Predictive Value of the Cally Score in Determining Surgical Strategy for Complicated Left-Sided Colonic Diverticulitis: A Retrospective Cohort Study
Abstract
1. Introduction
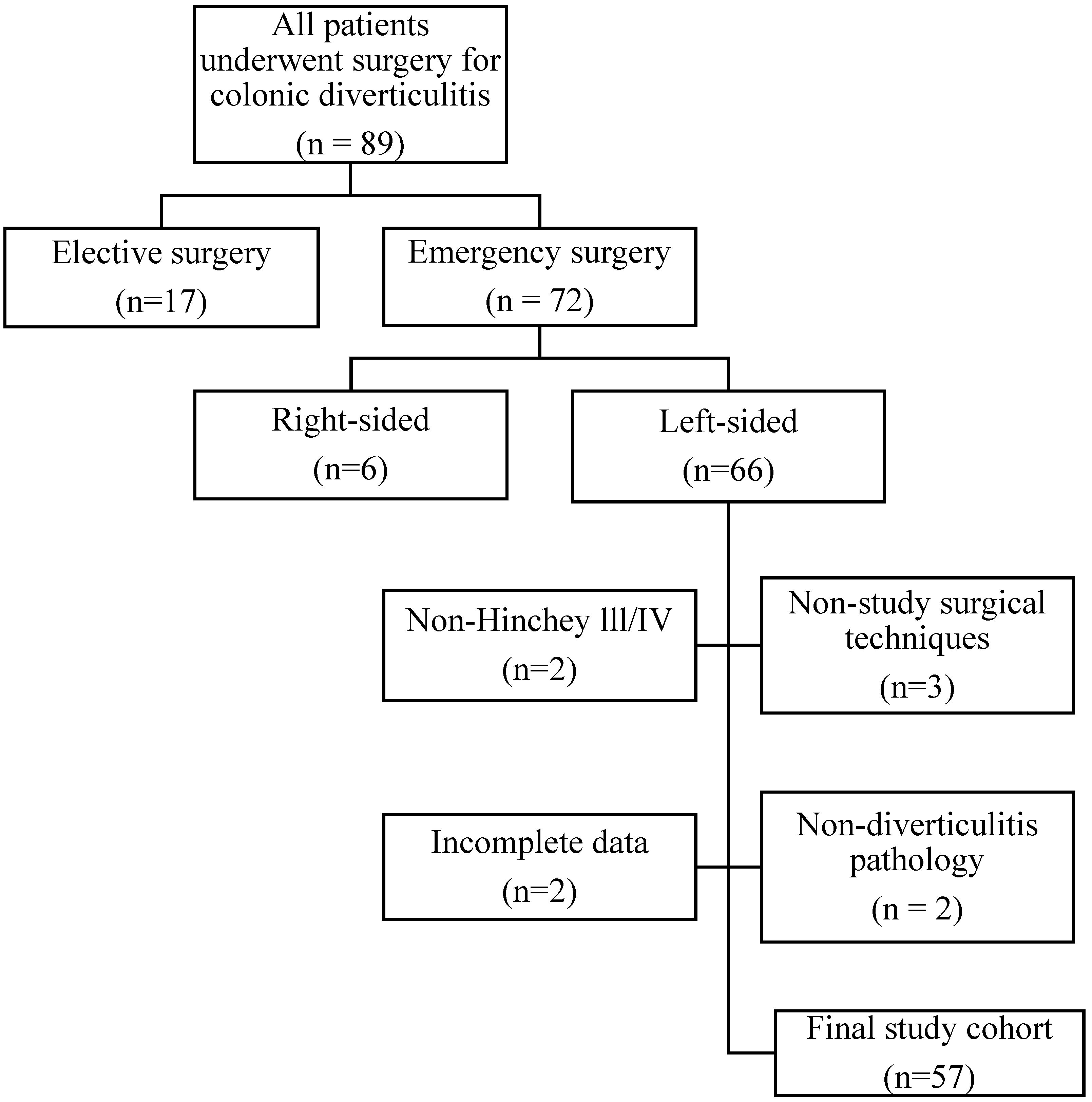
2. Materials and Methods
- Being over 18 years of age,
- Having complete access to data from hospital databases or clinical records,
- Having undergone operative treatment for Hinchey stage III or IV diverticulitis localized in the left-sided colon.
- Patients who have been treated operatively for reasons other than Hinchey stage III-IV (e.g., ileus, bleeding, fistula, unresponsiveness to conservative treatment),
- Surgical techniques other than resection and anastomosis (without diverting ileostomy) and the Hartmann procedure,
- Cases whose final pathology report is not compatible with diverticulitis.
2.1. Surgical Management
2.2. Statistical Analysis
3. Result
4. Discussion
5. Conclusions
- -
- A CALLY index < 0.45 was found to be an independent predictor of the Hartmann procedure in patients treated operatively for complicated left colonic diverticulitis.
- -
- The CALLY index is a practical index that combines CRP, albumin, and lymphocyte levels to comprehensively reflect the inflammatory response, immune status, and nutritional status.
- -
- Integration of this index into clinical decision processes may assist surgeons in more objective and personalized surgical technique decisions.
- -
- In addition, the study found that the Hartmann procedure was more frequently chosen in patients with albumin levels < 38.5 g/L and detected SIRS.
- -
- The findings indicate that not only anatomical staging but also the patient’s physiological status and laboratory parameters should be taken into account when deciding on the surgical technique.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Strate, L.L.; Morris, A.M. Epidemiology, Pathophysiology, and Treatment of Diverticulitis. Gastroenterology 2019, 156, 1282–1298.e1. [Google Scholar] [CrossRef] [PubMed]
- Imaeda, H.; Hibi, T. The Burden of Diverticular Disease and Its Complications: West versus East. Inflamm. Intest. Dis. 2018, 3, 61–68. [Google Scholar] [CrossRef]
- Shahedi, K.; Fuller, G.; Bolus, R.; Cohen, E.; Vu, M.; Shah, R.; Agarwal, N.; Kaneshiro, M.; Atia, M.; Sheen, V.; et al. Long-term risk of acute diverticulitis among patients with incidental diverticulosis found during colonoscopy. Clin. Gastroenterol. Hepatol. 2013, 11, 1609–1613. [Google Scholar] [CrossRef]
- Hupfeld, L.; Pommergaard, H.C.; Burcharth, J.; Rosenberg, J. Emergency admissions for complicated colonic diverticulitis are increasing: A nationwide register-based cohort study. Int. J. Color. Dis. 2018, 33, 879–886. [Google Scholar] [CrossRef]
- Acuna, S.A.; Wood, T.; Chesney, T.R.; Dossa, F.; Wexner, S.D.; Quereshy, F.A.; Chadi, S.A.; Baxter, N.N. Operative Strategies for Perforated Diverticulitis: A Systematic Review and Meta-analysis. Dis. Colon Rectum 2018, 61, 1442–1453. [Google Scholar] [CrossRef] [PubMed]
- Morris, A.M.; Regenbogen, S.E.; Hardiman, K.M.; Hendren, S. Sigmoid diverticulitis: A systematic review. JAMA 2014, 311, 287–297. [Google Scholar] [CrossRef] [PubMed]
- Obidike, P.C.; Lain, W.J.; Hoang, S.C. Robotic Surgical Management of Complicated Diverticulitis. Curr. Trauma Rep. 2025, 11, 14. [Google Scholar] [CrossRef]
- Huo, B.; Massey, L.H.; Seitidis, G.; Mavridis, D.; Antoniou, S.A.; EAES Diverticulitis Survey Advisory Group. Variation in the surgical management of complicated diverticulitis: A cross-sectional study of European surgeons. Surg. Endosc. 2025, 39, 691–698. [Google Scholar] [CrossRef] [PubMed]
- Cauley, C.E.; Patel, R.; Bordeianou, L. Use of Primary Anastomosis with Diverting Ileostomy in Patients with Acute Diverticulitis Requiring Urgent Operative Intervention. Dis. Colon Rectum 2018, 61, 586–592. [Google Scholar] [CrossRef]
- Rios Diaz, A.J.; Bevilacqua, L.A.; Habarth-Morales, T.E.; Zalewski, A.; Metcalfe, D.; Costanzo, C.; Yeo, C.J.; Palazzo, F. Primary anastomosis with diverting loop ileostomy vs. Hartmann’s procedure for acute diverticulitis: What happens after discharge? Results of a nationwide analysis. Surg. Endosc. 2024, 38, 2777–2787. [Google Scholar] [CrossRef] [PubMed]
- Riansuwan, W.; Hull, T.L.; Millan, M.M.; Hammel, J.P. Nonreversal of Hartmann’s procedure for diverticulitis: Derivation of a scoring system to predict nonreversal. Dis. Colon Rectum 2009, 52, 1400–1408. [Google Scholar] [CrossRef]
- Benli, S.; Tazeoğlu, D. The efficacy of hemoglobin, albumin, lymphocytes, and platelets (HALP) score in signifying acute appendicitis severity and postoperative outcomes. Updates Surg. 2023, 75, 1197–1202. [Google Scholar] [CrossRef]
- Angın, Y.S.; Şendil, A.M.; Zengin, A.; Ceylan, C.; Kılıç, M.; Ulaş, M. The predictive value of albumin-based nutritional indices for intestinal ischemia in strangulated abdominal wall hernias: An insight into the novel CALLY Index. Hernia 2025, 29, 168. [Google Scholar] [CrossRef]
- Bildik, B.; Çekmen, B.; Atiş, Ş.E.; Günaydın, Y.K.; Dorter, M. Evaluation of the relationship between Hemoglobin, Albumin, Lymphocyte, Platelet (HALP) score and treatment modality and mortality in patients with ileus. Ulus. Travma Acil Cerrahi Derg. 2023, 29, 1351–1356. [Google Scholar] [CrossRef]
- Sartelli, M.; Weber, D.G.; Kluger, Y.; Ansaloni, L.; Coccolini, F.; Abu-Zidan, F.; Augustin, G.; Ben-Ishay, O.; Biffl, W.L.; Bouliaris, K.; et al. 2020 update of the WSES guidelines for the management of acute colonic diverticulitis in the emergency setting. World J. Emerg. Surg. 2020, 15, 32. [Google Scholar] [CrossRef]
- Hall, J.; Hardiman, K.; Lee, S.; Lightner, A.; Stocchi, L.; Paquette, I.M.; Steele, S.R.; Feingold, D.L.; Prepared on behalf of the Clinical Practice Guidelines Committee of the American Society of Colon and Rectal Surgeons. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the Treatment of Left-Sided Colonic Diverticulitis. Dis. Colon Rectum 2020, 63, 728–747. [Google Scholar] [CrossRef]
- Yang, M.; Lin, S.Q.; Liu, X.Y.; Tang, M.; Hu, C.-L.; Wang, Z.-W.; Zhang, Q.; Zhang, X.; Song, M.-M.; Ruan, G.-T.; et al. Association between C-reactive protein-albumin-lymphocyte (CALLY) index and overall survival in patients with colorectal cancer: From the investigation on nutrition status and clinical outcome of common cancers study. Front. Immunol. 2023, 14, 1131496. [Google Scholar] [CrossRef] [PubMed]
- Demir, N.; Gökmen, İ.; Sağdıç Karateke, Y.; İlhan, A.; Yıldız, F.; Garbioğlu, D.B.; Yıldız, B. HALP score as a prognostic marker for overall survival in advanced pancreatic cancer. Front. Oncol. 2025, 15, 1542463. [Google Scholar] [CrossRef] [PubMed]
- Luo, B.; Tan, X.; Chen, L.; Zhou, K.; Lou, S. Combined association of systemic inflammatory response index and prognostic nutritional index with survival among US cancer survivors. BMC Cancer 2025, 25, 1114. [Google Scholar] [CrossRef] [PubMed]
- Demirelli, B.; Babacan, N.A.; Ercelep, Ö.; Öztürk, M.A.; Kaya, S.; Tanrıkulu, E.; Khalil, S.; Hasanov, R.; Alan, Ö.; Telli, T.A.; et al. Modified Glasgow Prognostic Score, Prognostic Nutritional Index and ECOG Performance Score Predicts Survival Better than Sarcopenia, Cachexia and Some Inflammatory Indices in Metastatic Gastric Cancer. Nutr. Cancer 2021, 73, 230–238. [Google Scholar] [CrossRef]
- Park, Y.Y.; Nam, S.; Han, J.H.; Lee, J.; Cheong, C. Predictive factors for conservative treatment failure of right colonic diverticulitis. Ann. Surg. Treat. Res. 2021, 100, 347–355. [Google Scholar] [CrossRef]
- Barlas, A.M.; Altıner, S.; Başpınar, A.; Aydın, S.M.; Doğanay, E.; Kaymak, Ş.; Ünal, Y. Predicting complicated acute diverticulitis with the HALP score: A retrospective study. Asian J. Surg. 2024, 48, 287–291. [Google Scholar] [CrossRef] [PubMed]
- Canlıkarakaya, F.; Ocaklı, S.; Doğan, İ.; Sucu, B.B.; Çınkıl, N.C. The role of inflammatory parameters in predicting acute complicated diverticulitis. Biomark. Med. 2025, 19, 463–469. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.M.; Bai PChang, J.; El Hechi, M.; Kongkaewpaisan, N.; Bonde, A.; Mendoza, A.E.; Saillant, N.N.; Fagenholz, P.J.; Velmahos, G.; Kaafarani, H.M. Hartmann’s Procedure vs Primary Anastomosis with Diverting Loop Ileostomy for Acute Diverticulitis: Nationwide Analysis of 2,729 Emergency Surgery Patients. J. Am. Coll. Surg. 2019, 229, 48–55. [Google Scholar] [CrossRef]
- Garfinkle, R.; Boutros, M. Current Management of Diverticulitis. Adv. Surg. 2024, 58, 87–106. [Google Scholar] [CrossRef]
- Shiraishi, T.; Nonaka, T.; Tominaga, T.; Takamura, Y.; Oishi, K.; Hashimoto, S.; Noda, K.; Ono, R.; Hisanaga, M.; Takeshita, H.; et al. The C-reactive protein-albumin-lymphocyte (CALLY) index is a useful predictor of postoperative complications in patients with a colonic stent for obstructive colorectal cancer: A Japanese multicenter study. Surg. Today 2025, 55, 502–509. [Google Scholar] [CrossRef]
- Akkuzu, M.Z.; Altıntaş, E.; Yaraş, S.; Sezgin, O.; Ateş, F.; Üçbilek, E.; Özdoğan, O. Controlling Nutritional Status (CONUT) Score and Prognostic Nutritional Index (PNI) Are Good Candidates for Prognostic Markers for Acute Pancreatitis. Medicina 2022, 59, 70. [Google Scholar] [CrossRef]
- Jain, V.; Nath, P.; Patro, S. Evaluation of diagnostic accuracy of inflammation markers [Neutrophil-Lymphocyte Ratio (NLR), Red cell Distribution Width (RDW), Prognostic Nutritional Index (PNI) and Lymphocyte Monocyte Ratio (LMR)] for outcomes in patients with acute pancreatitis. J. Assoc. Physicians India 2022, 70, 11–12. [Google Scholar] [PubMed]

| Primary Anastomosis (n = 17) | Hartmann’s Procedure (n = 40) | p Value | |
|---|---|---|---|
| Male sex β | 10 (58.52) | 25 (62.5) | 0.794 |
| Age α (years) | 56.47 ± 18.98 | 65.93 ± 14.09 | 0.042 |
| BMI Ω (kg/m2) | 26.44 ± 3.97 | 28.17 ± 4.51 | 0.176 |
| Diabetes mellitus β (Yes) | 1 (5.88) | 6 (15) | 0.337 |
| Pulmonary disease β (Yes) | 1 (5.88) | 11 (27.5) | 0.067 |
| Heart disease β (Yes) | 3 (17.64) | 16 (40) | 0.101 |
| Renal disease β (Yes) | 3 (17.64) | 3 (7.5) | 0.253 |
| SIRS β (Yes) | 2 (11.76) | 22 (55) | 0.002 |
| Hemoglobin α (g/dL) | 12.89 ± 2.04 | 12.63 ± 2.39 | 0.692 |
| Platelet Ω (109/L) | 300 (251.5–325.5) | 265 (227–345) | 0.595 |
| Lymphocyte Ω (109/L) | 1.80 (0.79–2.49) | 1.12 (0.70–1.46) | 0.02 |
| CRP Ω (mg/L) | 29.20 (17.75–147.10) | 153.50 (56.13–223.75) | 0.002 |
| PNI α | 49.86 ± 7.88 | 39.07 ± 8.19 | <0.001 |
| HALP Ω | 3365.37 (1442.51–5781.17) | 1594.44 (860.13–2399.7) | 0.018 |
| CALLY Ω | 1.02 (0.44–4.24) | 0.21 (0.11–0.47) | <0.001 |
| mGPS β (Score 2) | 1 (5.88) | 23 (57.5) | <0.001 |
| Albumin α (g/L) | 41.24 ± 4.02 | 33.68 ± 6.62 | <0.001 |
| Hinchey β (Stage IV) | 9 (52.94) | 29 (72.5) | 0.152 |
| Operative time α (min) | 150.59 ± 51.35 | 156.05 ± 58.06 | 0.738 |
| CDC β ≥ 3 | 2 (11.76) | 11 (27.5) | 0.195 |
| AUC (95% CI) | p Value | Cut-Off Value | Sensitivity (%) | Specificity (%) | |
|---|---|---|---|---|---|
| Age (years) | 0.646 (0.471–0.820) | 0.084 | 63.5 | 55.0 | 58.8 |
| CRP (mg/L) | 0.757 (0.606–0.907) | 0.002 | 68.5 | 70.0 | 70.6 |
| Albumin (g/L) | 0.835 (0.730–0.939) | <0.001 | 38.5 | 76.5 | 80.0 |
| Lymphocyte (109/L) | 0.696 (0.523–0.869) | 0.02 | 1.31 | 64.7 | 67.5 |
| PNI | 0.840 (0.732–0.948) | <0.001 | 43.22 | 76.5 | 77.5 |
| HALP | 0.700 (0.538–0.862) | 0.018 | 1800.98 | 58.8 | 55.0 |
| CALLY | 0.826 (0.718–0.935) | <0.001 | 0.45 | 70.6 | 72.5 |
| OR | 95% CI | p Value | |
|---|---|---|---|
| Albumin (<38.5 g/L) | 16.53 | 2.877–95.066 | 0.002 |
| SIRS (Yes) | 12.98 | 1.582–111.111 | 0.017 |
| CALLY (<0.45) | 6.40 | 1.136–36.158 | 0.035 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gungor, F.; Kılavuz, H.; Arslan, M.F.; Demir, M.; Korkmaz, Y.Y.; Bekraki, A.; Kurtulus, I. Predictive Value of the Cally Score in Determining Surgical Strategy for Complicated Left-Sided Colonic Diverticulitis: A Retrospective Cohort Study. Medicina 2025, 61, 1455. https://doi.org/10.3390/medicina61081455
Gungor F, Kılavuz H, Arslan MF, Demir M, Korkmaz YY, Bekraki A, Kurtulus I. Predictive Value of the Cally Score in Determining Surgical Strategy for Complicated Left-Sided Colonic Diverticulitis: A Retrospective Cohort Study. Medicina. 2025; 61(8):1455. https://doi.org/10.3390/medicina61081455
Chicago/Turabian StyleGungor, Feyyaz, Huseyin Kılavuz, Muhammed Furkan Arslan, Murat Demir, Yusuf Yunus Korkmaz, Ali Bekraki, and Idris Kurtulus. 2025. "Predictive Value of the Cally Score in Determining Surgical Strategy for Complicated Left-Sided Colonic Diverticulitis: A Retrospective Cohort Study" Medicina 61, no. 8: 1455. https://doi.org/10.3390/medicina61081455
APA StyleGungor, F., Kılavuz, H., Arslan, M. F., Demir, M., Korkmaz, Y. Y., Bekraki, A., & Kurtulus, I. (2025). Predictive Value of the Cally Score in Determining Surgical Strategy for Complicated Left-Sided Colonic Diverticulitis: A Retrospective Cohort Study. Medicina, 61(8), 1455. https://doi.org/10.3390/medicina61081455





