Effect of Regular Electrotherapy on Spinal Flexibility and Pain Sensitivity in Patients with Chronic Non-Specific Neck Pain and Low Back Pain: A Randomized Controlled Double-Blinded Pilot Trial
Abstract
1. Introduction
2. Materials and Methods
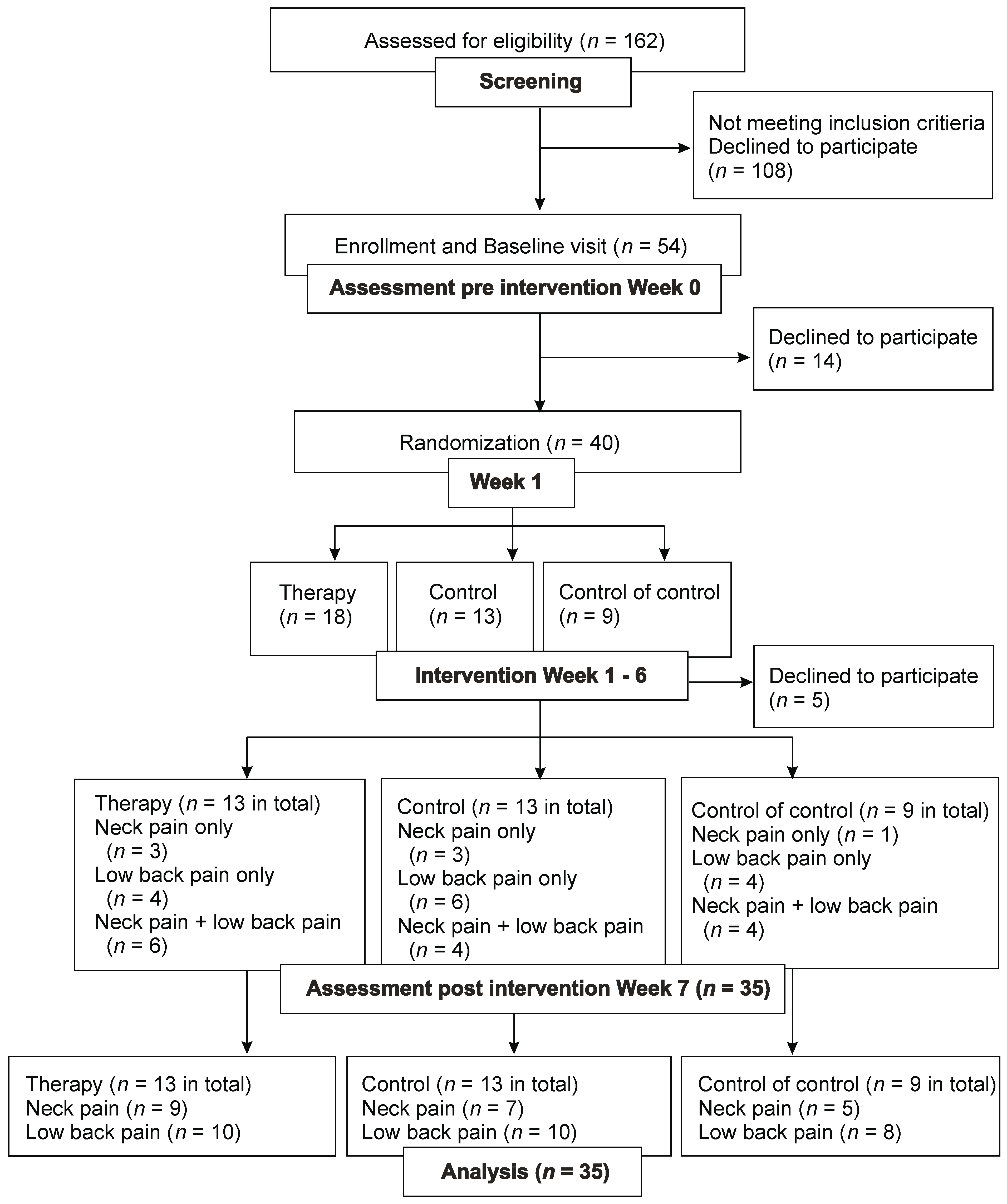
2.1. Study Design
2.2. Ethics and Clinical Registration
2.3. Study Population
2.4. Study Process
2.5. Randomization and Blinding
2.6. Outcome Measurements
2.7. Statistical Analysis
3. Results
3.1. Neck Pain
3.2. Low Back Pain
4. Discussion
5. Future Directions and Clinical Implications
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Maher, C.; Underwood, M.; Buchbinder, R. Non-specific low back pain. Lancet 2017, 389, 736–747. [Google Scholar] [CrossRef]
- Melzack, R.; Wall, P.D. Pain mechanisms: A new theory. Science 1965, 150, 971–979. [Google Scholar] [CrossRef]
- Vance, C.G.; Dailey, D.L.; Rakel, B.A.; Sluka, K.A. Using TENS for pain control: The state of the evidence. Pain Manag. 2014, 4, 197–209. [Google Scholar] [CrossRef]
- Do Carmo Almeida, T.C.; Dos Santos Figueiredo, F.W.; Barbosa Filho, V.C.; de Abreu, L.C.; Fonseca, F.L.A.; Adami, F. Effects of Transcutaneous Electrical Nerve Stimulation on Proinflammatory Cytokines: Systematic Review and Meta-Analysis. Mediat. Inflamm. 2018, 2018, 1094352. [Google Scholar] [CrossRef]
- Martimbianco, A.L.C.; Porfírio, G.J.; Pacheco, R.L.; Torloni, M.R.; Riera, R. Transcutaneous electrical nerve stimulation (TENS) for chronic neck painz. Cochrane Database Syst. Rev. 2019, 12, CD011927. [Google Scholar] [CrossRef]
- Khadilkar, A.; Odebiyi, D.O.; Brosseau, L.; Wells, G.A. Transcutaneous electrical nerve stimulation (TENS) versus placebo for chronic low-back pain. Cochrane Database Syst. Rev. 2008, 2008, CD003008. [Google Scholar] [CrossRef]
- Kroeling, P.; Gross, A.; Graham, N.; Burnie, S.J.; Szeto, G.; Goldsmith, C.H.; Haines, T.; Forget, M. Electrotherapy for neck pain. Cochrane Database Syst. Rev. 2013, CD004251. [Google Scholar] [CrossRef]
- Eriksson, M.B.E.; Sjölund, B.H.; Nielzén, S. Long term results of peripheral conditioning stimulation as an analgesic measure in chronic pain. Pain 2019, 6, 335–347. [Google Scholar] [CrossRef]
- Han, J.S. Acupuncture: Neuropeptide release produced by electrical stimulation of different frequencies. Trends Neurosci. 2003, 26, 17–22. [Google Scholar] [CrossRef]
- Van Hecke, O.; Hocking, L.J.; Torrance, N.; Campbell, A.; Padmanabhan, S.; Porteous, D.J.; McIntosh, A.M.; Burri, A.V.; Tanaka, H.; Williams, F.M.; et al. Chronic pain, depression and cardiovascular disease linked through a shared genetic predisposition: Analysis of a family-based cohort and twin study. PLoS ONE 2017, 12, e0170653. [Google Scholar] [CrossRef]
- Haedtke, C.; Smith, M.; VanBuren, J.; Klein, D.; Turvey, C. The Characteristics of Pain in Patients Diagnosed with Depression and Heart Failure. Pain Manag. Nurs. 2017, 18, 353–362. [Google Scholar] [CrossRef]
- Deyo, R.A.; Walsh, N.E.; Martin, D.C.; Schoenfeld, L.S.; Ramamurthy, S. A controlled trial of transcutaneous electrical nerve stimulation (TENS) and exercise for chronic low back pain. N. Engl. J. Med. 1990, 322, 1627–1634. [Google Scholar] [CrossRef]
- Rajfur, J.; Pasternok, M.; Rajfur, K.; Walewicz, K.; Fras, B.; Bolach, B.; Dymarek, R.; Rosinczuk, J.; Halski, T.; Taradaj, J. Efficacy of Selected Electrical Therapies on Chronic Low Back Pain: A Comparative Clinical Pilot Study. Med. Sci. Monit. 2017, 23, 85–100. [Google Scholar] [CrossRef] [PubMed]
- Kamper, S.J.; Apeldoorn, A.T.; Chiarotto, A.; Smeets, R.J.; Ostelo, R.W.; Guzman, J.; van Tulder, M.W. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain. Cochrane Syst. Rev. Meta-Anal. 2015, 18, 239–240. [Google Scholar] [CrossRef] [PubMed]
- Marin, T.J.; Van Eerd, D.; Irvin, E.; Couban, R.; Koes, B.W.; Malmivaara, A.; van Tulder, M.W.; Kamper, S.J. Multidisciplinary Biopsychosocial Rehabilitation for Subacute Low Back Pain. Cochrane Database Syst. Rev. 2017, 6, CD002193. [Google Scholar] [CrossRef]
- Van Laarhoven, A.I.; Vogelaar, M.L.; Wilder-Smith, O.H.; van Riel, P.L.; van de Kerkhof, P.C.; Kraaimaat, F.W.; Evers, A.W. Induction of nocebo and placebo effects on itch and pain by verbal suggestions. Pain 2011, 152, 1486–1494. [Google Scholar] [CrossRef]
- Nees, F.; Ditzen, B.; Flor, H. When shared pain is not half the pain: Enhanced central nervous system processing and verbal reports of pain in the presence of a solicitous spouse. Pain 2022, 163, e1006–e1012. [Google Scholar] [CrossRef]
- Sánchez Romero, E.A.; Lim, T.; Villafañe, J.H.; Boutin, G.; Aguado, V.; Pintado-Zugasti, A.; Alonso Pérez, J.L.; Fernández Carnero, J. The Influence of Verbal Suggestion on Post-Needling Soreness and Pain Processing after Dry Needling treatment: An Experimental Study. Int. J. Environ. Res. Public Health 2021, 18, 4206. [Google Scholar] [CrossRef]
- Fernández-Carnero, J.; Beltrán-Alacreu, H.; Arribas-Romano, A.; Cerezo-Téllez, E.; Cuenca-Zaldivar, J.N.; Sánchez-Romero, E.A.; Lara, S.L.; Villafane, J.H. Prediction of Patient Satisfaction after Treatment of Chronic Neck Pain with Mulligan’s Mobilization. Life 2022, 13, 48. [Google Scholar] [CrossRef]
- Ballestra, E.; Battaglino, A.; Cotella, D.; Rossettini, G.; Sanchez-Romero, E.A.; Villafane, J.H. Do patients’ expectations influence conservative treatment in Chronic Low Back Pain? A Narrative Review. Retos 2002, 46, 395–403. [Google Scholar] [CrossRef]
- Pérez, S.E.M.; González, L.L.; Acevedo, I.A.; Barrera, R.B.; Pérez, J.L.A.; Romero, E.A.S.; Reina, M.D.S.; Pérez, I.M.M.; Villafañe, J.H. Attitudes and beliefs towards low back pain (LBP) among physiotherapists in Spain. Bull. Fac. Phys. Ther. 2022, 27, 52. [Google Scholar] [CrossRef]
- Rossettini, G.; Carlino, E.; Testa, M. Clinical relevance of contextual factors as triggers of placebo and nocebo effects in musculoskeletal pain. BMC Musculoskelet. Disord. 2018, 19, 27. [Google Scholar] [CrossRef]
- Sherriff, B.; Clark, C.; Killingback, C.; Newell, D. Impact of contextual factors on patient outcomes following conservative low back pain treatment: Systematic review. Chiropr. Man. Therap. 2022, 30, 20. [Google Scholar] [CrossRef]
- James, K.E.; Bloch, D.A.; Lee, K.K.; Kraemer, H.C.; Fuller, R.K. An index for assessing blindness in a multi-centre clinical trial: Disulfiram for alcohol cessation—A VA cooperative study. Clinical Trial 1996, 15, 1421–1434. [Google Scholar] [CrossRef]
- Bang, H.; Ni, L.; Davis, C.E. Assessment of blinding in clinical trials. Control. Clin. Trials 2004, 25, 143–156. [Google Scholar] [CrossRef]
- Pop, T.; Austrup, H.; Preuss, R.; Niedziałek, M.; Zaniewska, A.; Sobolewski, M.; Dobrowolski, T.; Zwolińska, J. Effect of TENS on pain relief in patients with degenerative disc disease in lumbosacral spine. Ortop. Traumatol. Rehabil. 2010, 12, 289–300. [Google Scholar]
- Borsook, D.; Youssef, A.M.; Simons, L.; Elman, I.; Eccleston, C. When pain gets stuck: The evolution of pain chronification and treatment resistance. Pain 2018, 159, 2421–2436. [Google Scholar] [CrossRef]
- Tajerian, M.; Clark, J.D. Nonpharmacological Interventions in Targeting Pain-Related Brain Plasticity. Neural Plast. 2017, 2017, 2038573. [Google Scholar] [CrossRef]



| Age of Patients with Neck Pain in Years | BMI of Patients with Neck Pain | |
|---|---|---|
| Therapy (n = 9) | 48.2 ± 17.27 | 25.38 ± 4.87 |
| Control (n = 7) | 45.94 ± 14.59 | 22.28 ± 4.05 |
| Control of control (n = 5) | 49.61 ± 16.83 | 29.43 ± 8.37 |
| Age of Patients with Low Back Pain in Years | BMI of Patients with Low Back Pain | |
|---|---|---|
| Therapy (n = 10) | 56.66. ± 17.02 | 26.06 ± 3.85 |
| Control (n = 10) | 48.48 ± 17.7 | 24.96 ± 4.34 |
| Control of control (n = 8) | 52.64 ± 22.17 | 30.77 ± 9.05 |
| Neck Disability Index | SF-MPQ Neck Pain | Rolland Morris Questionnaire | SF-MPQ Low Back Pain | |
|---|---|---|---|---|
| Therapy | ||||
| 32.0 ± 19.72 | 76.22 ± 32.21 | 11.30 ± 3.95 | 71.4 ± 33.36 |
| 31.33 ± 20.83 | 68.11 ± 36.39 | 11.30 ± 6.09 | 77.2 ± 35.64 |
| Control | ||||
| 21.14 ± 8.55 | 59.71 ± 21.40 | 8.00 ± 4.99 | 59.40 ± 28.44 |
| 17.43 ± 7.80 | 54.14 ± 26.77 | 5.90 ± 5.69 | 44.30 ± 40.79 |
| Control of control | ||||
| 29.60 ± 8.30 | 72.60 ± 50.27 | 10.25 ± 6.50 | 40.88 ± 43.56 |
| 24.80 ± 15.01 | 82.00 ± 35.48 | 10.00 ± 6.72 | 55.00 ± 52.38 |
| Anteflexion | Retroflexion | Lateral Flexion to the Right | Lateral Flexion to the Left | Rotation to the Right | Rotation to the Left | |
| Therapy | ||||||
| 51.7 ± 8.4 | 62.2 ± 21.6 | 33.9 ± 9.6 | 32.8 ± 7.9 | 59.2 ± 18.7 | 56.7 ± 13.9 |
| 52.8 ± 13.2 | 63 ± 16.9 | 36.1 ± 10.5 | 33.7 ± 9.8 | 61.2 ± 16.5 | 62.8 ± 14.7 |
| Control | ||||||
| 46.9 ± 14.8 | 59 ± 17.4 | 34.9 ± 12 | 35.3 ± 7.9 | 54.9 ± 15.1 | 58.9 ± 12.2 |
| 49.3 ± 10.6 | 61.9 ± 19.5 | 33.6 ± 9.9 | 36.4 ± 11.4 | 60.4 ± 7.5 | 56.7 ± 11.7 |
| Control of control | ||||||
| 46 ± 15.2 | 50 ± 16.2 | 31.4 ± 8 | 32 ± 5.7 | 56.4 ± 13.3 | 52 ± 16.8 |
| 45.2 ± 13.1 | 48 ± 12.6 | 27.8 ± 12.3 | 33.2 ± 10.1 | 58.2 ± 14.9 | 56 ± 20.8 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Naka, A.; Kotz, C.; Gutmann, E.; Pramhas, S.; Schukro, R.P.J.; Ristl, R.; Schuhfried, O.; Crevenna, R.; Sator, S. Effect of Regular Electrotherapy on Spinal Flexibility and Pain Sensitivity in Patients with Chronic Non-Specific Neck Pain and Low Back Pain: A Randomized Controlled Double-Blinded Pilot Trial. Medicina 2023, 59, 823. https://doi.org/10.3390/medicina59050823
Naka A, Kotz C, Gutmann E, Pramhas S, Schukro RPJ, Ristl R, Schuhfried O, Crevenna R, Sator S. Effect of Regular Electrotherapy on Spinal Flexibility and Pain Sensitivity in Patients with Chronic Non-Specific Neck Pain and Low Back Pain: A Randomized Controlled Double-Blinded Pilot Trial. Medicina. 2023; 59(5):823. https://doi.org/10.3390/medicina59050823
Chicago/Turabian StyleNaka, Asami, Clea Kotz, Edith Gutmann, Sibylle Pramhas, Regina Patricia Juliane Schukro, Robin Ristl, Othmar Schuhfried, Richard Crevenna, and Sabine Sator. 2023. "Effect of Regular Electrotherapy on Spinal Flexibility and Pain Sensitivity in Patients with Chronic Non-Specific Neck Pain and Low Back Pain: A Randomized Controlled Double-Blinded Pilot Trial" Medicina 59, no. 5: 823. https://doi.org/10.3390/medicina59050823
APA StyleNaka, A., Kotz, C., Gutmann, E., Pramhas, S., Schukro, R. P. J., Ristl, R., Schuhfried, O., Crevenna, R., & Sator, S. (2023). Effect of Regular Electrotherapy on Spinal Flexibility and Pain Sensitivity in Patients with Chronic Non-Specific Neck Pain and Low Back Pain: A Randomized Controlled Double-Blinded Pilot Trial. Medicina, 59(5), 823. https://doi.org/10.3390/medicina59050823








