Cesarean Scar Ectopic Pregnancy—Case Series: Treatment Decision Algorithm and Success with Medical Treatment
Abstract
1. Background
2. Case Report
3. Discussion
3.1. Pathogenesis
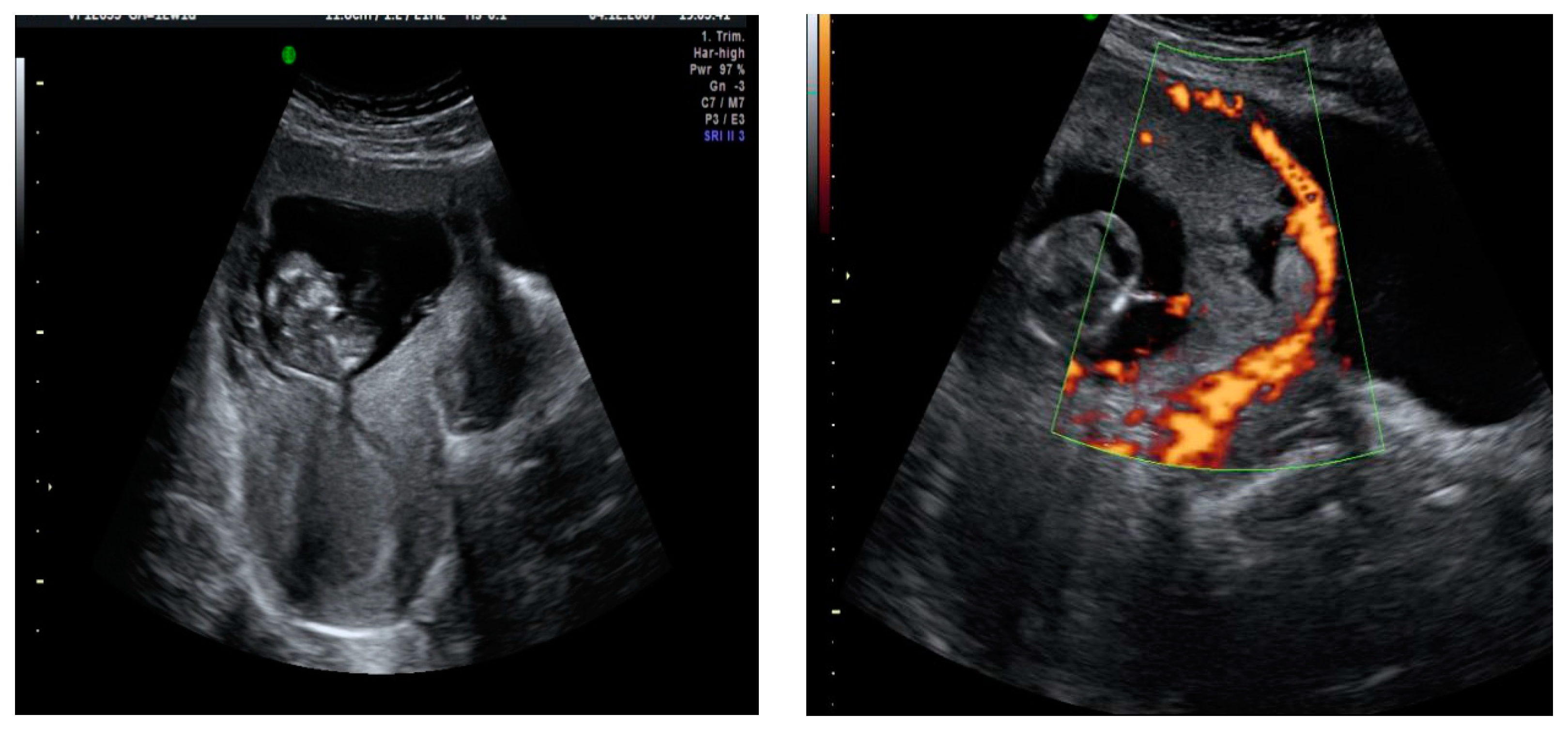
3.2. Diagnosis of CSEP
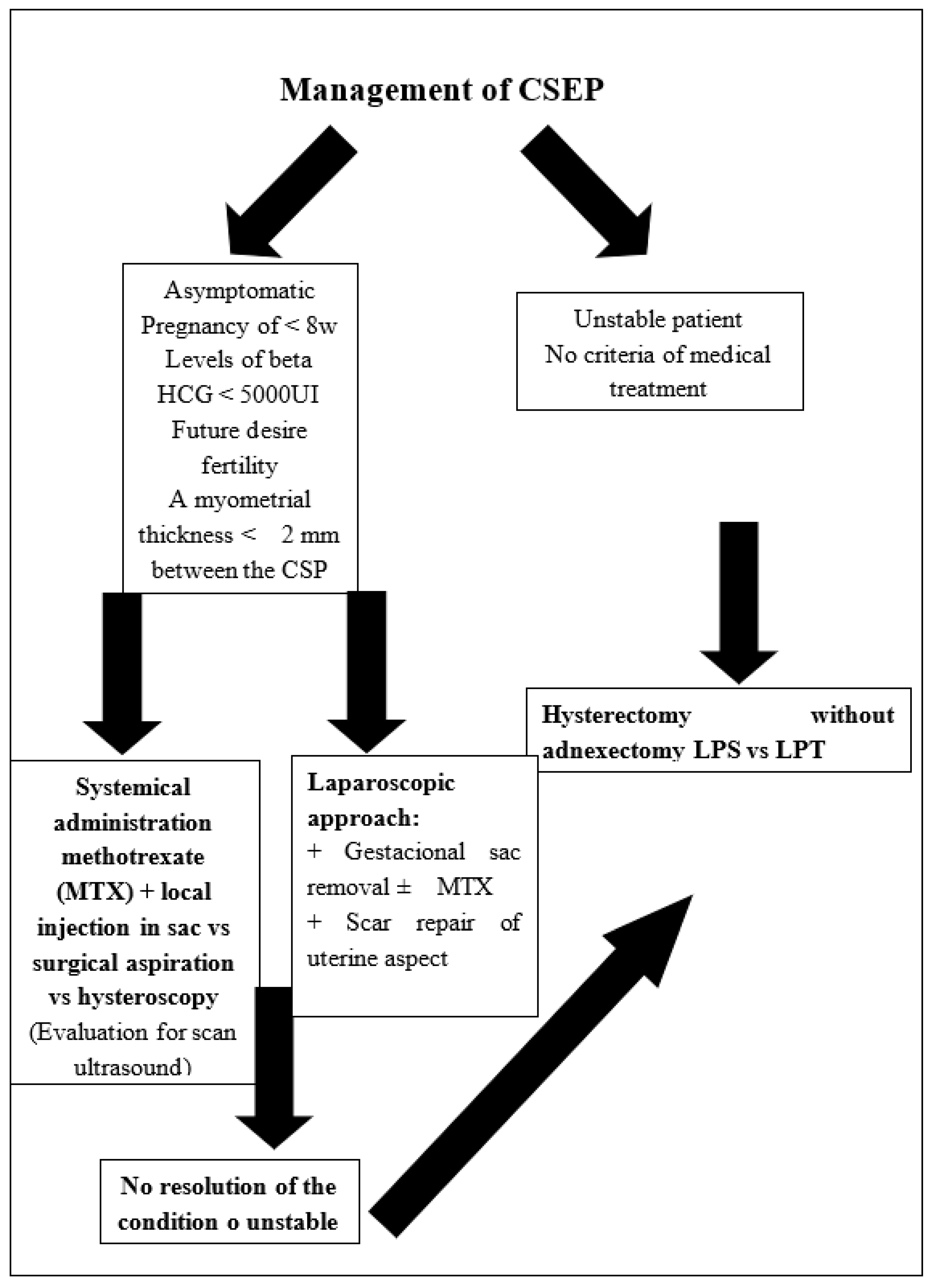
3.3. Treatment Options
3.3.1. Medical Treatment or Combined
3.3.2. Uterine Artery Embolization (UAE)
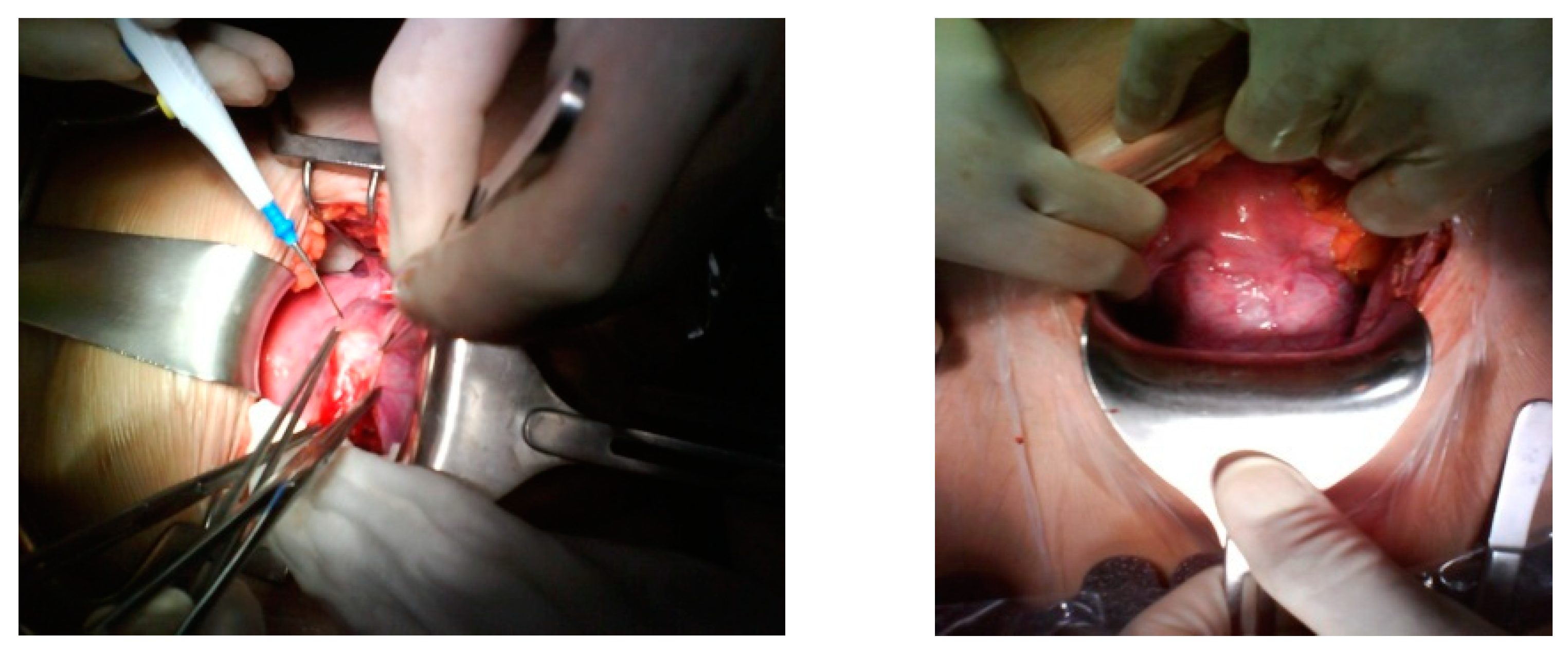
3.3.3. Surgical
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CS | Cesarean scar |
| CSEP | Cesarean scar ectopic pregnancy |
| CSP | Cesarean scar pregnancy |
| β-hCG | BetahCG |
| UI | International units |
| L | Liters |
| UAE | Uterine artery embolization |
| MTX | Methotrexate |
References
- ACOG Committee on Practice Bulletins Tubal ectopic pregnancy: ACOG practice bulletin. Clin. Manag. Guidel. Obs. Gynecol. 2018, 131, e91–e103.
- Fylstra, D.L. Ectopic pregnancy not within the (distal) fallopian tube: Etiology, diagnosis, and treatment. Am. J. Obs. Gynecol. 2012, 206, 289–299. [Google Scholar] [CrossRef] [PubMed]
- Rosen, T. Placenta accreta and cesarean scar pregnancy: Overlooked costs of the rising cesarean section rate. Clin. Perin. 2008, 35, 519–529. [Google Scholar] [CrossRef] [PubMed]
- Cömert, E.H.; Şal, H.; Ekici, Y.S.; Seda, E.; Guven, G. Cesarean scar pregnancy: A case report. Turk. Klin. Jinekoloji Obstet. 2018, 26, 37–39. [Google Scholar] [CrossRef][Green Version]
- Patel, M.A. Scar ectopic pregnancy. J. Med. Biol. Eng. 2015, 65, 372–375. [Google Scholar] [CrossRef] [PubMed]
- Rotas, M.A.; Haberman, S.; Levgur, M. Cesarean scar ectopic pregnancies etiology. Am. Coll. Obstet. Gynecol. 2006, 107, 1373–1381. [Google Scholar] [CrossRef] [PubMed]
- Zalduegui, M.M.; Ferreiro, S.I.; Vélez, A.R.; Monje Beltrán, M.L.; Vicedo Madrazo, E.M.; Martínez Portillo, R.J.; Llobet Roma, M.; Marqueta Sánchez, M. Cesarean scar ectopic pregnancy, a life threatening condition: A case report. Clin. Exp. Obstet. Gyn. 2019, 46, 313–316. [Google Scholar]
- Ash, A.; Smith, A.; Maxwell, D. Caesarean scar pregnancy. BJOG 2007, 114, 253–263. [Google Scholar] [CrossRef] [PubMed]
- Vial, Y.; Petignat, P.; Hohlfeld, P. Pregnancy in a cesarean scar. Ultrasound Obstet. Gynecol. 2000, 16, 592–593. [Google Scholar] [CrossRef]
- Hoffman, T.; Lin, J. Cesarean Scar Ectopic Pregnancy: Diagnosis With Ultrasound. Clin. Pract. Cases Emerg. Med. 2020, 4, 65–68. [Google Scholar] [CrossRef] [PubMed]
- Timor-Tritsch, I.E.; Monteagudo, A.; Cali, G.; El Refaey, H.; Kaelin Agten, A.; Arslan, A.A. Easy sonographic differential diagnosis between intrauterine pregnancy and cesarean delivery scar pregnancy in the early first trimester. Am. J. Obstet. Gynecol. 2016. [Google Scholar] [CrossRef] [PubMed]
- Riaz, R.M.; Williams, T.R.; Craig, B.M.; Myers, D.T. Cesarean scar ectopic pregnancy: Imaging features, current treatment options, and clinical outcomes. Abdom. Imaging 2015, 40, 2589–2599. [Google Scholar] [CrossRef] [PubMed]
- Jurkovic, D.; Hillaby, K.; Woelfer, B.; Lawrence, A.; Salim, R.; Elson, C.J. First-trimester diagnosis and management of pregnancies implanted into the lower uterine Caesarean section scar. Ultrasound Obstet. Gynecol. 2003, 21, 220–227. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.-J.; Yuen, L.-T.; Chao, A.-S.; Lee, C.-L.; Yen, C.-F.; Soong, Y.-K. Caesarean scar pregnancy successfully treated by operative hysteroscopy and suction curettage. BJOG 2005, 112, 839–840. [Google Scholar] [CrossRef] [PubMed]
- Zhuang, Y.; Huang, L. Uterine artery embolization compared with methotrexate for the management of pregnancy implanted within a cesarean scar. Am. J. Obstet. Gynecol. 2009. [Google Scholar] [CrossRef] [PubMed]
- Hartung, J.; Meckies, J. Management of a case of uterine scar pregnancy by transabdominal potassium chloride injection. Ultrasound Obstet. Gynecol. 2003, 21, 94–95. [Google Scholar] [CrossRef] [PubMed]
- Keung, J.J.; Spies, J.B.; Caridi, T.M. Uterine artery embolization: A review of current concepts. Best Pract. Res. Clin. Obstet. Gynaecol. 2018, 46, 66–73. [Google Scholar] [CrossRef] [PubMed]
- Deans, R.; Abbott, J. Hysteroscopic management of cesarean scar ectopic pregnancy. Fertil. Steril. 2009. [Google Scholar] [CrossRef]
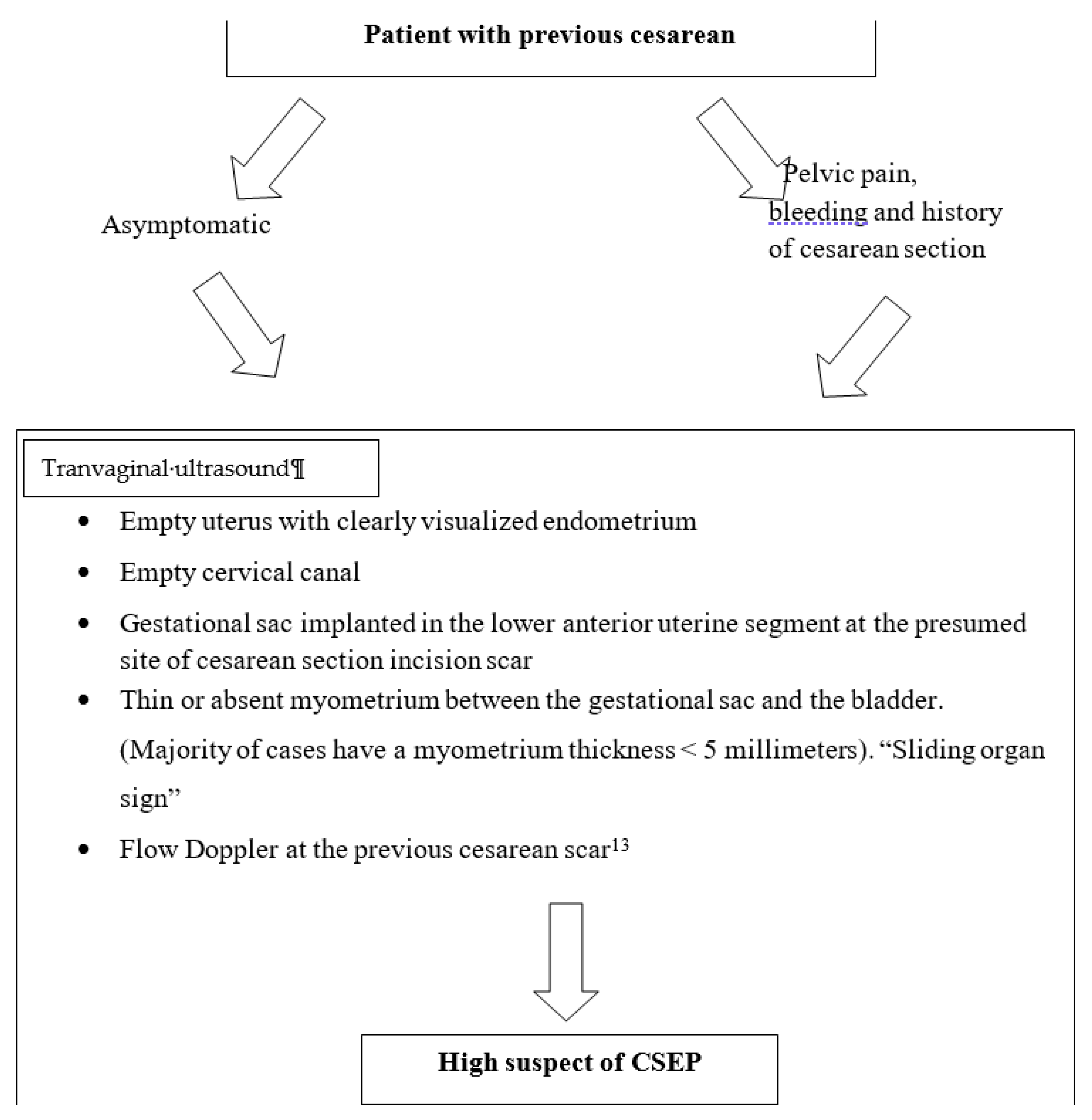




| CSEP Diagnostic Criteria [13] |
|---|
| 1. Empty uterus with clearly visualized endometrium |
| 2. Empty cervical canal |
| 3. Gestational sac implanted in the lower anterior uterine segment at the presumed site of cesarean section incision scar |
| 4. Thin or absent myometrium between the gestational sac and the bladder. (Majority of cases have a myometrium thickness <5 mm). “Sliding organ sign” |
| 5. Doppler flow at the previous cesarean scar [13]. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Morente, L.S.; León, A.I.G.; Reina, M.P.E.; Herrero, J.R.A.; Mesa, E.G.; López, J.S.J. Cesarean Scar Ectopic Pregnancy—Case Series: Treatment Decision Algorithm and Success with Medical Treatment. Medicina 2021, 57, 362. https://doi.org/10.3390/medicina57040362
Morente LS, León AIG, Reina MPE, Herrero JRA, Mesa EG, López JSJ. Cesarean Scar Ectopic Pregnancy—Case Series: Treatment Decision Algorithm and Success with Medical Treatment. Medicina. 2021; 57(4):362. https://doi.org/10.3390/medicina57040362
Chicago/Turabian StyleMorente, Lorena Sabonet, Ana I. Guzmán León, M. Pilar Espejo Reina, Jose R. Anderica Herrero, Ernesto González Mesa, and Jesús S. Jiménez López. 2021. "Cesarean Scar Ectopic Pregnancy—Case Series: Treatment Decision Algorithm and Success with Medical Treatment" Medicina 57, no. 4: 362. https://doi.org/10.3390/medicina57040362
APA StyleMorente, L. S., León, A. I. G., Reina, M. P. E., Herrero, J. R. A., Mesa, E. G., & López, J. S. J. (2021). Cesarean Scar Ectopic Pregnancy—Case Series: Treatment Decision Algorithm and Success with Medical Treatment. Medicina, 57(4), 362. https://doi.org/10.3390/medicina57040362








