SARS-CoV-2 Reinfection among Healthcare Workers in Mexico: Case Report and Literature Review
Abstract
1. Introduction
2. Methods
3. Case Reports
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Suárez, V.; Suarez Quezada, M.; Oros Ruiz, S.; Ronquillo De Jesús, E. Epidemiología de COVID-19 en México: Del 27 de febrero al 30 de abril de 2020. Rev. Clín. Esp. 2020, 220, 463–471. [Google Scholar] [CrossRef]
- Centro de Produccion CEPROPIE. Informe Diario Sobre Coronavirus COVID-19 en México. Secretaría de Salud. Martes 23 de Marzo [Internet]. 2021. Available online: https://www.youtube.com/watch?v=t4UraPe7bZc&ab_channel=CENTRODEPRODUCCIONCEPROPIE (accessed on 23 March 2021).
- CSSEGISandData. CSSEGISandData/COVID-19 [Internet]. 2021. Available online: https://github.com/CSSEGISandData/COVID-19 (accessed on 7 March 2021).
- Mehta, S.; Machado, F.; Kwizera, A.; Papazian, L.; Moss, M.; Azoulay, É.; Herridge, M. COVID-19: A heavy toll on health-care workers. Lancet Respir. Med. 2021, 9, 226–228. [Google Scholar] [CrossRef]
- Bandyopadhyay, S.; Baticulon, R.E.; Kadhum, M.; Alser, M.; Ojuka, D.K.; Badereddin, Y.; Kamath, A.; Parepalli, S.A.; Brown, G.; Iharchane, S.; et al. Infection and mortality of healthcare workers worldwide from COVID-19: A systematic review. BMJ Glob. Health 2020, 5, e003097. [Google Scholar] [CrossRef]
- Demos, E.; Martínez, Á.C. La Jornada—Enfermaron de Covid 195,558 Trabajadores de Salud en México [Internet]. Available online: https://www.jornada.com.mx (accessed on 15 March 2021).
- Agren, D. Understanding Mexican health worker COVID-19 deaths. Lancet 2020, 396, 807. [Google Scholar] [CrossRef]
- van Kampen, J.J.; van de Vijver, D.A.; Fraaij, P.L.; Haagmans, B.L.; Lamers, M.M.; Okba, N.; van den Akker, J.P.; Endeman, H.; Gommers, D.A.; Cornelissen, J.J.; et al. Duration and key determinants of infectious virus shedding in hospitalized patients with coronavirus disease-2019 (COVID-19). Nat. Commun. 2021, 12, 267. [Google Scholar] [CrossRef]
- Tomassini, S.; Kotecha, D.; Bird, P.W.; Folwell, A.; Biju, S.; Tang, J.W. Setting the criteria for SARS-CoV-2 reinfection—Six possible cases. J. Infect. 2021, 82, 282–287. [Google Scholar] [CrossRef]
- Yahav, D.; Yelin, D.; Eckerle, I.; Eberhardt, C.S.; Wang, J.; Cao, B.; Kaiser, L. Definitions for COVID-19 reinfection, relapse and PCR re-positivity. Clin. Microbiol. Infect. 2021, 27, 315–318. [Google Scholar] [CrossRef] [PubMed]
- Chen, D.; Xu, W.; Lei, Z.; Huang, Z.; Liu, J.; Gao, Z.; Peng, L. Recurrence of positive SARS-CoV-2 RNA in COVID-19: A case report. Int. J. Infect. Dis. 2020, 93, 297–299. [Google Scholar] [CrossRef] [PubMed]
- Ye, G.; Pan, Z.; Pan, Y.; Deng, Q.; Chen, L.; Li, J.; Li, Y.; Wang, X. Clinical characteristics of severe acute respiratory syndrome coronavirus 2 reactivation. J. Infect. 2020, 80, e14–e17. [Google Scholar] [CrossRef] [PubMed]
- Osman, A.A.; Al Daajani, M.M.; Alsahafi, A.J. Re-positive coronavirus disease 2019 PCR test: Could it be a reinfection? New Microbes New Infect. 2020, 37, 100748. [Google Scholar] [CrossRef]
- Li, J.; Zhang, L.; Liu, B.; Song, D. Case Report: Viral Shedding for 60 Days in a Woman with COVID-19. Am. J. Trop. Med. Hyg. 2020, 102, 1210–1213. [Google Scholar] [CrossRef]
- de Brito, C.A.A.; Lima, P.M.A.; de Brito, M.C.M.; de Oliveira, D.B. Second Episode of COVID-19 in Health Professionals: Report of Two Cases. Int. Med. Case Rep. J. 2020, 13, 471–475. [Google Scholar] [CrossRef]
- Ravioli, S.; Ochsner, H.; Lindner, G. Reactivation of COVID-19 pneumonia: A report of two cases. J. Infect. 2020, 81, e72–e73. [Google Scholar] [CrossRef] [PubMed]
- Popovici, J.; Pierce-Friedrich, L.; Kim, S.; Bin, S.; Run, V.; Lek, D.; Hee, K.H.D.; Lee Soon-U, L.; Cannon, M.V.; Serre, D.; et al. Recrudescence, Reinfection, or Relapse? A More Rigorous Framework to Assess Chloroquine Efficacy for Plasmodium vivax Malaria. J. Infect. Dis. 2019, 219, 315–322. [Google Scholar] [CrossRef]
- Gousseff, M.; Penot, P.; Gallay, L.; Batisse, D.; Benech, N.; Bouiller, K.; Collarino, R.; Conrad, A.; Slama, D.; Joseph, C.; et al. Clinical recurrences of COVID-19 symptoms after recovery: Viral relapse, reinfection or inflammatory rebound? J. Infect. 2020, 81, 816–846. [Google Scholar] [CrossRef] [PubMed]
- Korber, B.; Fischer, W.M.; Gnanakaran, S.; Yoon, H.; Theiler, J.; Abfalterer, W.; Hengartner, N.; Giorgi, E.E.; Bhattacharya, T.; Foley, B.; et al. Tracking Changes in SARS-CoV-2 Spike: Evidence that D614G Increases Infectivity of the COVID-19 Virus. Cell 2020, 182, 812–827. [Google Scholar] [CrossRef] [PubMed]
- Iwasaki, A. What reinfections mean for COVID-19. Lancet Infect. Dis. 2021, 21, 3–5. [Google Scholar] [CrossRef]
- To, K.K.W.; Hung, I.F.N.; Ip, J.D.; Chu, A.W.H.; Chan, W.M.; Tam, A.R.; Fong, C.H.Y.; Yuan, S.; Tsoi, H.W.; Ng, A.C.K.; et al. Coronavirus Disease 2019 (COVID-19) Re-infection by a Phylogenetically Distinct Severe Acute Respiratory Syndrome Coronavirus 2 Strain Confirmed by Whole Genome Sequencing. Clin. Infect. Dis. 2020. [Google Scholar] [CrossRef]
- Van Elslande, J.; Vermeersch, P.; Vandervoort, K.; Wawina-Bokalanga, T.; Vanmechelen, B.; Wollants, E.; Laenen, L.; André, E.; Van Ranst, M.; Lagrou, K.; et al. Symptomatic Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Reinfection by a Phylogenetically Distinct Strain. Clin. Infect. Dis. 2020. [Google Scholar] [CrossRef]
- Tillett, R.L.; Sevinsky, J.R.; Hartley, P.D.; Kerwin, H.; Crawford, N.; Gorzalski, A.; Laverdure, C.; Verma, S.C.; Rossetto, C.C.; Jackson, D.; et al. Genomic evidence for reinfection with SARS-CoV-2: A case study. Lancet Infect. Dis. 2021, 21, 52–58. [Google Scholar] [CrossRef]
- Prado-Vivar, B.; Becerra-Wong, M.; Guadalupe, J.J.; Marquez, S.; Gutierrez, B.; Rojas-Silva, P.; Grunauer, M.; Trueba, G.; Barragan, V.; Cardenas, P. COVID-19 Re-Infection by a Phylogenetically Distinct SARS-CoV-2 Variant, First Confirmed Event in South America. SSRN J. 2020. Available online: https://www.ssrn.com/abstract=3686174 (accessed on 21 April 2021). [CrossRef]
- Greaney, A.J.; Loes, A.N.; Crawford, K.H.D.; Starr, T.N.; Malone, K.D.; Chu, H.Y.; Bloom, J.D. Comprehensive mapping of mutations in the SARS-CoV-2 receptor-binding domain that affect recognition by polyclonal human plasma antibodies. Cell Host Microbe. 2021, 29, 463–476.e6. [Google Scholar] [CrossRef]
- Sabino, E.C.; Buss, L.F.; Carvalho, M.P.; Prete, C.A.; Crispim, M.A.; Fraiji, N.A.; Pereira, R.H.; Parag, K.V.; da Silva Peixoto, P.; Kraemer, M.U.; et al. Resurgence of COVID-19 in Manaus, Brazil, despite high seroprevalence. Lancet 2021, 397, 452–455. [Google Scholar] [CrossRef]
- Ringlander, J.; Nilsson, S.; Westin, J.; Lindh, M.; Martner, A.; Hellstrand, K. Low Incidence of Reinfection With Endemic Coronaviruses Diagnosed by Real-Time PCR. J. Infect. Dis. 2020. [Google Scholar] [CrossRef] [PubMed]
- Taboada, B.; Vazquez-Perez, J.A.; Muñoz-Medina, J.E.; Ramos-Cervantes, P.; Escalera-Zamudio, M.; Boukadida, C.; Sanchez-Flores, A.; Isa, P.; Mendieta-Condado, E.; Martínez-Orozco, J.A.; et al. Genomic Analysis of Early SARS-CoV-2 Variants Introduced in Mexico. J. Virol. 2020, 94, e01056-20. [Google Scholar] [CrossRef]
- Goldman, J.; Wang, K.; Röltgen, K.; Nielsen, S.; Roach, J.; Naccache, S.; Yang, F.; Wirz, O.; Yost, K.; Lee, J.; et al. Reinfection with SARS-CoV-2 and Failure of Humoral Immunity: A case report. MedRxiv 2020. [Google Scholar] [CrossRef]
- Kellam, P.; Barclay, W. The dynamics of humoral immune responses following SARS-CoV-2 infection and the potential for reinfection. J. Gen. Virol. 2020, 101, 791–797. [Google Scholar] [CrossRef] [PubMed]
- Bonifácio, L.P.; Pereira, A.P.S.; Balbão, V.D.M.P.; Fonseca, B.A.L.D.; Passos, A.D.C.; Bellissimo-Rodrigues, F. Are SARS-CoV-2 reinfection and Covid-19 recurrence possible? A case report from Brazil. Rev. Soc. Bras. Med. Trop. 2020, 53, e20200619. [Google Scholar] [CrossRef]
- Alizargar, J. Risk of reactivation or reinfection of novel coronavirus (COVID-19). J. Formos. Med. Assoc. 2020, 119, 1123. [Google Scholar] [CrossRef]
- Ibarrondo, F.J.; Fulcher, J.A.; Goodman-Meza, D.; Elliott, J.; Hofmann, C.; Hausner, M.A.; Ferbas, K.G.; Tobin, N.H.; Aldrovandi, G.M.; Yang, O.O. Rapid Decay of Anti–SARS-CoV-2 Antibodies in Persons with Mild Covid-19. N. Engl. J. Med. 2020, 383, 1085–1087. [Google Scholar] [CrossRef]
- Channappanavar, R.; Fett, C.; Zhao, J.; Meyerholz, D.K.; Perlman, S. Virus-Specific Memory CD8 T Cells Provide Substantial Protection from Lethal Severe Acute Respiratory Syndrome Coronavirus Infection. J. Virol. 2014, 88, 11034–11044. [Google Scholar] [CrossRef]
- Orientaciones Provisionales para la Detección de Casos de Reinfección por SARS-CoV-2—OPS/OMS|Organización Panamericana de la Salud [Internet]. Available online: https://www.paho.org/es/documentos/orientaciones-provisionales-para-deteccion-casos-reinfeccion-por-sars-cov-2 (accessed on 8 March 2021).
- Ledford, H. Coronavirus reinfections: Three questions scientists are asking. Nature 2020, 585, 168–169. [Google Scholar] [CrossRef]
- Lafaie, L.; Célarier, T.; Goethals, L.; Pozzetto, B.; Grange, S.; Ojardias, E.; Annweiler, C. Recurrence or Relapse of COVID-19 in Older Patients: A Description of Three Cases. J. Am. Geriatr. Soc. 2020, 68, 2179–2183. [Google Scholar] [CrossRef]
- Arafkas, M.; Khosrawipour, T.; Kocbach, P.; Zielinski, K.; Schubert, J.; Mikolajczyk, A.; Celinska, M.; Khosrawipour, V. Current meta-analysis does not support the possibility of COVID-19 reinfections. J. Med. Virol. 2021, 93, 1599–1604. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Xiao, J.; Sun, R.; Tang, X.; Liang, C.; Lin, H.; Zeng, L.; Hu, J.; Yuan, R.; Zhou, P.; et al. Prolonged Persistence of SARS-CoV-2 RNA in Body Fluids. Emerg. Infect. Dis. 2020, 26, 1834–1838. [Google Scholar] [CrossRef] [PubMed]
- Alvarez-Moreno, C.A.; Rodríguez-Morales, A.J. Testing Dilemmas: Post negative, positive SARS-CoV-2 RT-PCR—Is it a reinfection? Travel Med. Infect. Dis. 2020, 35, 101743. [Google Scholar] [CrossRef]
- Malkov, E. Simulation of coronavirus disease 2019 (COVID-19) scenarios with possibility of reinfection. Chaos Solitons Fractals 2020, 139, 110296. [Google Scholar] [CrossRef] [PubMed]
- Duggan, N.M.; Ludy, S.M.; Shannon, B.C.; Reisner, A.T.; Wilcox, S.R. Is novel coronavirus 2019 reinfection possible? Interpreting dynamic SARS-CoV-2 test results. Am. J. Emerg. Med. 2021, 39, e256.e1–e256.e3. [Google Scholar] [CrossRef] [PubMed]
- Roy, S. COVID-19 Reinfection: Myth or Truth? SN Compr. Clin. Med. 2020, 2, 710–713. [Google Scholar] [CrossRef]
- Chaturvedi, R.; Naidu, R.; Sheth, S.; Chakravarthy, K. Efficacy of Serology Testing in Predicting Reinfection in Patients with SARS-CoV-2. Disaster Med. Public Health Prep. 2020, 1–3. [Google Scholar] [CrossRef] [PubMed]
| Case 1 | Case 2 | Case 3 | Case 4 | |||||
|---|---|---|---|---|---|---|---|---|
| Age in years | 40 | 49 | 53 | 52 | ||||
| Gender | Female | Female | Male | Male | ||||
| Occupation | Nurse | Nurse | Pharmacy assistant | Internist | ||||
| Comorbidities | Yes | No | No | |||||
| First Infection | Second Infection | First Infection | Second Infection | First Infection | Second Infection | First Infection | Second Infection | |
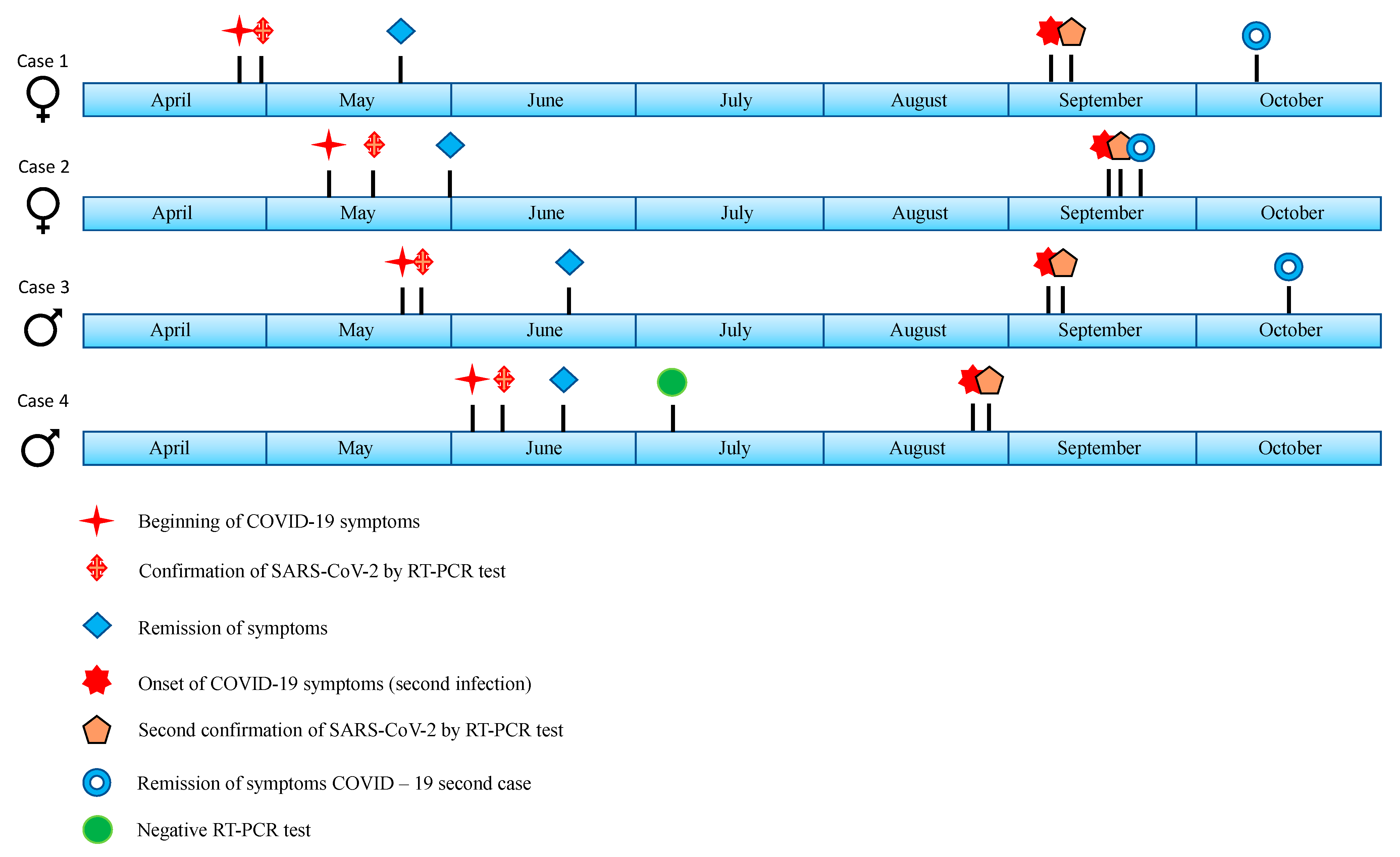
| Onset of symptoms | 26 April 2020 | 07 September 2020 | 10 May 2020 | 16 September 2020 | 22 May 2020 | 06 September 2020 | 03 June 2020 | 24 August 2020 |
| Symptom remission | 22 May 2020 | 10 October 2020 | 30 May 2020 | 21 September 2020 | 20 June 2020 | 15 October 2020 | 18 June 2020 | 17 November 2020 |
| Time between the onset of the first and second infection | 134 days | 129 days | 107 days | 82 days | ||||
| Time between remission of first infection and onset of second infection | 108 days | 109 days | 78 days | 67 days | ||||
| Symptoms | ||||||||
| Fever | Yes | Yes | Yes | Yes | ||||
| Dry cough | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| Headache | Yes | Yes | Yes | Yes | ||||
| Rhinorrhea | Yes | Yes | Yes | |||||
| General malaise | Yes | Yes | Yes | Yes | Yes | |||
| Anosmia | Yes | Yes | Yes | |||||
| Chills | Yes | Yes | ||||||
| Odynophagia | Yes | Yes | Yes | |||||
| Dyspnea | Minimum efforts | Medium efforts | Medium efforts | Medium efforts | Minimum efforts | |||
| Myalgia | Yes | Yes | Yes | Yes | Yes | |||
| Arthralgia | Yes | Yes | Yes | Yes | Yes | |||
| Decrease in oxygen saturation | Yes | Yes | Yes | |||||
| Exanthema | Maculopapular on upper and lower limbs, thorax, face and neck | Diffuse fine maculopapular | ||||||
| Dysgeusia | Yes | Yes | Yes | |||||
| Treatment | Paracetamol, nebulizations with budesonide plus ipratropium bromide, salmetol/fluticasone, salbutamol spray, loratadine. | Paracetamol, Salmeterol/ fluticasone, salbutamol spray, montelukast. | Paracetamol y azithromycin. | Budesonide/ formoterol and paracetamol. | Azithromycin, oseltamivir, paracetamol, prednisone, hydroxychloroquinine. | Azithromycin, ivermectin, paracetamol, benzonatate beads, prednisone, indomethacin, beclomethasone spray. | Lopinavir/ritonavir, dexamethasone, azithromycin. | Tocilizumab, linezolid, piperacillin/ tazobactam, enoxaparin, methylprednisolone, dexmedetomidine. |
| Pneumonia on the second event identified by imaging. | Yes | Yes | ||||||
| Supplemental oxygen requirement | Yes | Yes | Yes | |||||
| Hospital stay | Yes | Yes | ||||||
| Intensive care unit (ICU) stay | Yes | |||||||
| Assisted mechanical ventilation | Yes (11 days) | |||||||
| Clinical course | Exacerbation/Improvement | Discharged/Pulmonary sequela with postinfectious bullae | Improvement | Improvement | Improvement | Improvement | Improvement | Bilateral interstitial pneumonia/Improvement |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Garduño-Orbe, B.; Sánchez-Rebolledo, J.M.; Cortés-Rafael, M.; García-Jiménez, Y.; Perez-Ortiz, M.; Mendiola-Pastrana, I.R.; López-Ortiz, E.; López-Ortiz, G. SARS-CoV-2 Reinfection among Healthcare Workers in Mexico: Case Report and Literature Review. Medicina 2021, 57, 442. https://doi.org/10.3390/medicina57050442
Garduño-Orbe B, Sánchez-Rebolledo JM, Cortés-Rafael M, García-Jiménez Y, Perez-Ortiz M, Mendiola-Pastrana IR, López-Ortiz E, López-Ortiz G. SARS-CoV-2 Reinfection among Healthcare Workers in Mexico: Case Report and Literature Review. Medicina. 2021; 57(5):442. https://doi.org/10.3390/medicina57050442
Chicago/Turabian StyleGarduño-Orbe, Brenda, Juan Manuel Sánchez-Rebolledo, Mustafá Cortés-Rafael, Yuliana García-Jiménez, Marcelina Perez-Ortiz, Indira Rocío Mendiola-Pastrana, Eduardo López-Ortiz, and Geovani López-Ortiz. 2021. "SARS-CoV-2 Reinfection among Healthcare Workers in Mexico: Case Report and Literature Review" Medicina 57, no. 5: 442. https://doi.org/10.3390/medicina57050442
APA StyleGarduño-Orbe, B., Sánchez-Rebolledo, J. M., Cortés-Rafael, M., García-Jiménez, Y., Perez-Ortiz, M., Mendiola-Pastrana, I. R., López-Ortiz, E., & López-Ortiz, G. (2021). SARS-CoV-2 Reinfection among Healthcare Workers in Mexico: Case Report and Literature Review. Medicina, 57(5), 442. https://doi.org/10.3390/medicina57050442






