Is the Direct Anterior Approach for Total Hip Arthroplasty Effective in Obese Patients? Early Clinical and Radiographic Results from a Retrospective Comparative Study
Abstract
1. Introduction
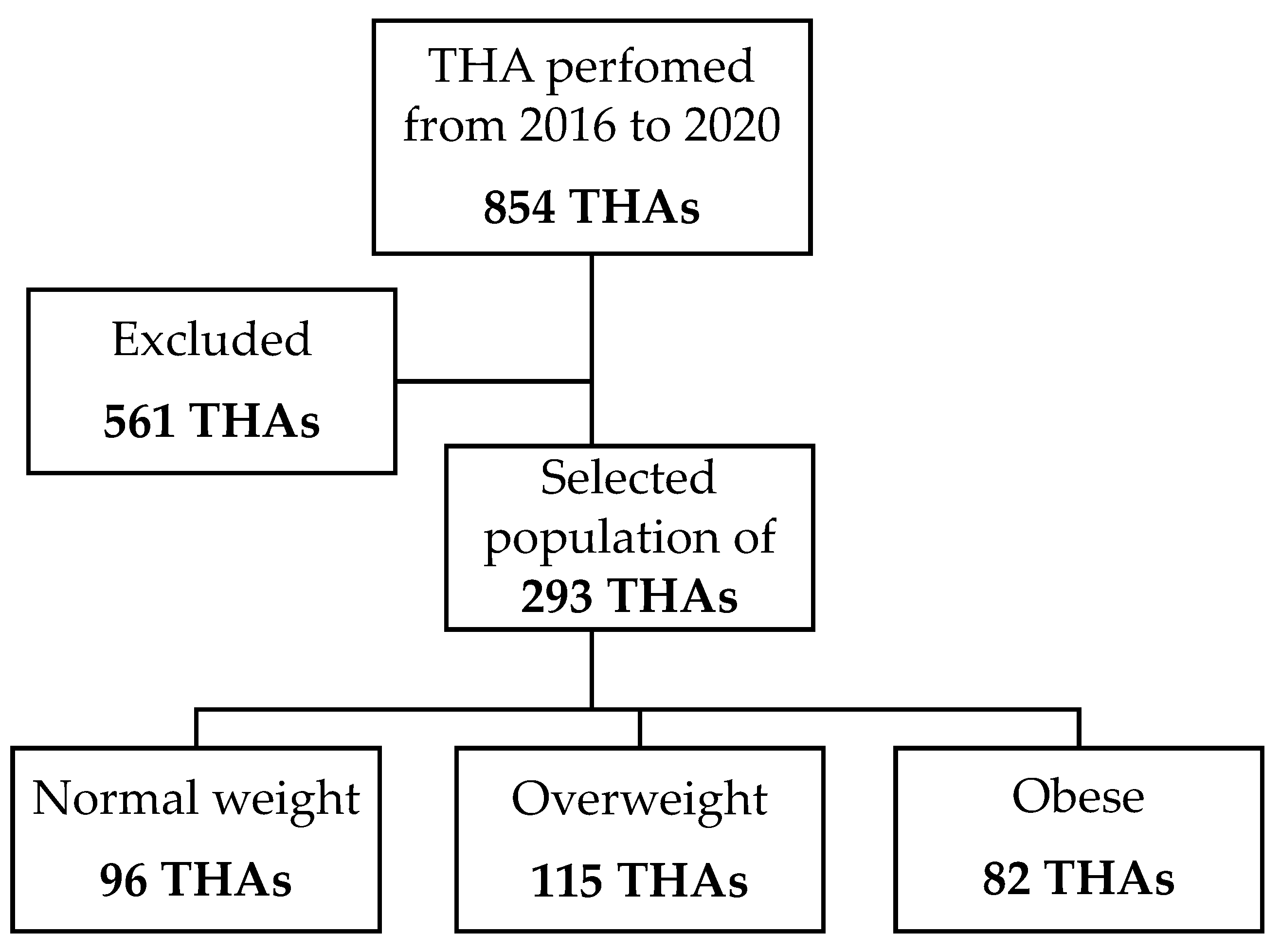
2. Materials and Methods
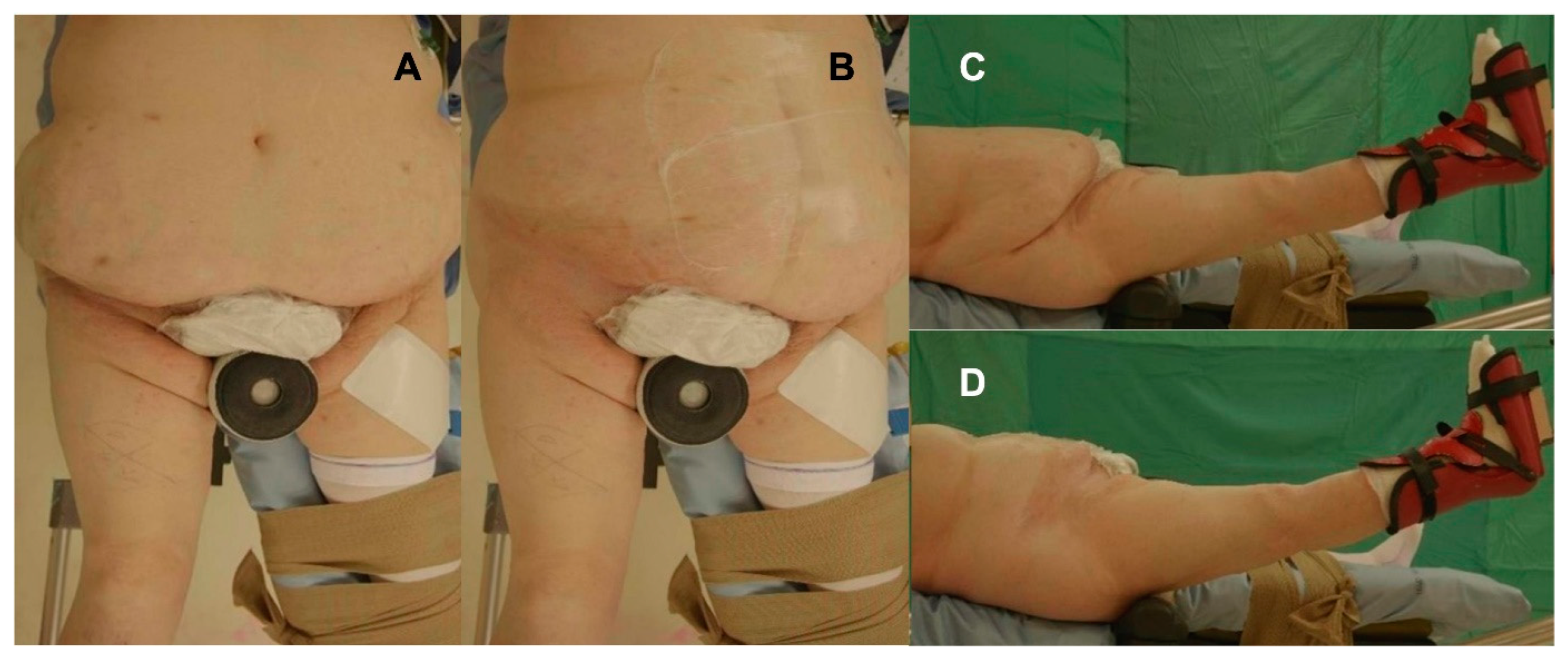
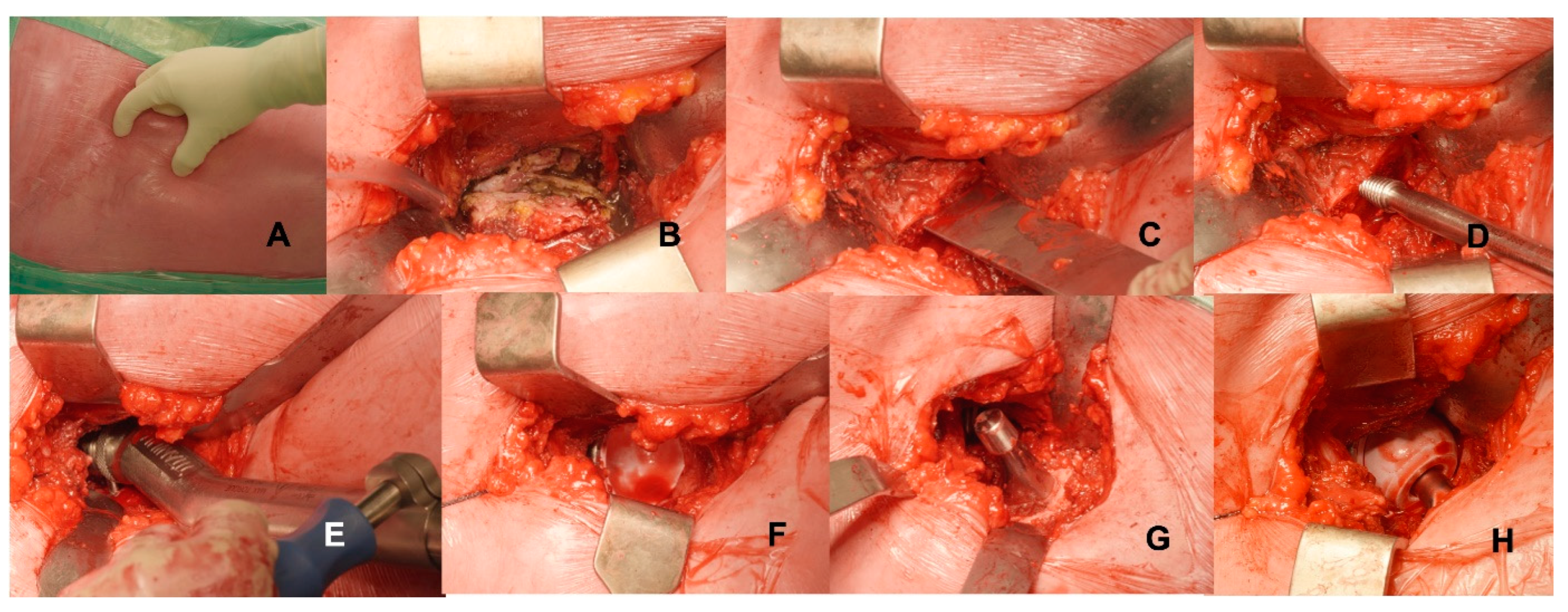
2.1. Surgical Technique
2.2. Post-Operative Care
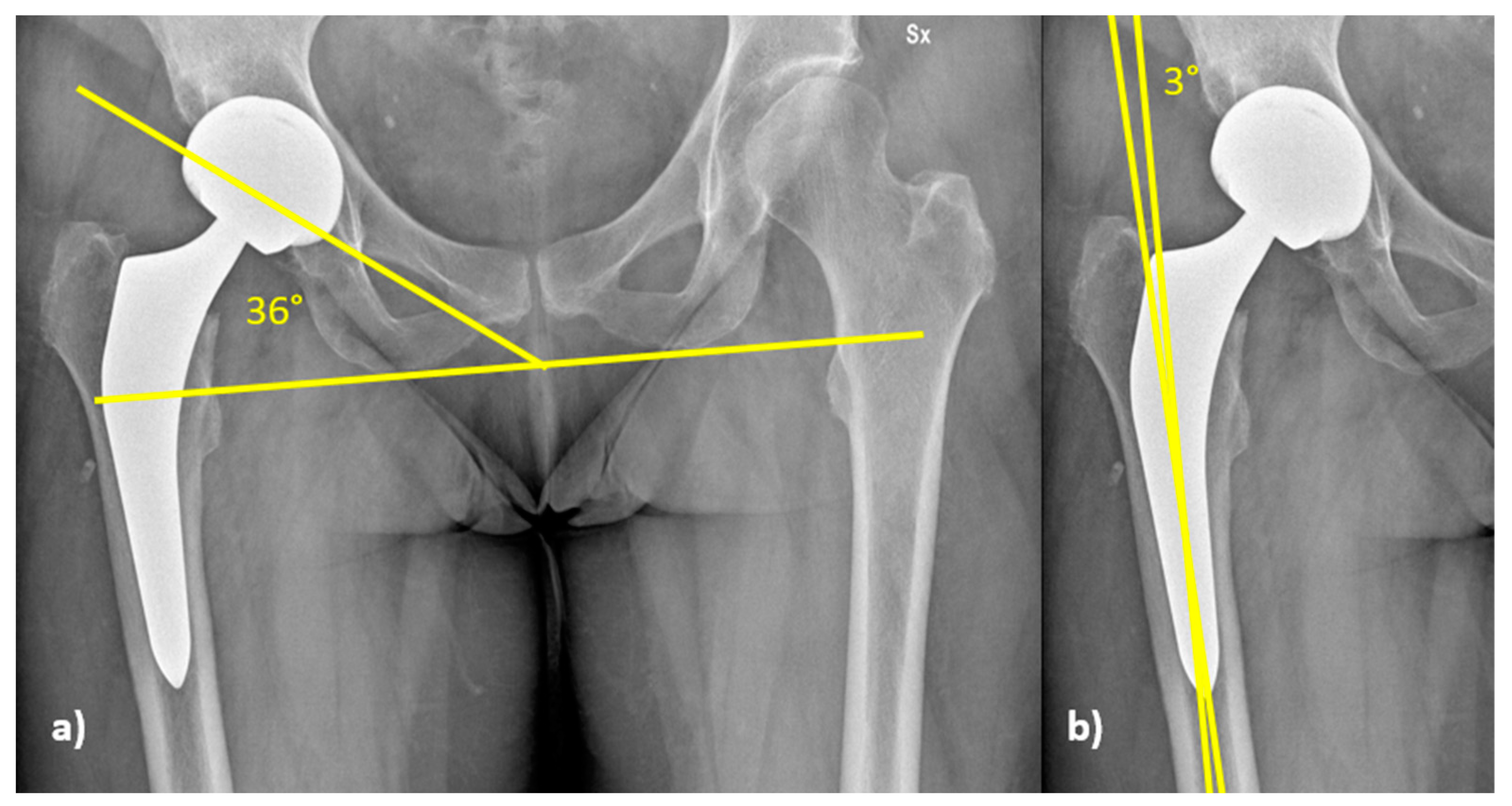
2.3. Radiological Evaluation
2.4. Statistical Analysis
3. Results
3.1. Patients’ Demographics and Characteristics
3.2. Radiographic Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviation
| THA | Total hip arthroplasty |
| DAA | Direct Anterior Approach |
| BMI | Body Mass Index |
| NW | Normal weight patients |
| OW | Overweight patients |
| OB | Obese patients |
| ASA | American Society of Anesthesiologists |
| NRS | Numerical Rating Scale |
References
- Yumuk, V.; Tsigos, C.; Fried, M.; Schindler, K.; Busetto, L.; Micic, D.; Toplak, H. European Guidelines for Obesity Management in Adults. Obes. Facts 2015, 8, 402–424. [Google Scholar] [CrossRef]
- Caroline, M.; Apovian, M.D. Obesity: Definition, Comorbidities, Causes, and Burden. Am. J. Manag. Care. 2016, 22, S176–S185. [Google Scholar]
- Andolfi, C.; Fisichella, P.M. Epidemiology of Obesity and Associated Comorbidities. J. Laparoendosc. Adv. Surg. Tech. 2018, 28, 919–924. [Google Scholar] [CrossRef] [PubMed]
- Khaodhiar, L.; McCowen, K.C.; Blackburn, G.L. Obesity and its comorbid conditions. Clin. Cornerstone 1999, 2, 17–31. [Google Scholar] [CrossRef] [PubMed]
- Obesity and Total Joint Arthroplasty. J. Arthroplast. 2013, 28, 714–721. [CrossRef]
- Runhaar, J.; Koes, B.W.; Clockaerts, S.; Bierma-Zeinstra, S.M.A. A systematic review on changed biomechanics of lower extremities in obese individuals: A possible role in development of osteoarthritis. Obes. Rev. 2011, 12, 1071–1082. [Google Scholar] [CrossRef] [PubMed]
- de Guia, N.; Zhu, N.; Keresteci, M.; Shi, J.E. Obesity and joint replacement surgery in Canada: Findings from the Canadian Joint Replacement Registry (CJRR). Healthc. PolicyPolit. De Sante 2006, 1, 36–43. [Google Scholar] [CrossRef]
- DeMik, D.E.; Bedard, N.A.; Dowdle, S.B.; Elkins, J.M.; Brown, T.S.; Gao, Y.; Callaghan, J.J. Complications and Obesity in Arthroplasty—A Hip is Not a Knee. J. Arthroplast. 2018, 33, 3281–3287. [Google Scholar] [CrossRef]
- Petis, S.; Howard, J.L.; Lanting, B.L.; Vasarhelyi, E.M. Surgical approach in primary total hip arthroplasty: Anatomy, technique and clinical outcomes. Can. J. Surg. 2015, 58, 128–139. [Google Scholar] [CrossRef] [PubMed]
- Pincus, D.; Jenkinson, R.; Paterson, M.; Leroux, T.; Ravi, B. Association Between Surgical Approach and Major Surgical Complications in Patients Undergoing Total Hip Arthroplasty. JAMA 2020, 323, 1070–1076. [Google Scholar] [CrossRef]
- Post, Z.D.; Orozco, F.; Diaz-Ledezma, C.; Hozack, W.J.; Ong, A. Direct anterior approach for total hip arthroplasty: Indications, technique, and results. J. Am. Acad. Orthop. Surg. 2014, 22, 595–603. [Google Scholar] [CrossRef] [PubMed]
- Faldini, C.; Perna, F.; Mazzotti, A.; Stefanini, N.; Panciera, A.; Geraci, G.; Mora, P.; Traina, F. Direct anterior approach versus posterolateral approach in total hip arthroplasty: Effects on early post-operative rehabilitation period. J. Biol. Regul. Homeost. Agents 2017, 31, 75–81. [Google Scholar]
- Faldini, C.; Perna, F.; Pilla, F.; Stefanini, N.; Pungetti, C.; Persiani, V.; Traina, F. Is a minimally invasive anterior approach effective in old patients? A pilot study. J. Biol. Regul. Homeost. Agents 2016, 30, 193–199. [Google Scholar] [PubMed]
- Russo, M.W.; Macdonell, J.R.; Paulus, M.C.; Keller, J.M.; Zawadsky, M.W. Increased Complications in Obese Patients Undergoing Direct Anterior Total Hip Arthroplasty. J. Arthroplast. 2015, 30, 1384–1387. [Google Scholar] [CrossRef] [PubMed]
- Shah, N.V.; Huddleston, H.P.; Wolff, D.T.; Newman, J.M.; Pivec, R.; Naziri, Q.; Shah, V.R.; Maheshwari, A.V. Does Surgical Approach for Total Hip Arthroplasty Impact Infection Risk in the Obese Patient? A Systematic Review. Orthopedics 2022, 45, e67–e72. [Google Scholar] [CrossRef]
- Watts, C.; Houdek, M.T.; Wagner, E.R.; Sculco, P.; Chalmers, B.P.; Taunton, M. High Risk of Wound Complications Following Direct Anterior Total Hip Arthroplasty in Obese Patients. J. Arthroplast. 2015, 30, 2296–2298. [Google Scholar] [CrossRef] [PubMed]
- Rhind, J.-H.; Baker, C.; Roberts, P.J. Total Hip Arthroplasty in the Obese Patient: Tips and Tricks and Review of the Literature. Indian J. Orthop. 2020, 54, 776–783. [Google Scholar] [CrossRef] [PubMed]
- Nizam, I.; Dabirrahmani, D.; Alva, A.; Choudary, D. Bikini anterior hip replacements in obese patients are not associated with an increased risk of complication. Arch. Orthop. Trauma Surg. 2021, 142, 2919–2926. [Google Scholar] [CrossRef]
- Argyrou, C.; Tzefronis, D.; Sarantis, M.; Kateros, K.; Poultsides, L.; Macheras, G.A. Total hip arthroplasty through the direct anterior approach in morbidly obese patients. Bone Jt. Open 2022, 3, 4–11. [Google Scholar] [CrossRef]
- Macheras, G.; Stasi, S.; Sarantis, M.; Triantafyllou, A.; Tzefronis, D.; A Papadakis, S. Direct anterior approach vs Hardinge in obese and nonobese osteoarthritic patients: A randomized controlled trial. World J. Orthop. 2021, 12, 877–890. [Google Scholar] [CrossRef] [PubMed]
- Johnston, F.E.; Wadden, T.A.; Stunkard, A.J.; Peña, M.; Wang, J.; Pierson, R.N.; Van Itallie, T.B. Body fat deposition in adult obese women. I Patterns of fat distribution. Am. J. Clin. Nutr. 1988, 47, 225–228. [Google Scholar] [CrossRef]
- Lewinnek, G.E.; Lewis, J.L.; Tarr, R.; Compere, C.L.; Zimmerman, J.R. Dislocations after total hip-replacement arthroplasties. J. Bone Joint. Surg. Am. 1978, 60, 217–220. [Google Scholar] [CrossRef]
- Khalily, C.; Lester, D. Results of a tapered cementless femoral stem implanted in varus. J. Arthroplast. 2002, 17, 463–466. [Google Scholar] [CrossRef]
- Haynes, J.; Nam, D.; Barrack, R.L. Obesity in total hip arthroplasty: Does it make a difference? Bone Jt. J. 2017, 99, 31–36. [Google Scholar] [CrossRef]
- Clement, N.D.; Deehan, D.J. Overweight and Obese Patients Require Total Hip and Total Knee Arthroplasty at a Younger Age. J. Orthop. Res. 2019, 38, 348–355. [Google Scholar] [CrossRef] [PubMed]
- Gurunathan, U.; Anderson, C.; Berry, K.E.; Whitehouse, S.L.; Crawford, R.W. Body mass index and in-hospital postoperative complications following primary total hip arthroplasty. HIP Int. 2018, 28, 613–621. [Google Scholar] [CrossRef] [PubMed]
- Antoniadis, A.; Dimitriou, D.; Flury, A.; Wiedmer, G.; Hasler, J.; Helmy, N. Is Direct Anterior Approach a Credible Option for Severely Obese Patients Undergoing Total Hip Arthroplasty? A Matched-Control, Retrospective, Clinical Study. J. Arthroplast. 2018, 33, 2535–2540. [Google Scholar] [CrossRef]
- Sang, W.; Zhu, L.; Ma, J.; Lu, H.; Wang, C. The Influence of Body Mass Index and Hip Anatomy on Direct Anterior Approach Total Hip Replacement. Med. Princ. Pract. Int. J. Kuwait. Univ. Health Sci. Cent. 2016, 25, 555–560. [Google Scholar] [CrossRef] [PubMed]
- Hartford, J.M.; Graw, B.P.; Frosch, D.L. Perioperative Complications Stratified by Body Mass Index for the Direct Anterior Approach to Total Hip Arthroplasty. J. Arthroplast. 2020, 35, 2652–2657. [Google Scholar] [CrossRef]
- Purcell, R.L.; Parks, N.L.; Gargiulo, J.M.; Hamilton, W.G. Severely Obese Patients Have a Higher Risk of Infection After Direct Anterior Approach Total Hip Arthroplasty. J. Arthroplast. 2016, 31, 162–165. [Google Scholar] [CrossRef]
- Luger, M.; Hipmair, G.; Schopper, C.; Schauer, B.; Hochgatterer, R.; Allerstorfer, J.; Gotterbarm, T.; Klasan, A. Low rate of early periprosthetic fractures in cementless short-stem total hip arthroplasty using a minimally invasive anterolateral approach. J. Orthop. Traumatol. 2021, 22, 1–9. [Google Scholar] [CrossRef]
- Alva, A.; Nizam, I.; Gogos, S. Minimizing complications in bikini incision direct anterior approach total hip arthroplasty: A single surgeon series of 865 cases. J. Exp. Orthop. 2021, 8, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Sprowls, G.R.; Allen, B.C.; Lundquist, K.F.; Sager, L.N.; Barnett, C.D. Incision site fat thickness and 90-day complications for direct anterior and posterior approach total hip arthroplasty. HIP Int. 2020, 32, 431–437. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, V.K.; Elbuluk, A.; Dundon, J.; Herrero, C.; Hernandez, C.; Vigdorchik, J.M.; Schwarzkopf, R.; Iorio, R.; Long, W.J. Surgical approach significantly affects the complication rates associated with total hip arthroplasty. Bone Jt. J. 2019, 101, 646–651. [Google Scholar] [CrossRef]
- Griffiths, S.Z.; Post, Z.D.; Buxbaum, E.J.; Paziuk, T.M.; Orozco, F.R.; Ong, A.C.; Ponzio, D.Y. Predictors of Perioperative Vancouver B Periprosthetic Femoral Fractures Associated With the Direct Anterior Approach to Total Hip Arthroplasty. J. Arthroplast. 2019, 35, 1407–1411. [Google Scholar] [CrossRef] [PubMed]
- Stringer, M.R.; Hooper, G.J.; Frampton, C.; Kieser, D.C.; Deng, Y. Periprosthetic fractures of the femur in primary total hip arthroplasty: A New Zealand Joint Registry analysis. ANZ J. Surg. 2021, 91, 404–408. [Google Scholar] [CrossRef]
- Sadhu, A.; Nam, D.; Coobs, B.R.; Barrack, T.N.; Nunley, R.M.; Barrack, R.L. Acetabular Component Position and the Risk of Dislocation Following Primary and Revision Total Hip Arthroplasty: A Matched Cohort Analysis. J. Arthroplast. 2017, 32, 987–991. [Google Scholar] [CrossRef]
- Davidovitch, R.; Riesgo, A.; Bolz, N.; Murphy, H.; Anoushiravani, A.A.; Snir, N. The Effect of Obesity on Fluoroscopy-Assisted Direct Anterior Approach Total Hip Arthroplasty. Bull. NYU Hosp. Jt. Dis. 2020, 78, 187–194. [Google Scholar]
- Haversath, M.; Lichetzki, M.; Serong, S.; Busch, A.; Landgraeber, S.; Jäger, M.; Tassemeier, T. The direct anterior approach provokes varus stem alignment when using a collarless straight tapered stem. Arch. Orthop. Trauma Surg. 2020, 141, 891–897. [Google Scholar] [CrossRef]
- Gillinov, S.M.; Joo, P.Y.; Zhu, J.R.; Moran, J.; Rubin, L.E.; Grauer, J.N. Incidence, Timing, and Predictors of Hip Dislocation After Primary Total Hip Arthroplasty for Osteoarthritis. J. Am. Acad. Orthop. Surg. 2022, 30, 1047–1053. [Google Scholar] [CrossRef]
- Manrique, J.; Paskey, T.; Tarabichi, M.; Restrepo, C.; Foltz, C.; Hozack, W.J. Total Hip Arthroplasty Through the Direct Anterior Approach Using a Bikini Incision Can Be Safely Performed in Obese Patients. J. Arthroplast. 2019, 34, 1723–1730. [Google Scholar] [CrossRef] [PubMed]
- Dienstknecht, T.; Lüring, C.; Tingart, M.; Grifka, J.; Sendtner, E. A minimally invasive approach for total hip arthroplasty does not diminish early post-operative outcome in obese patients: A prospective, randomised trial. Int. Orthop. 2013, 37, 1013–1018. [Google Scholar] [CrossRef] [PubMed]
| Patients Characteristics | NW (n = 96) | OW (n = 115) | OB (n = 82) |
|---|---|---|---|
| Age (Years) | 63.3 (34–86 years) | 63.9 (34–86 years) | 58.6 (36–83 years) |
| Sex (M/F) | 43% M/57% F (41 M 55 F) | 60% M/40% F (69 M 46 F) | 56% M/44% F (46 M 36 F) |
| ASA I | 39% (37) | 23% (26) | 16% (13) |
| ASA II | 47% (45) | 62% (71) | 63% (52) |
| ASA III | 14% (14) | 15% (18) | 21% (17) |
| Complications | NW | OW | OB | Total |
|---|---|---|---|---|
| Wound dehiscence | - | - | 1/82 (1.22%) | 1/293 (0.34%) |
| Intra-operative femur fracture | 1/96 (1.04%) | 1/115 (0.87%) | - | 2/293 (0.68%) |
| Dislocation | - | - | 2/82 (2.43%) | 2/293 (0.68%) |
| Aseptic loosening | 1/96 (1.04%) | - | 1/82 (1.22%) | 2/293 (0.68%) |
| Total | 2/96 (2.08%) | 1/115 (0.87%) | 4/82 (4.87%) | 7/293 (2.3%) |
| NW | OW | OB | ||
|---|---|---|---|---|
| NRS at 2nd post-operative day | 1.2 ± 1.0 | 1.3 ± 1.1 | 1.5 ± 1.0 | p = 0.346 |
| Day of post-operative stair climbing | 3.4 ± 1.7 | 3.5 ± 1.9 | 3.7 ± 1.7 | p = 0.456 |
| NW | OW | OB | Total | |
|---|---|---|---|---|
| Within Lewinnek’s safe zone | 74 (77.1%) | 86 (74.8%) | 62 (75.6%) | 222 (75.8%) |
| Out of Lewinnek’s safe zone | 22 (22.9%) | 29 (25.2%) | 20 (24.4%) | 71 (24.2%) |
| Total | 96 | 115 | 82 | 293 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Martino, A.; Stefanini, N.; Brunello, M.; Bordini, B.; Pilla, F.; Geraci, G.; D’Agostino, C.; Ruta, F.; Faldini, C. Is the Direct Anterior Approach for Total Hip Arthroplasty Effective in Obese Patients? Early Clinical and Radiographic Results from a Retrospective Comparative Study. Medicina 2023, 59, 769. https://doi.org/10.3390/medicina59040769
Di Martino A, Stefanini N, Brunello M, Bordini B, Pilla F, Geraci G, D’Agostino C, Ruta F, Faldini C. Is the Direct Anterior Approach for Total Hip Arthroplasty Effective in Obese Patients? Early Clinical and Radiographic Results from a Retrospective Comparative Study. Medicina. 2023; 59(4):769. https://doi.org/10.3390/medicina59040769
Chicago/Turabian StyleDi Martino, Alberto, Niccolò Stefanini, Matteo Brunello, Barbara Bordini, Federico Pilla, Giuseppe Geraci, Claudio D’Agostino, Federico Ruta, and Cesare Faldini. 2023. "Is the Direct Anterior Approach for Total Hip Arthroplasty Effective in Obese Patients? Early Clinical and Radiographic Results from a Retrospective Comparative Study" Medicina 59, no. 4: 769. https://doi.org/10.3390/medicina59040769
APA StyleDi Martino, A., Stefanini, N., Brunello, M., Bordini, B., Pilla, F., Geraci, G., D’Agostino, C., Ruta, F., & Faldini, C. (2023). Is the Direct Anterior Approach for Total Hip Arthroplasty Effective in Obese Patients? Early Clinical and Radiographic Results from a Retrospective Comparative Study. Medicina, 59(4), 769. https://doi.org/10.3390/medicina59040769









