study of Diverse Emerging Young Adults. J. Altern. Complement. Med. 2020. Available online: https://www.liebertpub.com/doi/pdfplus/10.1089/acm.2020.0077 (accessed on 8 June 2020). [CrossRef] [PubMed]
- Tong, J.; Qi, X.; He, Z.; Chen, S.; Pedersen, S.J.; Cooley, P.D.; Spencer-Rodgers, J.; He, S.; Zhu, X. The immediate and durable effects of yoga and physical fitness exercises on stress. J. Am. Coll. Health 2020, 1–9. [Google Scholar] [CrossRef]
- Voss, A.; Bogdanski, M.; Langohr, B.; Albrecht, R.; Sandbothe, M. Mindfulness-Based Student Training Leads to a Reduction in Physiological Evaluated Stress. Front. Psychol. 2020, 11, 645. [Google Scholar] [CrossRef]
- Frank, J.; Seifert, G.; Schroeder, R.; Gruhn, B.; Stritter, W.; Jeitler, M.; Steckhan, N.; Kessler, C.S.; Michalsen, A.; Voss, A. Yoga in school sports improves functioning of autonomic nervous system in young adults: A non-randomized controlled pilot study. PLoS ONE 2020, 15, e0231299. [Google Scholar] [CrossRef]


| Reference Location | Design | Setting | Participants | MBPA Mindfulness-Based Physical Activity | Physiological Health Markers Relevant Outcome Measures | Intervention | Study Quality |
|---|---|---|---|---|---|---|---|
| Albracht-Schulte & McComb, 2018 USA | 2-way randomized repeated-measures crossover clinical trial | HE University | 40 healthy, female college students Mean Age = 20.18 SD = 1.97 IG = 20 CG = 20 | YogaFit Beth Shaw’s Vinyasa Flow Series | Heart Rate HR (bpm) time-and frequency-domain measures of HRV, and state anxiety were assessed baseline, post- condition, and post-exposure to emotional stimuli | IG: one 30 min session of YogaFit CG: time-matched seated rest condition on separate days; after each condition, participants viewed 30 min of emotional picture stimuli | Good Trial registration: Retro- spectively registered 2/16/2018, clinical-trials.gov, Identifier: NCT 03458702 |
| Edwards et al., 2018 USA | RCT | HE University | N = 110 Mean Age = 21.4 SD = 2.4 Male 27% IG: walk n = 22, meditation n = 22, walk then meditation n = 22, meditation then walk n = 22 CG: n = 22 | 10-min yoga instructor guided mindfulness meditation, cues focused on breath/body present moment awareness through deep breathing exercises and a full-body scan | HR (bpm) at 8 time points: baseline, 5 min into the walk, 9 min into the walk, 5 min into the meditation, 9 min into the meditation, 3 min post walk/meditation Resting HR State anxiety Rating of Perceived Exertion RPE Borg 6–20 | mental and physical (MAP) training, 10 min single bout IG: walk, meditate, walk then meditate, meditate then walk CG: sit inactive control | Good |
| Gopal et al., 2011 India | RCT | HE Medical college | N = 60 Female medical students 17–20 years old IG n = 30 CG n = 30 | Yogic techniques Yogic prayer 2 min Sukshma Vyayam, micro exercises (6 min) Sthula Vyayama, macro exercises (4 min) Asanas, postures (12 min) Pranayama (4 min) Dhyana, meditation (5 min) | HR (bpm) baseline BP (SBP, DBP) Respiratory rate as physiological parameters with examination stress Biochemical serum parameters | IG: 12 weeks 35 min daily integrated yoga CG: no yoga, normal daily routine | Good |
| Jabir, Sadananda & Das, 2017 India | RCT | HE Medical college | N = 100 Mean Age = 18.26 SD = 0.63 Male 42% IG n = 50 CG n = 50 | Relaxing Asana, Balasana, Child Pose guided by a yoga therapist | Cardiac parameters HR baseline (bpm) BP (SBP, DBP) Mean arterial pressure Rate pressure product | IG: 90 days 10 min CG: without Asanas and yoga practice | Good |
| Kanojia et al., 2013 India | RCT | HE Medical College | N = 50 Mean Age = 18.6 SD = 1.08 Female IG n = 25 CG n = 25 | Integrated yoga Guided by qualified yoga trainer Yogic prayer (2 min) Sukshma Vyayam, micro exercises (5 min) Sthula Vyayama, macro exercises (5 min) Pranayama (3 min) Asanas, postures (20 min) Dhyana, meditation (5 min) | HR resting (bpm) BP (SBP, DBP) as autonomic parameters, parasympathetic reactivity tests, sympathetic reactivity tests | IG: integrated yoga practice 40 min, 6 days/week for 3 menstrual cycles CG: without yoga practice | Good |
| Madanmohan et al., 2008 India | Quasi-experimental | HE | N = 46 17–20 years old male = 30 female = 16 students IG n = 23 CG n = 23 | Asanas, pranayams, and shavasan trained yoga instructor | HR resting (bpm) BP (SBP, DBP) maximum inspiratory and expiratory pressure | IG: 90 min yoga 6 days/week for 6 weeks CG: without yoga practice | Fair |
| Qiu, Wang & Qin, 2015 China | RCT | HE Sports college | N = 30 21 and 22 years old IG A n = 10 IG B n = 10 CG n = 10 | Qigong IG A: Five-animal Exercise and IG B: Eight Silken Movements | HR baseline (bpm) Cardiac functions | IG (A and B): 5 × 60 min for 20 weeks CG: without qigong practice | Fair |
| Sharma et al., 2016, India | Quasi-experimental | HE Nursing college | N = 20 Nursing students, age from 17 to 21 IG n = 10 CG n = 10 | Yoga kriya | HR baseline (bpm) Blood Glucose BP (SBP, DBP) | IG: 30 days yoga kriya for 45 min for 6 days in a week CG: without yoga practice | Poor |
| Vasanthan et al., 2017 India | RCT (wait listed as a control) | HE Centre for Yoga Therapy Education and Research | N = 109 healthy volunteers age between 20 and 25 years IG1: n = 38 IG2: n = 38 CG n = 33 | IG1: received pranayam: pranav, savitri, nadi shuddhi and chandra nadi, IG2: received asan: pawanmuktasana, balasan, dharmikasan and shavasan | HR baseline (bpm) cardiovascular responses | 25 min/day for 6 days/week for 6 months IG1: received relaxing pranayam IG2: received relaxing asan, and CG: was wait listed | Fair |
| Zheng et al., 2015 China | Two-arm, randomized, parallel controlled trial | HE Fujian University of Traditional Chinese Medicine | N = 198 Mean Age = 20.6 SD = 1.1 Female = 133 (67.2%) IG n = 95 CG n = 103 | Tai Chi Chuan (TCC) 24 forms of simplified TCC | HR resting (bpm) BP (SBP, DBP) cardio-pulmonary function | IG: 60 min TCC sessions, 5 days per week for 12 weeks CG: activities as usual, daily diary of PA was recorded Follow-up period: 12 weeks with required PA log | Good |
| Madanmohan et al., 2004 India | Quasi-experimental | Secondary School | N = 43 Mean Age = 16.1 SD = 0.2 Male = 22 IG n = 26 CG n = 17 | Yoga, shavasan training | HR resting (bpm) BP (SBP, DBP) | IG: 15 min daily training, 4 days a week for 6 weeks CG: without yoga training | Poor |
| McClendon & Scott 2018 Africa | Quasi-experimental | Secondary After school program | N = 22 Mean Age = 14.1 SD = 0.83 Male = 5 IG n = 11 CG n = 11 | Yoga (pre-existing after school program) | HR resting (bpm) BP (SBP, DBP) | IG: 4 x week for 3 weeks CG: indoor track training | Fair |
| Kuppusamy et al., 2016 India | RCT | Secondary School | N = 60 Mean Age = 14.56 SD = 2.01 Male = 38 Female = 22 IG n = 30 CG n = 30 | Bhramari pranayama | HR resting (bpm) BP (SBP, DBP) | IG: one 45 min guided Bhramari pranayama CG: normal breathing | Good |
| Chang et al., 2013 Taiwan | Randomized prospective experimental control group | Primary School | N = 67 Mean Age & SD of 7th graders not specified Male = 34 Female = 33 IG n = 34 CG n = 33 | Laughing Qigong Program (LQP) | HR baseline (bpm) Cortisol BP (SBP, DBP) | 8 weeks 45 min “study-hall” sessions IG: LQP CG: book reading or homework | Fair |
| Sieverdes et al., 2014, USA | RCT | Primary School | N = 28 Mean Age = 12.3 SD = 0.4 Girls = 57% IG n = 14 CG n = 14 | Hatha yoga program (HYP) | HR resting (bpm) Cortisol BP (SBP, DBP) | 12 weeks 90 min (5 sessions biweekly) IG: HYP CG: attention control (AC) music or art class | Fair |
| Sousa et al., 2012 China | Prospective wait list controlled | Primary School | N = 16 Mean Age = 11.5 SD = 0.7 Male = 3 IG n = 8 CG n = 8 | Qigong “White Ball” | HR baseline (bpm) Cortisol BP (SBP, DBP) | 7 weeks 2 × 30 min guided and daily home practice with parents & record activities IG: qigong CG: without qigong training | Fair |
| Hagins, Haden & Daly, 2013 USA | RCT blinded evaluators | Primary School | N = 30 Mean Age = 10.75 SD = 0.45 Male 17 Female = 13 IG n = 15 CG n = 15 | Yoga | HR baseline (bpm) BP (SBP, DBP) on stress reactivity | 15 weeks 3 × 50 min IG: yoga CG: PE class | Good |
| Chen et al., 2016 China | RCT single-arm parallel | HE | N = 30 healthy females between 18 and 25 Female = 30 IG n = 15 CG n = 15 | Hatha yoga | Blood Glucose BP (SBP, DBP) | 8 weeks 2 × 60 min IG: Hatha yoga CG: without yoga training | Good |
| Kim, 2014 Republic of Korea | RCT | HE | N = 27 female nursing students Mean Age = 21.0 SD = 0.2 IG n = 12 CG n = 15 | Yogic exercises: surya namaskara, shavasana, and yoga nidra | Blood Glucose on life stress | 12 weeks 1 × 60 min IG: yoga CG: without yoga training | Fair |
| Seo et al., 2012 South Korea | RCT | Secondary School | N = 20 obese boys Mean Age = 14.7 SD = 0.5 Male = 20 IG n = 10 CG n = 10 | Yoga Asana training | Blood Glucose | 8 weeks 3 × 60 min IG: yoga asana CG: general health education | Fair |
| Fujisawa et al., 2018 Japan | RCT | HE Medical College | N = 120 Mean Age = 24.4 SD = 3.8 Male = 76 Female = 44 IG n = 40 CG n = 40 CG n = 40 | Laughter yoga (LY) | Cortisol | IG: one 30 min LY CG: 30 min comedy movie CG: 30 min quiet reading without humor | Good |
| Schmalzl et al., 2018 USA | RC pilot | HE University | N = 40 Mean Age = 24.91 SD = 5.99 Male = 17 Female = 23 IG n = 22 CG n = 18 | Yoga: movement Ashtanga Vinyasa; seated breathing exercises: ujjayi breath and variations | Cortisol | 8 weeks 1 × 45 min instructor led 6 × 20 min home program IG: yoga movement CG: seated breathing | Fair |
| Sullivan et al., 2019 USA | Quasi-experimental within subject | HE University graduate and undergraduate women | N = 33 Female Mean Age = 21 SD = 2 | Yoga: stretch and power | Cortisol | 1 × 60 min IG: stretch yoga, IG: power yoga, CG: watching a movie | Fair |
| West et al., 2004 USA | Quasi-experimental | HE Undergraduate | N = 69 Students enrolled in African dance, Hatha yoga, and biology classes Mean Age = 19 With range 17 to 24 Male = 22 Female = 47 IG n = 21 IG n = 18 CG n = 30 | Hatha yoga | Cortisol | 3 weeks Participants enrolled in IG: African dance, IG: Hatha yoga CG: biology class | Fair |
| Nelson et al., 2014 USA | Quasi-experimental | HE University | N = 56 Mean Age = 28.24 SD = 10.64 Male = 30 Female = 26 IG n = 25 CG n = 31 | Hatha yoga guided by trained instructor | BP (SBP, DBP) | 16 weeks 2 × 45 min IG: introductory Hatha yoga CG: lecture | Fair |
| Premalatha et al., 2018 India | RCT | Primary School | N = 201 Children 10 to 12 years old IG n = 104 CG n = 97 | Yoga guided by trained instructor | BP (SBP, DBP) | 6 months 5 days/week 60 min IG: 45 min physical exercise and 15 min yoga asana practice CG: daily routine | Fair |
| Outcome | Sample | Hedges’ g (95% CI) | p-Value | I2 Statistic |
|---|---|---|---|---|
| Heart Rate | Total Sample (N = 19) | −1.71 † (−2.43, −0.98) | <0.001 | 95.6% |
| Higher Education (n = 12) | −1.94 † (−2.93, −0.96) | <0.001 | 96.6% | |
| Secondary School (n = 3) | −2.13 (−5.54, 1.28) | 0.222 | 97.7% | |
| Primary School (n = 4) | −0.76 † (−1.22, −0.30) | 0.001 | 35.6% | |
| Blood Glucose | Total Sample (N = 4) | −1.91 (−3.90, 0.08) | 0.060 | 93.7% |
| Cortisol | Total Sample (N = 10) | −1.32 † (−2.50, −0.16) | 0.026 | 96.6% |
| Higher Education (n = 7) | −1.33 (−2.83, 0.17) | 0.082 | 97.3% | |
| Primary Schools (n= 3) | −1.37 (−2.89, 0.15) | 0.077 | 89.9% | |
| Blood Pressure | Total (N = 32) | −1.04 † (−1.53, −0.55) | <0.001 | 95.2% |
| Higher Education (n = 16) | −1.75 † (−2.40, −1.09) | <0.001 | 94.4% | |
| Secondary School (n = 6) | −1.30 (−3.31, 0.72) | 0.207 | 96.7% | |
| Primary School (n = 10) | 0.24 (−0.45, 0.94) | 0.490 | 93.6% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Strehli, I.; Burns, R.D.; Bai, Y.; Ziegenfuss, D.H.; Block, M.E.; Brusseau, T.A. Mind–Body Physical Activity Interventions and Stress-Related Physiological Markers in Educational Settings: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 224. https://doi.org/10.3390/ijerph18010224
Strehli I, Burns RD, Bai Y, Ziegenfuss DH, Block ME, Brusseau TA. Mind–Body Physical Activity Interventions and Stress-Related Physiological Markers in Educational Settings: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2021; 18(1):224. https://doi.org/10.3390/ijerph18010224
Chicago/Turabian StyleStrehli, Ildiko, Ryan D. Burns, Yang Bai, Donna H. Ziegenfuss, Martin E. Block, and Timothy A. Brusseau. 2021. "Mind–Body Physical Activity Interventions and Stress-Related Physiological Markers in Educational Settings: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 18, no. 1: 224. https://doi.org/10.3390/ijerph18010224
APA StyleStrehli, I., Burns, R. D., Bai, Y., Ziegenfuss, D. H., Block, M. E., & Brusseau, T. A. (2021). Mind–Body Physical Activity Interventions and Stress-Related Physiological Markers in Educational Settings: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 18(1), 224. https://doi.org/10.3390/ijerph18010224









