Effectiveness of 6-Week Nordic Walking Training on Functional Performance, Gait Quality, and Quality of Life in Parkinson’s Disease
Abstract
1. Introduction
2. Materials and Methods
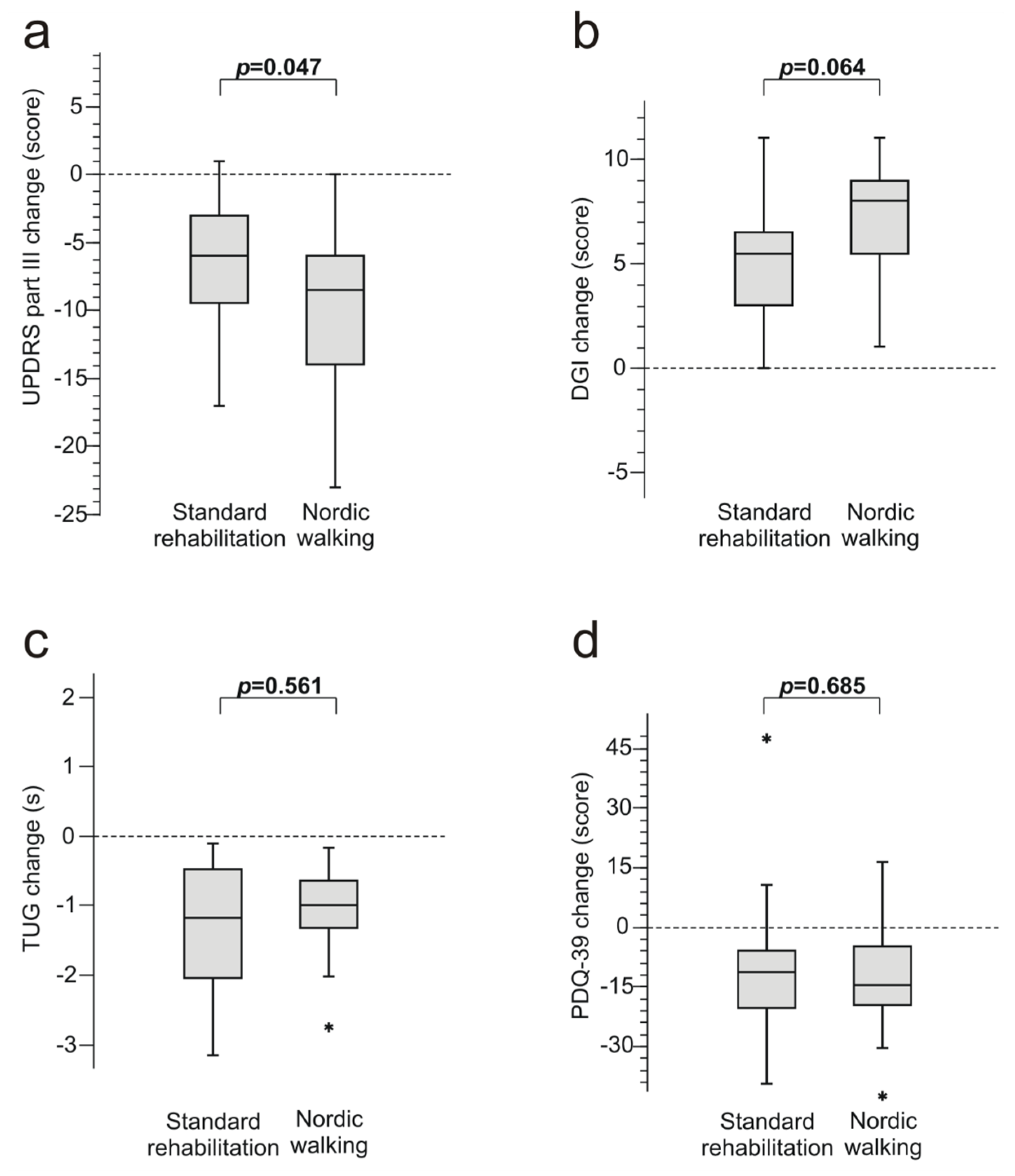
3. Results
3.1. Baseline Clinical Presentation
3.2. Results after 6 Weeks of Training
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Elbaz, A.; Carcaillon, L.; Kab, S.; Moisan, F. Epidemiology of parkinson’s disease. Rev. Neurol. 2016, 172, 14–26. [Google Scholar] [CrossRef] [PubMed]
- Intzandt, B.; Beck, E.N.; Silveira, C.R.A. The effects of exercise on cognition and gait in parkinson’s disease: A scoping review. Neurosci. Biobehav. Rev. 2018, 95, 136–169. [Google Scholar] [CrossRef] [PubMed]
- Cholewa, J.; Cholewa, J.; Gorzkowska, A.; Malecki, A.; Stanula, A. Can rehabilitation influence the efficiency of control signals in complex motion strategies? BioMed Res. Int. 2017, 2017, 3631624. [Google Scholar] [CrossRef] [PubMed]
- Lauze, M.; Daneault, J.F.; Duval, C. The effects of physical activity in parkinson’s disease: A review. J. Parkinsons Dis. 2016, 6, 685–698. [Google Scholar] [CrossRef] [PubMed]
- Cascaes da Silva, F.; Iop Rda, R.; Domingos Dos Santos, P.; Aguiar Bezerra de Melo, L.M.; Barbosa Gutierres Filho, P.J.; Da Silva, R. Effects of physical-exercise-based rehabilitation programs on the quality of life of patients with parkinson’s disease: A systematic review of randomized controlled trials. J. Aging Phys. Act. 2016, 24, 484–496. [Google Scholar] [CrossRef] [PubMed]
- Bowman, T.; Gervasoni, E.; Parelli, R.; Jonsdottir, J.; Ferrarin, M.; Cattaneo, D.; Carpinella, I. Predictors of mobility domain of health-related quality of life after rehabilitation in parkinson’s disease: A pilot study. Arch. Physiother. 2018, 8, 10. [Google Scholar] [CrossRef]
- Fox, S.H.; Katzenschlager, R.; Lim, S.Y.; Barton, B.; De Bie, R.M.A.; Seppi, K.; Coelho, M.; Sampaio, C.; Movement Disorder Society Evidence-Based Medicine Committee. International parkinson and movement disorder society evidence-based medicine review: Update on treatments for the motor symptoms of parkinson’s disease. Mov. Disord. 2018, 33, 1248–1266. [Google Scholar] [CrossRef]
- King, L.A.; Horak, F.B. Delaying mobility disability in people with parkinson disease using a sensorimotor agility exercise program. Phys. Ther. 2009, 89, 384–393. [Google Scholar] [CrossRef]
- Earhart, G.M.; Dibble, L.E.; Ellis, T.; Nieuwboer, A. Rehabilitation and parkinson’s disease 2013. Parkinsons Dis. 2013, 2013, 506375. [Google Scholar] [CrossRef] [PubMed]
- Ebersbach, G.; Ebersbach, A.; Gandor, F.; Wegner, B.; Wissel, J.; Kupsch, A. Impact of physical exercise on reaction time in patients with parkinson’s disease-data from the berlin big study. Arch. Phys. Med. Rehabil. 2014, 95, 996–999. [Google Scholar] [CrossRef]
- Duchesne, C.; Lungu, O.; Nadeau, A.; Robillard, M.E.; Bore, A.; Bobeuf, F.; Lafontaine, A.L.; Gheysen, F.; Bherer, L.; Doyon, J. Enhancing both motor and cognitive functioning in parkinson’s disease: Aerobic exercise as a rehabilitative intervention. Brain Cogn. 2015, 99, 68–77. [Google Scholar] [CrossRef] [PubMed]
- Picelli, A.; Varalta, V.; Melotti, C.; Zatezalo, V.; Fonte, C.; Amato, S.; Saltuari, L.; Santamato, A.; Fiore, P.; Smania, N. Effects of treadmill training on cognitive and motor features of patients with mild to moderate parkinson’s disease: A pilot, single-blind, randomized controlled trial. Funct. Neurol. 2016, 31, 25–31. [Google Scholar] [PubMed]
- Nadeau, A.; Lungu, O.; Duchesne, C.; Robillard, M.E.; Bore, A.; Bobeuf, F.; Plamondon, R.; Lafontaine, A.L.; Gheysen, F.; Bherer, L.; et al. A 12-week cycling training regimen improves gait and executive functions concomitantly in people with parkinson’s disease. Front. Hum. Neurosci. 2016, 10, 690. [Google Scholar] [CrossRef] [PubMed]
- Van der Kolk, N.M.; De Vries, N.M.; Penko, A.L.; Van der Vlugt, M.; Mulder, A.A.; Post, B.; Alberts, J.L.; Bloem, B.R. A remotely supervised home-based aerobic exercise programme is feasible for patients with parkinson’s disease: Results of a small randomised feasibility trial. J. Neurol. Neurosurg. Psychiatry 2018, 89, 1003–1005. [Google Scholar] [CrossRef]
- Studer, V.; Maestri, R.; Clerici, I.; Spina, L.; Zivi, I.; Ferrazzoli, D.; Frazzitta, G. Treadmill training with cues and feedback improves gait in people with more advanced parkinson’s disease. J. Parkinsons Dis. 2017, 7, 729–739. [Google Scholar] [CrossRef]
- Cugusi, L.; Manca, A.; Dragone, D.; Deriu, F.; Solla, P.; Secci, C.; Monticone, M.; Mercuro, G. Nordic walking for the management of people with parkinson disease: A systematic review. PM R 2017, 9, 1157–1166. [Google Scholar] [CrossRef]
- Lim, I.; Van Wegen, E.; De Goede, C.; Deutekom, M.; Nieuwboer, A.; Willems, A.; Jones, D.; Rochester, L.; Kwakkel, G. Effects of external rhythmical cueing on gait in patients with parkinson’s disease: A systematic review. Clin. Rehabil. 2005, 19, 695–713. [Google Scholar] [CrossRef]
- Brauer, S.G.; Morris, M.E. Can people with parkinson’s disease improve dual tasking when walking? Gait Posture 2010, 31, 229–233. [Google Scholar] [CrossRef]
- Warlop, T.; Detrembleur, C.; Buxes Lopez, M.; Stoquart, G.; Lejeune, T.; Jeanjean, A. Does nordic walking restore the temporal organization of gait variability in parkinson’s disease? J. Neuroeng. Rehabil. 2017, 14, 17. [Google Scholar] [CrossRef]
- Reuter, I.; Mehnert, S.; Leone, P.; Kaps, M.; Oechsner, M.; Engelhardt, M. Effects of a flexibility and relaxation programme, walking, and nordic walking on parkinson’s disease. J. Aging Res. 2011, 2011, 232473. [Google Scholar] [CrossRef]
- Van Eijkeren, F.J.; Reijmers, R.S.; Kleinveld, M.J.; Minten, A.; Bruggen, J.P.; Bloem, B.R. Nordic walking improves mobility in parkinson’s disease. Mov. Disord. 2008, 23, 2239–2243. [Google Scholar] [CrossRef]
- Cugusi, L.; Solla, P.; Serpe, R.; Carzedda, T.; Piras, L.; Oggianu, M.; Gabba, S.; Di Blasio, A.; Bergamin, M.; Cannas, A.; et al. Effects of a nordic walking program on motor and non-motor symptoms, functional performance and body composition in patients with parkinson’s disease. Neurorehabilitation 2015, 37, 245–254. [Google Scholar] [CrossRef]
- Franzoni, L.T.; Monteiro, E.P.; Oliveira, H.B.; Da Rosa, R.G.; Costa, R.R.; Rieder, C.; Martinez, F.G.; Peyre-Tartaruga, L.A. A 9-week nordic and free walking improve postural balance in parkinson’s disease. Sports Med. Int. Open 2018, 2, E28–E34. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Gougeon, M.A.; Nantel, J. Nordic walking improves gait power profiles at the knee joint in parkinson’s disease. J. Aging Phys. Act. 2018, 26, 84–88. [Google Scholar] [CrossRef] [PubMed]
- Hughes, A.J.; Daniel, S.E.; Kilford, L.; Lees, A.J. Accuracy of clinical diagnosis of idiopathic parkinson’s disease: A clinico-pathological study of 100 cases. J. Neurol. Neurosurg. Psychiatry 1992, 55, 181–184. [Google Scholar] [CrossRef]
- Hoehn, M.M.; Yahr, M.D. Parkinsonism: Onset, progression and mortality. Neurology 1967, 17, 427–442. [Google Scholar] [CrossRef]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Fox, S.H.; Katzenschlager, R.; Lim, S.Y.; Ravina, B.; Seppi, K.; Coelho, M.; Poewe, W.; Rascol, O.; Goetz, C.G.; Sampaio, C. The movement disorder society evidence-based medicine review update: Treatments for the motor symptoms of parkinson’s disease. Mov. Disord. 2011, 26, S42–S80. [Google Scholar] [CrossRef]
- Zesiewicz, T.A.; Evatt, M.L. Potential influences of complementary therapy on motor and non-motor complications in parkinson’s disease. CNS Drugs 2009, 23, 817–835. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Xie, C.L.; Wang, W.W.; Lu, L.; Fu, D.L.; Wang, X.T.; Zheng, G.Q. Epidemiology of complementary and alternative medicine use in patients with parkinson’s disease. J. Clin. Neurosci. 2013, 20, 1062–1067. [Google Scholar] [CrossRef] [PubMed]
- Hackney, M.E.; Earhart, G.M. Health-related quality of life and alternative forms of exercise in parkinson disease. Parkinsonism Relat. Disord. 2009, 15, 644–648. [Google Scholar] [CrossRef] [PubMed]
- Fahn, S.; Elton, R. UPDRS Development Committee. Unified parkinson’s disease rating scale. In Recent Developments in Parkinson’s Disease; Fahn, S., Marsden, C., Calne, D., Goldstein, M., Eds.; Macmillan: Florham Park, NJ, USA, 1987; pp. 153–163. [Google Scholar]
- Movement Disorder Society Task Force on Rating Scales for Parkinson’s Disease. The unified parkinson’s disease rating scale (updrs): Status and recommendations. Mov. Disord. 2003, 18, 738–750. [Google Scholar] [CrossRef]
- Schrag, A.; Sampaio, C.; Counsell, N.; Poewe, W. Minimal clinically important change on the unified parkinson’s disease rating scale. Mov. Disord. 2006, 21, 1200–1207. [Google Scholar] [CrossRef] [PubMed]
- Shulman, L.M.; Gruber-Baldini, A.L.; Anderson, K.E.; Fishman, P.S.; Reich, S.G.; Weiner, W.J. The clinically important difference on the unified parkinson’s disease rating scale. Arch. Neurol. 2010, 67, 64–70. [Google Scholar] [CrossRef] [PubMed]
- Tinetti, M.E. Performance-oriented assessment of mobility problems in elderly patients. J. Am. Geriatr. Soc. 1986, 34, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Mathias, S.; Nayak, U.S.; Isaacs, B. Balance in elderly patients: The “get-up and go” test. Arch. Phys. Med. Rehabil. 1986, 67, 387–389. [Google Scholar]
- Podsiadlo, D.; Richardson, S. The timed “up & go”: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar]
- Dibble, L.E.; Lange, M. Predicting falls in individuals with parkinson disease: A reconsideration of clinical balance measures. J. Neurol. Phys. Ther. 2006, 30, 60–67. [Google Scholar] [CrossRef]
- Huang, S.L.; Hsieh, C.L.; Wu, R.M.; Tai, C.H.; Lin, C.H.; Lu, W.S. Minimal detectable change of the timed “up & go” test and the dynamic gait index in people with parkinson disease. Phys. Ther. 2011, 91, 114–121. [Google Scholar]
- Peto, V.; Jenkinson, C.; Fitzpatrick, R. Pdq-39: A review of the development, validation and application of a parkinson’s disease quality of life questionnaire and its associated measures. J. Neurol. 1998, 245, S10–S14. [Google Scholar] [CrossRef]
- Bang, D.H.; Shin, W.S. Effects of an intensive nordic walking intervention on the balance function and walking ability of individuals with parkinson’s disease: A randomized controlled pilot trial. Aging Clin. Exp. Res. 2017, 29, 993–999. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, E.P.; Franzoni, L.T.; Cubillos, D.M.; De Oliveira Fagundes, A.; Carvalho, A.R.; Oliveira, H.B.; Pantoja, P.D.; Schuch, F.B.; Rieder, C.R.; Martinez, F.G.; et al. Effects of nordic walking training on functional parameters in parkinson’s disease: A randomized controlled clinical trial. Scand. J. Med. Sci. Sports 2017, 27, 351–358. [Google Scholar] [CrossRef]
- Ebersbach, G.; Ebersbach, A.; Edler, D.; Kaufhold, O.; Kusch, M.; Kupsch, A.; Wissel, J. Comparing exercise in parkinson’s disease--the berlin lsvt(r)big study. Mov. Disord. 2010, 25, 1902–1908. [Google Scholar] [CrossRef] [PubMed]
- Horvath, K.; Aschermann, Z.; Kovacs, M.; Makkos, A.; Harmat, M.; Janszky, J.; Komoly, S.; Karadi, K.; Kovacs, N. Changes in quality of life in parkinson’s disease: How large must they be to be relevant? Neuroepidemiology 2017, 48, 1–8. [Google Scholar] [CrossRef]
- Nonnekes, J.; Nieuwboer, A. Towards personalized rehabilitation for gait impairments in parkinson’s disease. J. Parkinsons Dis. 2018, 8, S101–S106. [Google Scholar] [CrossRef] [PubMed]
- Dipasquale, S.; Meroni, R.; Sasanelli, F.; Messineo, I.; Piscitelli, D.; Perin, C.; Cornaggia, C.M.; Cerri, C.G. Physical therapy versus a general exercise programme in patients with hoehn yahr stage ii parkinson’s disease: A randomized controlled trial. J. Parkinsons Dis. 2017, 7, 203–210. [Google Scholar] [CrossRef] [PubMed]
- Muhlack, S.; Welnic, J.; Woitalla, D.; Muller, T. Exercise improves efficacy of levodopa in patients with parkinson’s disease. Mov. Disord. 2007, 22, 427–430. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Harmer, P.; Fitzgerald, K.; Eckstrom, E.; Stock, R.; Galver, J.; Maddalozzo, G.; Batya, S.S. Tai chi and postural stability in patients with parkinson’s disease. N. Engl. J. Med. 2012, 366, 511–519. [Google Scholar] [CrossRef]
- Morris, M.E.; Menz, H.B.; McGinley, J.L.; Watts, J.J.; Huxham, F.E.; Murphy, A.T.; Danoudis, M.E.; Iansek, R. A randomized controlled trial to reduce falls in people with parkinson’s disease. Neurorehabilit. Neural Repair 2015, 29, 777–785. [Google Scholar] [CrossRef]
- Silva-Batista, C.; Corcos, D.M.; Kanegusuku, H.; Piemonte, M.E.P.; Gobbi, L.T.B.; De Lima-Pardini, A.C.; De Mello, M.T.; Forjaz, C.L.M.; Ugrinowitsch, C. Balance and fear of falling in subjects with parkinson’s disease is improved after exercises with motor complexity. Gait Posture 2018, 61, 90–97. [Google Scholar] [CrossRef]
- Shen, X.; Wong-Yu, I.S.; Mak, M.K. Effects of exercise on falls, balance, and gait ability in parkinson’s disease: A meta-analysis. Neurorehabilit. Neural Repair 2016, 30, 512–527. [Google Scholar] [CrossRef] [PubMed]
- Bombieri, F.; Schena, F.; Pellegrini, B.; Barone, P.; Tinazzi, M.; Erro, R. Walking on four limbs: A systematic review of nordic walking in parkinson disease. Parkinsonism Relat. Disord. 2017, 38, 8–12. [Google Scholar] [CrossRef] [PubMed]
- Keus, S.H.; Bloem, B.R.; Hendriks, E.J.; Bredero-Cohen, A.B.; Munneke, M.; Practice Recommendations Development, G. Evidence-based analysis of physical therapy in parkinson’s disease with recommendations for practice and research. Mov. Disord. 2007, 22, 451–460. [Google Scholar] [CrossRef] [PubMed]
- Cerri, S.; Mus, L.; Blandini, F. Parkinson’s disease in women and men: What’s the difference? J. Parkinsons Dis. 2019, 9, 501–515. [Google Scholar] [CrossRef]
- Goetz, C.G.; Tilley, B.C.; Shaftman, S.R.; Stebbins, G.T.; Fahn, S.; Martinez-Martin, P.; Poewe, W.; Sampaio, C.; Stern, M.B.; Dodel, R.; et al. Movement disorder society-sponsored revision of the unified parkinson’s disease rating scale (mds-updrs): Scale presentation and clinimetric testing results. Mov. Disord. 2008, 23, 2129–2170. [Google Scholar] [CrossRef]
| NW N = 20 | SR N = 20 | |
|---|---|---|
| Women, n (%) | 10 (50.0) | 10 (50.0) |
| Age, years | 62.5 (50–75) | 65.5 (54–75) |
| Age at onset, years | 56.5 (35–70) | 59.0 (45–72) |
| Duration of treatment, years | 6.0 (3–18) | 5.0 (2–14) |
| Hoehn and Yahr stage, n (%) | II, 9 (45.0) III, 11 (55.0) | II, 11 (55.0) III, 9 (45.0) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szefler-Derela, J.; Arkuszewski, M.; Knapik, A.; Wasiuk-Zowada, D.; Gorzkowska, A.; Krzystanek, E. Effectiveness of 6-Week Nordic Walking Training on Functional Performance, Gait Quality, and Quality of Life in Parkinson’s Disease. Medicina 2020, 56, 356. https://doi.org/10.3390/medicina56070356
Szefler-Derela J, Arkuszewski M, Knapik A, Wasiuk-Zowada D, Gorzkowska A, Krzystanek E. Effectiveness of 6-Week Nordic Walking Training on Functional Performance, Gait Quality, and Quality of Life in Parkinson’s Disease. Medicina. 2020; 56(7):356. https://doi.org/10.3390/medicina56070356
Chicago/Turabian StyleSzefler-Derela, Justyna, Michal Arkuszewski, Andrzej Knapik, Dagmara Wasiuk-Zowada, Agnieszka Gorzkowska, and Ewa Krzystanek. 2020. "Effectiveness of 6-Week Nordic Walking Training on Functional Performance, Gait Quality, and Quality of Life in Parkinson’s Disease" Medicina 56, no. 7: 356. https://doi.org/10.3390/medicina56070356
APA StyleSzefler-Derela, J., Arkuszewski, M., Knapik, A., Wasiuk-Zowada, D., Gorzkowska, A., & Krzystanek, E. (2020). Effectiveness of 6-Week Nordic Walking Training on Functional Performance, Gait Quality, and Quality of Life in Parkinson’s Disease. Medicina, 56(7), 356. https://doi.org/10.3390/medicina56070356





