Microendoscope-Assisted Versus Open Posterior Lumbar Interbody Fusion for Lumbar Degenerative Disease: A Multicenter Retrospective Cohort Study
Abstract
1. Introduction
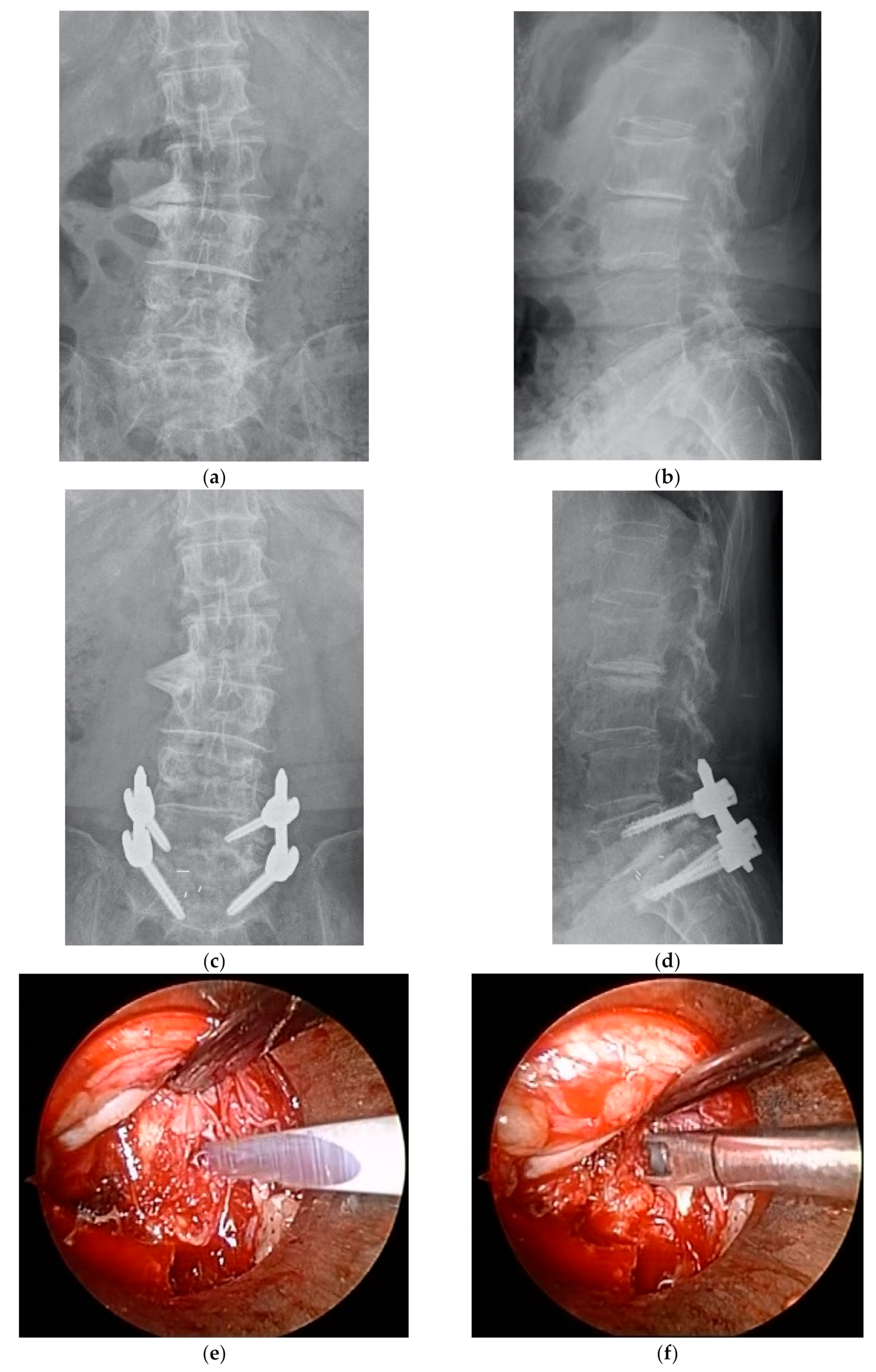
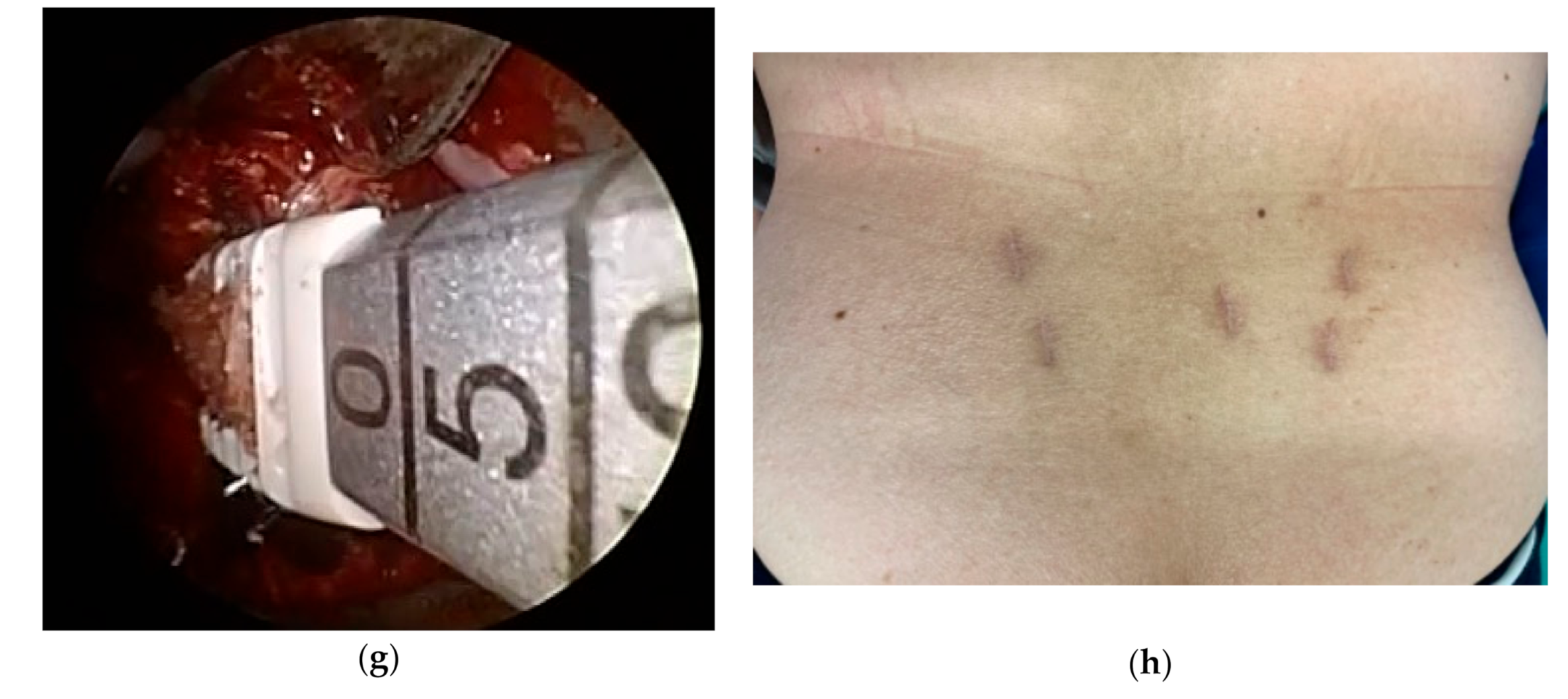
2. Material and Methods
2.1. Study Design
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Turner, J.A.; Ersek, M.; Herron, L.; Haselkorn, J.; Kent, D.; Ciol, M.A.; Deyo, R. Patient outcomes after lumbar spinal fusions. JAMA 1992, 268, 907–911. [Google Scholar] [CrossRef]
- Potter, B.K.; Freedman, B.A.; Verwiebe, E.G.; Hall, J.M.; Polly, D.W., Jr.; Kuklo, T.R. Transforaminal lumbar interbody fusion: Clinical and radiographs results and complications in 100 consecutive patients. J. Spinal Disord. Tech. 2005, 18, 337–346. [Google Scholar] [CrossRef] [PubMed]
- Okuda, S.; Miyauchi, A.; Oda, T.; Haku, T.; Yamamoto, T.; Iwasaki, M. Surgical complications of posterior lumbar interbody fusion with total facetectomy in 251 patients. J. Neurosurg. Spine 2006, 4, 304–309. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; Han, C.; Jiang, H.; Tian, P. The Effect of Obesity on Clinical Outcomes After Minimally Invasive Surgery of the Spine: A Systematic Review and Meta-Analysis. World Nurosourg. 2018, 110, e438–e449. [Google Scholar] [CrossRef] [PubMed]
- Banczerowski, P.; Czigléczki, G.; Papp, Z.; Veres, R.; Rappaport, H.Z.; Vajda, J. Minimally invasive spine surgery: Systematic review. Neurosurg. Rev. 2015, 38, 11–26. [Google Scholar] [CrossRef] [PubMed]
- Foley, K.T.; Smith, M.M. Microendoscopic discectomy. Tech. Nurosurg. 1997, 3, 301–307. [Google Scholar]
- Smith, N.A.; Masters, J.; Jensen, C.; Khan, A.; Sprowson, A. Systematic review of microendoscopic discectomy for lumbar disc herniation. Eur. Spine J. 2013, 22, 2458–2465. [Google Scholar] [CrossRef] [PubMed]
- He, J.; Xiao, S.; Wu, Z.; Yuan, Z. Microendoscopic discectomy versus open discectomy for lumbar disc herniation: A meta-analysis. Eur. Spine J. 2016, 25, 1373–1381. [Google Scholar] [CrossRef]
- Pao, J.L.; Chen, W.C.; Chen, P.Q. Clinical outcomes of microendoscopic decompressive laminectomy for degenerative lumbar spinal stenosis. Eur. Spine J. 2009, 18, 672–678. [Google Scholar] [CrossRef] [PubMed]
- Minamide, A.; Yoshida, M.; Yamada, H.; Nakagawa, Y.; Kawai, M.; Maio, K.; Hashizume, H.; Iwasaki, H.; Tsutsui, S. Endoscope-assisted spinal decompression surgery for lumbar spinal stenosis. J. Neurosurg. Spine 2013, 19, 664–671. [Google Scholar] [CrossRef]
- Castro-Menendez, M.; Bravo-Ricoy, J.A.; Casal-Moro, R.; Hernández-Blanco, M.; Jorge-Barreiro, F.J. Midterm outcome after microendoscopic decompressive laminectomy for lumbar spinal stenosis: 4-year prospective study. Neurosurgery 2009, 65, 100–110. [Google Scholar] [CrossRef]
- Inanami, H.; Saiki, F.; Oshima, Y. Microendoscope-assisted posterior lumbar interbody fusion: A technical note. J. Spine Surg. 2018, 4, 408–413. [Google Scholar] [CrossRef]
- Wang, Y.-T.; Wu, X.-T.; Chen, H.; Wang, C. Endoscopy-assisted posterior lumbar interbody fusion in a single segment. J. Clin. Neurosci. 2014, 21, 287–292. [Google Scholar] [CrossRef]
- Rihn, J.A.; Makda, J.; Hong, J.; Patel, R.; Hilibrand, A.S.; Anderson, D.G.; Vaccaro, A.R.; Albert, T.J. The use of RhBMP-2 in single-level transforaminal lumbar interbody fusion: A clinical and radiographic analysis. Eur. Spine J. 2009, 18, 1629–1636. [Google Scholar] [CrossRef] [PubMed]
- Mannion, R.J.; Nowitzke, A.M.; Wood, M.J. Promoting fusion in minimally invasive lumbar interbody stabilization with low-dose bone morphogenic protein-2—But what is the cost? Spine J. 2011, 11, 527–533. [Google Scholar] [CrossRef] [PubMed]
- Khan, N.R.; Clark, A.J.; Lee, S.L.; Venable, G.T.; Rossi, N.B.; Foley, K.T. Surgical Outcomes for Minimally Invasive vs. Open Transforaminal Lumbar Interbody Fusion: An Updated Systematic Review and Meta-analysis. Neurosurgery 2015, 77, 847–874. [Google Scholar] [CrossRef] [PubMed]
- Qu, J.-T.; Tang, Y.; Wang, M.; Tang, X.-D.; Zhang, T.-J.; Shi, G.-H.; Chen, L.; Hu, Y.; Wang, Z.-T.; Zhou, Y. Comparison of MIS vs. open PLIF/TLIF with regard to clinical improvement, fusion rate, and incidence major complication: A meta-analysis. Eur. Spine J. 2015, 24, 1058–1065. [Google Scholar]
- Goldstein, C.L.; Macwan, K.; Sundararajan, K.; Rampersaud, Y.R. Perioperative outcomes and adverse events of minimally invasive versus open posterior lumbar fusion: Meta-analysis and systematic review. J. Neurosurg. Spine 2016, 24, 416–427. [Google Scholar] [CrossRef]
- Li, A.; Li, X.; Zhong, Y. Is minimally invasive superior than open transforaminal lumbar interbody fusion for single-level degenerative lumbar disease: A meta-analysis. J. Orthop. Surg. Res. 2018, 13, 241. [Google Scholar] [CrossRef]
- Rong, L.-M.; Xie, P.-G.; Shi, D.-H.; Dong, J.-W.; Liu, B.; Feng, F.; Cai, D.-Z. Spinal surgeons’ learning curve for lumbar microendoscopic discectomy: A prospective study of our first 50 and latest 10 cases. Chin. Med. J. 2008, 121, 2148–2151. [Google Scholar] [CrossRef]
- Nowitzke, A.M. Assessment of the learning curve for lumbar microendoscopic discectomy. Neurosurgery 2005, 56, 755–762. [Google Scholar] [CrossRef]
- Yao, Y.-C.; Lin, H.-H.; Chou, P.-H.; Wang, S.-T.; Chang, M.-C. Differences in the interbody bone graft area fusion rate between minimally invasive and traditional open transforaminal lumbar inter body fusion. a retrospective short-term image analysis. Eur. Spine J. 2019, 28, 2095–2102. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, K.; Kitahara, H.; Yamagata, M.; Murakami, M.; Takata, K.; Miyamoto, K.; Mimura, M.; Akahashi, Y.; Moriya, H. Long-term results of anterior interbody fusion for treatment of degenerative spondylolisthesis. Spine 1990, 15, 1211–1215. [Google Scholar] [CrossRef]
- Christensen, F.B.; Hansen, E.S.; Eiskjaer, S.P.; Høy, K.; Helmig, P.; Neumann, P.; Niedermann, B.; Bünger, C.E. Circumferential lumbar spinal fusion with Brantigan cage versus posterolateral fusion with titanium Cotrel-Dubousset instrumentation: A prospective, randomized clinical study of 146 patients. Spine 2002, 27, 2674–2683. [Google Scholar] [CrossRef] [PubMed]
- Tokuhashi, Y.; Ajiro, Y.; Umezawa, N. Follow-up of patients with delayed union after posterior fusion with pedicle screw fixation. Spine 2008, 33, 786–791. [Google Scholar] [CrossRef] [PubMed]
| ME Group | Open Group | p | |
|---|---|---|---|
| Follow up rate (%) | 79% (57/72) | 75% (58/77) | 0.57 |
| Mean age (years) | 65.2 ± 11.9 | 67.5 ± 9.0 | 0.32 |
| (range) | (21–84) | 39–90 | |
| Gender (M/F) | 31/26 | 26/32 | 0.31 |
| Height (cm) | 162.7 ± 8.9 | 164.9 ± 9.3 | 0.44 |
| (range) | (137.6–183.0) | (141.0–178.7) | |
| Body weight (kg) | 65.3 ± 11.7 | 67.1 ± 11.4 | 0.63 |
| (range) | (38.5–105.7) | (42.0–82.3) | |
| BMI | 23.9 ± 4.4 | 24.0 ± 3.9 | 0.90 |
| (range) | (17.0–33.4) | (18.1–38.2) | |
| Diagnosis | 0.58 | ||
| Degenerative spondylolisthesis | 31 | 33 | |
| Spondylolytic spondylolisthesis | 9 | 7 | |
| Foraminal stenosis | 17 | 18 | |
| Level of fusion | 0.73 | ||
| L3–L4 | 2 | 1 | |
| L4–L5 | 35 | 31 | |
| L5–S1 | 20 | 26 |
| ME Group (n = 57) | Open Group (n = 58) | p | |
|---|---|---|---|
| Operative time (min) | 128.0 ± 34.9 | 176.6 ± 37.3 | 0.001 |
| (range) | 59–228 | 103–295 | |
| Intraoperative blood loss (mL) | 81.0 ± 92.8 | 315.2 ± 214.1 | 0.001 |
| (range) | 10–650 | 75–1080 | |
| Number of cages | 1.27 (1–2) | 1.36 (1–2) | 0.54 |
| Cage type (PEEK/titanium) | 55/2 | 54/4 | 0.41 |
| Intraoperative complications | 3 | 3 | 0.98 |
| all cases dural tear | all cases dural tear | ||
| Duration of hospital stay (day) | 10.7 ± 2.0 | 18.5 ± 6.1 | 0.001 |
| (range) | (8–17) | (10–47) | |
| Postoperative complications | 3 | 2 | 0.79 |
| cageloosening, | hematoma, | ||
| infection, | Vertebral body fracture | ||
| screw loosening |
| ME Group | Open Group | p | |
|---|---|---|---|
| NRS Low back pain | |||
| Preoperative | 5.89 ± 2.6 | 6.24 ± 3.0 | 0.76 |
| Postoperative | 2.42 ±1.9 | 3.51 ± 2.1 | 0.12 |
| NRS Leg pain | |||
| Preoperative | 5.22 ± 3.2 | 5.77 ± 3.9 | 0.64 |
| Postoperative | 2.16 ± 1.8 | 2.76 ± 2.69 | 0.34 |
| ODI | |||
| Preoperative | 20.8 ± 9.2 | 20.2 ± 10.8 | 0.89 |
| Postoperative | 6.9 ± 5.3 | 8.8 ± 5.8 | 0.44 |
| EQ-5D | |||
| Preoperative | 0.56 ± 0.12 | 0.53 ± 0.15 | 0.71 |
| Postoperative | 0.79 ± 0.17 | 0.70 ± 0.18 | 0.51 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fukushima, M.; Ohtomo, N.; Noma, M.; Kumanomido, Y.; Nakarai, H.; Tozawa, K.; Yoshida, Y.; Sakamoto, R.; Miyahara, J.; Anno, M.; et al. Microendoscope-Assisted Versus Open Posterior Lumbar Interbody Fusion for Lumbar Degenerative Disease: A Multicenter Retrospective Cohort Study. Medicina 2021, 57, 150. https://doi.org/10.3390/medicina57020150
Fukushima M, Ohtomo N, Noma M, Kumanomido Y, Nakarai H, Tozawa K, Yoshida Y, Sakamoto R, Miyahara J, Anno M, et al. Microendoscope-Assisted Versus Open Posterior Lumbar Interbody Fusion for Lumbar Degenerative Disease: A Multicenter Retrospective Cohort Study. Medicina. 2021; 57(2):150. https://doi.org/10.3390/medicina57020150
Chicago/Turabian StyleFukushima, Masayoshi, Nozomu Ohtomo, Michita Noma, Yudai Kumanomido, Hiroyuki Nakarai, Keiichiro Tozawa, Yuichi Yoshida, Ryuji Sakamoto, Junya Miyahara, Masato Anno, and et al. 2021. "Microendoscope-Assisted Versus Open Posterior Lumbar Interbody Fusion for Lumbar Degenerative Disease: A Multicenter Retrospective Cohort Study" Medicina 57, no. 2: 150. https://doi.org/10.3390/medicina57020150
APA StyleFukushima, M., Ohtomo, N., Noma, M., Kumanomido, Y., Nakarai, H., Tozawa, K., Yoshida, Y., Sakamoto, R., Miyahara, J., Anno, M., Kawamura, N., Higashikawa, A., Takeshita, Y., Inanami, H., Tanaka, S., & Oshima, Y. (2021). Microendoscope-Assisted Versus Open Posterior Lumbar Interbody Fusion for Lumbar Degenerative Disease: A Multicenter Retrospective Cohort Study. Medicina, 57(2), 150. https://doi.org/10.3390/medicina57020150







