Cyclic Progesterone Therapy in Androgenic Polycystic Ovary Syndrome (PCOS)—A 6-Month Pilot Study of a Single Woman’s Experience Changes
Abstract
1. Introduction
2. Materials and Methods
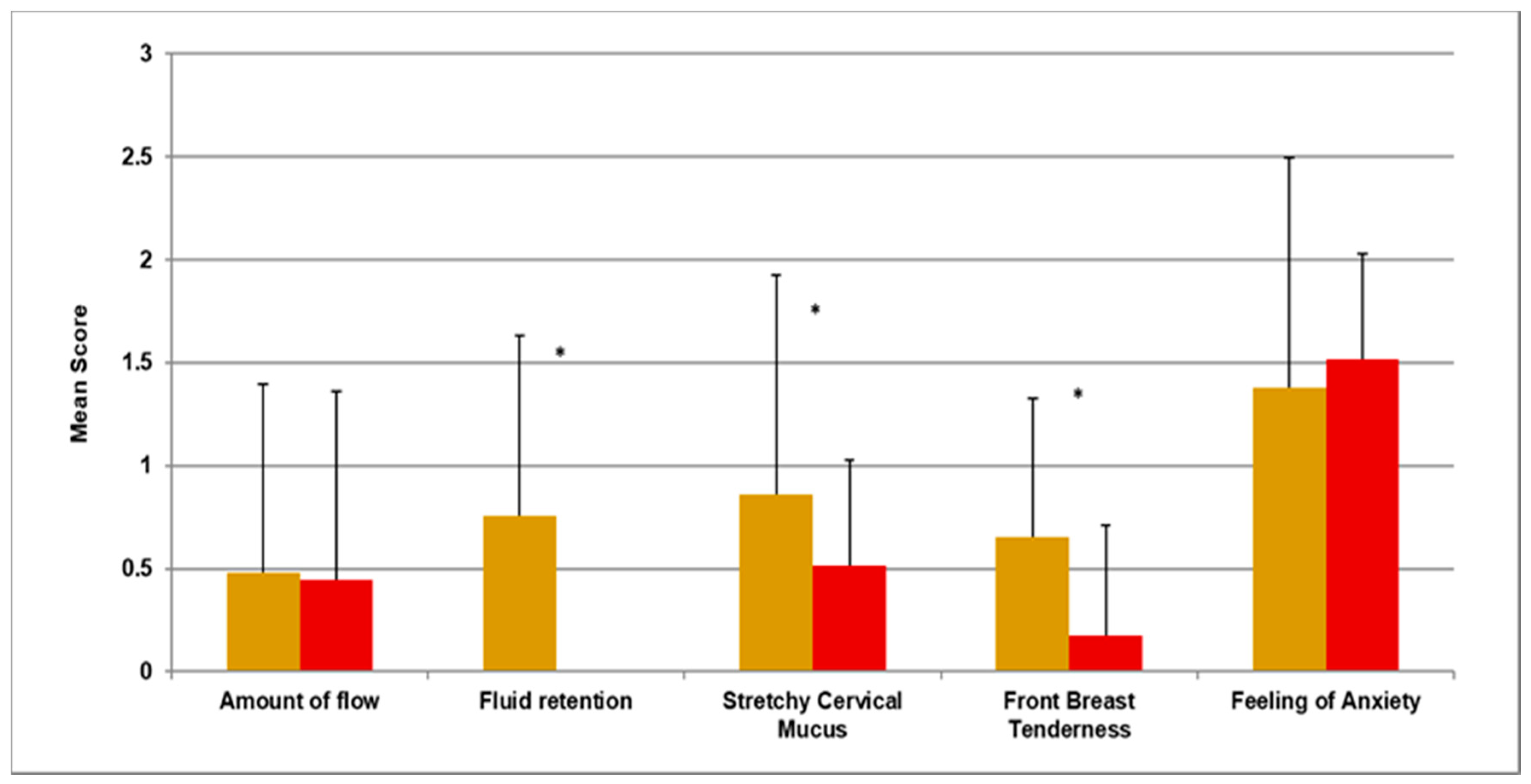
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Teede, H.J.; Misso, M.L.; Costello, M.F.; Dokras, A.; Laven, J.; Moran, L.; Piltonen, T.; Norman, R.J. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Clin. Endocrinol. 2018, 89, 251–268. [Google Scholar] [CrossRef]
- Bozdag, G.; Mumusoglu, S.; Zengin, D.; Karabulut, E.; Yildiz, B.O. The prevalence and phenotypic features of polycystic ovary syndrome: A systematic review and meta-Analysis. Hum. Reprod. 2016, 31, 2841–2855. [Google Scholar] [CrossRef] [PubMed]
- Gibson-Helm, M.; Teede, H.; Dunaif, A.; Dokras, A. Delayed diagnosis and a lack of information associated with dissatisfaction in women with polycystic ovary syndrome. J. Clin. Endocrinol. Metab. 2017, 102, 604–612. [Google Scholar] [CrossRef] [PubMed]
- Pathak, G.; Nichter, M. Polycystic ovary syndrome in globalizing India: An ecosocial perspective on an emerging lifestyle disease. Soc. Sci. Med. 2015, 146, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Dokras, A.; Stener-Victorin, E.; Yildiz, B.O.; Li, R.; Ottey, S.; Shah, D.; Epperson, N.; Teede, H. Androgen Excess-Polycystic Ovary Syndrome Society: Position statement on depression, anxiety, quality of life, and eating disorders in polycystic ovary syndrome. Fertil. Steril. 2018, 109, 888–899. [Google Scholar] [CrossRef] [PubMed]
- Azziz, R.; Carmina, E.; Chen, Z.; Dunaif, A.; Laven, J.S.; Legro, R.S.; Lizneva, D.; Natterson-Horowtiz, B.; Teede, H.J.; Yildiz, B.O. Polycystic ovary syndrome. Nat. Rev. Dis. Prim. 2016, 2, 16057. [Google Scholar] [CrossRef]
- Barry, J.A.; Azizia, M.M.; Hardiman, P.J. Risk of endometrial, ovarian and breast cancer in women with polycystic ovary syndrome: A systematic review and meta-analysis. Hum. Reprod. Update 2014, 20, 748–758. [Google Scholar] [CrossRef] [PubMed]
- Dokras, A.; Sarwer, D.B.; Allison, K.C.; Milman, L.; Kris-Etherton, P.; Kunselman, A.R.; Stetter, C.M.; Williams, N.I.; Gnatuk, C.L.; Estes, S.J.; et al. Weight loss and lowering androgens predict improvements in health-related quality of life in women with PCOS. J. Clin. Endocrinol. Metab. 2016, 101, 2966–2974. [Google Scholar] [CrossRef]
- Falsetti, L.; Gambera, A.; Tisi, G. Efficacy of the combination ethinyl oestradiol and cyproterone acetate on endocrine, clinical and ultrasonographic profile in polycystic ovarian syndrome. Hum. Reprod. 2001, 16, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Kalyan, S.; Goshtesabi, A.; Sarray, S.; Joannou, A.; Almawi, W.Y. Assessing C reactive protein/albumin ratio as a new biomarker for polycystic ovary syndrome: A case-control study of women from Bahraini medical clinics. BMJ Open 2018, 8, e021860. [Google Scholar] [CrossRef]
- Pastor, C.L.; Griffin-Korf, M.L.; Aloi, J.A.; Evans, W.S.; Marshall, J.C. Polycystic ovary syndrome: Evidence for reduced sensitivity of the gonadotropin-releasing hormone pulse generator to inhibition by estradiol and progesterone. J. Clin. Endocrinol. Metab. 1998, 83, 582–590. [Google Scholar] [CrossRef] [PubMed]
- Prior, J.C. The Case for A New PCOS Therapy. 2018. Available online: https://helloclue.com/articles/cycle-a-z/the-case-for-a-new-pcos-therapy (accessed on 29 November 2018).
- Blank, S.K.; McCartney, C.R.; Marshall, J.C. The origins and sequelae of abnormal neuroendocrine function in polycystic ovary syndrome. Hum. Reprod. Update 2006, 12, 351–361. [Google Scholar] [CrossRef] [PubMed]
- Briden, L.; Shirin, S.; Prior, J.C. The central role of ovulatory disturbances in the etiology of androgenic polycystic ovary syndrome (PCOS)—Evidence for treatment with cyclic progesterone. Drug Discov. Today Dis. Model. 2020, 32, 71–82. [Google Scholar] [CrossRef]
- Soules, M.R.; Steiner, R.A.; Clifton, D.K.; Cohen, N.L.; Aksel, S.B.W. Progesterone modulation of pulsatile luteinizing hormone secretion in normal women. J. Clin. Endocrinol. Metab. 1984, 58, 378–383. [Google Scholar] [CrossRef] [PubMed]
- Cheung, A.P.; Lu, J.K.H.; Chang, R.J. Pulsatile gonadotrophin secretion in women with polycystic ovary syndrome after gonadotrophin-releasing hormone agonist treatment. Hum. Reprod. 1997, 12, 1156–1164. [Google Scholar] [CrossRef][Green Version]
- Baird, D.T.; Corker, C.S.; Davidson, D.W.; Hunter, W.M.; Michie, E.A.; Van Look, P.F.A. Pituitary-ovarian relationships in polycystic ovary syndrome. J. Clin. Endocrinol. Metab. 1977, 45, 798–809. [Google Scholar] [CrossRef]
- Dennerstein, L.; Spencer-Gardner, C.; Gotts, G.; Brown, J.B.; Smith, M.A.; Burrows, G.D. Progesterone and the premenstrual syndrome: A double blind cross-over trial. Br. Med. J. 1985, 290, 1617. [Google Scholar] [CrossRef]
- Livadas, S.; Boutzios, G.; Economou, F.; Alexandraki, K.; Xyrafis, X.; Christou, M.; Zerva, A.; Karachalios, A.; Tantalaki, E.; Diamanti-Kandarakis, E. The effect of oral micronized progesterone on hormonal and metabolic parameters in anovulatory patients with polycystic ovary syndrome. Fertil. Steril. 2010, 94, 242–246. [Google Scholar] [CrossRef]
- Bagis, T.; Gokcel, A.; Zeyneloglu, H.B.; Tarim, E.; Kilicdag, E.B.; Haydardedeoglu, B. The effects of short-term medroxyprogesterone acetate and micronized progesterone on glucose metabolism and lipid profiles in patients with polycystic ovary syndrome: A prospective randomized study. J. Clin. Endocrinol. Metab. 2002, 87, 4536–4540. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Prior, J.C. Exercise-associated menstrual disturbances. In Reproductive Endocrinology, Surgery and Technology; Adashi, E.Y., Rock, J.A., Rosenwaks, Z.E., Eds.; Raven Press: New York, NY, USA, 1996; p. 6. [Google Scholar]
- ClinicaKey. Drug Monograph Progesterone: Elsevier; 26 August 2020. Available online: https://www-clinicalkey-com.www.proxy.cpsbc.ca/#!/content/drug_monograph/6-s2.0-515 (accessed on 6 January 2021).
- Prior, J.C.; Vigna, Y.M.; Barr, S.I.; Rexworthy, C.; Lentle, B.C. Cyclic medroxyprogesterone treatment increases bone density: A controlled trial in active women with menstrual cycle disturbances. Am. J. Med. 1994, 96, 521–530. [Google Scholar] [CrossRef]
- Buckler, H.M.; Bangah, M.; Healy, D.L.; Burger, H.G. Vaginal progesterone administration in physiological doses normalizes raised luteinizing hormone levels in patients with polycystic ovarian syndrome. Gynecol. Endocrinol. 1992, 6, 275–282. [Google Scholar] [CrossRef]
- Harvey, A.T.; Hitchcock, C.L.; Prior, J.C. Ovulation disturbances and mood across the menstrual cycles of healthy women. J. Psychosom. Obstet. Gynecol. 2009, 30, 207–214. [Google Scholar] [CrossRef] [PubMed]
- White, C.P.; Hitchcock, C.L.; Vigna, Y.M.; Prior, J.C. Fluid Retention over the Menstrual Cycle: 1-Year Data from the Prospective Ovulation Cohort. Obstet. Gynecol. Int. 2011, 2011, 138451. [Google Scholar] [CrossRef] [PubMed]
- Macbeth, A.B.; Goshtasebi, A.; Mercer, G.W.; Prior, J.C. Does Interest in Sex Peak at Mid-Cycle in Ovulatory Menstrual Cycles of Healthy, Community Dwelling Women? An 11-Month Prospective Observational Study. Women Reprod. Health 2021, 8, 79–91. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shirin, S.; Murray, F.; Goshtasebi, A.; Kalidasan, D.; Prior, J.C. Cyclic Progesterone Therapy in Androgenic Polycystic Ovary Syndrome (PCOS)—A 6-Month Pilot Study of a Single Woman’s Experience Changes. Medicina 2021, 57, 1024. https://doi.org/10.3390/medicina57101024
Shirin S, Murray F, Goshtasebi A, Kalidasan D, Prior JC. Cyclic Progesterone Therapy in Androgenic Polycystic Ovary Syndrome (PCOS)—A 6-Month Pilot Study of a Single Woman’s Experience Changes. Medicina. 2021; 57(10):1024. https://doi.org/10.3390/medicina57101024
Chicago/Turabian StyleShirin, Sonia, Faye Murray, Azita Goshtasebi, Dharani Kalidasan, and Jerilynn C. Prior. 2021. "Cyclic Progesterone Therapy in Androgenic Polycystic Ovary Syndrome (PCOS)—A 6-Month Pilot Study of a Single Woman’s Experience Changes" Medicina 57, no. 10: 1024. https://doi.org/10.3390/medicina57101024
APA StyleShirin, S., Murray, F., Goshtasebi, A., Kalidasan, D., & Prior, J. C. (2021). Cyclic Progesterone Therapy in Androgenic Polycystic Ovary Syndrome (PCOS)—A 6-Month Pilot Study of a Single Woman’s Experience Changes. Medicina, 57(10), 1024. https://doi.org/10.3390/medicina57101024





