Correlations of Sesamoid Bone Subluxation with the Radiologic Measures of Hallux Valgus and Its Clinical Implications
Abstract
1. Introduction
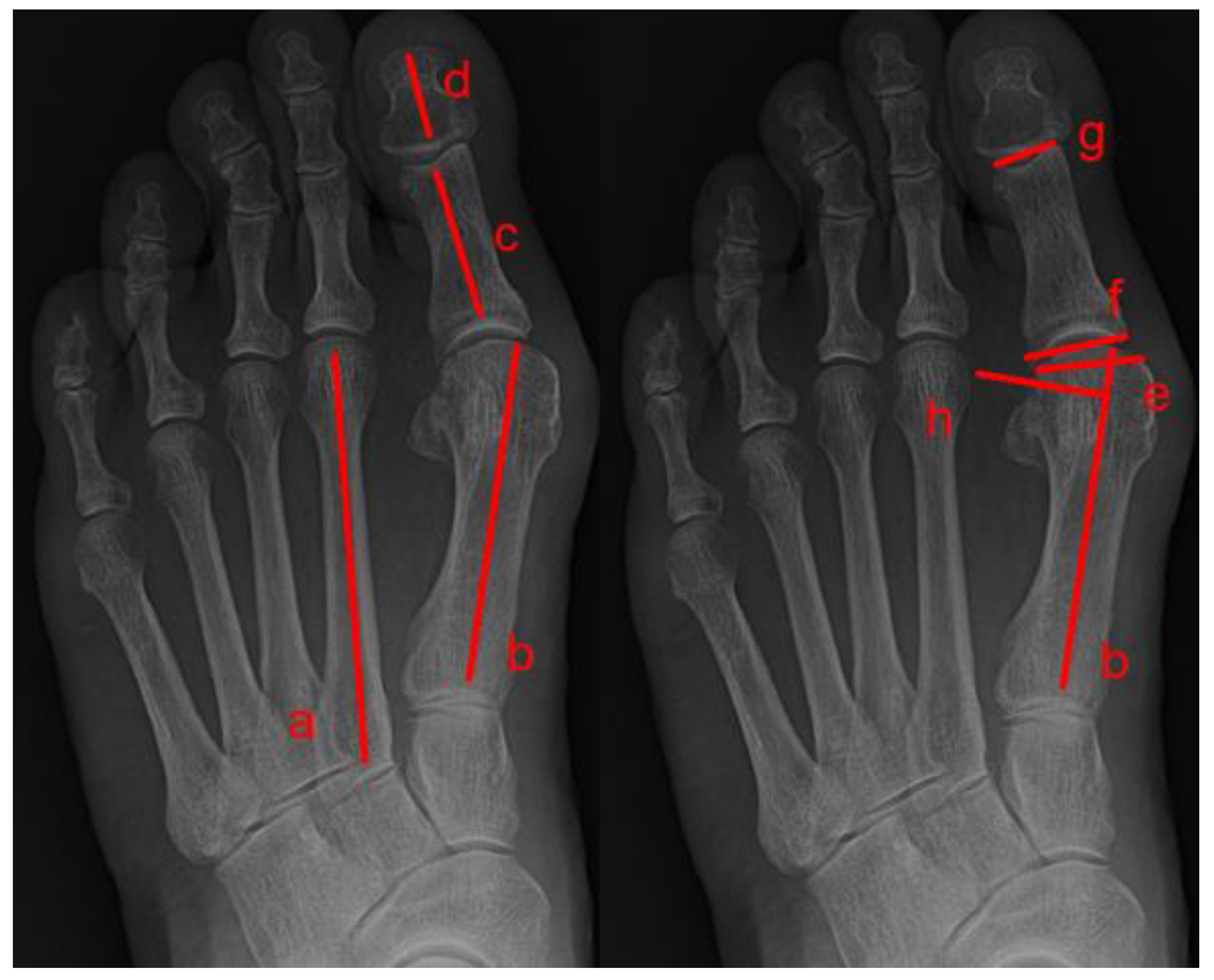
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nix, S.; Smith, M.; Vicenzino, B. Prevalence of hallux valgus in the general population: A systematic review and meta-analysis. J. Foot Ankle Res. 2010, 3, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, K.; Metikala, S.; Mehta, S.D.; Fryhofer, G.W.; Farber, D.C.; Prat, D. The role of weightbearing computed tomography scan in hallux valgus. Foot Ankle Int. 2021, 42, 287–293. [Google Scholar] [CrossRef] [PubMed]
- Campbell, J.T. Hallux valgus: Adult and juvenile. In Orthopaedic Knowledge Update: Foot and Ankle; American Academy of Orthopaedic Surgeons: Rosemont, IL, USA, 2004. [Google Scholar]
- Biz, C.; Maso, G.; Malgarini, E.; Tagliapietra, J.; Ruggieri, P. Hypermobility of the First Ray: The Cinderella of the measurements conventionally assessed for correction of Hallux Valgus. Acta Bio Med. Atenei Parm. 2020, 91, 47. [Google Scholar]
- Zhong, Z.; Zhang, P.; Duan, H.; Yang, H.; Li, Q.; He, F. A Comparison between x-ray imaging and an innovative computer-aided design method based on weightbearing CT scan images for assessing hallux valgus. J. Foot Ankle Surg. 2021, 60, 6–10. [Google Scholar] [CrossRef] [PubMed]
- Grande-del-Arco, J.; Becerro-de-Bengoa-Vallejo, R.; Palomo-López, P.; López-López, D.; Calvo-Lobo, C.; Pérez-Boal, E.; Losa-Iglesias, M.E.; Martin-Villa, C.; Rodriguez-Sanz, D. Radiographic analysis on the distortion of the anatomy of first metatarsal head in dorsoplantar projection. Diagnostics 2020, 10, 552. [Google Scholar] [CrossRef] [PubMed]
- Coughlin, M.J.; Mann, R.A.; Saltzman, C.L. Surgery of the foot and ankle. Rev. Rev. 2007, 26, 1. [Google Scholar]
- Steinberg, N.; Finestone, A.; Noff, M.; Zeev, A.; Dar, G. Relationship between lower extremity alignment and hallux valgus in women. Foot Ankle Int. 2013, 34, 824–831. [Google Scholar] [CrossRef] [PubMed]
- Yavuz, M.; Hetherington, V.J.; Botek, G.; Hirschman, G.B.; Bardsley, L.; Davis, B.L. Forefoot plantar shear stress distribution in hallux valgus patients. Gait Posture 2009, 30, 257–259. [Google Scholar] [CrossRef]
- Zhang, Y.; Awrejcewicz, J.; Szymanowska, O.; Shen, S.; Zhao, X.; Baker, J.S.; Gu, Y. Effects of severe hallux valgus on metatarsal stress and the metatarsophalangeal loading during balanced standing: A finite element analysis. Comput. Biol. Med. 2018, 97, 1–7. [Google Scholar] [CrossRef]
- Wülker, N.; Mittag, F. The treatment of hallux valgus. Dtsch. Ärztebl. Int. 2012, 109, 857. [Google Scholar] [CrossRef]
- Malagelada, F.; Sahirad, C.; Dalmau-Pastor, M.; Vega, J.; Bhumbra, R.; Manzanares-Céspedes, M.C.; Laffenêtre, O. Minimally invasive surgery for hallux valgus: A systematic review of current surgical techniques. Int. Orthop. 2019, 43, 625–637. [Google Scholar] [CrossRef] [PubMed]
- Chopra, S.; Moerenhout, K.; Crevoisier, X. Subjective versus objective assessment in early clinical outcome of modified Lapidus procedure for hallux valgus deformity. Clin. Biomech. 2016, 32, 187–193. [Google Scholar] [CrossRef] [PubMed]
- Biz, C.; Fosser, M.; Dalmau-Pastor, M.; Corradin, M.; Rodà, M.G.; Aldegheri, R.; Ruggieri, P. Functional and radiographic outcomes of hallux valgus correction by mini-invasive surgery with Reverdin-Isham and Akin percutaneous osteotomies: A longitudinal prospective study with a 48-month follow-up. J. Orthop. Surg. Res. 2016, 11, 157. [Google Scholar] [CrossRef] [PubMed]
- Kaufmann, G.; Dammerer, D.; Heyenbrock, F.; Braito, M.; Moertlbauer, L.; Liebensteiner, M. Minimally invasive versus open chevron osteotomy for hallux valgus correction: A randomized controlled trial. Int. Orthop. 2019, 43, 343–350. [Google Scholar] [CrossRef]
- Doty, J.F.; Alvarez, R.G.; Ervin, T.B.; Heard, A.; Gilbreath, J.; Richardson, N.S. Biomechanical evaluation of custom foot orthoses for hallux valgus deformity. J. Foot Ankle Surg. 2015, 54, 852–855. [Google Scholar] [CrossRef]
- Farzadi, M.; Safaeepour, Z.; Mousavi, M.E.; Saeedi, H. Effect of medial arch support foot orthosis on plantar pressure distribution in females with mild-to-moderate hallux valgus after one month of follow-up. Prosthet. Orthot. Int. 2015, 39, 134–139. [Google Scholar] [CrossRef]
- Lee, S.-M.; Lee, J.-H. Effects of balance taping using kinesiology tape in a patient with moderate hallux valgus: A case report. Medicine 2016, 95, e5357. [Google Scholar] [CrossRef]
- Karabicak, G.O.; Bek, N.; Tiftikci, U. Short-term effects of kinesiotaping on pain and joint alignment in conservative treatment of hallux valgus. J. Manip. Physiol. Ther. 2015, 38, 564–571. [Google Scholar] [CrossRef]
- Holowka, N.B.; Wallace, I.J.; Lieberman, D.E. Foot strength and stiffness are related to footwear use in a comparison of minimally-vs. conventionally-shod populations. Sci. Rep. 2018, 8, 3679. [Google Scholar] [CrossRef]
- Chhaya, S.A.; Brawner, M.; Hobbs, P.; Chhaya, N.; Garcia, G.; Loredo, R. Understanding hallux valgus deformity: What the surgeon wants to know from the conventional radiograph. Curr. Probl. Diagn. Radiol. 2008, 37, 127–137. [Google Scholar] [CrossRef]
- Lee, K.M.; Ahn, S.; Chung, C.Y.; Sung, K.H.; Park, M.S. Reliability and relationship of radiographic measurements in hallux valgus. Clin. Orthop. Relat. Res. 2012, 470, 2613–2621. [Google Scholar] [CrossRef] [PubMed]
- Perera, A.; Mason, L.; Stephens, M. The pathogenesis of hallux valgus. J. Bone Jt. Surg. 2011, 93, 1650–1661. [Google Scholar] [CrossRef] [PubMed]
- Shi, G.G.; Whalen, J.L.; Turner, N.S., III; Kitaoka, H.B. Operative approach to adult hallux valgus deformity: Principles and techniques. JAAOS J. Am. Acad. Orthop. Surg. 2020, 28, 410–418. [Google Scholar] [CrossRef]
- Okuda, R.; Kinoshita, M.; Yasuda, T.; Jotoku, T.; Shima, H.; Takamura, M. Hallux valgus angle as a predictor of recurrence following proximal metatarsal osteotomy. J. Orthop. Sci. 2011, 16, 760–764. [Google Scholar] [CrossRef]
- Agrawal, Y.; Desai, A.; Mehta, J. Lateral sesamoid position in hallux valgus: Correlation with the conventional radiological assessment. Foot Ankle Surg. 2011, 17, 308–311. [Google Scholar] [CrossRef]
- Katsui, R.; Samoto, N.; Taniguchi, A.; Akahane, M.; Isomoto, S.; Sugimoto, K.; Tanaka, Y. Relationship between displacement and degenerative changes of the sesamoids in hallux valgus. Foot Ankle Int. 2016, 37, 1303–1309. [Google Scholar] [CrossRef]
- Okuda, R.; Kinoshita, M.; Yasuda, T.; Jotoku, T.; Kitano, N.; Shima, H. Postoperative incomplete reduction of the sesamoids as a risk factor for recurrence of hallux valgus. J. Bone Jt. Surg. 2009, 91, 1637–1645. [Google Scholar] [CrossRef] [PubMed]
- De Cesar Netto, C.; Saito, G.H.; Roney, A.; Day, J.; Greditzer, H.; Sofka, C.; Ellis, S.J.; Weight Bearing CT Society; Richter, M.; Barg, A.; et al. Combined weightbearing CT and MRI assessment of flexible progressive collapsing foot deformity. Foot Ankle Surg. 2021, 27, 884–891. [Google Scholar] [CrossRef]
- Netto, C.d.C.; Li, S.; Vivtcharenko, V.; Auch, E.; Lintz, F.; Ellis, S.J.; Femino, J.E.; de Cesar Netto, C. Three-Dimensional Distance and Coverage Maps in the Assessment of Peritalar Subluxation in Progressive Collapsing Foot Deformity. Foot Ankle Orthop. 2022, 7, 2473011421S00177. [Google Scholar] [CrossRef]
- Bakshi, N.; Steadman, J.; Philippi, M.; Arena, C.; Leake, R.; Saltzman, C.L.; Barg, A. Association between hindfoot alignment and first metatarsal rotation. Foot Ankle Int. 2022, 43, 105–112. [Google Scholar] [CrossRef]
- Collan, L.; Kankare, J.A.; Mattila, K. The biomechanics of the first metatarsal bone in hallux valgus: A preliminary study utilizing a weight bearing extremity CT. Foot Ankle Surg. 2013, 19, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Bryant, A.; Tinley, P.; Singer, K. A comparison of radiographic measurements in normal, hallux valgus, and hallux limitus feet. J. Foot Ankle Surg. 2000, 39, 39–43. [Google Scholar] [CrossRef]
- D’Arcangelo, P.R.; Landorf, K.B.; Munteanu, S.E.; Zammit, G.V.; Menz, H.B. Radiographic correlates of hallux valgus severity in older people. J. Foot Ankle Res. 2011, 4, 1. [Google Scholar] [CrossRef]
- Menz, H.B.; Munteanu, S.E. Radiographic validation of the Manchester scale for the classification of hallux valgus deformity. Rheumatology 2005, 44, 1061–1066. [Google Scholar] [CrossRef] [PubMed]
- Koo, T.K.; Li, M.Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef]
- Srivastava, S.; Chockalingam, N.; El Fakhri, T. Radiographic angles in hallux valgus: Comparison between manual and computer-assisted measurements. J. Foot Ankle Surg. 2010, 49, 523–528. [Google Scholar] [CrossRef]
- Biz, C.; Crimì, A.; Fantoni, I.; Tagliapietra, J.; Ruggieri, P. Functional and radiographic outcomes of minimally invasive intramedullary nail device (MIIND) for moderate to severe hallux valgus. Foot Ankle Int. 2021, 42, 409–424. [Google Scholar] [CrossRef]
- Xiang, L.; Mei, Q.; Wang, A.; Shim, V.; Fernandez, J.; Gu, Y. Evaluating function in the hallux valgus foot following a 12-week minimalist footwear intervention: A pilot computational analysis. J. Biomech. 2022, 132, 110941. [Google Scholar] [CrossRef]
- Janssen, D.M.; Sanders, A.P.; Guldemond, N.A.; Hermus, J.; Walenkamp, G.H.; Van Rhijn, L.W. A comparison of hallux valgus angles assessed with computerised plantar pressure measurements, clinical examination and radiography in patients with diabetes. J. Foot Ankle Res. 2014, 7, 1–9. [Google Scholar] [CrossRef]
- Cullen, N.; Robinson, A.; Chayya, N.; Kes, J. Variation of the distal metatarsal articular angle with axial rotation of the first metatarsal. In Orthopaedic Proceedings; The British Editorial Society of Bone & Joint Surgery: London, UK, 2008; p. 228. [Google Scholar]
- Chi, T.D.; Davitt, J.; Younger, A.; Holt, S.; Sangeorzan, B.J. Intra-and inter-observer reliability of the distal metatarsal articular angle in adult hallux valgus. Foot Ankle Int. 2002, 23, 722–726. [Google Scholar] [CrossRef] [PubMed]
- Talbot, K.D.; Saltzman, C.L. Assessing sesamoid subluxation: How good is the AP radiograph? Foot Ankle Int. 1998, 19, 547–554. [Google Scholar] [CrossRef] [PubMed]
- Mann, R.A.; Coughlin, M.J. Hallux valgus—Etiology, anatomy, treatment and surgical considerations. Clin. Orthop. Relat. Res. 1981, 157, 31–41. [Google Scholar] [CrossRef]
- Silver, D. The operative treatment of hallux valgus. J. Bone Jt. Surg. 1923, 5, 225–232. [Google Scholar]
- Saragas, N.P.; Becker, P.J. Comparative radiographic analysis of parameters in feet with and without hallux valgus. Foot Ankle Int. 1995, 16, 139–143. [Google Scholar] [CrossRef]
- Hardy, R.; Clapham, J. Observations on hallux valgus. J. Bone Jt. Surg. Br. Vol. 1951, 33, 376–391. [Google Scholar] [CrossRef] [PubMed]
- Kuwano, T.; Nagamine, R.; Sakaki, K.; Urabe, K.; Iwamoto, Y. New radiographic analysis of sesamoid rotation in hallux valgus: Comparison with conventional evaluation methods. Foot Ankle Int. 2002, 23, 811–817. [Google Scholar] [CrossRef]
- Yildirim, Y.; Cabukoglu, C.; Erol, B.; Esemenli, T. Effect of metatarsophalangeal joint position on the reliability of the tangential sesamoid view in determining sesamoid position. Foot Ankle Int. 2005, 26, 247–250. [Google Scholar] [CrossRef]
- Lee, K.; Cho, N.; Park, H.; Seon, J.; Lee, S. A comparison of proximal and distal Chevron osteotomy, both with lateral soft-tissue release, for moderate to severe hallux valgus in patients undergoing simultaneous bilateral correction: A prospective randomised controlled trial. Bone Jt. J. 2015, 97, 202–207. [Google Scholar] [CrossRef]


| Total | 205 |
|---|---|
| Excluded patients | 25 |
| Patient number | 180 |
| Age | 52.78 |
| Male:Female | 18:162 |
| Operated feet | 240 |
| Operated sided Right:Left:Bilateral | 54:66:60 |
| Grade | |
|---|---|
| 0 | No sesamoid lateral displacement |
| 1 | Sesamoid overlap < 25% |
| 2 | 25% < Sesamoid overlap < 50% |
| 3 | 50% < Sesamoid overlap < 75% |
| 4 | 75% < Sesamoid overlap |
| Observer1 | Observer2 | Observer3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| CCC | 95% CI | CCC | 95% CI | CCC | 95% CI | ||||
| R HVA | 0.890 | (0.844 | 0.923) | 0.989 | (0.984 | 0.992) | 0.649 | (0.530 | 0.743) |
| R IMA | 0.810 | (0.736 | 0.865) | 0.909 | (0.872 | 0.936) | 0.756 | (0.669 | 0.823) |
| R DMAA | 0.650 | (0.535 | 0.741) | 0.842 | (0.779 | 0.888) | 0.306 | (0.135 | 0.460) |
| R T-MA | 0.875 | (0.824 | 0.913) | 0.974 | (0.962 | 0.982) | 0.541 | (0.411 | 0.650) |
| R Ppa | 0.734 | (0.637 | 0.808) | 0.922 | (0.889 | 0.945) | 0.396 | (0.238 | 0.533) |
| R HIA | 0.804 | (0.731 | 0.859) | 0.924 | (0.892 | 0.947) | 0.734 | (0.638 | 0.807) |
| L HVA | 0.964 | (0.950 | 0.975) | 0.986 | (0.981 | 0.990) | 0.945 | (0.922 | 0.961) |
| L IMA | 0.154 | (0.052 | 0.253) | 0.950 | (0.930 | 0.964) | 0.704 | (0.605 | 0.782) |
| L DMAA | 0.611 | (0.494 | 0.706) | 0.860 | (0.806 | 0.899) | 0.335 | (0.177 | 0.476) |
| L T-Ma | 0.864 | (0.813 | 0.902) | 0.979 | (0.970 | 0.985) | 0.554 | (0.435 | 0.653) |
| L Ppa | 0.827 | (0.764 | 0.874) | 0.908 | (0.873 | 0.935) | 0.395 | (0.266 | 0.510) |
| L HIA | 0.754 | (0.671 | 0.819) | 0.932 | (0.904 | 0.951) | 0.503 | (0.361 | 0.623) |
| CCC: Concordance correlation coefficient | |||||||||
| Observer1 | Observer2 | Observer3 | |||||||
| Weighted Kappa | 95% CI | Weighted Kappa | 95% CI | Weighted Kappa | 95% CI | ||||
| R Sesa | 0.647 | (0.515 | 0.778) | 0.924 | (0.874 | 0.974) | 1.000 | (1.000 | 1.000) |
| L Sesa | 0.692 | (0.583 | 0.800) | 0.966 | (0.932 | 1.000) | 0.994 | (0.982 | 1.000) |
| Observer1 | Observer2 | Observer3 | |||||||
| Kappa | 95% CI | Kappa | 95% CI | Kappa | 95% CI | ||||
| R Cong | 0.581 | (0.378 | 0.784) | 0.936 | (0.864 | 1.000) | 0.939 | (0.856 | 1.000) |
| L Cong | 0.468 | (0.285 | 0.651) | 0.937 | (0.866 | 1.000) | 1.000 | (1.000 | 1.000) |
| First | Second | |||||
|---|---|---|---|---|---|---|
| CCC | 95% CI | CCC | 95% CI | |||
| R HVA | 0.747 | (0.591 | 0.843) | 0.867 | (0.810 | 0.907) |
| R IMA | 0.377 | (0.271 | 0.481) | 0.407 | (0.318 | 0.507) |
| R DMAA | 0.285 | (0.183 | 0.411) | 0.189 | (0.099 | 0.320) |
| R T-MA | 0.640 | (0.552 | 0.718) | 0.611 | (0.528 | 0.690) |
| R Ppa | 0.531 | (0.393 | 0.634) | 0.644 | (0.521 | 0.727) |
| R HIA | 0.656 | (0.551 | 0.774) | 0.773 | (0.692 | 0.843) |
| L HVA | 0.861 | (0.785 | 0.898) | 0.866 | (0.802 | 0.903) |
| L IMA | 0.131 | (0.020 | 0.542) | 0.539 | (0.424 | 0.623) |
| L DMAA | 0.322 | (0.237 | 0.424) | 0.206 | (0.101 | 0.320) |
| L T-Ma | 0.667 | (0.588 | 0.740) | 0.575 | (0.485 | 0.663) |
| L Ppa | 0.489 | (0.369 | 0.660) | 0.752 | (0.664 | 0.853) |
| L HIA | 0.591 | (0.500 | 0.674) | 0.675 | (0.599 | 0.753) |
| CCC: Concordance correlation coefficient | ||||||
| first | second | |||||
| Kendall’s Coefficient | p-value | Kendall’s Coefficient | p-value | |||
| R Sesa | 0.890 | <0.0001 | 0.846 | <0.0001 | ||
| L Sesa | 0.817 | <0.0001 | 0.819 | <0.0001 | ||
| 1st | 2nd | |||||
| Kappa | 95% CI | Kappa | 95% CI | |||
| R Cong | 0.412 | (0.306 | 0.519) | 0.393 | (0.286 | 0.499) |
| L Cong | 0.501 | (0.400 | 0.602) | 0.483 | (0.382 | 0.584) |
| Sesamoid Subluxation | p-Value † | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | |||||||
| Patients, n | 1 | 5 | 18 | 19 | 70 | ||||||
| HVA | 16.40 | 20.40 | ±4.62 | 24.49 | ±6.37 | 23.36 | ±5.45 | 33.39 | ±9.40 | <0.0001 | |
| IMA | 4.40 | 10.22 | ±1.97 | 11.14 | ±2.24 | 11.24 | ±1.81 | 14.52 | ±2.61 | <0.0001 | |
| DMAA | 8.00 | 15.36 | ±9.78 | 11.90 | ±6.13 | 10.91 | ±5.13 | 12.81 | ±5.80 | 0.4906 | |
| T-MA | 5.90 | 5.92 | ±10.69 | 4.74 | ±4.81 | 0.90 | ±6.51 | 0.72 | ±6.96 | 0.1122 | |
| Ppa | 14.20 | 5.02 | ±3.53 | 7.56 | ±4.01 | 8.24 | ±4.29 | 6.80 | ±4.27 | 0.2065 | |
| HIA | 19.20 | 11.24 | ±4.90 | 10.83 | ±4.18 | 9.78 | ±3.46 | 7.19 | ±4.74 | 0.0009 | |
| Cong | <0.0001 | ||||||||||
| C | 1 | (100.0%) | 4 | (80.0%) | 4 | (22.2%) | 7 | (36.8%) | 5 | (7.1%) | |
| N | 0 | (0.0%) | 1 | (20.0%) | 14 | (77.8%) | 12 | (63.2%) | 65 | (92.9%) | |
| Sesamoid Subluxation | p-Value † | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | |||||||
| Patients, n | 1 | 5 | 18 | 20 | 70 | ||||||
| HVA | 15.30 | 15.44 | ±7.15 | 22.91 | ±6.86 | 23.07 | ±4.18 | 32.59 | ±8.94 | <0.0001 | |
| IMA | 5.60 | 9.14 | ±3.43 | 10.60 | ±1.92 | 11.04 | ±2.12 | 14.82 | ±2.53 | <0.0001 | |
| DMAA | 0.90 | 10.02 | ±7.11 | 8.83 | ±7.05 | 9.85 | ±4.91 | 11.42 | ±5.83 | 0.2089 | |
| T-MA | 16.80 | 5.08 | ±6.17 | 3.64 | ±7.11 | 1.41 | ±6.25 | 0.56 | ±7.29 | 0.0710 | |
| Ppa | 6.40 | 9.80 | ±3.40 | 7.16 | ±4.27 | 8.74 | ±3.97 | 6.85 | ±4.35 | 0.3061 | |
| HIA | 15.10 | 13.82 | ±4.99 | 11.24 | ±4.92 | 11.12 | ±3.01 | 8.48 | ±4.96 | 0.0107 | |
| Cong | <0.0001 | ||||||||||
| C | 1 | (100.0%) | 5 | (100.0%) | 10 | (55.6%) | 13 | (65.0%) | 5 | (7.1%) | |
| N | 0 | (0.0%) | 0 | (0.0%) | 8 | (44.4%) | 7 | (35.0%) | 65 | (92.9%) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.H.; Kim, Y.H.; Cha, J.Y.; Lee, Y.K. Correlations of Sesamoid Bone Subluxation with the Radiologic Measures of Hallux Valgus and Its Clinical Implications. Medicina 2023, 59, 876. https://doi.org/10.3390/medicina59050876
Kim SH, Kim YH, Cha JY, Lee YK. Correlations of Sesamoid Bone Subluxation with the Radiologic Measures of Hallux Valgus and Its Clinical Implications. Medicina. 2023; 59(5):876. https://doi.org/10.3390/medicina59050876
Chicago/Turabian StyleKim, Sung Hwan, Young Hwan Kim, Joo Young Cha, and Young Koo Lee. 2023. "Correlations of Sesamoid Bone Subluxation with the Radiologic Measures of Hallux Valgus and Its Clinical Implications" Medicina 59, no. 5: 876. https://doi.org/10.3390/medicina59050876
APA StyleKim, S. H., Kim, Y. H., Cha, J. Y., & Lee, Y. K. (2023). Correlations of Sesamoid Bone Subluxation with the Radiologic Measures of Hallux Valgus and Its Clinical Implications. Medicina, 59(5), 876. https://doi.org/10.3390/medicina59050876






