Vaginal Bipolar Radiofrequency Treatment of Mild SUI: A Pilot Retrospective Study
Abstract
1. Introduction
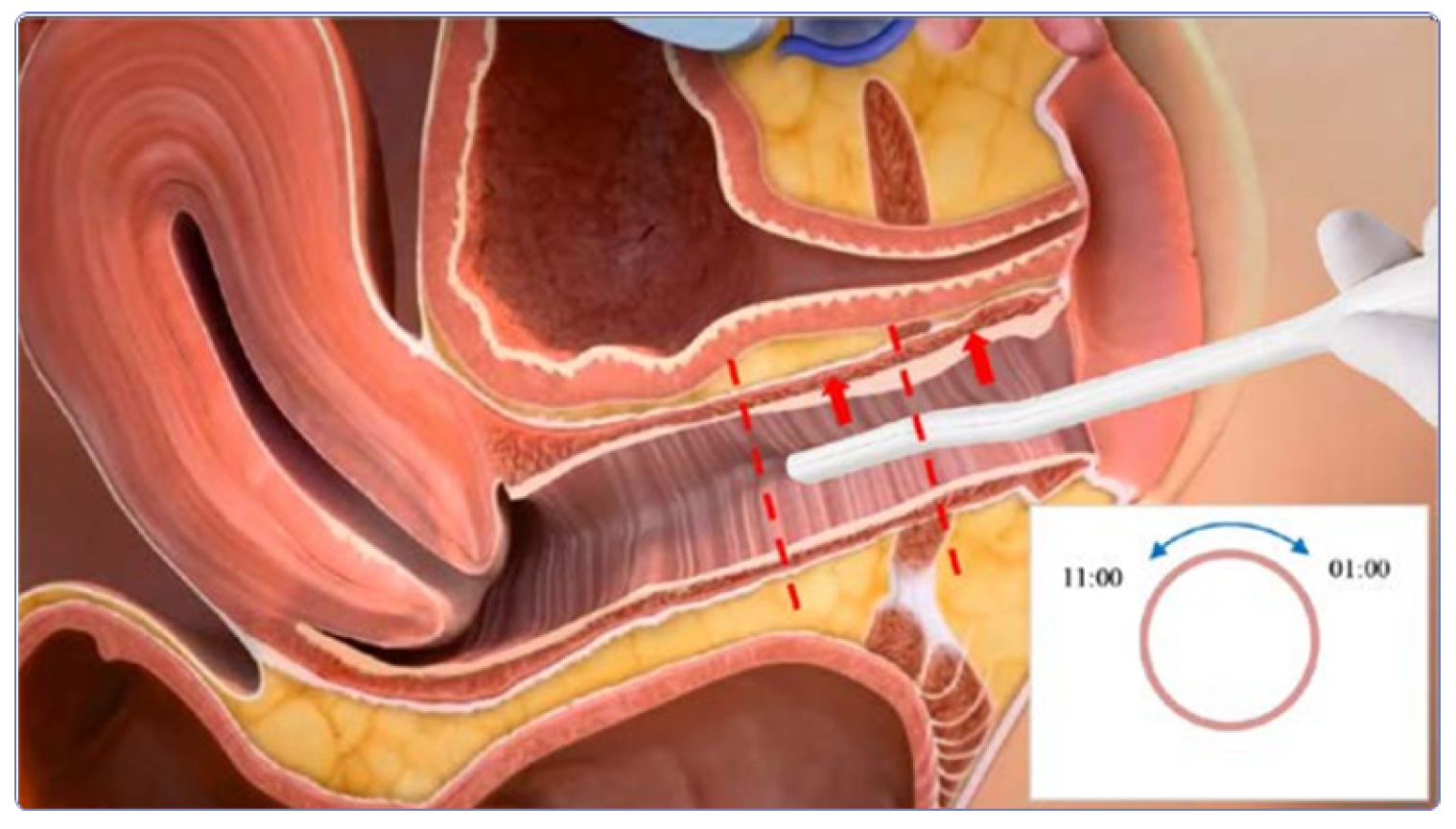
2. Materials and Methods
2.1. Patient Selection
2.2. Pre-Treatment Indications
2.3. Study Protocol
2.4. Post-Treatment Indications
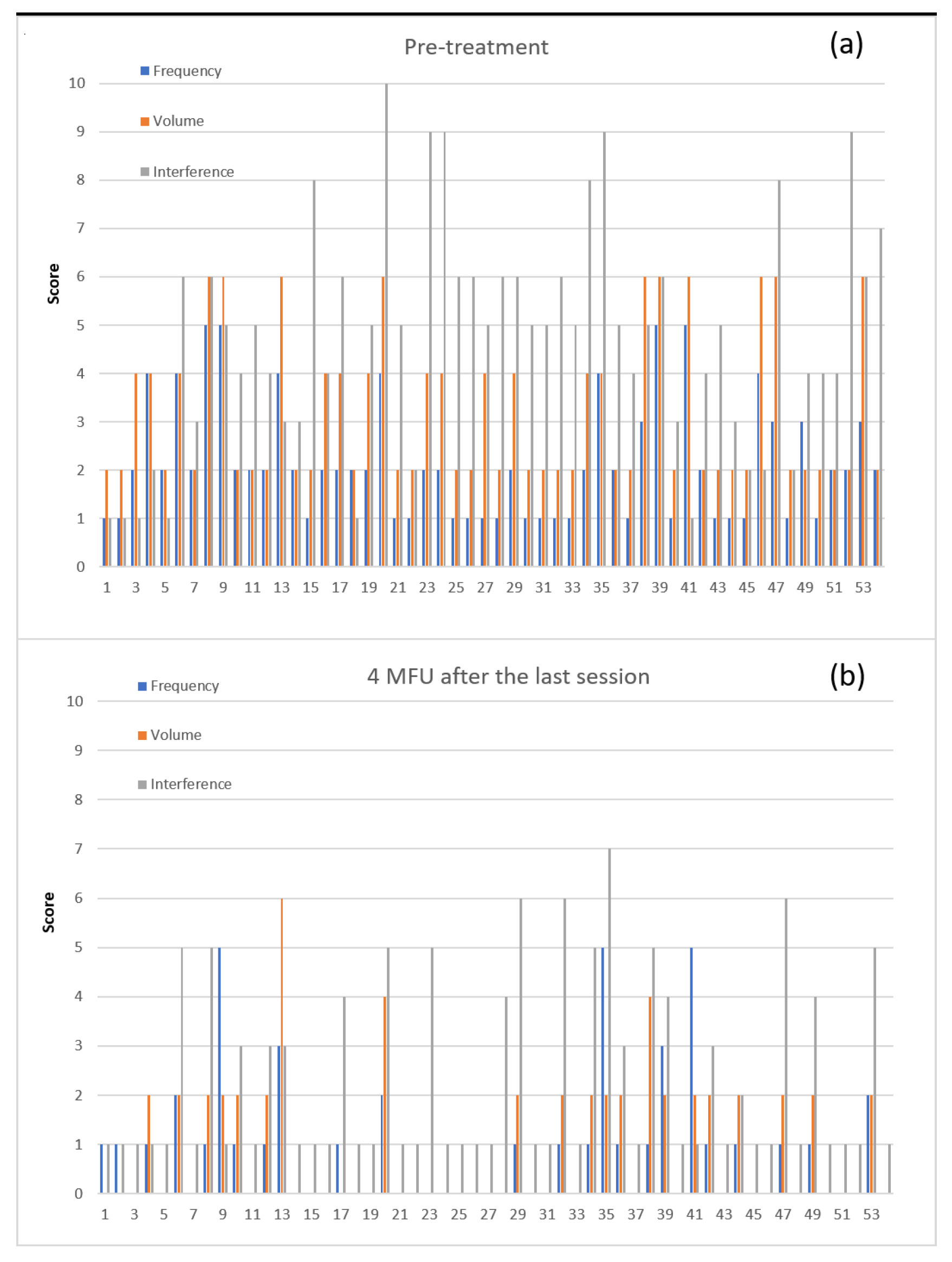
3. Results
4. Discussions
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
Appendix B

References
- Abrams, P.; Cardozo, L.; Fall, M.; Griffiths, D.; Rosier, P.; Ulmsten, U.; Kerrebroeck, P.V.; Victor, A.; Wein, A. The standardisation of terminology in lower urinary tract function: Report from the standardisation subcommittee of the International Continence Society. Urology 2003, 61, 37–49. [Google Scholar] [CrossRef]
- Milsom, I.; Gyhagen, M. The prevalence of urinary incontinence. Climacteric 2019, 22, 217–222. [Google Scholar] [CrossRef] [PubMed]
- Fleischmann, N.; Flisser, A.J.; Blaivas, J.G.; Panagopoulos, G. Sphincteric urinary incontinence: Relationship of vesical leak point pressure, urethral mobility and severity of incontinence. J. Urol. 2003, 169, 999–1002. [Google Scholar] [CrossRef] [PubMed]
- Petros, P. The integral system. Cent European. J. Urol. 2011, 64, 110–119. [Google Scholar] [CrossRef]
- Lapitan, M.C.; Cody, J.D. Open retropubic colposuspension for urinary incontinence in women. Cochrane Database Syst. Rev. 2012, 6, CD002912. [Google Scholar] [CrossRef]
- Fitzgerald, M.P.; Mollenhauer, J.; Hale, D.S.; Benson, J.T.; Brubaker, L. Urethral collagen morphologic characteristics among women with genuine stress incontinence. Am. J. Obstet. Gynecol. 2000, 182, 1565–1574. [Google Scholar] [CrossRef]
- Mohamed, L.E.; Sonal, C.; Angel, L.; Keyvan, N. Nonablative radiofrequency for skin rejuvenation. Dermatol. Surg. 2010, 36, 577–589. [Google Scholar] [CrossRef]
- Belenky, I.; Margulis, A.; Elman, M.; Bar-Yosef, U.; Paun, S.D. Exploring channeling optimized radiofrequency energy: A review of radiofrequency history and applications in esthetic fields. Adv. Ther. 2012, 29, 249–266. [Google Scholar] [CrossRef]
- David, J.; Goldberg, M.D. Nonablative Laser Technology Radiofrequency. Aesthet. Surg. J. 2004, 24, 180–181. [Google Scholar] [CrossRef]
- Dmochowski, R.R.; Avon, M.; Ross, J.; Cooper, J.M.; Kaplan, R.; Love, B.; Kohli, N.; Albala, D.; Shingleton, B. Transvaginal radio frequency treatment of the endopelvic fascia: A prospective eval-uation for the treatment of genuine stress urinary incontinence. J. Urol. 2003, 169, 1028–1032. [Google Scholar] [CrossRef]
- Appell, R.A.; Juma, S.; Wells, W.G.; Lenihan, J.P.; Klimberg, I.W.; Kanellos, A.; Reilley, S.F. Transurethral radiofrequency energy collagen micro-remodeling for the treatment of female stress urinary incontinence. Neurourol. Urodyn. 2006, 25, 331–336. [Google Scholar] [CrossRef] [PubMed]
- Elser, D.M.; Mitchell, G.K.; Miklos, J.R.; Nickell, K.G.; Cline, K.; Winkler, H.; Wells, W.G. Nonsurgical transurethral collagen denaturation for stress urinary incontinence in women 18-month results from a prospective long-term study. Neurourol. Urodyn. 2010, 29, 1424–1428. [Google Scholar] [CrossRef] [PubMed]
- Sand, P.K.; Owens, G.M.; Black, E.J.; Anderson, L.H.; Martinson, M.S. Cost effectiveness of radiofrequency microremodeling for stress urinary incontinence. Int. Urogynecol. J. 2014, 25, 517–523. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kang, D.; Han, J.; Neuberger, M.M.; Moy, M.L.; Wallace, S.A.; Alonso-Coello, P.; Dahm, P. Transurethral radiofrequency collagen dena-turation for the treatment of women with urinary inconti-nence. Cochrane Database Syst.Rev. 2015, 3, CD010217. [Google Scholar] [CrossRef]
- Abdelaziz, A.; Dell, J.; Karram, M. Transvaginal radiofrequency energy for the treatment of urinary stress incontinence: A comparison of monopolar and bipolar technologies in both pre- and post-menopausal patients. Neurourol. Urodyn. 2021, 40, 1804–1810. [Google Scholar] [CrossRef] [PubMed]
- González, I.P.; Rizo, D.V.; Garibay, I.; Galvan, R. The Role of Bipolar Radiofrequency (Bprf) as a Mechanism of Bio-Stimulation for the Treatment of Vulvo-Vaginal Laxity: A Novel Approach. International J. Clin. Exp. Med. Res. 2021, 5, 367–376. [Google Scholar] [CrossRef]
- Ibinaeva, I.S.; Apolikhina, I.A.; Makhmedzhanova, F.N.; Muslimova, S.Z. ICIQ-SF questionnaire in women with urinary inconti-nence. Urologiia 2012, 1, 38–42. [Google Scholar]
- Klovning, A.; Avery, K.; Sandvik, H.; Hunskaar, S. Comparison of two questionnaires for assessing the severity of urinary incon-tinence: The ICIQ-UI SF versus the incontinence severity index. Comp. Study Neurourol. Urodyn. 2009, 28, 411–415. [Google Scholar] [CrossRef]
- Kirchin, V.; Page, T.; Keegan, P.E.; Atiemo, K.O.; Cody, J.D.; McClinton, S.; Aluko, P. Urethral injection therapy for urinary incontinence in women. Rev. Cochrane Database Syst. Rev. 2017, 7, CD003881. [Google Scholar] [CrossRef]
- Cavkaytar, S.; Kokanali, M.K.; Topcu, H.O.; Aksakal, O.S.; Doğanay, M. Effect of home-based Kegel exercises on quality of life in women with stress and mixed urinary incontinence. J Obstet. Gynaecol. 2015, 35, 407–410. [Google Scholar] [CrossRef]
- Lamin, E.; Parrillo, L.M.; Newman, D.K.; Smith, A.L. Pelvic Floor Muscle Training: Underutilization in the USA. Curr. Urol. Rep. 2016, 17, 10. [Google Scholar] [CrossRef] [PubMed]
- Yount, S.M.; Fay, R.A.; Kissler, K.J. Prenatal and Postpartum Experience Knowledge, and Engagement with Kegels: A Longitudin al, Prospective, Multisite Study. J. Womens Health 2020, 30, 891–901. [Google Scholar] [CrossRef] [PubMed]
- Shobeiri, S.A.; Kerkhof, M.H.; Minassian, V.A.; Bazi, T. IUGA committee opinion: Laser based vaginal devices for treatment of stress urinary incontinence, genitourinary syndrome of menopause, and vaginal laxity. Int. Urogynecol. J. 2019, 30, 371–376. [Google Scholar] [CrossRef] [PubMed]
- González, P.I.; Jaguszewska, K.; Cardona, J.L.; Lukaszuk, M. Long-term effect of thermo ablative fractional CO2 laser treatment as a novel approach to urinary incontinence management in women with genitourinary syndrome of menopause. Int. Uro. Gynecol. J. 2018, 29, 211–215. [Google Scholar] [CrossRef]
- Conté, C.; Jauffret, T.; Vieillefosse, S.; Hermieu, J.F.; Deffieux, X. Laser procedure for female urinary stress incontinence: A review of the literature. Prog. Urol. 2017, 27, 1076–1083. [Google Scholar] [CrossRef]
- Franić, D.; Fistonić, I. Laser Therapy in the Treatment of Female Urinary Incontinence and Genitourinary Syndrome of Meno-pause: An Update. BioMed Res. Int. 2019, 2019, 1576359. [Google Scholar] [CrossRef]
- Hashim, P.W.; Nia, J.K.; Zade, J.; Farberg, A.S.; Goldenberg, G. Noninvasive vaginal rejuvenation. Cutis 2018, 102, 243–246. [Google Scholar]
- Bergsland, J. Major innovations and trends in the medical device sector. Acta Inform. Med. 2012, 20, 44–46. [Google Scholar] [CrossRef]
- Millheiser, L.S.; Pauls, R.N.; Herbst, S.J.; Chen, B.H. Radiofrequency treatment of vaginal laxity after vaginal delivery: Nonsurgical vaginal tightening. Clin. Trial J. Sex. Med. 2010, 7, 3088–3095. [Google Scholar] [CrossRef]
- Sekiguchi, Y.; Utsugisawa, Y.; Azekosi, Y.; Kinjo, M.; Song, M.; Kubota, Y.; Kingsberg, S.A.; Krychman, M.L. Laxity of the vaginal in-troitus after childbirth: Nonsurgical outpatient procedure for vaginal tissue restoration and improved sexual satisfaction using low-energy radiofrequency thermal therapy. J. Womens Health 2013, 22, 775–781. [Google Scholar] [CrossRef]
- Alinsod, R.M. Transcutaneous temperature controlled radiofrequency for orgasmic dysfunction. Clin. Trial Lasers Surg. Med. 2016, 48, 641–645. [Google Scholar] [CrossRef] [PubMed]
- Dillon, B.; Dmochowski, R. Radiofrequency for the treatment of stress urinary incontinence in women. Rev. Curr. Urol. Rep. 2009, 5, 369–374. [Google Scholar] [CrossRef] [PubMed]
- Appell, R.A.; Davila, G.W. Treatment options for patients with suboptimal response to surgery for stress urinary incontinence. Curr. Med. Res. Opin. 2007, 23, 285–292. [Google Scholar] [CrossRef] [PubMed]
- Dayan, E.; Ramirez, H.; Theodorou, S. Radiofrequency Treatment of Labia Minora and Majora: A Minimally Invasive Approach to Vulva Restoration. Plast Reconstr. Surg. Glob. Open 2020, 22, e2418. [Google Scholar] [CrossRef]
- Magon, N.; Alinsod, R. ThermiVa: The Revolutionary Technology for Vulvovaginal Rejuvenation and Noninvasive Management of Female SUI. J. Obstet. Gynaecol. 2016, 66, 300–302. [Google Scholar] [CrossRef][Green Version]
- Gonzalez, P.I.; Velez Rizo, D.L. Vaginal bipolar radiofrequency as non-surgical treatment of stress urinary incontinence: Case series study. J. Biol. Regul. Homeost. Agents 2021, 35, 271–274. [Google Scholar] [CrossRef]
- Hantash, B.M.; Ubeid, A.A.; Chang, H.; Kafi, R.; Renton, B. Bipolar fractional radiofrequency treatment induces neoelastogenesis and neocollagenesis. Control. Clin. Trial Lasers Surg. Med. 2009, 41, 1–9. [Google Scholar] [CrossRef]
- Traish, A.M.; Kang, H.P.; Saad, F.; Guay, A.T. Dehydroepiandrosterone (DHEA)-a precursor steroid or an active hormone in hu-man physiology. Rev. J. Sex Med. 2011, 8, 2960–2982. [Google Scholar] [CrossRef]
- Preminger, B.A.; Kurtzman, J.S.; Dayan, E. A Systematic Review of Nonsurgical Vulvovaginal Restoration Devices: An Evi-dence-Based Examination of Safety and Efficacy. Plast. Reconstr. Surg. 2020, 146, 552e–564e. [Google Scholar] [CrossRef]
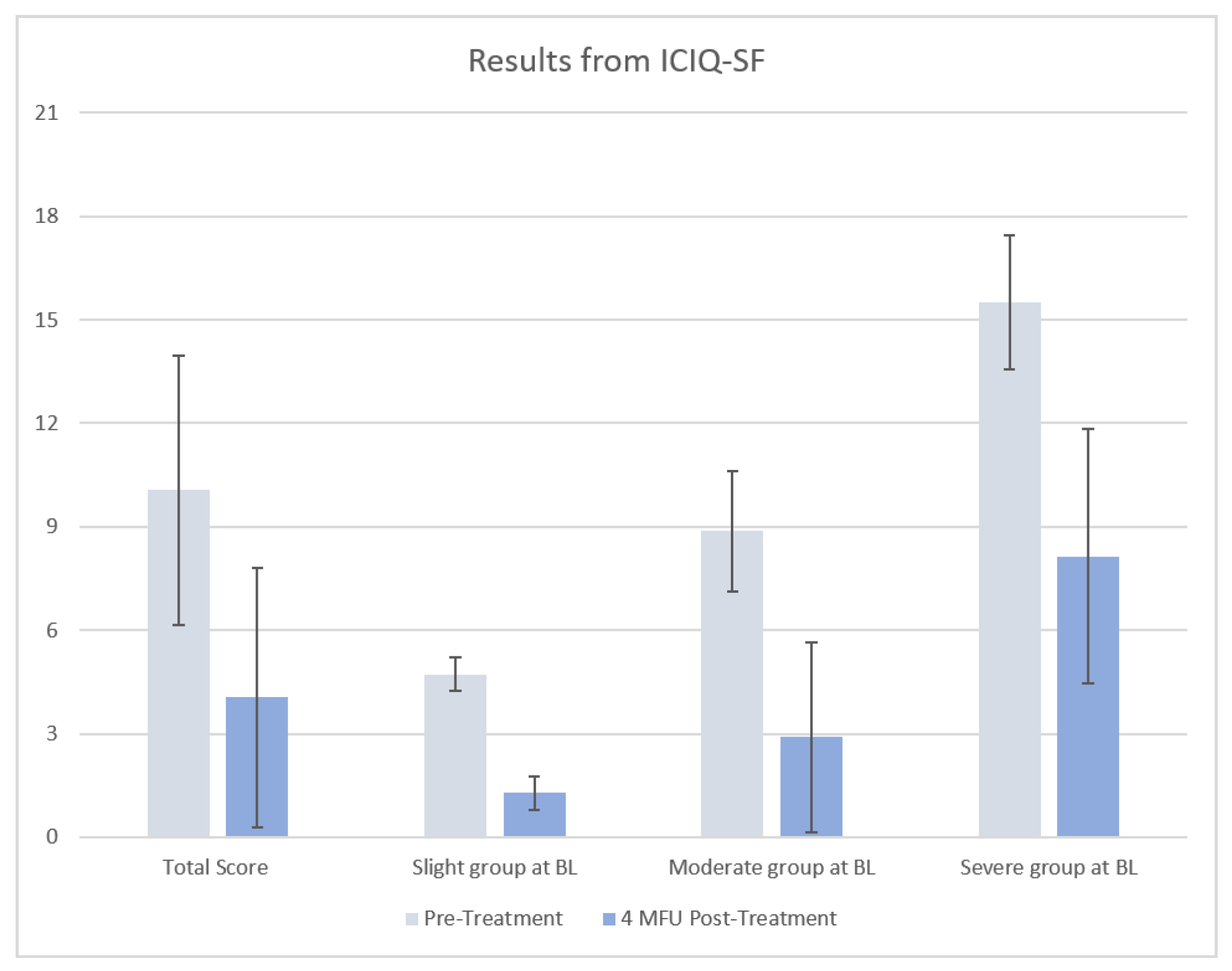
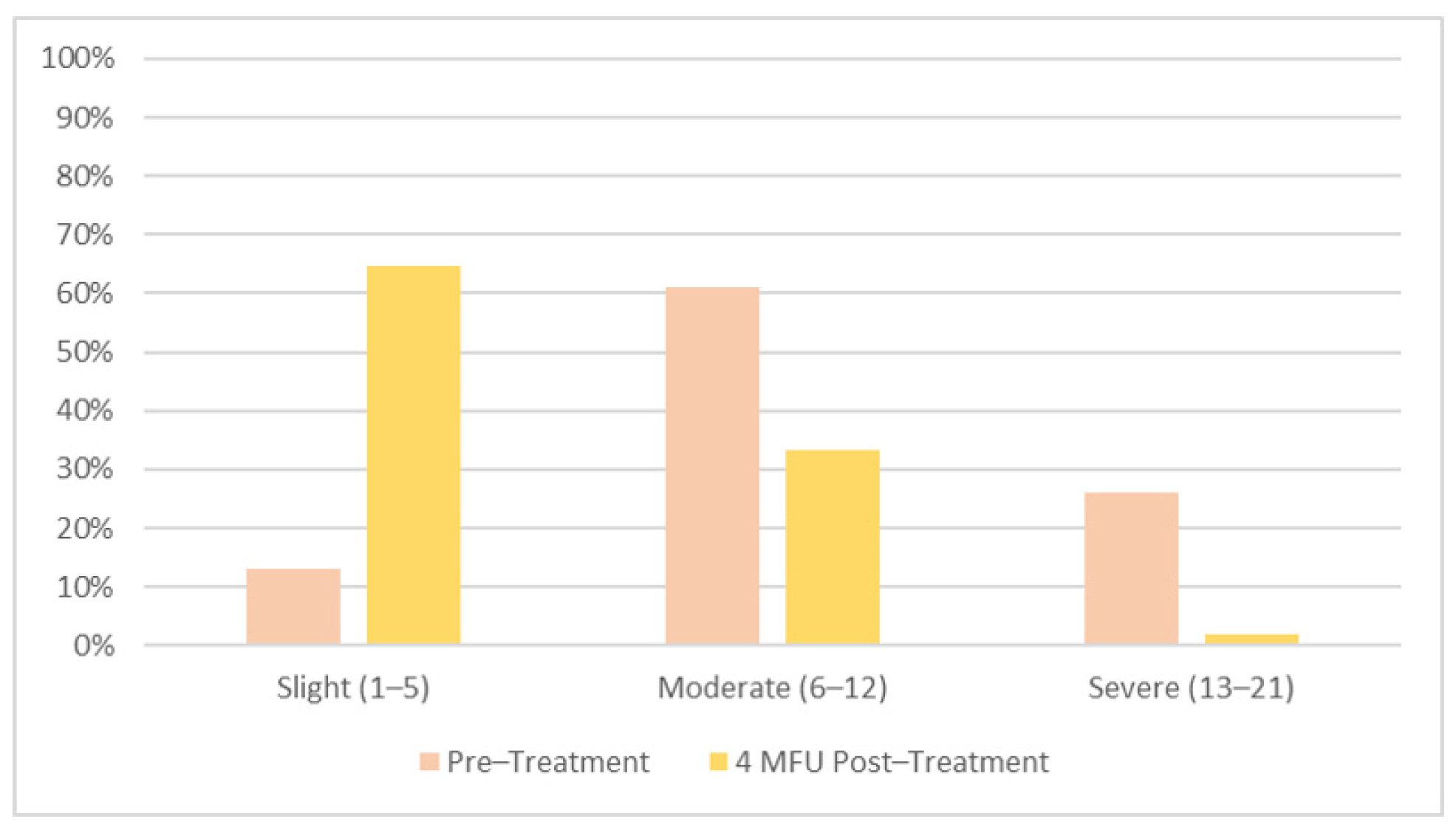
| Questionnaire ICIQ-SF | Score Range | Pre-Treatment | Post-Treatment | p-Value |
|---|---|---|---|---|
| Frequency | 0–5 | 2.1 ± 1.3 | 0.8 ±1.3 | p < 0.0001 |
| Volume | 0–6 | 3.2 ± 1.6 | 0.9 ± 1.4 | p < 0.0001 |
| Interference | 1–10 | 4.7 ± 2.4 | 2.3 ± 1.9 | p < 0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mezzana, P.; Garibay, I.; Fusco, I. Vaginal Bipolar Radiofrequency Treatment of Mild SUI: A Pilot Retrospective Study. Medicina 2022, 58, 181. https://doi.org/10.3390/medicina58020181
Mezzana P, Garibay I, Fusco I. Vaginal Bipolar Radiofrequency Treatment of Mild SUI: A Pilot Retrospective Study. Medicina. 2022; 58(2):181. https://doi.org/10.3390/medicina58020181
Chicago/Turabian StyleMezzana, Paolo, Ignacio Garibay, and Irene Fusco. 2022. "Vaginal Bipolar Radiofrequency Treatment of Mild SUI: A Pilot Retrospective Study" Medicina 58, no. 2: 181. https://doi.org/10.3390/medicina58020181
APA StyleMezzana, P., Garibay, I., & Fusco, I. (2022). Vaginal Bipolar Radiofrequency Treatment of Mild SUI: A Pilot Retrospective Study. Medicina, 58(2), 181. https://doi.org/10.3390/medicina58020181






