Abstract
The novel coronavirus disease 2019 (COVID-19) is associated with several cardiovascular manifestations including myocardial injury, myocarditis, arrhythmia, and pulmonary embolism. Rare cases of stress-induced cardiomyopathy, or takotsubo syndrome have also been reported during the acute infection, and secondary to stress following lockdown and self-isolation. Diagnosis in the setting of the acute infection is challenging since conventional imaging modalities such as transthoracic echocardiography and coronary angiography should be restricted to minimize physician-patient contact until the patients is tested negative for COVID-19. The use of point of care hand-held ultrasound is appropriate for this purpose. The overall course of the disease seems to be similar to takotsubo in the general population. Physicians should be familiar with the clinical presentation, possible complications, and management of takotsubo during COVID-19 outbreak. Here, we review the special considerations in the diagnosis and management of takotsubo syndrome during the current pandemic.
1. Introduction
The novel coronavirus disease 2019 (COVID-19) constitutes an ongoing medical challenge through involvement of multiple organs. The disease is caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and it was first identified in December 2019 in the city of Wuhan, Hubei, China [1]. Several COVID-19-related cardiovascular complications have been described, including myocardial injury, myocarditis, arrhythmia, and pulmonary embolism [2,3,4]. In addition, data has accumulated indicating increased morbidity and mortality rates among patients with background cardiovascular disease during the acute infection [5,6,7,8]. Takotsubo syndrome (TTS) is one of the rare cardiovascular manifestations that has also been reported in COVID-19 [9]. TTS, also called “broken heart syndrome” or stress-induced cardiomyopathy, is a type of acute reversible heart failure that mainly affects postmenopausal women. Various physical or emotional stressors, such as fierce argument, public speaking, grief, happiness, major surgery, and various infectious diseases [10,11] typically precedes the syndrome. Clinical presentation often mimics acute coronary syndrome (ACS) with chest pain, ECG and echocardiographic changes, and elevated cardiac biomarkers [12,13]. Key criteria for diagnosis include typical echocardiographic appearance of basal hypercontractility and apical ballooning, and patent coronary arteries without obstructive disease during angiography [14]. Here, we review the special considerations for the diagnosis and management of TTS and the possible impact of the overwhelming stress accompanying its incidence during the current pandemic.
2. Takotsubo Syndrome in the Setting of Acute COVID-19
2.1. Epidemiology
Similar to other cardiovascular complications, TTS have been reported early with the onset of the COVID-19 pandemic [15,16,17]. In the majority of the reported cases, TTS was with typical echocardiographic appearance of apical ballooning and basal hypercontractility. Late onset [18] and reverse variants (characterized by hypercontractility of the apical region and basal hypokinesia) have also been reported [19,20,21,22,23], and in one case, a patient presented with acute ischemic stroke [24]. According to several echocardiographic studies, the incidence of TTS among infected patients with COVID-19 is around 2–4% [15,16,17]. In the general population, the incidence is about 1–2% among patients presenting with suspected acute coronary syndrome, and it is expected to be higher in elderly women [25,26]. While traditionally TTS predominantly affects women, about one third of COVID-19 related cases were in men [27].
2.2. Pathways and Potential Mechanisms
Acute emotional or physical stressors induce an increase in the levels and bioavailability of catecholamines and cortisol in the blood, which mediate several pathways of epicardial coronary spasm, microvascular dysfunction and direct myocyte injury, all are key findings in TTS [28,29,30]. Clues for the essential role of catecholamines in TTS include the high plasma levels in the affected patients, and the induction of TTS-like disease following epinephrine or norepinephrine administration [31,32]. While catecholamines produce positive inotropic effects through Gs-coupling protein, they activate the β2-Adreoreceptor differently in cardiac tissue. When high levels of epinephrine (but not epinephrine) are secreted, it triggers the β2-adrenoceptor to switch from Gs to Gi coupling. This switch to Gi is dominant in the apical part of cardiac tissue, and it is aimed at limiting the degree of myocardial injury during catecholamine surge induced by the cardiotoxic activation of β1- and β2-adrenoceptor Gs pathways [33]. This unique pattern of protein coupling results finally in cardiac inhibition in the apical part with concomitant compensatory stimulation of the basal section. The result is the unique apical ballooning appearance observed in takotsubo. Of note, biomarkers of myonecrosis, such as troponin are mildly elevated in TTS except for rare cases of severe disease, whereas natriuretic peptides (NPs), a marker for cardiac wall stress, are typically highly elevated [34,35]. Patients with COVID-19 have high circulating levels of catecholamines secondary to endogenous excretion during the acute stress, and often to exogenous intravenous infusion of adrenaline and noradrenaline used to maintain adequate blood supply in critically ill patients [36]. Other than catecholamines, the hypothalamic–pituitary–adrenal (HPA) axis is also activated in severe COVID-19, which finally results in hypercortisolism and corticotropin suppression [37]. Notably, the relation between high cortisol levels and TTS is not well established yet, since TTS has been described in cases of cortisol excess [38] and in secondary adrenal deficiency [39]. In addition, cumulative evidence does exist regarding the neural spread of the virus, mainly in the cortex and hypothalamus [40]. The release of several inflammatory cytokines such as interleukin-6 and tumor necrosis factor-α in the cytokine storm accompanying severe COVID-19 may also induce catecholamines surge [41]. Probably, the mechanism of TTS during the acute infection is multifactorial and mediated by direct effects of cytokine storm and microvascular dysfunction as seen in other infections. It is not clear, however, why high incidence of TTS has been reported during specific infections other than SARS-CoV-2, particularly influenza virus infection [42,43,44,45,46,47]. Moreover, TTS cases have been reported also following COVID-19 vaccinations [48]. It should be noted that disease-induced stress and catecholamine surge may also aggravate these pathways, and such an overlap in mechanisms seems reasonable. Elevated levels of catecholamine were observed in the aortic root and coronary sinus in patients with COVID-19 and TTS [9].
2.3. Diagnostic Considerations
2.3.1. Echocardiography
One of the major limitations in managing patients during the COVID-19 pandemic is the need for minimizing physician–patient contact, at least for the first 1–2 days of patient admission. The current practice during the new Omicron variant outbreak (and perhaps for possible upcoming variants), even with the high percentage of vaccinated patients, is to minimize contact until the patient is tested negative. This need leads to restricted use of several essential imaging modalities, and to the emerging increased use of modified techniques. The use of hand-held point-of-care ultrasound (POCUS) is extremely beneficial for rapid screening of the cardiac structure and function. The yield of POCUS was proved in several cardiovascular conditions including pulmonary embolism, tamponade, myocardial infarction and TTS [49,50,51]. The feasibility and rapid use of POCUS enables general assessment of cardiac condition with minimal exposure to infected patients.
2.3.2. ECG
Common ECG findings in TTS include ST-segment elevation in the precordial leads with no reciprocal changes or Q waves, anterior T wave inversion, and QT-interval prolongation [52,53,54]. It should be noted that in COVID-19, QT prolongation may be a side effect of using proarrhythmic drugs such as quinidine and azithromycin [55,56,57].
2.3.3. Biomarkers
One of the laboratory characteristics of TTS is the discordance in elevation of troponin and N-terminal pro B-type natriuretic peptide (NT-proBNP) levels. Since TTS is not associated with myonecrosis, the elevation in troponin is usually mild unless in severe forms of TTS, while NT-proBNP is significantly elevated reflecting increased wall stress [34,35]. The high NT-proBNP/troponin ratio should be used cautiously in COVID-19 patients for the purpose of TTS diagnosis, since high values of these biomarkers are already increased in patients tested positive for COVID-19.
2.3.4. Coronary Angiography and Cardiac Computed Tomography
The demonstration of patent coronaries without obstructive disease (particularly in the left anterior descending coronary artery) is essential for TTS diagnosis. According to the current reported cases of COVID-19 related TTS, angiography was performed in about 50% of the cases [27]. This finding is probably a consequence of the recommendation for restricting the contact with patients. The use of other modalities such as computed tomography is a reliable alternative for this purpose. In stable patients with preserved global left ventricular function and high suspicion for TTS according to clinical course, ECG, and echocardiography, exclusion of obstructive coronary artery disease using cardiac computed tomography is recommended in order to reduce the risk of contamination. In unstable patients, coronary angiography is mandatory. A simple algorithm for TTS diagnosis during the COVID-19 pandemic is given in Figure 1.
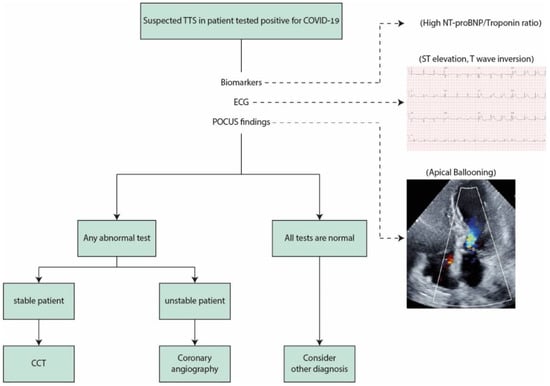
Figure 1.
TTS diagnostic algorithm during COVID-19. TTS: takotsubo syndrome; COVID-19: coronavirus disease 2019; POCUS: point-of-care cardiac ultrasound; CCT: coronary computed tomography.
In case of suspected TTS in patients tested positive for COVID-19, basic tests are recommended. Typical biomarker profile is mild elevation in troponin with excessive NT-proBNP elevation reflecting minor myonecrosis and high cardiac wall stress. The use of POCUS is useful and helps to identify typical wall motion abnormality and exclude other conditions. If all these tests are within normal limits, TTS is unlikely. When the diagnosis is very likely based on the aforementioned tests, and the patient is in stable condition, exclusion of obstructive coronary artery disease using CCT is required. In unstable patients, invasive coronary angiography is the recommended next step.
2.4. Clinical Course and Outcomes
Based on the current available data, 80% of patients with COVID-19 related TTS experienced complete recovery. Nearly 60% of patients received inotropic or ventilatory support, whereas mechanical circulatory support (V-V ECMO) was provided only in one patient [27,57]. Thromboembolic events occurred in 2 cases [24,58] and arrhythmia in another 2 cases [59,60]. It should be noted that thromboembolic (venous and arterial) events have been reported in COVID-19 patients regardless to the occurrence of TTS, particularly in severe cases. In one large registry, major arterial or venous thromboembolic events occurred in 35.3% of COVID-19 patients admitted to intensive care unit (ICU) and in 2.6% of hospitalized non-ICU patients, while symptomatic venous thromboembolism was documented in 27% and 2.2% of ICU and non-ICU patients, respectively [61]. Table 1 summarizes the outcomes of selected cases of TTS in COVID-19 patients [18,19,20,21,22,23,24,57,58,59,60,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79].

Table 1.
Outcomes of patients with TTS in COVID-19.
2.5. Treatment
The treatment of COVID-19 related TTS should be based on treating the infectious disease. Generally, the treatment of TTS is conservative with focus on mental and physical stress relieve. When left ventricular dysfunction is present, beta-blockers and Angiotensin-converting enzyme (ACE) inhibitor are recommended and associated with improved survival [80,81]. Caution is needed when there is left ventricular outflow tract obstruction since inotropic agents are contraindicated in these cases while beta-blockers are beneficial in reducing the obstruction [17]. Antiplatelet therapy is not routinely recommended and may be associated with increased mortality [82]. Despite the role of catecholamine in the pathogenesis of TTS, there is no consensus that beta-blockers use is associated with decrease in TTS recurrence [22]. It should be emphasized that although TTS course is generally benign, lethal complications such as cardiogenic shock, malignant ventricular arrhythmia, and thromboembolic events may occur, and the overall prognosis is comparable to that of ACS [12,83].
2.6. Stress-Induced Takotsubo during Lockdown and Self Isolation
One of the major impacts of the current pandemic are its psychological and social effects, mainly among elderly. High rates of depression and anxiety during lockdown and self-isolation periods have been reported [84]. The social deprivation, which became a direct consequence of COVID-19, may jeopardize patient adherence to therapy, routine medical check-up and follow-up visits, which in turn aggravates depression and anxiety, creating a vicious cycle. The issue whether TTS incidence was affected by COVID-19 burden was addressed in several studies with inconsistent results [85,86,87]. The difference in the results between the studies may be related to different social status of the study population, length of the study period, and the effect of the pandemic on the particular region. Overall, there appears to be an association between TTS incidence and COVID-19 since this cardiomyopathy is mainly mediated by stress-related pathways [88].
3. Prevention
The main potential strategies for TTS prevention during COVID-19 should be focused on limiting stress during this everchanging pandemic. Vaccination against the virus is effective in disease prevention, and it should be encouraged particularly for elderly people and high-risk patients with background comorbidities. It is reasonable to assume that vaccinated patients will experience less stress and anxiety during the pandemic waves. Physicians should be familiar with the possible associations between TTS and COVID-19 since rapid diagnosis and management is essential for avoiding unnecessary medications. Currently, no specific drug is proven to prevent or reduce the incidence of recurrent takotsubo.
4. Conclusions
Similar to other cardiovascular problems, the COVID-19 pandemic poses several challenges in TTS management as well. In order to reduce the risk of contact with patients, POCUS and CCT are preferred over standard echocardiography and invasive angiography, respectively. The management of COVID-19 related TTS should not be different from TTS in the general population. The incidence of stress-induced cardiomyopathy is expected to increase in the general population driven by the ongoing social deprivation and depression. Physicians should be familiar with the clinical presentation, possible complications, and management of takotsubo during COVID-19 outbreak.
Author Contributions
Conceptualization, G.M.; methodology, G.M. and S.A.; writing—review and editing, G.M.; visualization and supervision, S.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Wu, F.; Zhao, S.; Yu, B.; Chen, Y.M.; Wang, W.; Song, Z.G.; Hu, Y.; Tao, Z.W.; Tian, J.H.; Pei, Y.Y.; et al. A new coronavirus associated with human respiratory disease in China. Nature 2020, 579, 265–269. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giustino, G.; Pinney, S.P.; Lala, A.; Reddy, V.Y.; Johnston-Cox, H.A.; Mechanick, J.I.; Halperin, J.L.; Fuster, V. Coronavirus and Cardiovascular Disease, Myocardial Injury, and Arrhythmia: JACC Focus Seminar. J. Am. Coll. Cardiol. 2020, 76, 2011–2023. [Google Scholar] [CrossRef] [PubMed]
- Nishiga, M.; Wang, D.W.; Han, Y.; Lewis, D.B.; Wu, J.C. COVID-19 and cardiovascular disease: From basic mechanisms to clinical perspectives. Nat. Rev. Cardiol. 2020, 17, 543–558. [Google Scholar] [CrossRef] [PubMed]
- Madjid, M.; Safavi-Naeini, P.; Solomon, S.D.; Vardeny, O. Potential Effects of Coronaviruses on the Cardiovascular System: A Review. JAMA Cardiol. 2020, 5, 831–840. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shi, S.; Qin, M.; Cai, Y.; Liu, T.; Shen, B.; Yang, F.; Cao, S.; Liu, X.; Xiang, Y.; Zhao, Q.; et al. Characteristics and clinical significance of myocardial injury in patients with severe coronavirus disease 2019. Eur. Heart J. 2020, 41, 2070–2079. [Google Scholar] [CrossRef] [PubMed]
- Guo, T.; Fan, Y.; Chen, M.; Wu, X.; Zhang, L.; He, T.; Wang, H.; Wan, J.; Wang, X.; Lu, Z. Cardiovascular Implications of Fatal Outcomes of Patients With Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020, 5, 811–818. [Google Scholar] [CrossRef] [Green Version]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Shi, S.; Qin, M.; Shen, B.; Cai, Y.; Liu, T.; Yang, F.; Gong, W.; Liu, X.; Liang, J.; Zhao, Q.; et al. Association of Cardiac Injury with Mortality in Hospitalized Patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020, 5, 802–810. [Google Scholar] [CrossRef] [Green Version]
- Okura, H. Update of takotsubo syndrome in the era of COVID-19. J. Cardiol. 2021, 77, 361–369. [Google Scholar] [CrossRef]
- Kato, K.; Lyon, A.R.; Ghadri, J.R.; Templin, C. Takotsubo syndrome: Aetiology, presentation and treatment. Heart 2017, 103, 1461–1469. [Google Scholar] [CrossRef]
- Lyon, A.R.; Bossone, E.; Schneider, B.; Sechtem, U.; Citro, R.; Underwood, S.R.; Sheppard, M.N.; Figtree, G.A.; Parodi, G.; Akashi, Y.J.; et al. Current state of knowledge on Takotsubo syndrome: A Position Statement from the Taskforce on Takotsubo Syndrome of the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 2016, 18, 8–27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Templin, C.; Ghadri, J.R.; Diekmann, J.; Napp, L.C.; Bataiosu, D.R.; Jaguszewski, M.; Cammann, V.L.; Sarcon, A.; Geyer, V.; Neumann, C.A.; et al. Clinical Features and Outcomes of Takotsubo (Stress) Cardiomyopathy. N. Engl. J. Med. 2015, 373, 929–938. [Google Scholar] [PubMed] [Green Version]
- Moady, G.; Vons, S.; Atar, S. A Comparative Retrospective Study of Patients with Takotsubo Syndrome and Acute Coronary Syndrome. Isr. Med. Assoc. J. 2021, 23, 107–110. [Google Scholar] [PubMed]
- Ghadri, J.R.; Wittstein, I.S.; Prasad, A.; Sharkey, S.; Dote, K.; Akashi, Y.J.; Cammann, V.L.; Crea, F.; Galiuto, L.; Desmet, W.; et al. International Expert Consensus Document on Takotsubo Syndrome (Part I): Clinical Characteristics, Diagnostic Criteria, and Pathophysiology. Eur. Heart J. 2018, 39, 2032–2046. [Google Scholar] [CrossRef] [Green Version]
- Hegde, S.; Khan, R.; Zordok, M.; Maysky, M. Characteristics and outcome of patients with COVID-19 complicated by Takotsubo cardiomyopathy: Case series with literature review. Open Heart 2020, 7, e001360. [Google Scholar] [CrossRef]
- Giustino, G.; Croft, L.B.; Oates, C.P.; Rahman, K.; Lerakis, S.; Reddy, V.Y.; Goldman, M. Takotsubo Cardiomyopathy in COVID-19. J. Am. Coll. Cardiol. 2020, 76, 628–629. [Google Scholar] [CrossRef]
- Dweck, M.R.; Bularga, A.; Hahn, R.T.; Bing, R.; Lee, K.K.; Chapman, A.R.; White, A.; Salvo, G.D.; Sade, L.E.; Pearce, K.; et al. Global evaluation of echocardiography in patients with COVID-19. Eur. Heart J. Cardiovasc. Imaging 2020, 21, 949–958. [Google Scholar] [CrossRef]
- Bottiroli, M.; De Caria, D.; Belli, O.; Calini, A.; Andreoni, P.; Siragusa, A.; Moreo, A.; Ammirati, E.; Mondino, M.; Fumagalli, R. Takotsubo syndrome as a complication in a critically ill COVID-19 patient. ESC Heart Fail. ESC Heart Fail. 2020, 7, 4297–4300. [Google Scholar] [CrossRef]
- Faqihi, F.; Alharthy, A.; Alshaya, R.; Papanikolaou, J.; Kutsogiannis, D.J.; Brindley, P.G.; Karakitsos, D. Reverse takotsubo cardiomyopathy in fulminant COVID-19 associated with cytokine release syndrome and resolution following therapeutic plasma exchange: A case-report. BMC Cardiovasc. Disord. 2020, 20, 389. [Google Scholar]
- Nguyen, D.; Nguyen, T.; De Bels, D.; Castro Rodriguez, J. A case of Takotsubo cardiomyopathy with COVID 19. Eur. Heart J. Cardiovasc. Imaging 2020, 21, 1052. [Google Scholar]
- Panchal, A.; Kyvernitakis, A.; Biederman, R. An Interesting Case of COVID-19 Induced Reversed Takotsubo Cardiomyopathy and Insight on Cardiac Biomarkers. Cureus 2020, 12, e11296. [Google Scholar] [CrossRef] [PubMed]
- Sala, S.; Peretto, G.; Gramegna, M.; Palmisano, A.; Villatore, A.; Vignale, D.; De Cobelli, F.; Tresoldi, M.; Cappelletti, A.M.; Basso, C.; et al. Acute myocarditis presenting as a reverse Tako-Tsubo syndrome in a patient with SARS-CoV-2 respiratory infection. Eur. Heart J. 2020, 41, 1861–1862. [Google Scholar] [CrossRef] [PubMed]
- Dabbagh, M.F.; Aurora, L.; D’Souza, P.; Weinmann, A.J.; Bhargava, P.; Basir, M.B. Cardiac Tamponade Secondary to COVID-19. JACC Case Rep. 2020, 2, 1326–1330. [Google Scholar] [CrossRef] [PubMed]
- Kariyanna, P.T.; Chandrakumar, H.P.; Jayarangaiah, A.; Khan, A.; Vulkanov, V.; Ashamalla, M.; Salifu, M.O.; McFarlane , S.I. Apical Takotsubo Cardiomyopathy in a COVID-19 Patient Presenting with Stroke: A Case Report and Pathophysiologic Insights. Am. J. Med. Case Rep. 2020, 8, 350–357. [Google Scholar] [CrossRef]
- Akashi, Y.J.; Nef, H.M.; Lyon, A.R. Epidemiology and pathophysiology of Takotsubo syndrome. Nat. Rev. Cardiol. 2015, 12, 387–397. [Google Scholar] [CrossRef] [Green Version]
- Citro, R.; Radano, I.; Bellino, M.; Mauro, C.; Okura, H.; Bossone, E.; Akashy, Y.J. Epidemiology, Pathogenesis, and Clinical Course of Takotsubo Syndrome. Heart Fail. Clin. 2022, 18, 125–137. [Google Scholar] [CrossRef]
- Moady, G.; Atar, S. Takotsubo Syndrome during the COVID-19 Pandemic: State-of-the-Art Review. CJC Open 2021, 3, 1249–1256. [Google Scholar] [CrossRef]
- Wittstein, I.S. The Sympathetic Nervous System in the Pathogenesis of Takotsubo Syndrome. Heart Fail. Clin. 2016, 12, 485–498. [Google Scholar] [CrossRef]
- Wittstein, I.S.; Thiemann, D.R.; Lima, J.A.; Baughman, K.L.; Schulman, S.P.; Gerstenblith, G.; Wu, K.C.; Rade, J.J.; Bivalacqua, T.J.; Champion, H.C. Neurohumoral features of myocardial stunning due to sudden emotional stress. N. Engl. J. Med. 2005, 352, 539–548. [Google Scholar] [CrossRef]
- Pelliccia, F.; Kaski, J.C.; Crea, F.; Camici, P.G. Pathophysiology of Takotsubo Syndrome. Circulation 2017, 135, 2426–2441. [Google Scholar] [CrossRef]
- Abraham, J.; Mudd, J.O.; Kapur, N.K.; Klein, K.; Champion, H.C.; Wittstein, I.S. Stress cardiomyopathy after intravenous administration of catecholamines and beta-receptor agonists. J. Am. Coll. Cardiol. 2009, 53, 1320–1325. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kido, K.; Guglin, M. Drug-Induced Takotsubo Cardiomyopathy. J. Cardiovasc. Pharmacol. Ther. 2017, 22, 552–563. [Google Scholar] [CrossRef] [PubMed]
- Paur, H.; Wright, P.T.; Sikkel, M.B.; Tranter, M.H.; Mansfield, C.; O’Gara, P.; Stuckey, D.J.; Nikolaev, V.O.; Diakonov, I.; Pannell, L.; et al. High levels of circulating epinephrine trigger apical cardiodepression in a β2-adrenergic receptor/Gi-dependent manner: A new model of Takotsubo cardiomyopathy. Circulation 2012, 126, 697–706. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stiermaier, T.; Santoro, F.; Graf, T.; Guastafierro, F.; Tarantino, N.; De Gennaro, L.; Caldarola, P.; Di Biase, M.; Thiele, H.; Brunetti, N.D.; et al. Prognostic value of N-Terminal Pro-B-Type Natriuretic Peptide in Takotsubo syndrome. Clin. Res. Cardiol. 2018, 107, 597–606. [Google Scholar] [CrossRef]
- Fröhlich, G.M.; Schoch, B.; Schmid, F.; Keller, P.; Sudano, I.; Lüscher, T.F.; Noll, G.; Ruschitzka, F.; Enseleit, F. Takotsubo cardiomyopathy has a unique cardiac biomarker profile: NT-proBNP/myoglobin and NT-proBNP/troponin T ratios for the differential diagnosis of acute coronary syndromes and stress induced cardiomyopathy. Int. J. Cardiol. 2012, 154, 328–332. [Google Scholar] [CrossRef] [Green Version]
- Gubbi, S.; Nazari, M.A.; Taieb, D.; Klubo-Gwiezdzinska, J.; Pacak, K. Catecholamine physiology and its implications in patients with COVID-19. Lancet Diabetes Endocrinol. 2020, 8, 978–986. [Google Scholar] [CrossRef]
- Boonen, E.; Vervenne, H.; Meersseman, P.; Andrew, R.; Mortier, L.; Declercq, P.E.; Vanwijngaerden, Y.M.; Spriet, I.; Wouters, P.J.; Vander Perre, S.; et al. Reduced cortisol metabolism during critical illness. N. Engl. J. Med. 2013, 368, 1477–1488. [Google Scholar] [CrossRef] [Green Version]
- Wickboldt, N.; Pache, J.C.; Dietrich, P.Y.; Toso, C.; Gallay, C.; Brochard, L.; Merlani, P.; Pugin, D. Takotsubo syndrome secondary to adrenal adenocarcinoma: Cortisol as a possible culprit. Am. J. Respir. Crit. Care Med. 2012, 186, 1061–1062. [Google Scholar] [CrossRef]
- Sakihara, S.; Kageyama, K.; Nigawara, T.; Kidani, Y.; Suda, T. Ampulla (takotsubo) cardiomyopathy caused by secondary adrenal insufficiency in ACTH isolated deficiency. Endocr. J. 2007, 54, 631–636. [Google Scholar] [CrossRef] [Green Version]
- Tanasa, I.A.; Manciuc, C.; Carauleanu, A.; Navolan, D.B.; Bohiltea, R.E.; Nemescu, D. Anosmia and ageusia associated with coronavirus infection (COVID-19)—what is known? Exp. Ther. Med. 2020, 20, 2344–2347. [Google Scholar] [CrossRef]
- Staedtke, V.; Bai, R.Y.; Kim, K.; Darvas, M.; Davila, M.L.; Riggins, G.J.; Rothman, P.B.; Papadopoulos, N.; Kinzler, K.W.; Vogelstein, B.; et al. Disruption of a self-amplifying catecholamine loop reduces cytokine release syndrome. Nature 2018, 564, 273–277. [Google Scholar] [CrossRef]
- Lozano, A.; Bastante, T.; Salamanca, J.; Aguilar, R.; Montes de Oca, R.; Rodríguez, D.; Alfonso, F. Tako-tsubo cardiomyopathy triggered by Influenza A virus infection. Int. J. Cardiol. 2014, 174, e52–e53. [Google Scholar] [CrossRef] [PubMed]
- Elikowski, W.; Małek-Elikowska, M.; Lisiecka, M.; Trypuć, Z.; Mozer-Lisewska, I. Takotsubo cardiomyopathy triggered by influenza B. Pol. Merkur. Lek. 2018, 45, 67–70. [Google Scholar]
- Buzon, J.; Roignot, O.; Lemoine, S.; Perez, P.; Kimmoun, A.; Levy, B.; Novy, E. Takotsubo Cardiomyopathy Triggered by Influenza A Virus. Intern. Med. 2015, 54, 2017–2019. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Golfeyz, S.; Kobayashi, T.; Aoi, S.; Harrington, M. Possible association of influenza A infection and reverse takotsubo syndrome. BMJ Case Rep. 2018, 11, e226289. [Google Scholar] [CrossRef]
- Faircloth, E.L.; Memon, S. Stressing Out from the Flu: A Case of Influenza A-associated Transient Cardiomyopathy. Cureus 2019, 11, e4918. [Google Scholar] [CrossRef] [Green Version]
- Nakamura, M.; Nakagaito, M.; Hori, M.; Ueno, H.; Kinugawa, K. A case of Takotsubo cardiomyopathy with cardiogenic shock after influenza infection successfully recovered by IMPELLA support. J. Artif. Organs 2019, 22, 330–333. [Google Scholar] [CrossRef]
- Fazlollahi, A.; Zahmatyar, M.; Noori, M.; Nejadghaderi, S.A.; Sullman, M.J.M.; Shekarriz-Foumani, R.; Kolahi, A.A.; Singh, K.; Safiri, S. Cardiac complications following mRNA COVID-19 vaccines: A systematic review of case reports and case series. Rev. Med. Virol. 2021, 17, e2318. [Google Scholar] [CrossRef]
- Madias, J.E. COVID-19, POCUS, and Takotsubo. Am. J. Cardiol. 2021, 141, 157. [Google Scholar] [CrossRef]
- Barnicle, R.; Bracey, A.; Secko, M. Early Identification of Takotsubo syndrome in the emergency department using point-of-care echocardiography: A case series. J. Clin. Ultrasound 2021, 49, 413–419. [Google Scholar] [CrossRef]
- Picard, M.H.; Weiner, R.B. Echocardiography in the Time of COVID-19. J. Am. Soc. Echocardiogr. 2020, 33, 674–675. [Google Scholar] [CrossRef] [PubMed]
- Frangieh, A.H.; Obeid, S.; Ghadri, J.R.; Imori, Y.; D’Ascenzo, F.; Kovac, M.; Ruschitzka, F.; Lüscher, T.F.; Duru, F.; Templin, C.; et al. ECG Criteria to Differentiate Between Takotsubo (Stress) Cardiomyopathy and Myocardial Infarction. J. Am. Heart Assoc. 2016, 5, e003418. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chhabra, L.; Butt, N.; Ahmad, S.A.; Kayani, W.T.; Sangong, A.; Patel, V.; Bharaj, G.; Khalid, N. Electrocardiographic changes in Takotsubo cardiomyopathy. J. Electrocardiol. 2021, 65, 28–33. [Google Scholar] [CrossRef] [PubMed]
- Thakar, S.; Chandra, P.; Hollander, G.; Lichstein, E. Electrocardiographic changes in Takotsubo cardiomyopathy. Pacing Clin. Electrophysiol. 2011, 34, 1278–1282. [Google Scholar] [CrossRef]
- Kochi, A.N.; Tagliari, A.P.; Forleo, G.B.; Fassini, G.M.; Tondo, C. Cardiac and arrhythmic complications in patients with COVID-19. J. Cardiovasc. Electrophysiol. 2020, 31, 1003–1008. [Google Scholar] [CrossRef] [Green Version]
- Dherange, P.; Lang, J.; Qian, P.; Oberfeld, B.; Sauer, W.H.; Koplan, B.; Tedrow, U. Arrhythmias and COVID-19: A Review. JACC Clin. Electrophysiol. 2020, 6, 1193–1204. [Google Scholar] [CrossRef]
- Chao, C.J.; DeValeria, P.A.; Sen, A.; Lee, H.; Pedrotty, D.M.; Patel, B.; Arsanjani, R.; Naqvi, T.Z. Reversible cardiac dysfunction in severe COVID-19 infection, mechanisms and case report. Echocardiography 2020, 37, 1465–1469. [Google Scholar] [CrossRef]
- Bernardi, N.; Calvi, E.; Cimino, G.; Pascariello, G.; Nardi, M.; Cani, D.; Faggiano, P.; Vizzardi, E.; Nunzia, D.M.; Marco, M. COVID-19 Pneumonia, Takotsubo Syndrome, and Left Ventricle Thrombi. JACC Case Rep. 2020, 2, 1359–1364. [Google Scholar] [CrossRef]
- Sattar, Y.; Connerney, M.; Ullah, W.; Philippou, A.; Slack, D.; McCarthy, B.; Kroll, S.; Luddington, S.; Ruiz Maya, T.; Alraies, M.C. COVID-19 Presenting as Takotsubo Cardiomyopathy Complicated with Atrial Fibrillation. Int. J. Cardiol. Heart Vasc. 2020, 29, 100580. [Google Scholar] [CrossRef]
- Tsao, C.W.; Strom, J.B.; Chang, J.D.; Manning, W.J. COVID-19-Associated Stress (Takotsubo) Cardiomyopathy. Circ. Cardiovasc. Imaging 2020, 13, e011222. [Google Scholar] [CrossRef]
- Bikdeli, B.; Madhavan, M.V.; Jimenez, D.; Chuich, T.; Dreyfus, I.; Driggin, E.; Nigoghossian, C.; Ageno, W.; Madjid, M.; Guo, Y.; et al. COVID-19 and Thrombotic or Thromboembolic Disease: Implications for Prevention, Antithrombotic Therapy, and Follow-Up: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2020, 75, 2950–2973. [Google Scholar] [CrossRef] [PubMed]
- Titi, L.; Magnanimi, E.; Mancone, M.; Infusino, F.; Coppola, G.; Del Nonno, F.; Colombo, D.; Nardacci, R.; Falasca, L.; d’Amati, G.; et al. Fatal Takotsubo syndrome in critical COVID-19 related pneumonia. Cardiovasc. Pathol. 2020, 51, 107314. [Google Scholar] [CrossRef] [PubMed]
- Bapat, A.; Maan, A.; Heist, E.K. Stress-Induced Cardiomyopathy Secondary to COVID-19. Case Rep Cardiol. 2020, 2020, 8842150. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharyya, P.J.; Attri, P.K.; Farooqui, W. Takotsubo cardiomyopathy in early term pregnancy: A rare cardiac complication of SARS-CoV-2 infection. BMJ Case Rep. 2020, 13, e239104. [Google Scholar] [CrossRef] [PubMed]
- Dave, S.; Thibodeau, J.T.; Styrvoky, K.; Bhatt, S.H. Takotsubo Cardiomyopathy in a Coronavirus Disease-2019-Positive Patient: A Case Report. A&A Pract. 2020, 14, e01304. [Google Scholar]
- Gomez, J.M.D.; Nair, G.; Nanavaty, P.; Rao, A.; Marinescu, K.; Suboc, T. COVID-19-associated takotsubo cardiomyopathy. BMJ Case Rep. 2020, 13, e236811. [Google Scholar] [CrossRef]
- Torabi, A.J.; Villegas-Galaviz, J.; Guglin, M.; Frick, K.; Rao, R. Cardiogenic shock following cardiac tamponade and Takotsubo in COVID-19. Future Cardiol. 2021, 17, 631–635. [Google Scholar] [CrossRef]
- Koh, M.C.Y.; Li, T.Y.W.; Ong, J.S.Y.; Somani, J.; Ambhore, A.A. Stress Cardiomyopathy with Transient Biventricular Dysfunction Following Recent COVID-19 Infection. Acta Cardiol. Sin. 2021, 37, 204–207. [Google Scholar]
- Khalid, Y.; Dasu, N.; Dasu, K. A case of novel coronavirus (COVID-19)-induced viral myocarditis mimicking a Takotsubo cardiomyopathy. HeartRhythm Case Rep. 2020, 6, 473–476. [Google Scholar] [CrossRef]
- Manzur-Sandoval, D.; Carmona-Levario, P.; García-Cruz, E. Giant inverted T waves in a patient with COVID-19 infection. Ann. Emerg. Med. 2021, 77, 264–267. [Google Scholar] [CrossRef]
- Minhas, A.S.; Scheel, P.; Garibaldi, B.; Liu, G.; Horton, M.; Jennings, M.; Jones, S.R.; Michos, E.D.; Hays, A.G. Takotsubo Syndrome in the Setting of COVID-19. JACC Case Rep. 2020, 2, 1321–1325. [Google Scholar] [CrossRef] [PubMed]
- Moderato, L.; Monello, A.; Lazzeroni, D.; Binno, S.; Giacalone, R.; Ferraro, S.; Piepoli, M.F.; Villani, G.Q. Sindrome Takotsubo in corso di polmonite da SARS-CoV-2: Una possibile complicanza cardiovascolare [Takotsubo syndrome during SARS-CoV-2 pneumonia: A possible cardiovascular complication]. G. Ital. Cardiol. 2020, 21, 417–420. [Google Scholar]
- Oyarzabal, L.; Gómez-Hospital, J.A.; Comin-Colet, J. Tako-tsubo syndrome associated with COVID-19. Rev. Esp. Cardiol. 2020, 73, 846. [Google Scholar] [CrossRef] [PubMed]
- Pasqualetto, M.C.; Secco, E.; Nizzetto, M.; Scevola, M.; Altafini, L.; Cester, A.; Rigo, F. Stress Cardiomyopathy in COVID-19 Disease. Eur. J. Case Rep. Intern. Med. 2020, 7, 001718. [Google Scholar] [PubMed]
- Van Osch, D.; Asselbergs, F.W.; Teske, A.J. Takotsubo cardiomyopathy in COVID-19: A case report. Haemodynamic and therapeutic considerations. Eur. Heart J. Case Rep. 2020, 4, 1–6. [Google Scholar] [CrossRef]
- Roca, E.; Lombardi, C.; Campana, M.; Vivaldi, O.; Bigni, B.; Bertozzi, B.; Passalacqua, G. Takotsubo Syndrome Associated with COVID-19. Eur. J. Case Rep. Intern. Med. 2020, 7, 001665. [Google Scholar] [CrossRef]
- Sang, C.J., III; Heindl, B.; Von Mering, G.; Brott, B.; Kopf, R.S.; Benson, P.V.; Rajapreyar, I. Stress-Induced Cardiomyopathy Precipitated by COVID-19 and Influenza A Coinfection. JACC Case Rep. 2020, 2, 1356–1358. [Google Scholar] [CrossRef]
- Taza, F.; Zulty, M.; Kanwal, A.; Grove, D. Takotsubo cardiomyopathy triggered by SARS-CoV-2 infection in a critically ill patient. BMJ Case Rep. 2020, 13, e236561. [Google Scholar] [CrossRef]
- Solano-López, J.; Sánchez-Recalde, A.; Zamorano, J.L. SARS-CoV-2, a novel virus with an unusual cardiac feature: Inverted takotsubo syndrome. Eur. Heart J. 2020, 41, 3106. [Google Scholar] [CrossRef]
- Medina de Chazal, H.; Del Buono, M.G.; Keyser-Marcus, L.; Ma, L.; Moeller, F.G.; Berrocal, D. Stress Cardiomyopathy Diagnosis and Treatment: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2018, 72, 1955–1971. [Google Scholar] [CrossRef]
- Sattar, Y.; Siew, K.S.W.; Connerney, M.; Ullah, W.; Alraies, M.C. Management of Takotsubo Syndrome: A Comprehensive Review. Cureus 2020, 12, e6556. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rizzetto, F.; Lia, M.; Widmann, M.; Tavella, D.; Zanolla, L.; Pighi, M.; Ferrero, V.; Ribichini, F.L. Prognostic impact of antiplatelet therapy in Takotsubo syndrome: A systematic review and meta-analysis of the literature. Heart Fail. Rev. 2021; Online ahead of print. [Google Scholar]
- Redfors, B.; Jha, S.; Thorleifsson, S.; Jernberg, T.; Angerås, O.; Frobert, O.; Petursson, P.; Tornvall, P.; Sarno, G.; Ekenbäck, C.; et al. Short- and Long-Term Clinical Outcomes for Patients with Takotsubo Syndrome and Patients with Myocardial Infarction: A Report from the Swedish Coronary Angiography and Angioplasty Registry. J. Am. Heart Assoc. 2021, 10, e017290. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [Green Version]
- Delmas, C.; Bouisset, F.; Lairez, O. COVID-19 pandemic: No increase of takotsubo syndrome occurrence despite high-stress conditions. ESC Heart Fail. 2020, 7, 2143. [Google Scholar] [CrossRef]
- Barbieri, L.; Galli, F.; Conconi, B.; Gregorini, T.; Lucreziotti, S.; Mafrici, A.; Pravettoni, G.; Sommaruga, M.; Carugo, S. Takotsubo syndrome in COVID-19 era: Is psychological distress the key? J. Psychosom. Res. 2021, 140, 110297. [Google Scholar] [CrossRef]
- Jabri, A.; Kalra, A.; Kumar, A.; Alameh, A.; Adroja, S.; Bashir, H.; Nowacki, A.S.; Shah, R.; Khubber, S.; Kanaa’N, A.; et al. Incidence of Stress Cardiomyopathy during the Coronavirus Disease 2019 Pandemic. JAMA Netw. Open 2020, 3, e2014780. [Google Scholar] [CrossRef]
- Moady, G.; Atar, S. Quarantine-induced Stress Cardiomyopathy (Takotsubo syndrome) during the COVID-19 pandemic. Isr. Med. Assoc. J. 2021, 23, 149–152. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).