Unique Characteristics and Applications of Reverse Superior Labial Artery Island Flaps: A Case Series
Abstract
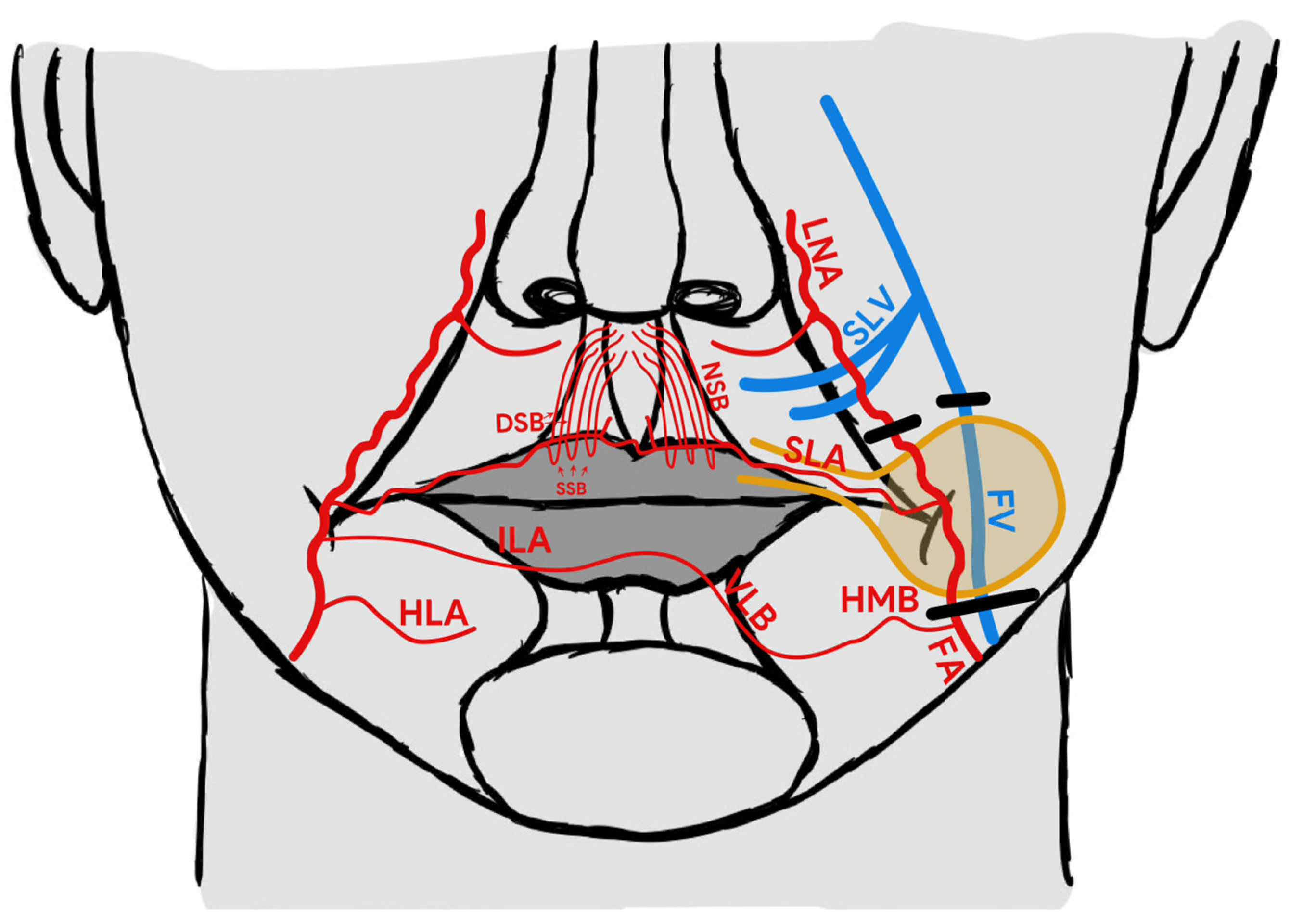
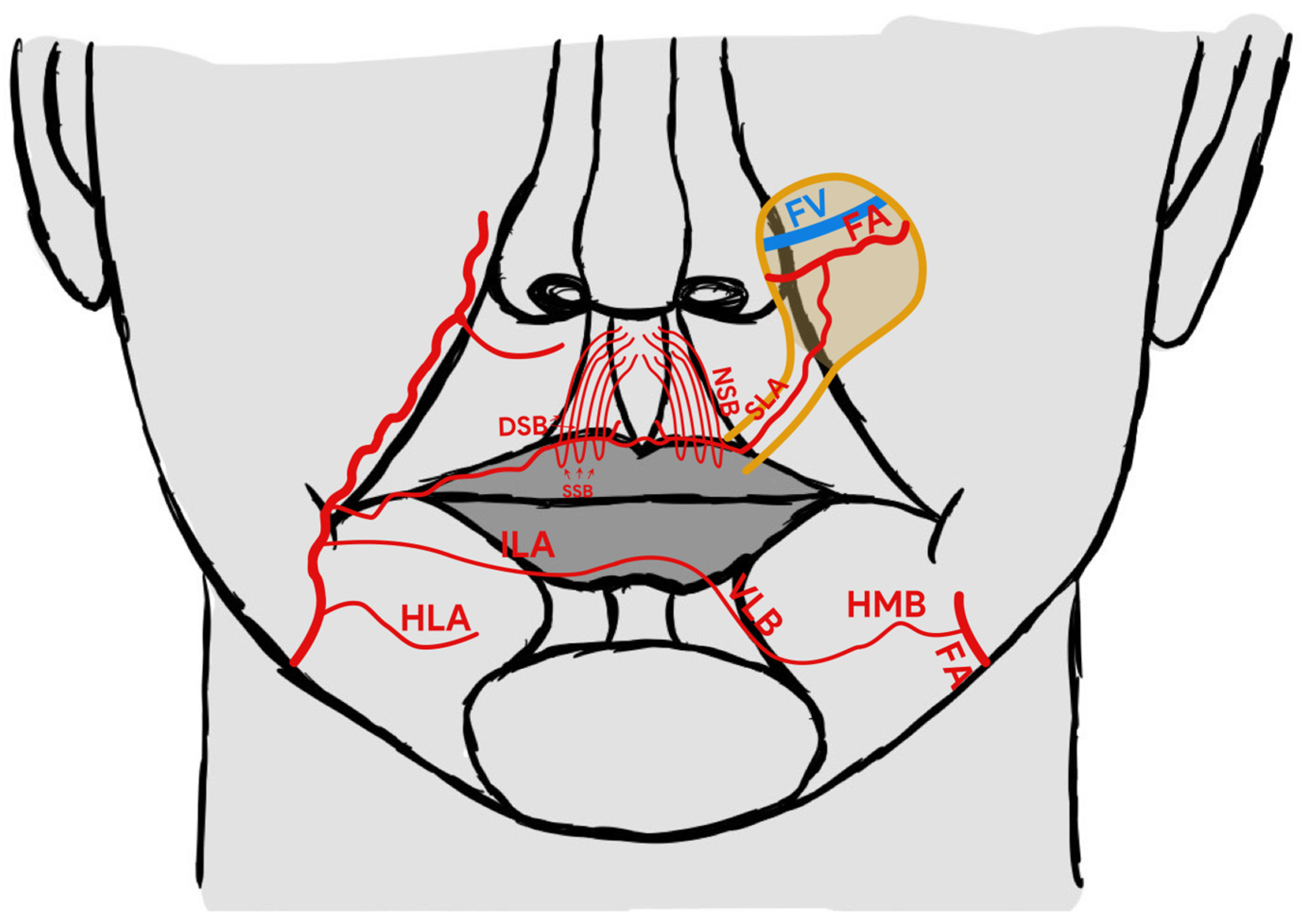
:1. Introduction
2. Case Report
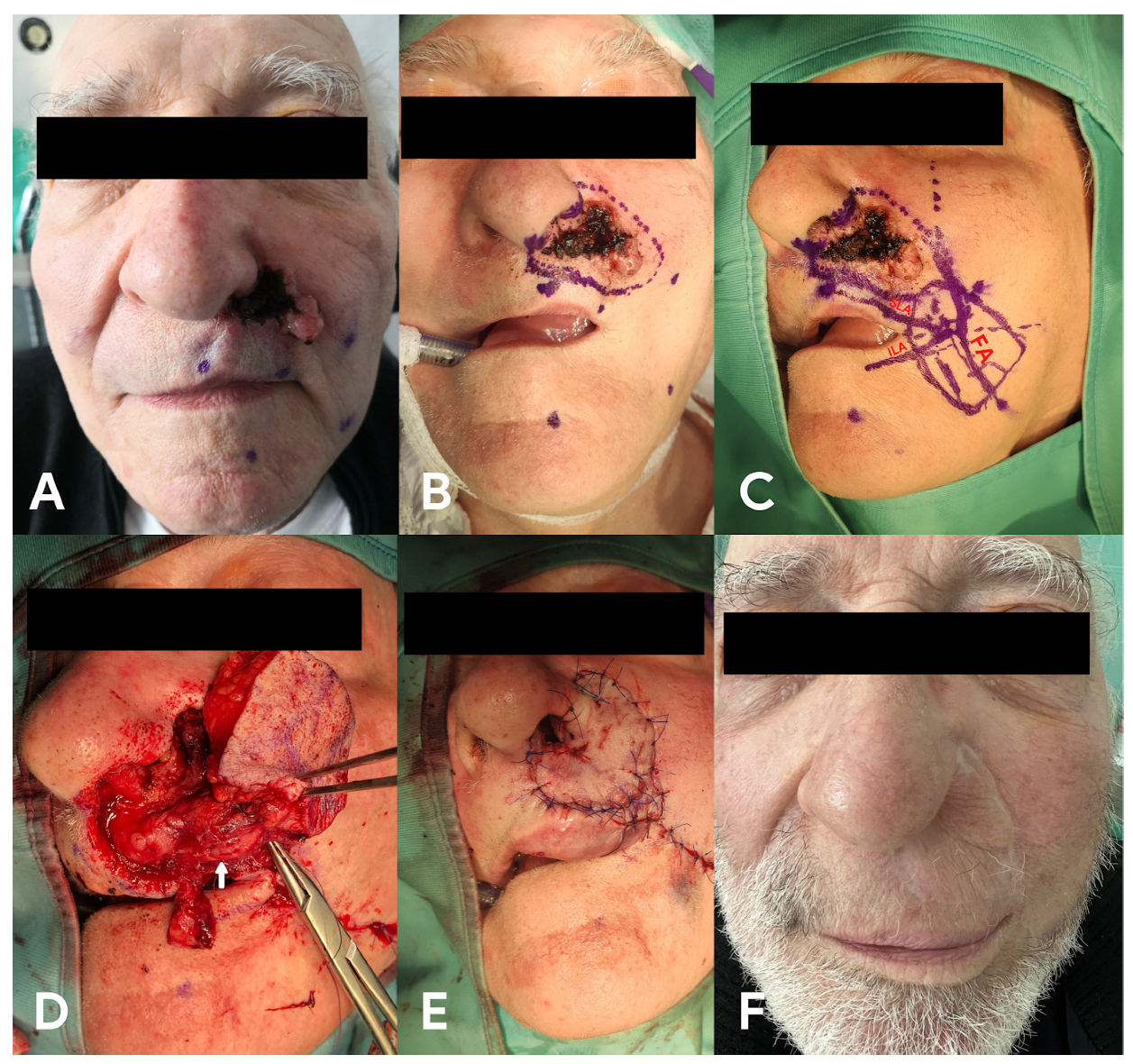
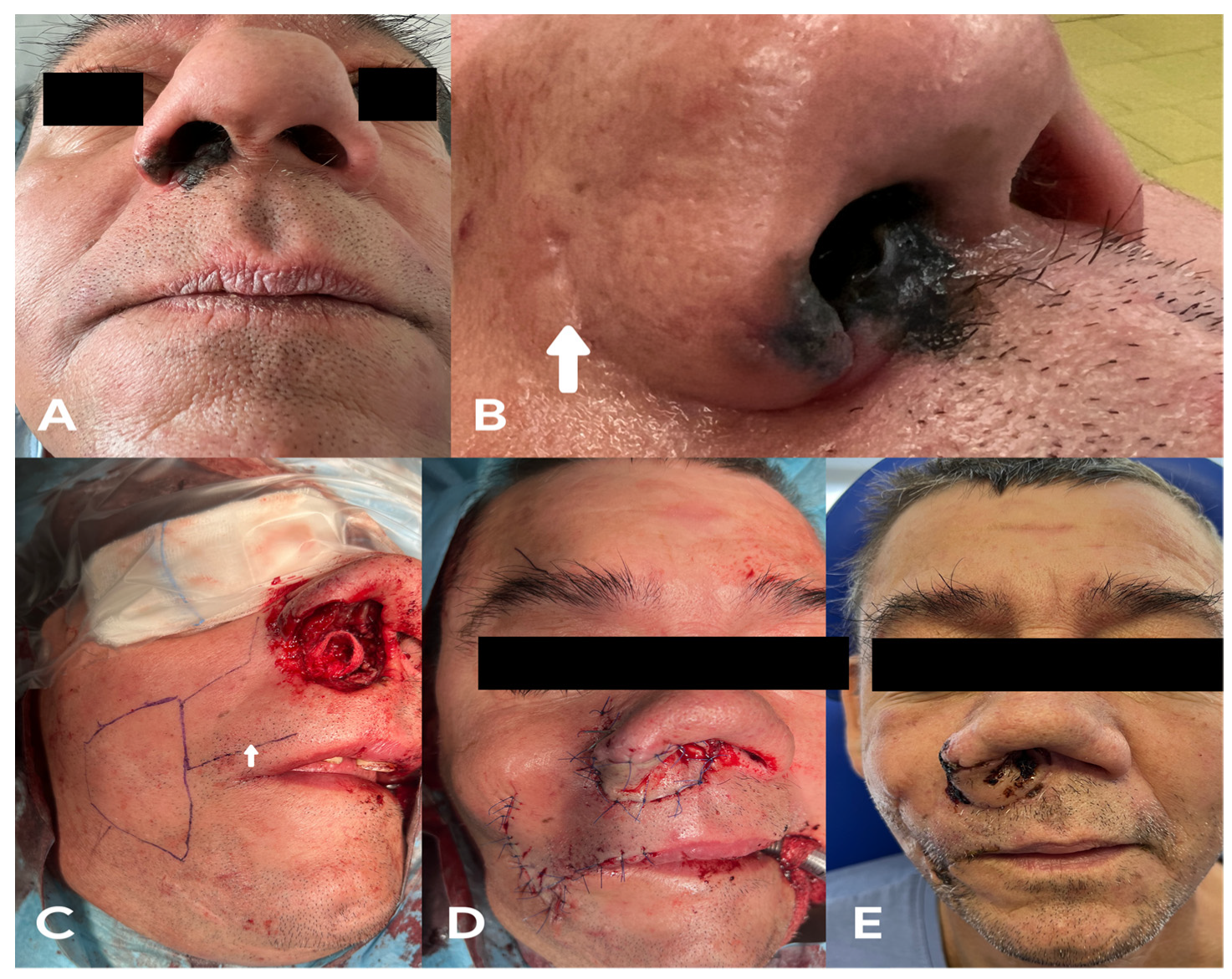
2.1. Case 1
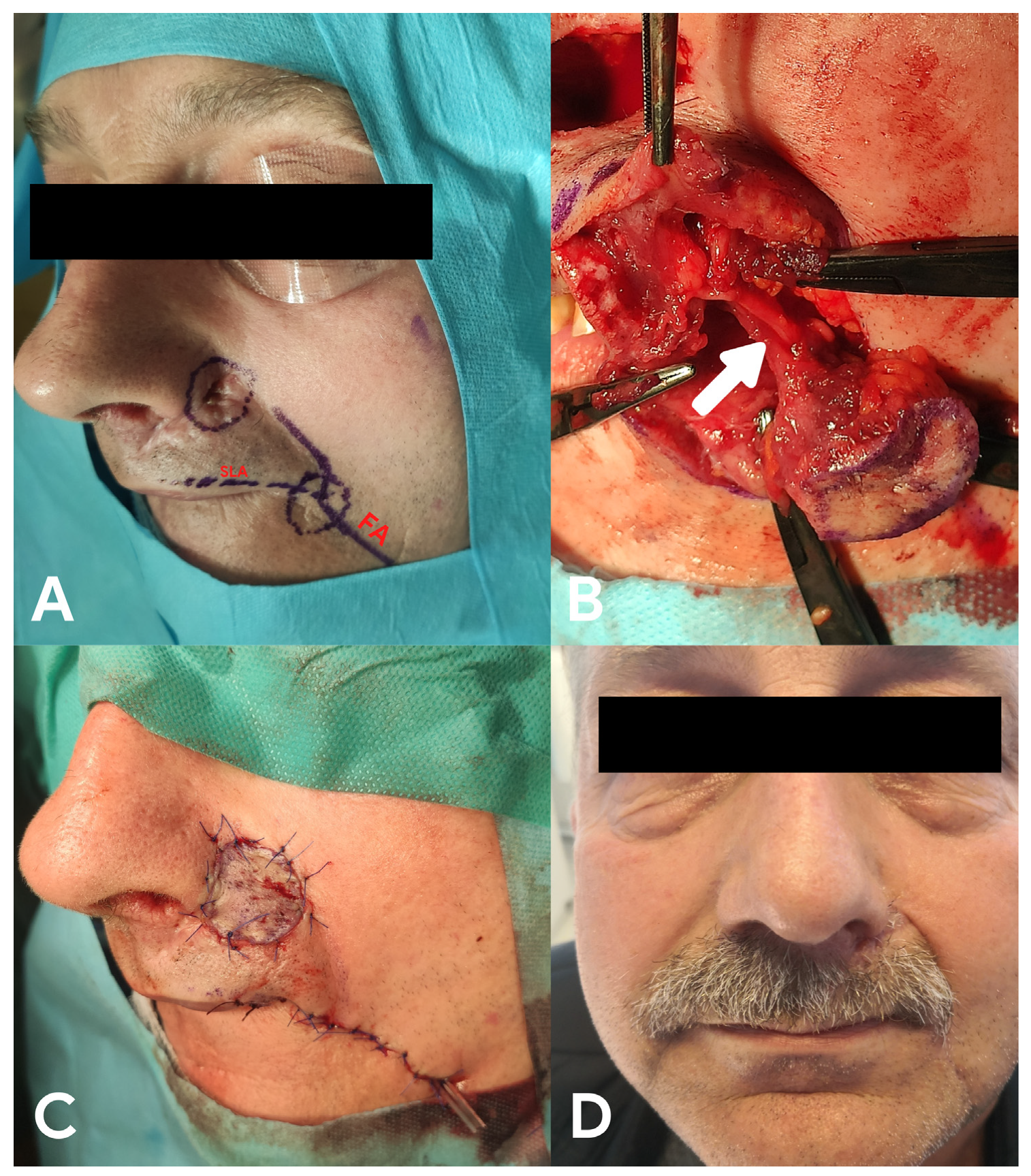
2.2. Case 2
2.3. Case 3
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bostwick, J.; Briedis, J.; Jurkiewicz, M.J. The reverse flow temporal artery island flap. Clin. Plast. Surg. 1976, 3, 441–445. [Google Scholar] [CrossRef]
- Khan, U. Reverse-flow island sural flap. Plast. Reconstr. Surg. 2002, 110, 1592–1593. [Google Scholar] [CrossRef] [PubMed]
- Yamauchi, M.; Yotsuyanagi, T.; Ezoe, K.; Saito, T.; Ikeda, K.; Arai, K. Reverse facial artery flap from the submental region. J. Plast. Reconstr. Aesthet. Surg. 2010, 63, 583–588. [Google Scholar] [CrossRef] [PubMed]
- Haq, A.; Singh, V.; Sharma, S. The reverse flow extensor digitorum brevis flap for dorsal foot defects-A single center study. J. Plast. Reconstr. Aesthet. Surg. 2021, 74, 2957–2964. [Google Scholar] [CrossRef] [PubMed]
- di Summa, P.G.; Sapino, G.; Guillier, D.; Dash, J.; Hart, A.; Raffoul, W. Reverse-Flow Versus Perforator Propeller Lateral Arm Flap for Elbow Reconstruction. Ann. Plast. Surg. 2020, 84, 535–540. [Google Scholar] [CrossRef] [PubMed]
- Saaiq, M.; Zimri, F.U.K. Reverse Flow Superficial Sural Artery Fasciocutaneous Flap: A Comparison of Outcome between Interpolated Flap Design versus Islanded Flap Design. World J. Plast. Surg. 2019, 8, 316–323. [Google Scholar] [PubMed]
- Pascone, M.; Papa, G. The reverse auricular flap for the reconstruction of extended defects of the lower eyelid. Br. J. Plast. Surg. 2005, 58, 806–811. [Google Scholar] [CrossRef]
- Torii, S.; Namiki, Y.; Mori, R. Reverse-flow island flap: Clinical report and venous drainage. Plast. Reconstr. Surg. 1987, 79, 600–609. [Google Scholar] [CrossRef] [PubMed]
- Turan, A.; Kostakoğlu, N.; Tuncel, U. Reverse superior labial artery flap in reconstruction of nose and medial cheek defects. Ann. Plast. Surg. 2015, 74, 418–425. [Google Scholar] [CrossRef] [PubMed]
- Siwetz, M.; Turnowsky, N.; Hammer, N.; Pretterklieber, M.; Wree, A.; Antipova, V. A Rare Case of Facial Artery Branching-A Review of the Literature and a Case Report with Clinical Implications. Medicina 2021, 57, 1172. [Google Scholar] [CrossRef] [PubMed]
- Niranjan, N.S. An anatomical study of the facial artery. Ann. Plast. Surg. 1988, 21, 14–22. [Google Scholar] [CrossRef]
- Park, C.; Lineaweaver, W.C.; Buncke, H.J. New perioral arterial flaps: Anatomic study and clinical application. Plast. Reconstr. Surg. 1994, 94, 268–276. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Lee, H.J.; Kim, Y.S.; Kim, H.J.; Hu, K.S. What is the difference between the inferior labial artery and the horizontal labiomental artery? Surg. Radiol. Anat. 2015, 37, 947–953. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, Y.; Tajima, S. The influence of arterial inflow and venous outflow on the survival of reversed-flow island flaps: An experimental study. Plast. Reconstr. Surg. 1997, 99, 2021–2029. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, M.; Chen, H.K.; Hidetomo, H.; Watanabe, A.; Sakiyama, K.; Kim, H.J.; Murakami, G.; Rodríguez-Vázquez, J.F.; Abe, S. Superior labial artery and vein anastomosis configuration to be considered in lip augmentation. Ann. Anat. 2022, 239, 151808. [Google Scholar] [CrossRef] [PubMed]
- Camuzard, O.; Foissac, R.; Georgiou, C.; Andot, L.; Alcaraz, F.; Baqué, P.; Bronsard, N.; Poissonnet, G. Facial artery perforator flap for reconstruction of perinasal defects: An anatomical study and clinical application. J. Craniomaxillofac. Surg. 2015, 43, 2057–2065. [Google Scholar] [CrossRef] [PubMed]
- Jing, Z.; Yu, G.; Wang, D.; You, M.; Zhang, S. Study of venous drainage in retrograde island flaps by fluorescence tracing technique in a rabbit model. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2008, 22, 959–963. (In Chinese) [Google Scholar] [PubMed]
- Turan, A.; Kostakoglu, N. Reverse Superior Labial Artery Flap in Reconstruction of Nose and Medial Cheek Large Defects: Reply. Ann. Plast. Surg. 2016, 76, 132–133. [Google Scholar] [CrossRef] [PubMed]
- Hwang, K. Surgical anatomy of the facial nerve relating to facial rejuvenation surgery. J. Craniofac. Surg. 2014, 25, 1476–1481. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zwierz, A.; Masna, K.; Perczak, M.; Burduk, P. Unique Characteristics and Applications of Reverse Superior Labial Artery Island Flaps: A Case Series. Medicina 2022, 58, 1012. https://doi.org/10.3390/medicina58081012
Zwierz A, Masna K, Perczak M, Burduk P. Unique Characteristics and Applications of Reverse Superior Labial Artery Island Flaps: A Case Series. Medicina. 2022; 58(8):1012. https://doi.org/10.3390/medicina58081012
Chicago/Turabian StyleZwierz, Aleksander, Krystyna Masna, Marcin Perczak, and Paweł Burduk. 2022. "Unique Characteristics and Applications of Reverse Superior Labial Artery Island Flaps: A Case Series" Medicina 58, no. 8: 1012. https://doi.org/10.3390/medicina58081012
APA StyleZwierz, A., Masna, K., Perczak, M., & Burduk, P. (2022). Unique Characteristics and Applications of Reverse Superior Labial Artery Island Flaps: A Case Series. Medicina, 58(8), 1012. https://doi.org/10.3390/medicina58081012





