Transcatheter Arterial Embolization for Spontaneous Hepatic Rupture Associated with HELLP Syndrome: A Case Report
Abstract
:1. Introduction
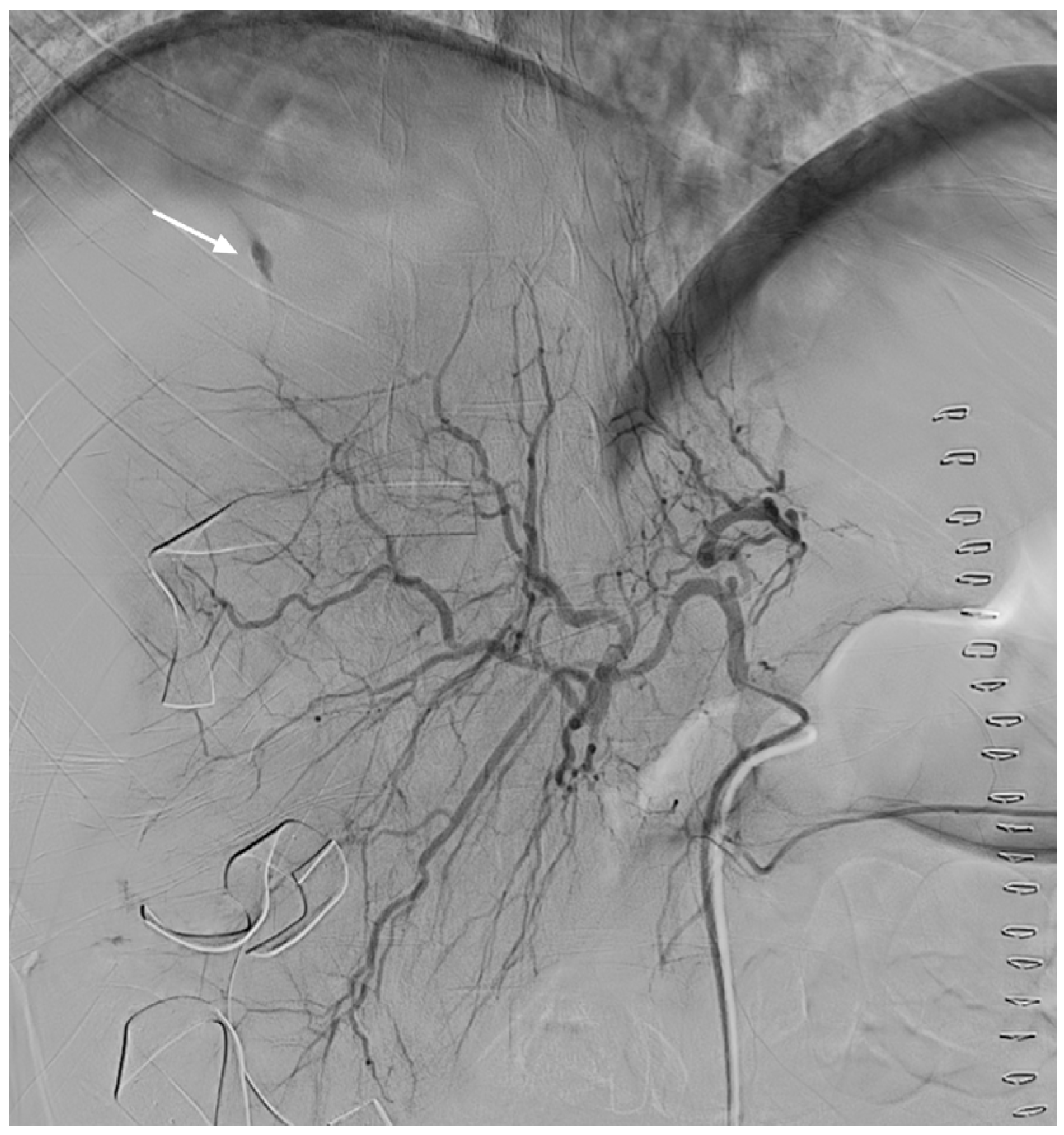
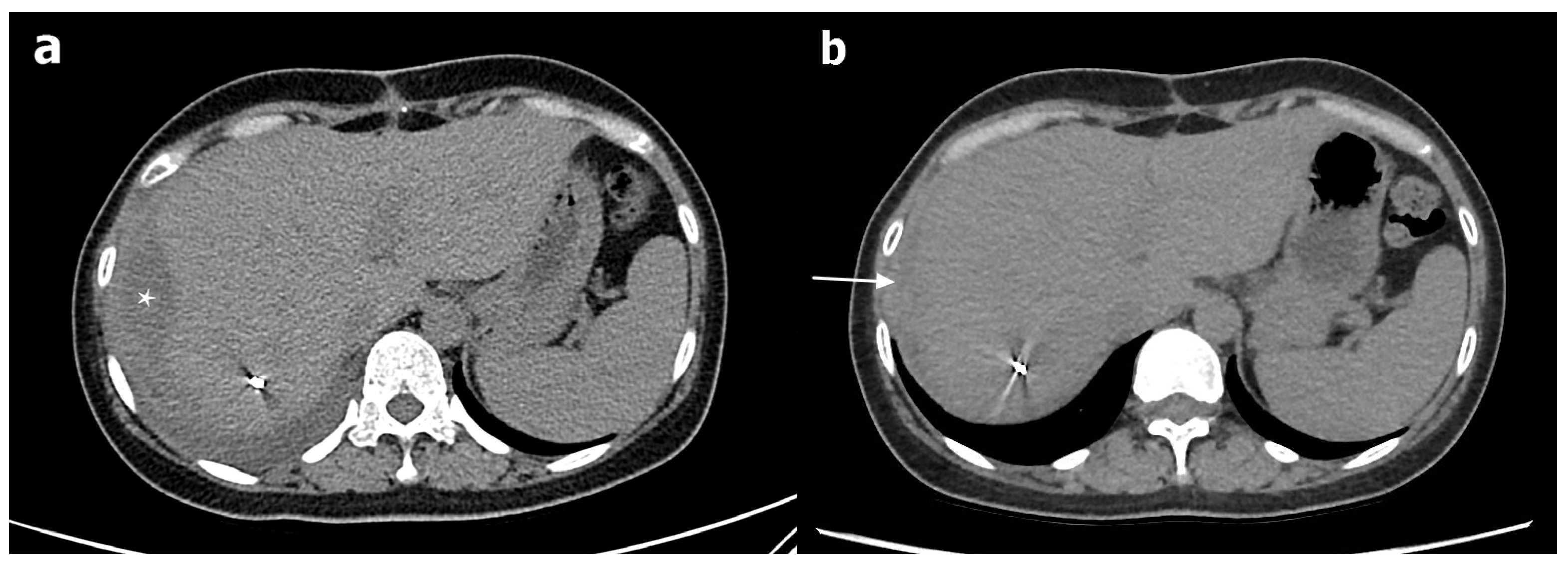
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Araujo, A.C.; Leao, M.D.; Nobrega, M.H.; Bezerra, P.F.; Pereira, F.V.; Dantas, E.M.; Azevedo, G.D.; Jeronimo, S.M. Characteristics and treatment of hepatic rupture caused by HELLP syndrome. Am. J. Obstet. Gynecol. 2006, 195, 129–133. [Google Scholar] [CrossRef] [PubMed]
- Miguelote, R.F.; Costa, V.; Vivas, J.; Gonzaga, L.; Menezes, C.A. Postpartum spontaneous rupture of a liver hematoma associated with preeclampsia and HELLP syndrome. Arch. Gynecol. Obstet. 2009, 279, 923–926. [Google Scholar] [CrossRef] [PubMed]
- Smith, L.G., Jr.; Moise, K.J., Jr.; Dildy, G.A., 3rd; Carpenter, R.J., Jr. Spontaneous rupture of liver during pregnancy: Current therapy. Obstet. Gynecol. 1991, 77, 171–175. [Google Scholar] [CrossRef] [PubMed]
- Vigil-De Gracia, P.; Ortega-Paz, L. Pre-eclampsia/eclampsia and hepatic rupture. Int. J. Gynaecol. Obstet. 2012, 118, 186–189. [Google Scholar] [CrossRef] [PubMed]
- Ditisheim, A.; Sibai, B.M. Diagnosis and management of HELLP syndrome complicated by liver hematoma. Clin. Obstet. Gynecol. 2017, 60, 190–197. [Google Scholar] [CrossRef] [PubMed]
- Pavlis, T.; Aloizos, S.; Aravosita, P.; Mystakelli, C.; Petrochilou, D.; Dimopoulos, N.; Gourgiotis, S. Diagnosis and surgical management of spontaneous hepatic rupture associated with HELLP syndrome. J. Surg. Educ. 2009, 66, 163–167. [Google Scholar] [CrossRef] [PubMed]
- Terasaki, K.K.; Quinn, M.F.; Lundell, C.J.; Finck, E.J.; Pentecost, M.J. Spontaneous hepatic hemorrhage in preeclampsia: Treatment with hepatic arterial embolization. Radiology 1990, 174, 1039–1041. [Google Scholar] [CrossRef] [PubMed]
- Dubey, S.; Rani, J. Hepatic rupture in preeclampsia and HELLP syndrome: A catastrophic presentation. Taiwan J. Obstet. Gynecol. 2020, 59, 643–651. [Google Scholar] [CrossRef] [PubMed]
- Millan, C.A.; Forero, J.C. Right hepatectomy after spontaneous hepatic rupture in a patient with preeclampsia: A case report. Int. J. Surg. Case Rep. 2017, 39, 250–252. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Lee, S.M.; Kim, J.W.; Shin, J.H. Recent update of embolization of postpartum hemorrhage. Korean J. Radiol. 2018, 19, 585–596. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nam, I.-C.; Won, J.-H.; Kim, S.; Bae, K.; Jeon, K.-N.; Moon, J.-I.; Cho, E.; Park, J.-E.; Jang, J.-Y.; Park, S.-E. Transcatheter Arterial Embolization for Spontaneous Hepatic Rupture Associated with HELLP Syndrome: A Case Report. Medicina 2021, 57, 1055. https://doi.org/10.3390/medicina57101055
Nam I-C, Won J-H, Kim S, Bae K, Jeon K-N, Moon J-I, Cho E, Park J-E, Jang J-Y, Park S-E. Transcatheter Arterial Embolization for Spontaneous Hepatic Rupture Associated with HELLP Syndrome: A Case Report. Medicina. 2021; 57(10):1055. https://doi.org/10.3390/medicina57101055
Chicago/Turabian StyleNam, In-Chul, Jung-Ho Won, Sungbin Kim, Kyungsoo Bae, Kyung-Nyeo Jeon, Jin-Il Moon, Eun Cho, Ji-Eun Park, Jae-Yool Jang, and Sung-Eun Park. 2021. "Transcatheter Arterial Embolization for Spontaneous Hepatic Rupture Associated with HELLP Syndrome: A Case Report" Medicina 57, no. 10: 1055. https://doi.org/10.3390/medicina57101055
APA StyleNam, I.-C., Won, J.-H., Kim, S., Bae, K., Jeon, K.-N., Moon, J.-I., Cho, E., Park, J.-E., Jang, J.-Y., & Park, S.-E. (2021). Transcatheter Arterial Embolization for Spontaneous Hepatic Rupture Associated with HELLP Syndrome: A Case Report. Medicina, 57(10), 1055. https://doi.org/10.3390/medicina57101055






