Protocol for a Trial Assessing the Impacts of School-Based WaSH Interventions on Children’s Health Literacy, Handwashing, and Nutrition Status in Low- and Middle-Income Countries
Abstract
1. Introduction
1.1. Background
1.2. Objectives
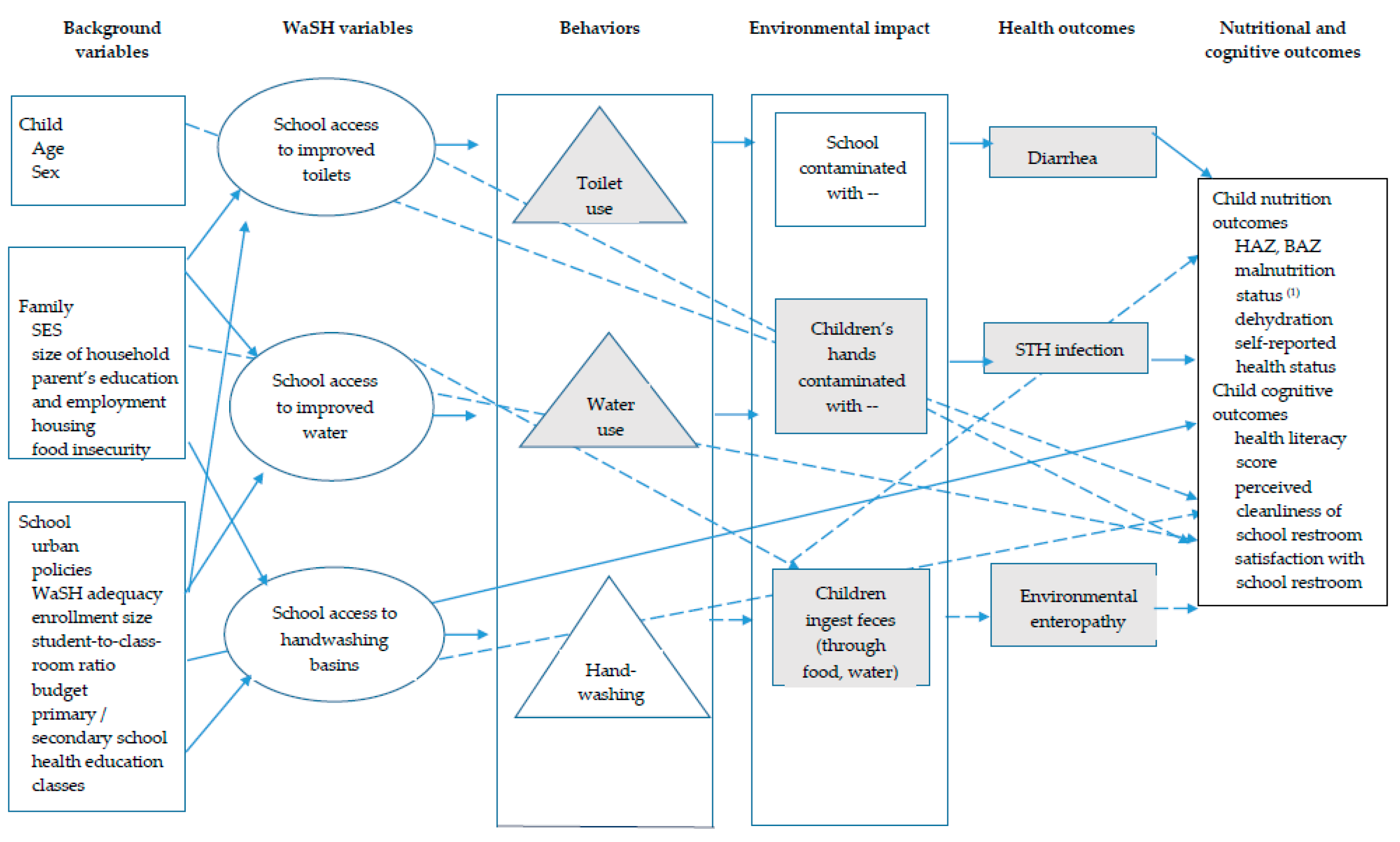
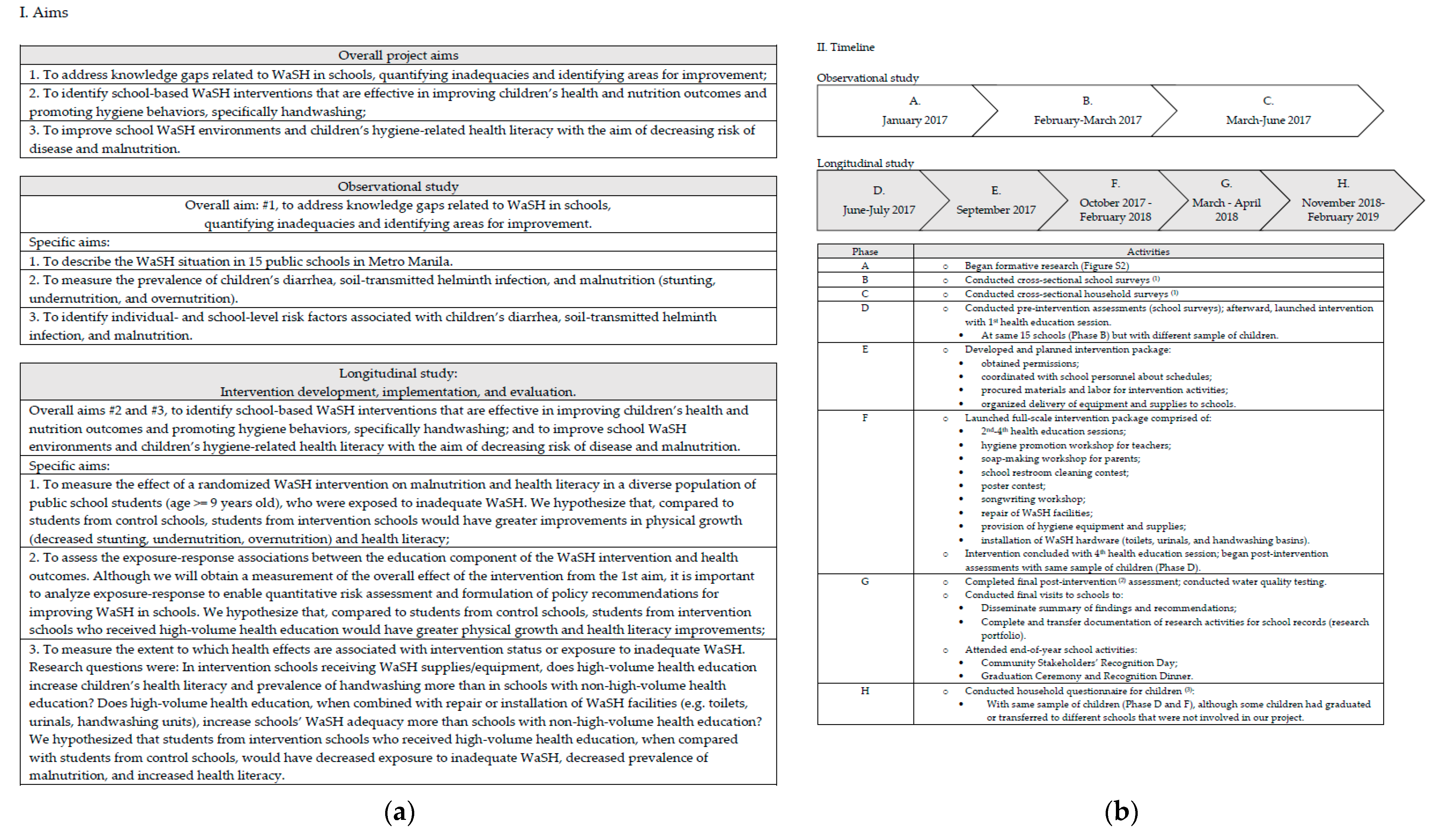
2. Research Methodology
2.1. Study Overview and Design
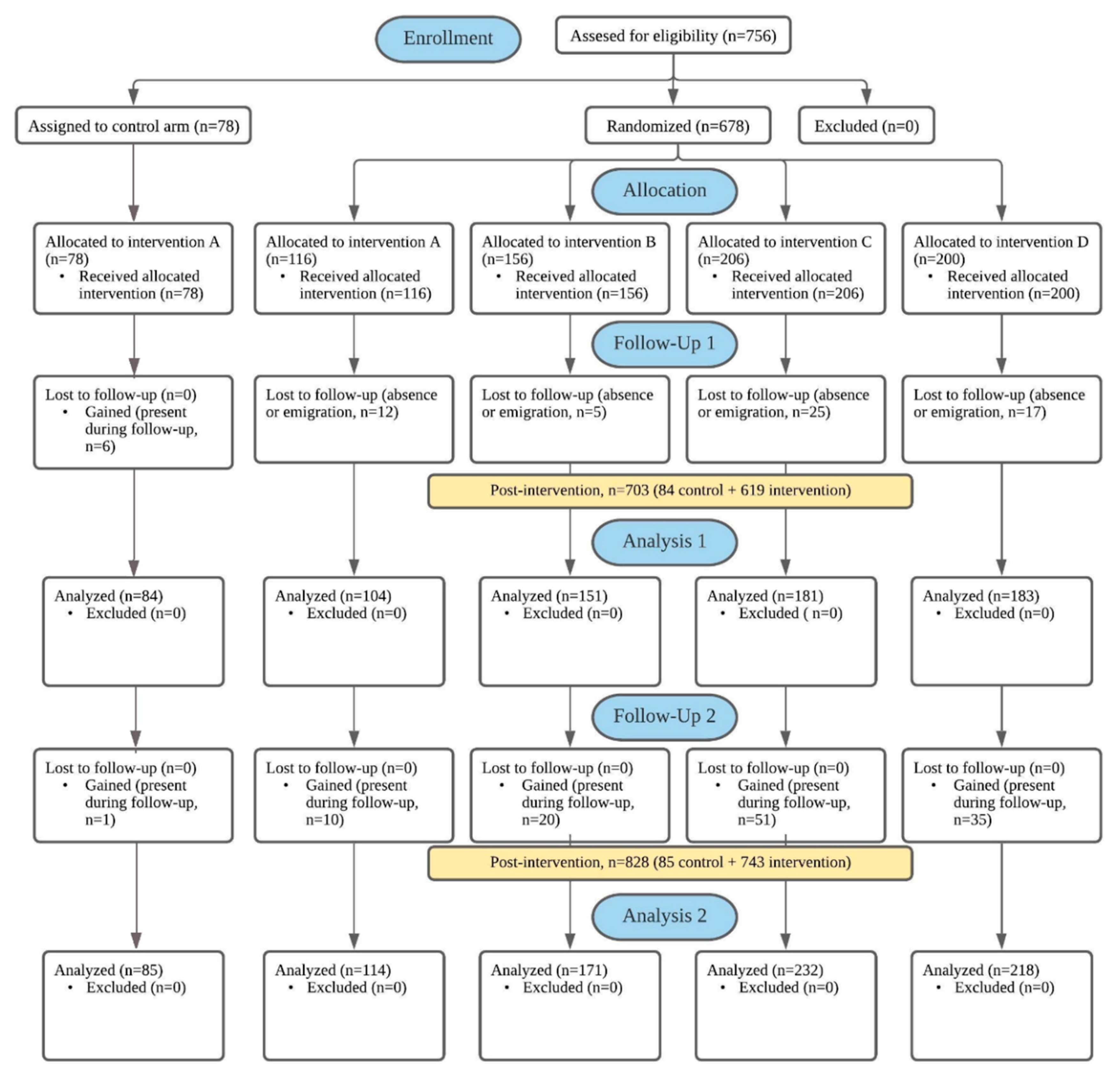
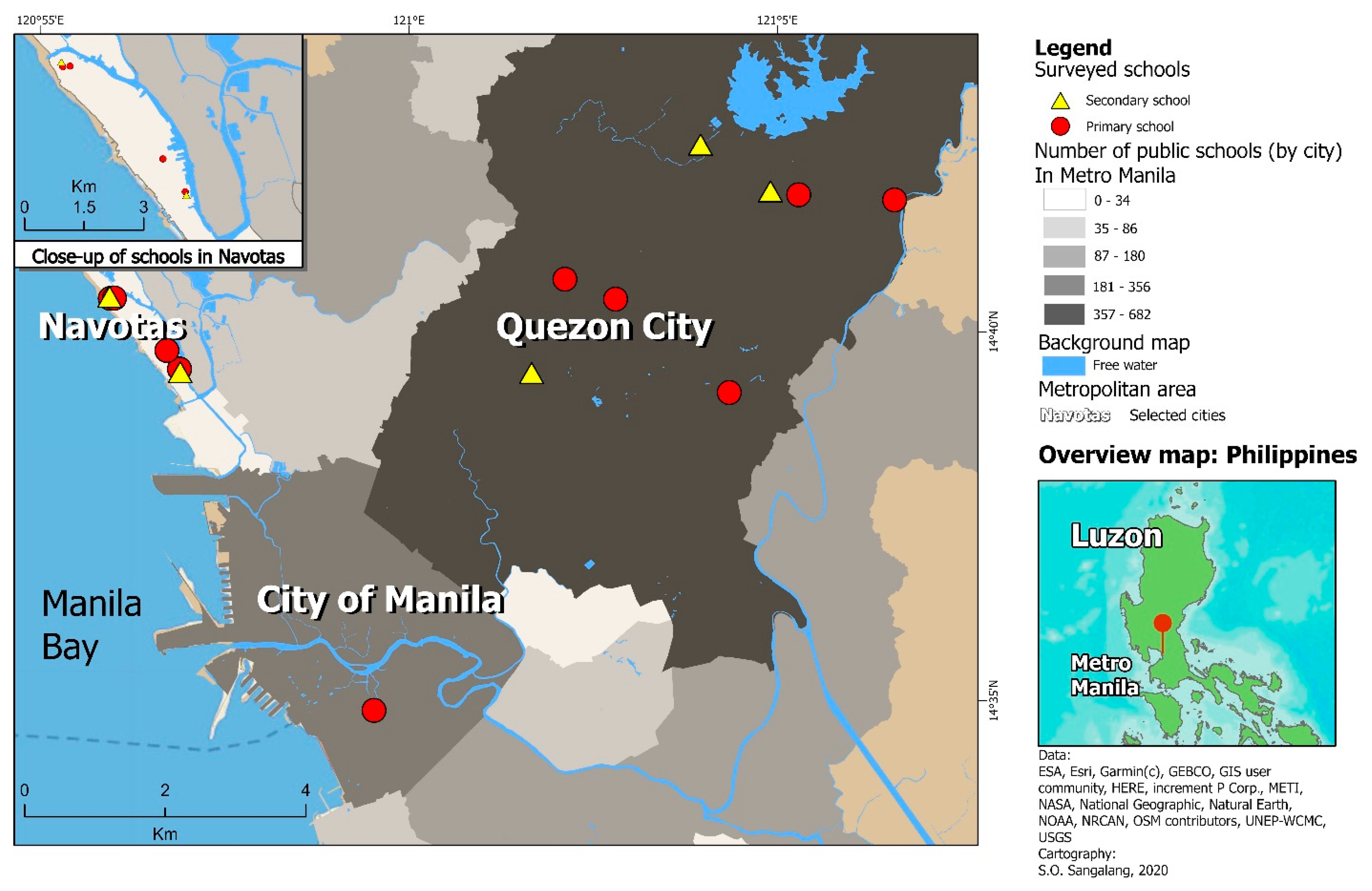
2.2. Study Population
2.3. Sampling and Recruitment
2.4. Ethics Approval
2.5. Data Collection
2.5.1. Assessing Primary Intervention Outcomes
2.5.2. Assessing Secondary Intervention Outcomes
2.5.3. Baseline Survey and Randomization
2.5.4. Follow-Up and Other Assessments
2.6. Intervention
2.7. Trial and Data Management
2.7.1. Protocol Standardization and Data Quality Control
2.7.2. Dissemination
2.8. Statistical Analysis
2.8.1. Descriptive Analyses
2.8.2. Inferential Statistical Analyses
3. Discussion
Implications for Research and Policy
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Malnutrition. Key Facts. Available online: https://www.who.int/news-room/fact-sheets/detail/malnutrition#:~:text=Malnutrition (accessed on 30 October 2020).
- WHO. The Double Burden of Malnutrition Policy Brief; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Development Initiatives. 2018 Global Nutrition Report: Shining a Light to Spur Action on Nutrition; Development Initiatives: Bristol, UK, 2018. [Google Scholar]
- WHO. Nutrition Landscape Information System (NLIS) Country Profile Indicators Interpretation Guide; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Black, R.E.; Victora, C.G.; Walker, S.P.; Bhutta, Z.A.; Christian, P.; de Onis, M.; Ezzati, M.; Grantham-McGregor, S.; Katz, J.; Martorell, R.; et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef]
- Naghavi, M.; Abajobir, A.A.; Abbafati, C.; Abbas, K.M.; Abd-Allah, F.; Abera, S.F.; Aboyans, V.; Adetokunboh, O.; Afshin, A.; Agrawal, A.; et al. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1151–1210. [Google Scholar] [CrossRef]
- FAO. Food Systems for Better Nutrition; Food and Agriculture Organization of the United Nations: Rome, Italy, 2013. [Google Scholar]
- AUC; NEPAD; UNECA; WFP. The Cost of Hunger in Africa: Social and Economic Impact of Child Undernutrition in Egypt, Ethiopia, Swaziland and Uganda Abridged Report; United Nations Economic Commission for Africa: Addis Ababa, Ethiopia, 2014. [Google Scholar]
- Troeger, C.; Blacker, B.F.; Khalil, I.A.; Rao, P.C.; Cao, S.; Zimsen, S.R.; Albertson, S.B.; Stanaway, J.D.; Deshpande, A.; Abebe, Z.; et al. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of diarrhoea in 195 countries: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Infect. Dis. 2018, 18, 1211–1228. [Google Scholar] [CrossRef]
- Weatherhead, J.E.; Hotez, P.J.; Mejia, R. The global state of helminth control and elimination in children. Pediatr. Clin. N. Am. 2017, 64, 867–877. [Google Scholar] [CrossRef] [PubMed]
- Clasen, T.; Boisson, S.; Routray, P.; Torondel, B.; Bell, M.; Cumming, O.; Ensink, J.; Freeman, M.; Jenkins, M.; Odagiri, M.; et al. Effectiveness of a rural sanitation programme on diarrhoea, soil-transmitted helminth infection, and child malnutrition in Odisha, India: A cluster-randomised trial. Lancet Glob. Health 2014, 2, e645–e653. [Google Scholar] [CrossRef]
- Luby, S.P.; Rahman, M.; Arnold, B.F.; Unicomb, L.; Ashraf, S.; Winch, P.J.; Stewart, C.P.; Begum, F.; Hussain, F.; Benjamin-Chung, J.; et al. Effects of water quality, sanitation, handwashing, and nutritional interventions on diarrhoea and child growth in rural Bangladesh: A cluster randomised controlled trial. Lancet Glob. Health 2018, 6, e302–e315. [Google Scholar] [CrossRef]
- Prüss-Ustün, A.; Wolf, J.; Bartram, J.; Clasen, T.; Cumming, O.; Freeman, M.C.; Gordon, B.; Hunter, P.R.; Medlicott, K.; Johnston, R. Burden of disease from inadequate water, sanitation and hygiene for selected adverse health outcomes: An updated analysis with a focus on low-and middle-income countries. Int. J. Hyg. Environ. Health 2019, 222, 765–777. [Google Scholar] [CrossRef] [PubMed]
- UN. The World’s Cities in 2018: Data Booklet; United Nations: New York, NY, USA, 2018. [Google Scholar]
- World Bank. Available online: https://data.worldbank.org/indicator/SP.POP.TOTL?locations=PH (accessed on 24 September 2020).
- Philippine Statistics Authority. Available online: https://psa.gov.ph/content/population-national-capital-region-based-2015-census-population-0 (accessed on 1 September 2020).
- Philippine Statistics Authority. Available online: https://psa.gov.ph/content/philippine-population-density-based-2015-census-population (accessed on 2 September 2020).
- Our World in Data. UN Habitat GUO. Available online: https://ourworldindata.org/grapher/population-density-by-city?country=Bangkok~Beijing~Delhi~Dhaka~Manila~Mexico%20City~Mumbai~Sao%20Paulo~Shanghai~Taipei~Tokyo (accessed on 2 September 2020).
- Malabad, C.G. Food security status of Filipino households. In Proceedings of the 2019 National Nutrition Summit, Manila, Philippines, 25 June 2019. [Google Scholar]
- Vargas, M.B. Nutritional status of Filipino school children (6–10 years old). In Proceedings of the 2019 National Nutrition Summit, Manila, Philippines, 25 June 2019. [Google Scholar]
- UNICEF. The Economic Consequences of Undernutrition in the Philippines: A Damage Assessment Report (DAR); United Nations International Children’s Emergency Fund: Mandaluyong, Philippines, 2018. [Google Scholar]
- Save the Children. Cost of Hunger: Philippines. The Economic Impact of Child Undernutrition on Education and Productivity in the Philippines; Save the Children Philippines: Makati City, Philippines, 2016. [Google Scholar]
- DepEd. Elementary and junior and senior high school enrollment, school years 2014–2019. Unpublished work; dataset.
- DepEd. Number of public classrooms in elementary and junior high school, enrollment for school years 2018–2019. Unpublished work; dataset.
- Sangalang, S.; Ottong, Z.J.; Medina, S.A.M.; Lemence, A.L.G.; Singson, P.A.; Anglo, M.V.; Valencia, J.C.; Canja, R.J.; Kistemann, T.; Borgemeister, C.; et al. Effectiveness of a School-Based Water, Sanitation, and Hygiene Intervention to Improve Handwashing, Health Literacy, and Nutrition Status: Results from a Cluster-Randomized Controlled Trial. Unpublished work, manuscript in preparation.
- Dearden, K.; Schott, W.; Crookston, B.; Humphries, D.; Penny, M.; Behrman, J.R. Children with access to improved sanitation but not improved water are at lower risk of stunting compared to children without access: A cohort study in Ethiopia, India, Peru, and Vietnam. BMC Public Health 2017, 17. [Google Scholar] [CrossRef] [PubMed]
- Sangalang, S.; Prado, N.; Lemence, A.; Cayetano, M.; Lu, J.; Valencia, J.; Kistemann, T.; Borgemeister, C. Diarrhea, Helminth Infection, Dehydration, and Malnutrition Associated with Water, Sanitation, and Hygiene Facilities and Poor Handwashing in Schools in Metro Manila, Philippines: A Cross-Sectional Study. Am. J. Trop. Med. Hyg. 2020. Under review. [Google Scholar] [CrossRef]
- Schulz, K.F.; Altman, D.G.; Moher, D.; CONSORT Group. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. BMJ 2010, 23, 332–340. [Google Scholar] [CrossRef] [PubMed]
- WHO. BMI-for-Age Boys. 5 to 19 years (z-scores) 2007. Available online: https://www.who.int/growthref/bmifa_boys_z_5_19_labels.pdf?ua=1 (accessed on 4 September 2020).
- WHO. BMI-for-Age Girls. 5 to 19 years (z-scores) 2007. Available online: https://www.who.int/growthref/bmifa_girls_z_5_19_labels.pdf?ua=1 (accessed on 4 September 2020).
- WHO. Height-for-Age Boys. 5 to 19 years (z-scores) 2007. Available online: https://www.who.int/growthref/cht_hfa_boys_z_5_19years.pdf?ua=1 (accessed on 4 September 2020).
- WHO. Height-for-Age Girls. 5 to 19 years (z-scores) 2007. Available online: https://www.who.int/growthref/cht_hfa_girls_z_5_19years.pdf?ua=1 (accessed on 4 September 2020).
- Pagana, K.D.; Pagana, T.J.; Pagana, T.N. Mosby’s Diagnostic and Laboratory Test Reference, 12th ed.; Elsevier Inc.: Saint Louis, MO, USA, 2015; pp. 671–672, 956–957. [Google Scholar]
- WHO; UNICEF. Progress on Sanitation and Drinking-Water: 2010 Update; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- DOH. Implementing Rules and Regulations of Chapter VI, “School Sanitation and Health Services”, of the Code on Sanitation of the Philippines (P.D. 856); Department of Health: Manila, Philippines, 1998. [Google Scholar]
- WHO. Water, Sanitation and Hygiene Standards for Schools in Low-Cost Settings; Adams, J., Bartram, J., Chartier, Y., Sims, J., Eds.; World Health Organization: Geneva, Switzerland, 2009. [Google Scholar]
- Bar-David, Y.; Urkin, J.; Kozminsky, E. The effect of voluntary dehydration on cognitive functions of elementary school children. Acta Paediatr. 2005, 94, 1667–1673. [Google Scholar] [CrossRef] [PubMed]
- Bar-David, Y.; Urkin, J.; Landau, D.; Bar-David, Z.; Pilpel, D. Voluntary dehydration among elementary school children residing in a hot arid environment. J. Hum. Nutr. Diet 2009, 22, 455–460. [Google Scholar] [CrossRef] [PubMed]
- Baron, S.; Courbebaisse, M.; Lepicard, E.M.; Friedlander, G. Assessment of hydration status in a large population. Br. J. Nutr. 2015, 113, 147–158. [Google Scholar] [CrossRef] [PubMed]
- DepEd. DepEd Order No. 10, s. 26. In Policy and Guidelines for the Comprehensive Water, Sanitation, and Hygiene in Schools (WinS) Program; Department of Education: Pasig City, Philippines, 2016. [Google Scholar]
- UN. Global Indicator Framework for the Sustainable Development Goals and Targets of the 2030 Agenda for Sustainable Development; United Nations: Geneva, Switzerland, 2016. [Google Scholar]
- Benjamini, Y.; Hochberg, Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. J. R. Stat. Soc. Ser. B 1995, 57, 289–300. [Google Scholar] [CrossRef]
- Little, R.J.A.; Rubin, D.B. Statistical Analysis with Missing Data; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2020. [Google Scholar]
- Or, P.P.L.; Wong, B.Y.M.; Chung, J.W.Y. To investigate the association between the health literacy and hand hygiene practices of the older adults to help them fight against infectious diseases in Hong Kong. Am. J. Infect. Control 2020, 48, 485–489. [Google Scholar] [CrossRef] [PubMed]
- Riiser, K.; Helseth, S.; Haraldstad, K.; Torbjørnsen, A.; Richardsen, K. Adolescents’ health literacy, health protective measures, and health-related quality of life during the Covid-19 pandemic. PLoS ONE 2020, 15, e0238161. [Google Scholar] [CrossRef] [PubMed]
- Appiah-Brempong, E.; Harris, M.J.; Newton, S.; Gulis, G. Examining school-based hygiene facilities: A quantitative assessment in a Ghanaian municipality. BMC Public Health 2018, 18, 581. [Google Scholar] [CrossRef]
- Jordanova, T.; Cronk, R.; Obando, W.; Medina, O.Z.; Kinoshita, R.; Bartram, J. Water, sanitation, and hygiene in schools in low socio-economic regions in Nicaragua: A cross-sectional survey. Int. J. Environ. Res. Public Health 2015, 12, 6197–6217. [Google Scholar] [CrossRef] [PubMed]
- Lindquist, M.A.; Mejia, A. Zen and the art of multiple comparisons. Psychosom. Med. 2015, 77, 114–125. [Google Scholar] [CrossRef] [PubMed]
- Valensisi, G. COVID-19 and Global Poverty: Are LDCs Being Left Behind? Eur. J. Dev. Res. 2020, 32, 1535–1557. [Google Scholar] [CrossRef] [PubMed]
- Lapidor, E. Out of the spotlight: COVID-19 and the Global South. Available online: https://www.justsecurity.org/71570/out-of-the-spotlight-covid-19-and-the-global-south/ (accessed on 28 August 2020).
| Indicator | Definition | Reference | |
|---|---|---|---|
| Malnutrition | |||
| Stunting | Stunted | HAZ < −2 | [4,31,32] |
| Undernutrition | Underweight (“thin”) | −3 < BAZ < −2 | [4,29,30] |
| Wasted (“severely thin”) | BAZ < −3 | [4,29,30] | |
| Over-nutrition | Overweight | 1 < BAZ < 2 | [4,29,30] |
| Obese | BAZ > 2 | [4,29,30] | |
| Acute dehydration Concentrated urine Moderately concentrated urine Severely concentrated urine WaSH adequacy | sg ≥ 1.020 sg = 1.025 sg = 1.030 | [33] Category used in present study Category used in present study | |
| Sanitation | |||
| Improved | Facility that hygienically separates human excreta from human contact | e.g., flush toilet, pour-flush latrines, ventilated improved pit latrines and pit latrines with a slab or covered pit | [34] |
| Unimproved | Facility that does not hygienically separates human excreta from human contact | e.g., pit latrines without slabs or platforms or open pit, hanging latrines, bucket latrines, open defecation, disposal of human feces with other forms of solid waste | [34] |
| Male student-to-toilet ratio | Less than 50 students | 1 toilet, 1 urinal, 1 handwashing basin | [35] |
| 50 or more students | 2 toilets, 1 urinal, 2 handwashing basins | [35] | |
| For each additional 100 students | 1 toilet, 1 urinal, 1 handwashing basin | [35] | |
| Female student-to-toilet ratio | Less than 30 students | 1 toilet, 1 handwashing basin | [35] |
| 30–100 students | 2 toilets, 2 handwashing basins | [35] | |
| For each additional 50 students | 1 toilet | [35] | |
| For each additional 100 students | 1 handwashing basin | [35] | |
| Male student-to-toilet ratio | 50 students | 1 toilet, 1 urinal (or 50 cm of urinal wall) | [36] |
| Female student-to-toilet ratio | 25 students | 1 toilet | [36] |
| Student-to-handwashing basin ratio | N/A | N/A | No WHO guidelines available |
| Male student-to-toilet ratio | Low | ≤ 50:1 | Category used in present study |
| Medium | 51:1–100:1 | Category used in present study | |
| High | ≥ 101:1 | Category used in present study | |
| Female student-to-toilet ratio | Low | ≤ 50:1 | Category used in present study |
| Medium | 51:1–100:1 | Category used in present study | |
| High | ≥ 101:1 | Category used in present study | |
| Student-to-handwashing basin ratio | Low Medium High | ≤ 50:1 51:1-150:1 ≥151:1 | Category used in present study Category used in present study Category used in present study |
| Instrument | Types of Data Collected | Frequency and Time Period (s) |
|---|---|---|
| WaSH-related knowledge, attitudes, and practices (KAP) questionnaire for children | Self-reported:
| 1 time: February–March 2017 |
| Health examination (form) for children | Observed:
| 3 times: February–March 2017; different sample of students during June–July 2017 and February–March 2018 |
| Interview (form) for school principal (1) | Self-reported:
| 2 times: March–June 2017; November–December 2018 |
| School restroom inspection checklist | Observed:
| 2 times: February–March 2017; September–December 2018 |
| Interview (form) for parent/guardian | Self-reported:
| 1 time: March–June 2017 |
| Home restroom inspection checklist | Observed:
| 1 time: March–June 2017 |
| Health literacy questionnaire for children | Self-reported:
| 2 times: June–July 2017 and February–March 2018 |
| Handwashing observation form | Observed:
| 2 times: October 2017; February–March 2018 |
| Water quality testing form | Observed:
| 1 time: April 2018 (2) |
| Household questionnaire for children | Self-reported:
| 1 time: November 2018–February 2019 |
| N/A |
| Various |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sangalang, S.O.; Medina, S.A.J.; Ottong, Z.J.; Lemence, A.L.G.; Totanes, D.; Valencia, J.C.; Singson, P.A.A.; Olaguera, M.; Prado, N.O.; Ocaña, R.M.Z.; et al. Protocol for a Trial Assessing the Impacts of School-Based WaSH Interventions on Children’s Health Literacy, Handwashing, and Nutrition Status in Low- and Middle-Income Countries. Int. J. Environ. Res. Public Health 2021, 18, 226. https://doi.org/10.3390/ijerph18010226
Sangalang SO, Medina SAJ, Ottong ZJ, Lemence ALG, Totanes D, Valencia JC, Singson PAA, Olaguera M, Prado NO, Ocaña RMZ, et al. Protocol for a Trial Assessing the Impacts of School-Based WaSH Interventions on Children’s Health Literacy, Handwashing, and Nutrition Status in Low- and Middle-Income Countries. International Journal of Environmental Research and Public Health. 2021; 18(1):226. https://doi.org/10.3390/ijerph18010226
Chicago/Turabian StyleSangalang, Stephanie O., Shelley Anne J. Medina, Zheina J. Ottong, Allen Lemuel G. Lemence, Donrey Totanes, John Cedrick Valencia, Patricia Andrea A. Singson, Mikaela Olaguera, Nelissa O. Prado, Roezel Mari Z. Ocaña, and et al. 2021. "Protocol for a Trial Assessing the Impacts of School-Based WaSH Interventions on Children’s Health Literacy, Handwashing, and Nutrition Status in Low- and Middle-Income Countries" International Journal of Environmental Research and Public Health 18, no. 1: 226. https://doi.org/10.3390/ijerph18010226
APA StyleSangalang, S. O., Medina, S. A. J., Ottong, Z. J., Lemence, A. L. G., Totanes, D., Valencia, J. C., Singson, P. A. A., Olaguera, M., Prado, N. O., Ocaña, R. M. Z., Canja, R. J. F., Benolirao, A. J. T., Mariano, S. M. F., Gavieres, J. G., Aquino, C. P., Latag, E. C., Anglo, M. V. J. C., Borgemeister, C., & Kistemann, T. (2021). Protocol for a Trial Assessing the Impacts of School-Based WaSH Interventions on Children’s Health Literacy, Handwashing, and Nutrition Status in Low- and Middle-Income Countries. International Journal of Environmental Research and Public Health, 18(1), 226. https://doi.org/10.3390/ijerph18010226









