Ultrasonographic Assessment of Meniscus Damage in the Context of Clinical Manifestations
Abstract
1. Introduction
1.1. Background
1.2. The Most Important Practical Aspects of Meniscus Anatomy
1.3. The Method of Examination and the Physiological Image of the Meniscus in Ultrasonography
1.4. Diagnostic Methods in Meniscal Pathologies Imaging
2. Materials and Methods
3. Results
3.1. Most Common Pathologies of Menisci
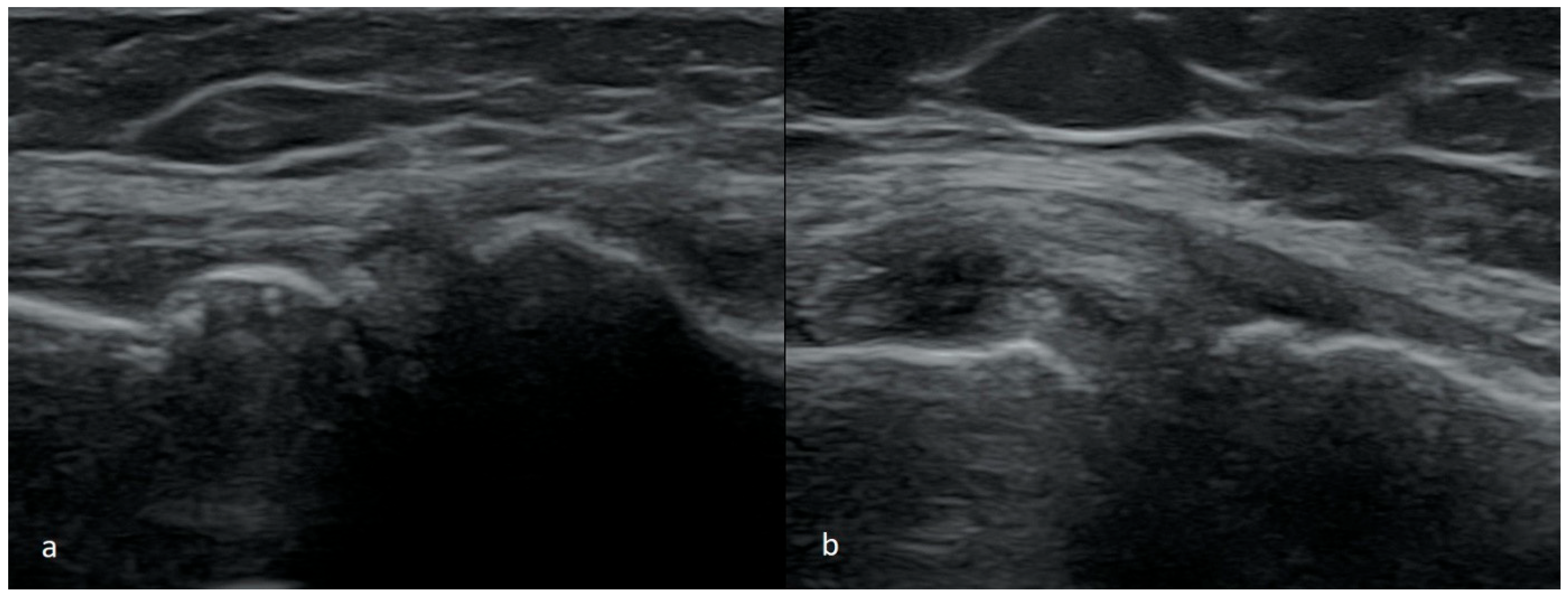
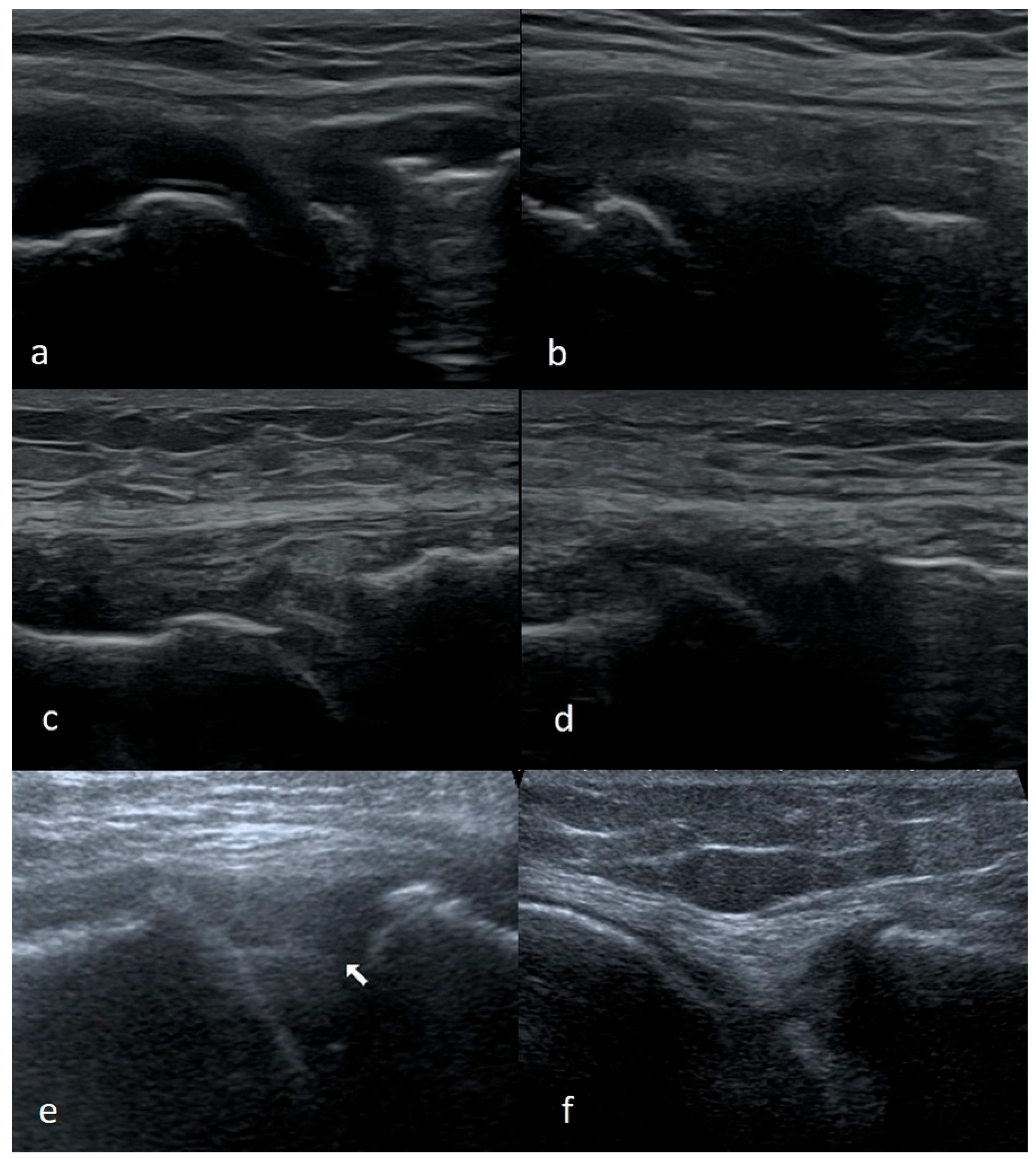
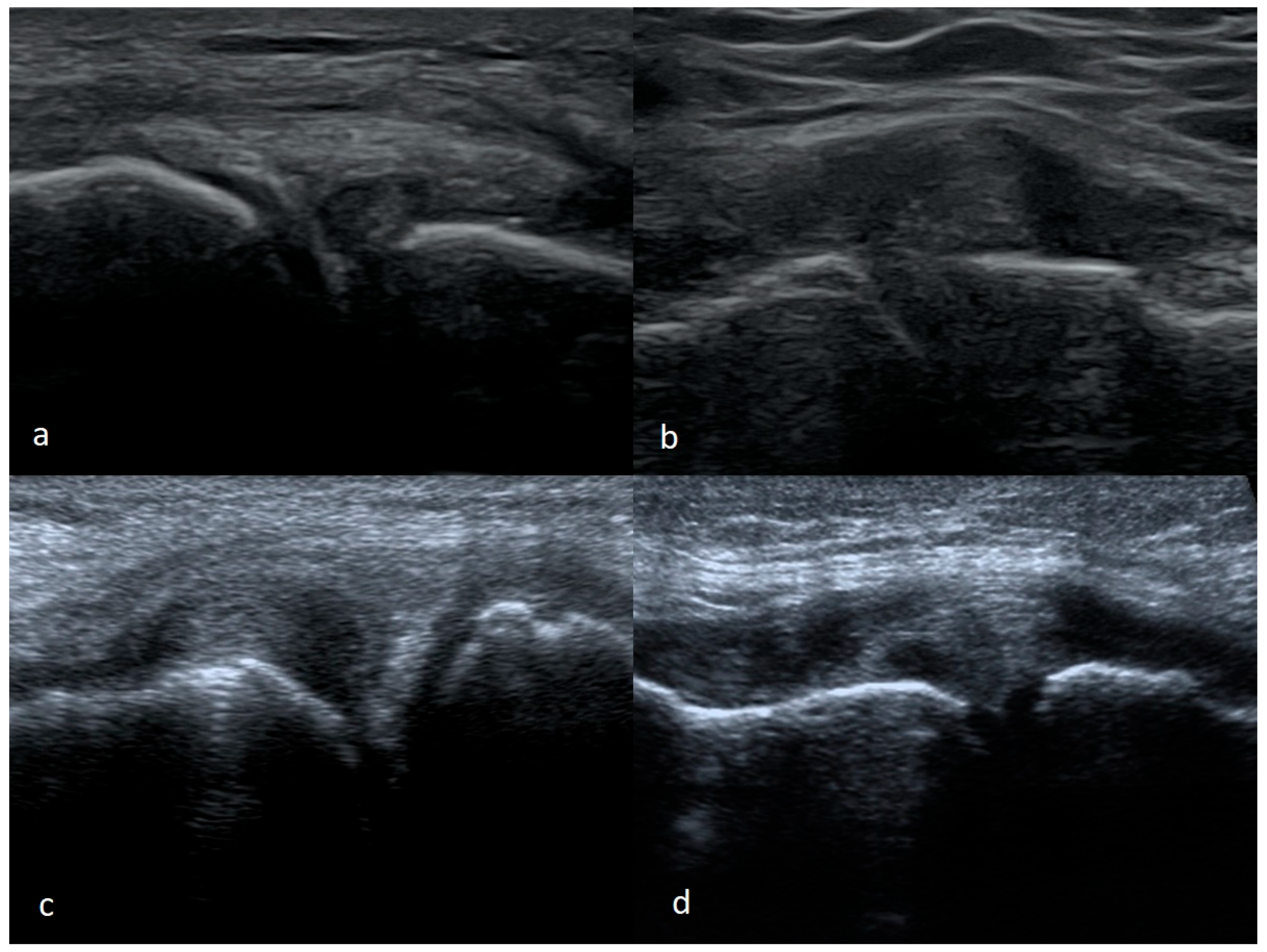
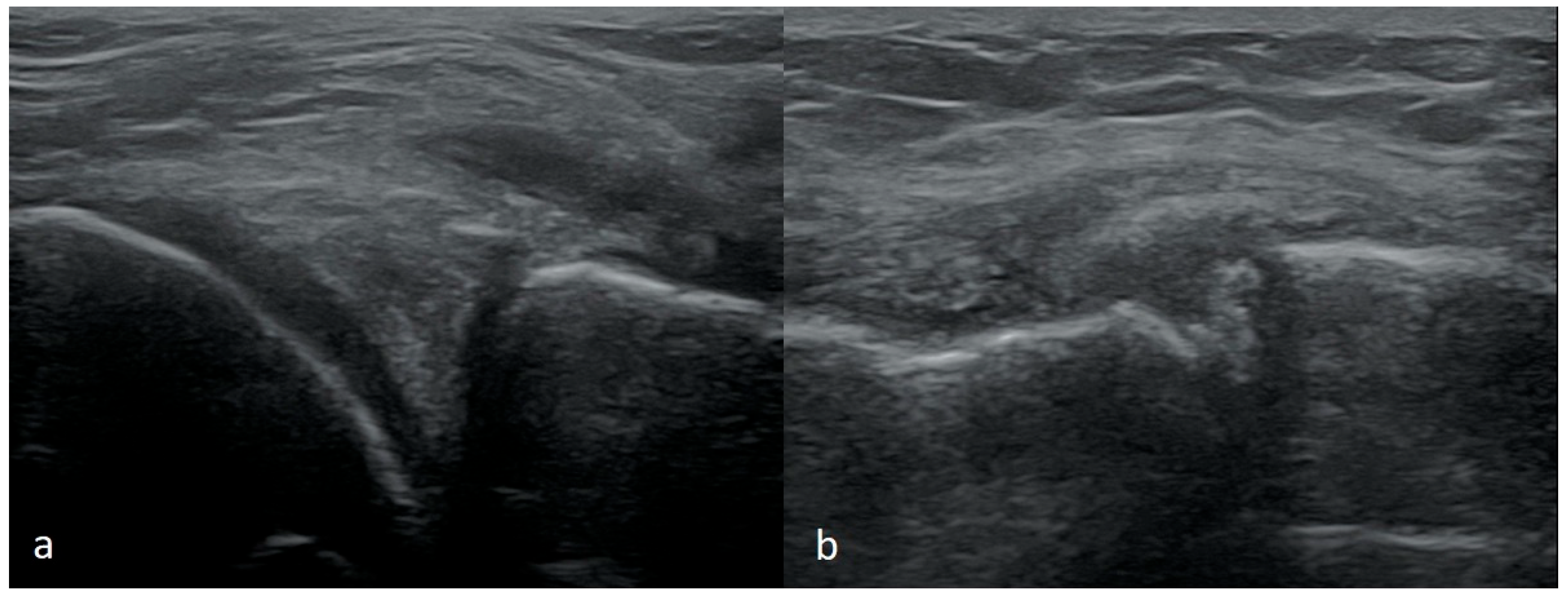
3.1.1. Meniscus Tears
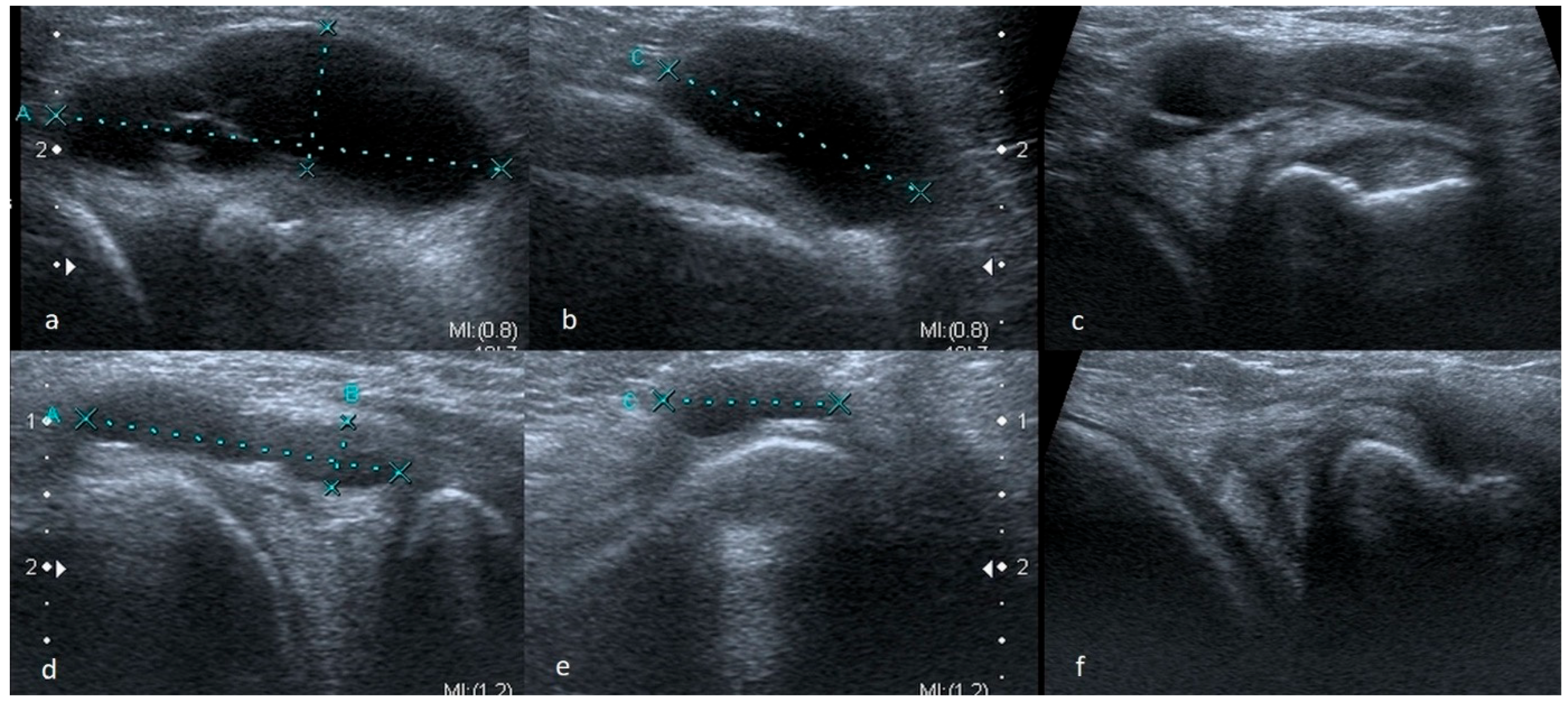
3.1.2. Meniscus Cysts
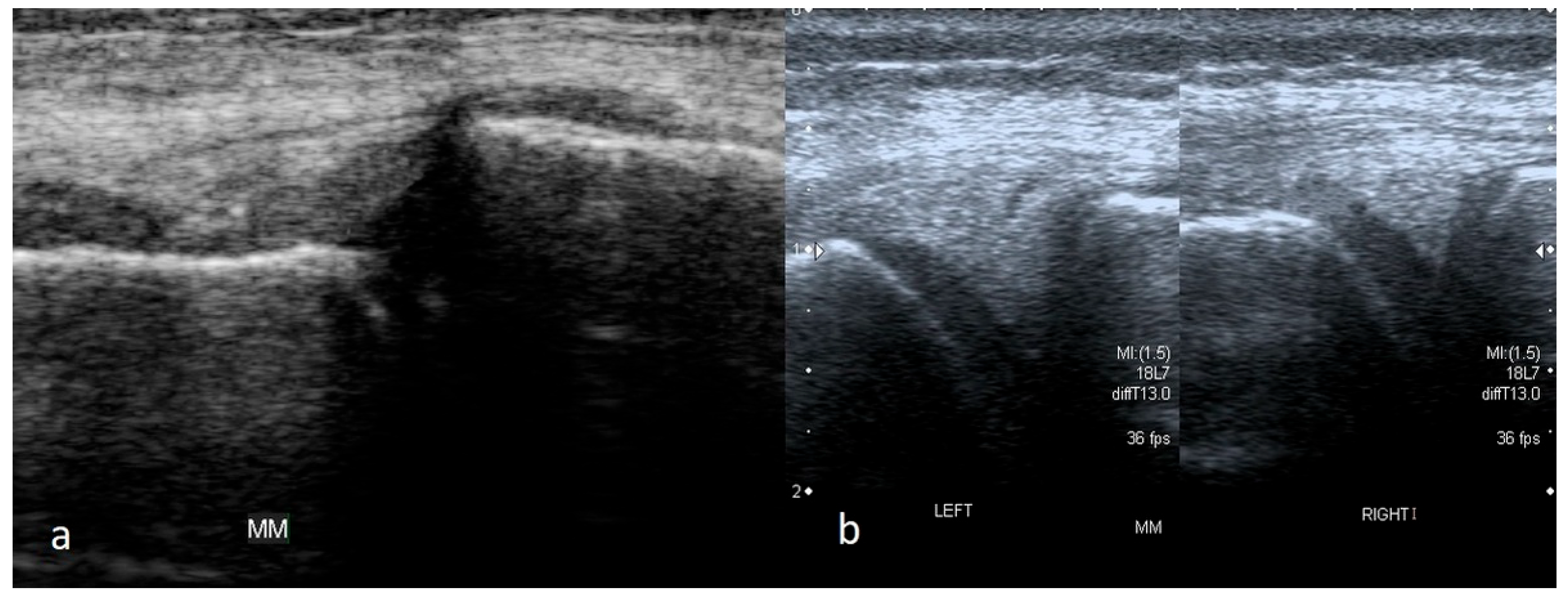
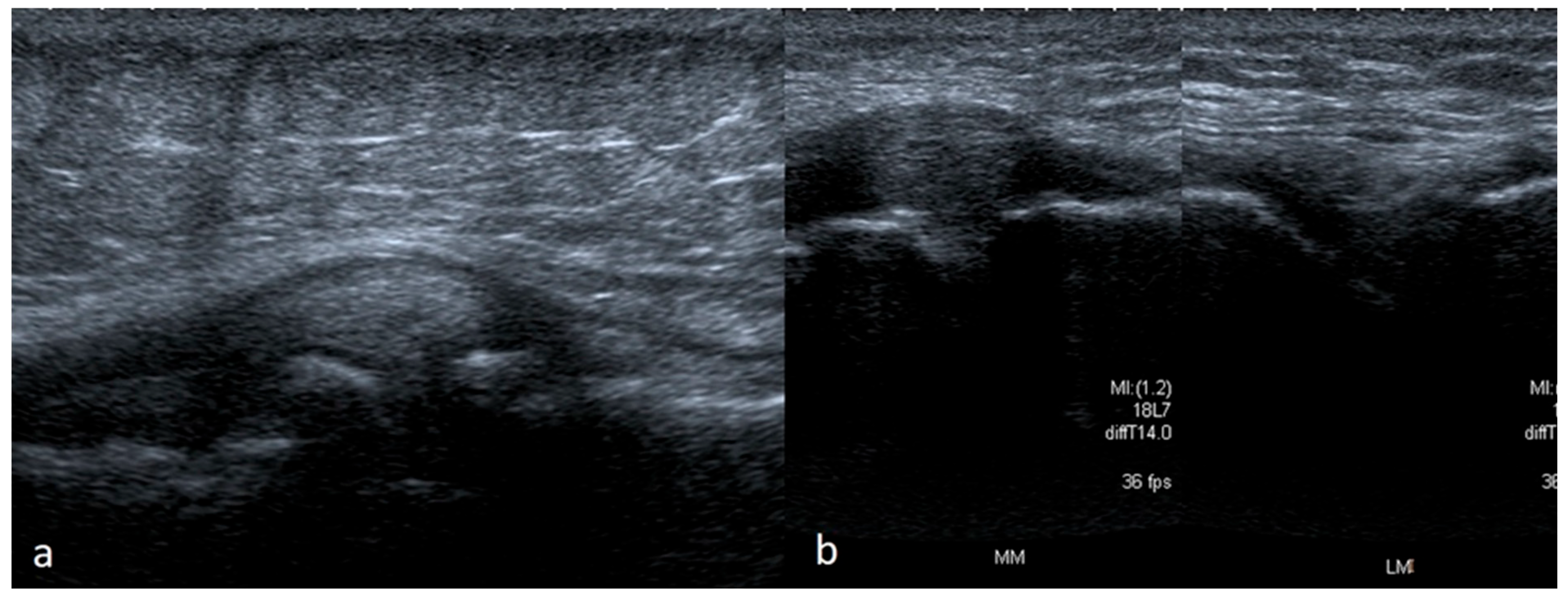
3.1.3. Bucket-Handle Tears
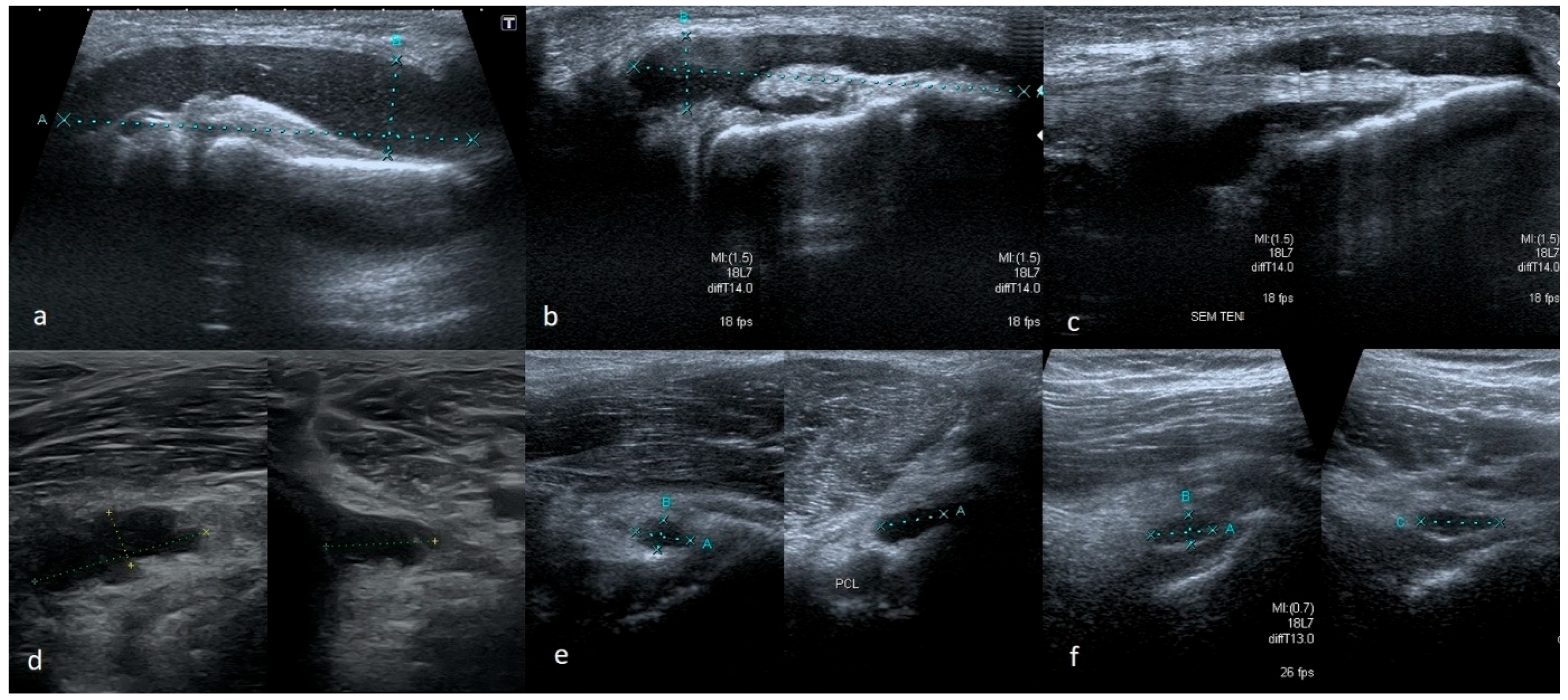
3.1.4. Meniscal Flap Tears
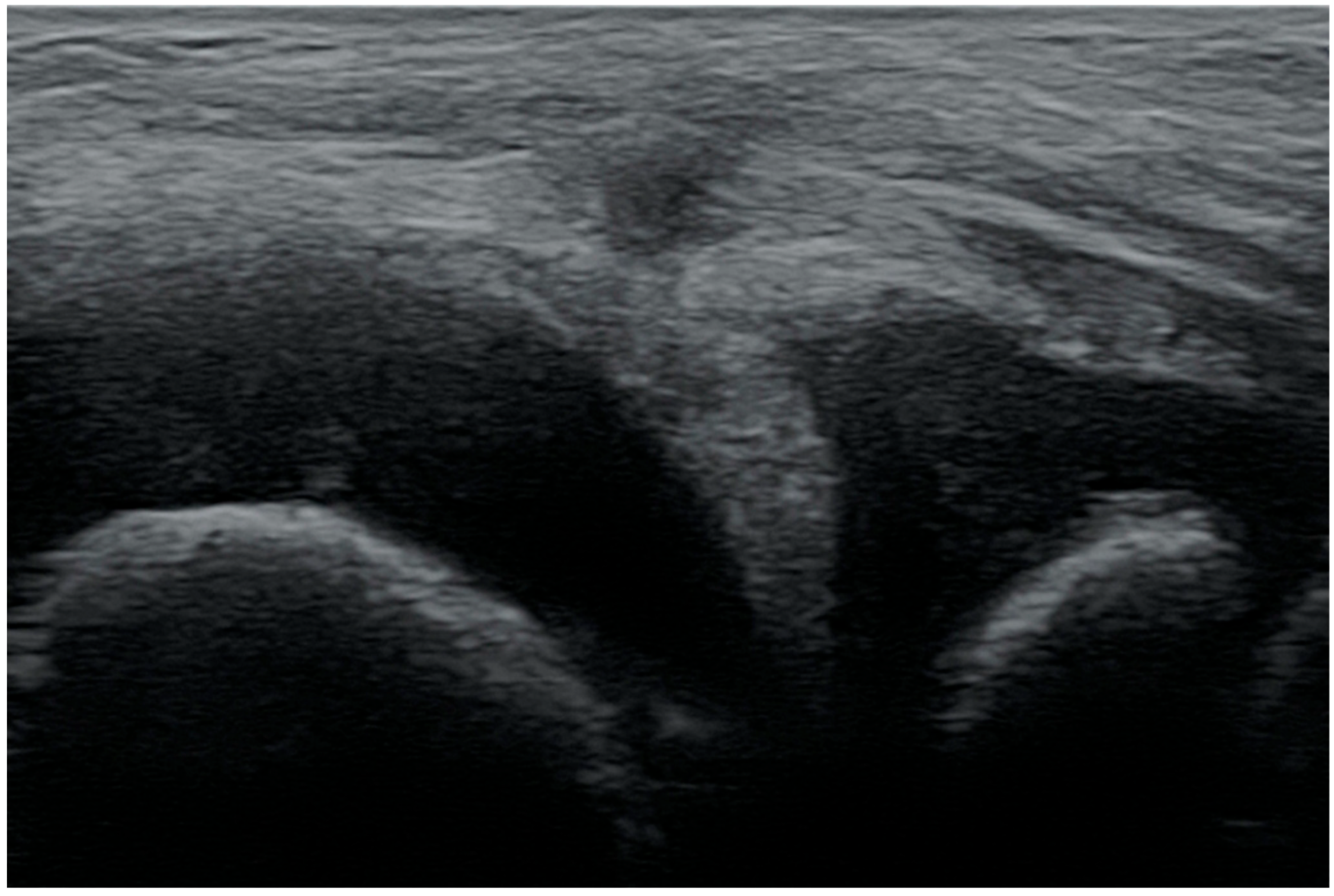
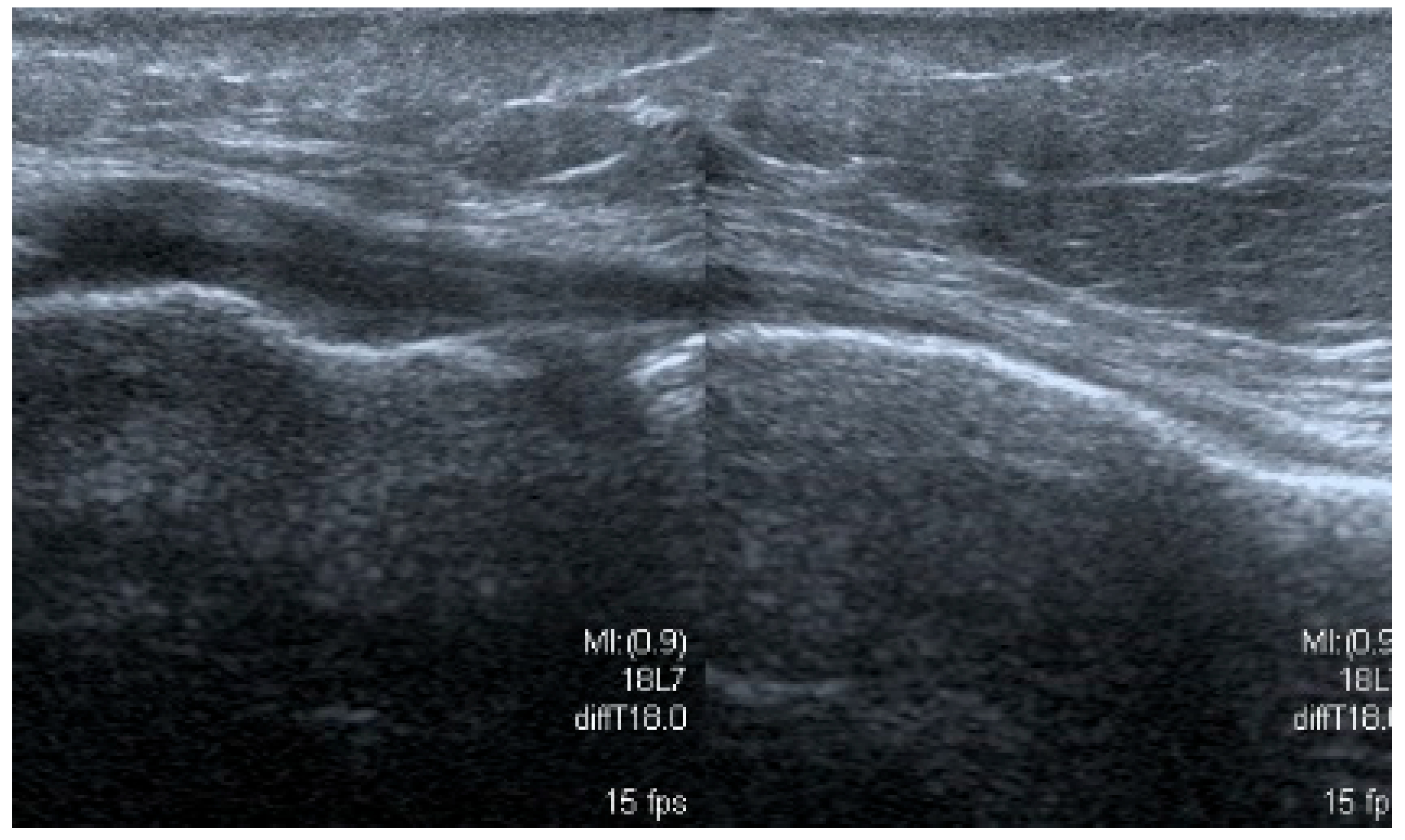
3.1.5. Degenerative Changes of Menisci
3.2. The Results of the Retrospective Analysis
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Brantigan, O.C.; Voshell, A.F. Ligaments of the knee joint; the relationship of the ligament of Humphry to the ligament of Wrisberg. J. Bone Jt. Surg. 1946, 28, 66. [Google Scholar] [PubMed]
- Flandry, F.; Hommel, G. Normal anatomy and biomechanics of the knee. Sports Med. Arthrosc. Rev. 2011, 19, 82–92. [Google Scholar] [CrossRef] [PubMed]
- Kummer, B. Anatomie und Biomechanik des Kniegelenksmeniscus [Anatomy and biomechanics of the meniscus of the knee joint]. Langenbecks Arch. Chir. 1987, 372, 241–246. (In German) [Google Scholar] [CrossRef] [PubMed]
- Renström, P.; Johnson, R.J. Anatomy and biomechanics of the menisci. Clin. Sports Med. 1990, 9, 523–538. [Google Scholar] [CrossRef] [PubMed]
- Fox, A.J.; Wanivenhaus, F.; Burge, A.J.; Warren, R.F.; Rodeo, S.A. The human meniscus: A review of anatomy, function, injury, and advances in treatment. Clin. Anat. 2015, 28, 269–287. [Google Scholar] [CrossRef] [PubMed]
- Markes, A.R.; Hodax, J.D.; Ma, C.B. Meniscus Form and Function. Clin. Sports Med. 2020, 39, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Mureşan, S.; Mureşan, M.; Voidăzan, S.; Neagoe, R. The accuracy of musculoskeletal ultrasound examination for the exploration of meniscus injuries in athletes. J. Sports Med. Phys. Fit. 2017, 57, 589–594. [Google Scholar] [CrossRef] [PubMed]
- Elshimy, A.; Osman, A.M.; Awad, M.E.S.; Abdel Aziz, M.M. Diagnostic accuracy of point-of-care knee ultrasound for evaluation of meniscus and collateral ligaments pathology in comparison with MRI. Acta Radiol. 2023, 64, 2283–2292. [Google Scholar] [CrossRef] [PubMed]
- Johnson, S.E.; Kruse, R.C.; Boettcher, B.J. The Role of Ultrasound in the Diagnosis and Treatment of Meniscal Injuries. Curr. Rev. Musculoskelet. Med. 2024, 17, 171–184. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ahmadi, O.; Motififard, M.; Heydari, F.; Hatami, S.; Meibody, A.A. The predictive value of point-of-care ultrasonography versus magnetic resonance imaging in assessing medial meniscal tears in patients with acute knee injury. Clin. Exp. Emerg. Med. 2024, 11, 188–194. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Smith, B.W.; Green, G.A. Acute knee injuries: Part I. History and physical examination. Am. Fam. Physician 1995, 51, 615–621. [Google Scholar] [PubMed]
- Karachalios, T.; Hantes, M.; Zibis, A.H.; Zachos, V.; Karantanas, A.H.; Malizos, K.N. Diagnostic accuracy of a new clinical test (the Thessaly test) for early detection of meniscal tears. J. Bone Jt. Surg. Am. 2005, 87, 955–962. [Google Scholar] [CrossRef] [PubMed]
- Harrison, B.K.; Abell, B.E.; Gibson, T.W. The Thessaly test for detection of meniscal tears: Validation of a new physical examination technique for primary care medicine. Clin. J. Sport Med. 2009, 19, 9–12. [Google Scholar] [CrossRef] [PubMed]
- Konan, S.; Rayan, F.; Haddad, F.S. Do physical diagnostic tests accurately detect meniscal tears? Knee Surg. Sports Traumatol. Arthrosc. 2009, 17, 806–811. [Google Scholar] [CrossRef] [PubMed]
- Solomon, D.H.; Simel, D.L.; Bates, D.W.; Katz, J.N.; Schaffer, J.L. The rational clinical examination. Does this patient have a torn meniscus or ligament of the knee? Value of the physical examination. JAMA 2001, 286, 1610–1620. [Google Scholar] [CrossRef] [PubMed]
- Ockert, B.; Haasters, F.; Polzer, H.; Grote, S.; Kessler, M.A.; Mutschler, W.; Kanz, K.G. Der verletzte Meniskus: Wie sicher ist die klinische Untersuchung? Eine Metaanalyse [Value of the clinical examination in suspected meniscal injuries. A meta-analysis]. Unfallchirurg 2010, 113, 293–299. (In German) [Google Scholar] [CrossRef] [PubMed]
- Lee, S.Y.; Jee, W.H.; Kim, J.M. Radial tear of the medial meniscal root: Reliability and accuracy of MRI for diagnosis. AJR. Am. J. Roentgenol. 2008, 191, 81–85. [Google Scholar] [CrossRef] [PubMed]
- Culvenor, A.G.; Øiestad, B.E.; Hart, H.F.; Stefanik, J.J.; Guermazi, A.; Crossley, K.M. Prevalence of knee osteoarthritis features on magnetic resonance imaging in asymptomatic uninjured adults: A systematic review and meta-analysis. Br. J. Sports Med. 2019, 53, 1268–1278. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rutten, M.J.; Collins, J.M.; van Kampen, A.; Jager, G.J. Meniscal cysts: Detection with high-resolution sonography. AJR. Am. J. Roentgenol. 1998, 171, 491–496. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Paczesny, Ł.; Kruczyński, J. Ultrasound of the knee. In Seminars in Ultrasound, CT and MRI; WB Saunders: Orlando, FL, USA, 2011; Volume 32, pp. 114–124. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.J.; Chow, K. Ultrasound of the knee. In Seminars in Musculoskeletal Radiology; Thieme Medical Publishers: New York, NY USA, 2007; Volume 11, pp. 137–148. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, J.A.; Ruangchaijatuporn, T.; Khoury, V.; Magerkurth, O. Ultrasound of the Knee: Common Pathology Excluding Extensor Mechanism. In Seminars in Musculoskeletal Radiology; Thieme Medical Publishers: New York, NY USA, 2017; Volume 21, pp. 102–112. [Google Scholar] [CrossRef] [PubMed]
- Alves, T.I.; Girish, G.; Kalume Brigido, M.; Jacobson, J.A. US of the Knee: Scanning Techniques, Pitfalls, and Pathologic Conditions. Radiographics 2016, 36, 1759–1775. [Google Scholar] [CrossRef] [PubMed]
- Bellisari, G.; Samora, W.; Klingele, K. Meniscus tears in children. Sports Med. Arthrosc. Rev. 2011, 19, 50–55. [Google Scholar] [CrossRef] [PubMed]
- Kramer, D.E.; Micheli, L.J. Meniscal tears and discoid meniscus in children: Diagnosis and treatment. J. Am. Acad. Orthop. Surg. 2009, 17, 698–707. [Google Scholar] [CrossRef] [PubMed]
- Jackson, J.L.; O’Malley, P.G.; Kroenke, K. Evaluation of acute knee pain in primary care. Ann. Intern. Med. 2003, 139, 575–588. [Google Scholar] [CrossRef] [PubMed]
- Frobell w Cooper, R.; Morris, H.; Hutchinson, M. Acute knee injuries. In Brukner & Khan’s Clinical Sports Medicine: Injuries; Brukner, P., Clarsen, B., Cook, J., Cools, A., Crossley, K., Hutchinson, M., McCrory, P., Bahr, R., Khan, K., Eds.; McGraw Hill: New York, NY, USA, 2017; Volume 1, p. 5e. Available online: https://csm.mhmedical.com/content.aspx?bookid=1970§ionid=168694712 (accessed on 20 December 2021).
- Howell, R.; Kumar, N.S.; Patel, N.; Tom, J. Degenerative meniscus: Pathogenesis, diagnosis, and treatment options. World J. Orthop. 2014, 5, 597–602. [Google Scholar] [CrossRef] [PubMed]
- Lubowitz, J.H.; Brand, J.C.; Rossi, M.J. Nonoperative Management of Degenerative Meniscus Tears Is Worth a Try. Arthroscopy 2020, 36, 327–328. [Google Scholar] [CrossRef] [PubMed]
- Wells, M.E.; Scanaliato, J.P.; Dunn, J.C.; Garcia, E.J. Meniscal Injuries: Mechanism and Classification. Sports Med. Arthrosc. Rev. 2021, 29, 154–157. [Google Scholar] [CrossRef] [PubMed]
- Wolf, B.R.; Gulbrandsen, T.R. Degenerative Meniscus Tear in Older Athletes. Clin. Sports Med. 2020, 39, 197–209. [Google Scholar] [CrossRef] [PubMed]
- Beaufils, P.; Becker, R.; Kopf, S.; Englund, M.; Verdonk, R.; Ollivier, M.; Seil, R. Surgical management of degenerative meniscus lesions: The 2016 ESSKA meniscus consensus. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 335–346. [Google Scholar] [CrossRef] [PubMed]
- Kise, N.J.; Risberg, M.A.; Stensrud, S.; Ranstam, J.; Engebretsen, L.; Roos, E.M. Exercise therapy versus arthroscopic partial meniscectomy for degenerative meniscal tear in middle aged patients: Randomised controlled trial with two year follow-up. BMJ 2016, 354, i3740, Erratum in BMJ 2017, 356, j266; Erratum in BMJ 2018, 363, k4893. [Google Scholar] [CrossRef] [PubMed]
- Shetty, A.A.; Tindall, A.J.; James, K.D.; Relwani, J.; Fernando, K.W. Accuracy of hand-held ultrasound scanning in detecting meniscal tears. J. Bone Jt. Surg. Br. 2008, 90, 1045–1048. [Google Scholar] [CrossRef] [PubMed]
- Park, G.Y.; Kim, J.M.; Lee, S.M.; Lee, M.Y. The value of ultrasonography in the detection of meniscal tears diagnosed by magnetic resonance imaging. Am. J. Phys. Med. Rehabil. 2008, 87, 14–20. [Google Scholar] [CrossRef] [PubMed]
- Xia, X.P.; Chen, H.L.; Zhou, B. Ultrasonography for meniscal injuries in knee joint: A systematic review and meta-analysis. J. Sports Med. Phys. Fit. 2016, 56, 1179–1187. [Google Scholar] [PubMed]
- Awan, F.; Mondal, P.; van der Merwe, J.M.; Vassos, N.; Obaid, H. The Utility of a Community-Based Knee Ultrasound in Detecting Meniscal Tears: A Retrospective Analysis in Comparison with MRI. Healthcare 2024, 12, 2051. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shanbhogue, A.K.; Sandhu, M.S.; Singh, P.; Ojili, V.; Khandelwal, N.; Sen, R. Real time spatial compound ultrasound in the evaluation of meniscal injuries: A comparison study with conventional ultrasound and MRI. Knee 2009, 16, 191–195. [Google Scholar] [CrossRef] [PubMed]
- Wareluk, P.; Szopinski, K.T. Value of modern sonography in the assessment of meniscal lesions. Eur. J. Radiol. 2012, 81, 2366–2369. [Google Scholar] [CrossRef] [PubMed]
- Cook, J.L.; Cook, C.R.; Stannard, J.P.; Vaughn, G.; Wilson, N.; Roller, B.L.; Stoker, A.M.; Jayabalan, P.; Hdeib, M.; Kuroki, K. MRI versus ultrasonography to assess meniscal abnormalities in acute knees. J. Knee. Surg. 2014, 27, 319–324. [Google Scholar] [CrossRef] [PubMed]
- Alizadeh, A.; Babaei Jandaghi, A.; Keshavarz Zirak, A.; Karimi, A.; Mardani-Kivi, M.; Rajabzadeh, A. Knee sonography as a diagnostic test for medial meniscal tears in young patients. Eur. J. Orthop. Surg. Traumatol. 2013, 23, 927–931. [Google Scholar] [CrossRef] [PubMed]
- Brimmo, O.A.; Smith, P.A.; Cook, C.R.; Cook, J.L. Sonographic Diagnosis of an Acute Lateral Meniscus Tear in a Division I Collegiate American Football Player. J. Knee Surg. Rep. 2015, 1, 057–059. [Google Scholar] [CrossRef]
- Gray, S.D.; Kaplan, P.A.; Dussault, R.G. Imaging of the knee. Current status. Orthop. Clin. N. Am. 1997, 28, 643–658. [Google Scholar] [CrossRef] [PubMed]
- Bureau, N.J.; Kaplan, P.A.; Dussault, R.G. MRI of the knee: A simplified approach. Curr. Probl. Diagn. Radiol. 1995, 24, 4–49. [Google Scholar] [CrossRef] [PubMed]
- Crawford, R.; Walley, G.; Bridgman, S.; Maffulli, N. Magnetic resonance imaging versus arthroscopy in the diagnosis of knee pathology, concentrating on meniscal lesions and ACL tears: A systematic review. Br. Med. Bull. 2007, 84, 5–23. [Google Scholar] [CrossRef] [PubMed]
- Boden, S.D.; Davis, D.O.; Dina, T.S.; Stoller, D.W.; Brown, S.D.; Vailas, J.C.; Labropoulos, P.A. A prospective and blinded investigation of magnetic resonance imaging of the knee. Abnormal findings in asymptomatic subjects. Clin. Orthop. Relat. Res. 1992, 282, 177–185. [Google Scholar] [CrossRef] [PubMed]
- Englund, M.; Guermazi, A.; Gale, D.; Hunter, D.J.; Aliabadi, P.; Clancy, M.; Felson, D.T. Incidental meniscal findings on knee MRI in middle-aged and elderly persons. N. Engl. J. Med. 2008, 359, 1108–1115. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zanetti, M.; Pfirrmann, C.W.; Schmid, M.R.; Romero, J.; Seifert, B.; Hodler, J. Patients with suspected meniscal tears: Prevalence of abnormalities seen on MRI of 100 symptomatic and 100 contralateral asymptomatic knees. AJR Am. J. Roentgenol. 2003, 181, 635–641. [Google Scholar] [CrossRef] [PubMed]


| Pathology | % of Identified Lesions | Echogenicity Pattern | Mobility/Pain |
|---|---|---|---|
| Degenerative lesions | 70.9 |
|
|
| Cystic lesions | 13.4 |
|
|
| Complex tears | 6.0 |
|
|
| Flap tears | 3.7 |
|
|
| Vertical pericapsular tears | 2.2 |
|
|
| Partial thickness tears | 2.2 |
|
|
| Bucket-handle-type tears | 1.5 |
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Poboży, T.; Konarski, W.; Janowski, K.; Michalak, K.; Poboży, K.; Domańska-Poboża, J. Ultrasonographic Assessment of Meniscus Damage in the Context of Clinical Manifestations. Medicina 2025, 61, 1339. https://doi.org/10.3390/medicina61081339
Poboży T, Konarski W, Janowski K, Michalak K, Poboży K, Domańska-Poboża J. Ultrasonographic Assessment of Meniscus Damage in the Context of Clinical Manifestations. Medicina. 2025; 61(8):1339. https://doi.org/10.3390/medicina61081339
Chicago/Turabian StylePoboży, Tomasz, Wojciech Konarski, Kacper Janowski, Klaudia Michalak, Kamil Poboży, and Julia Domańska-Poboża. 2025. "Ultrasonographic Assessment of Meniscus Damage in the Context of Clinical Manifestations" Medicina 61, no. 8: 1339. https://doi.org/10.3390/medicina61081339
APA StylePoboży, T., Konarski, W., Janowski, K., Michalak, K., Poboży, K., & Domańska-Poboża, J. (2025). Ultrasonographic Assessment of Meniscus Damage in the Context of Clinical Manifestations. Medicina, 61(8), 1339. https://doi.org/10.3390/medicina61081339






