A Nutraceutical Approach to Menopausal Complaints
Abstract
1. Introduction
2. Treatment Approaches
3. Phytoestrogens
Isoflavones
4. Herbal Derivatives
4.1. Actaea racemosa
4.2. Evening Primrose Oil
4.3. Foeniculum vulgare
4.4. Ginkgo biloba
4.5. Glycyrrhiza glabra
4.6. Hypericum perforatum
4.7. Medicago sativa
4.8. Melissa officinalis
4.9. Panax ginseng
4.10. Passiflora incarnata
4.11. Pimpinella anisum
4.12. Salvia officinalis
4.13. Trifolium pretense
4.14. Trigonella foenum
4.15. Valerian officinalis
4.16. Vitex agnus-castus
5. Vitamins
6. Other Compounds
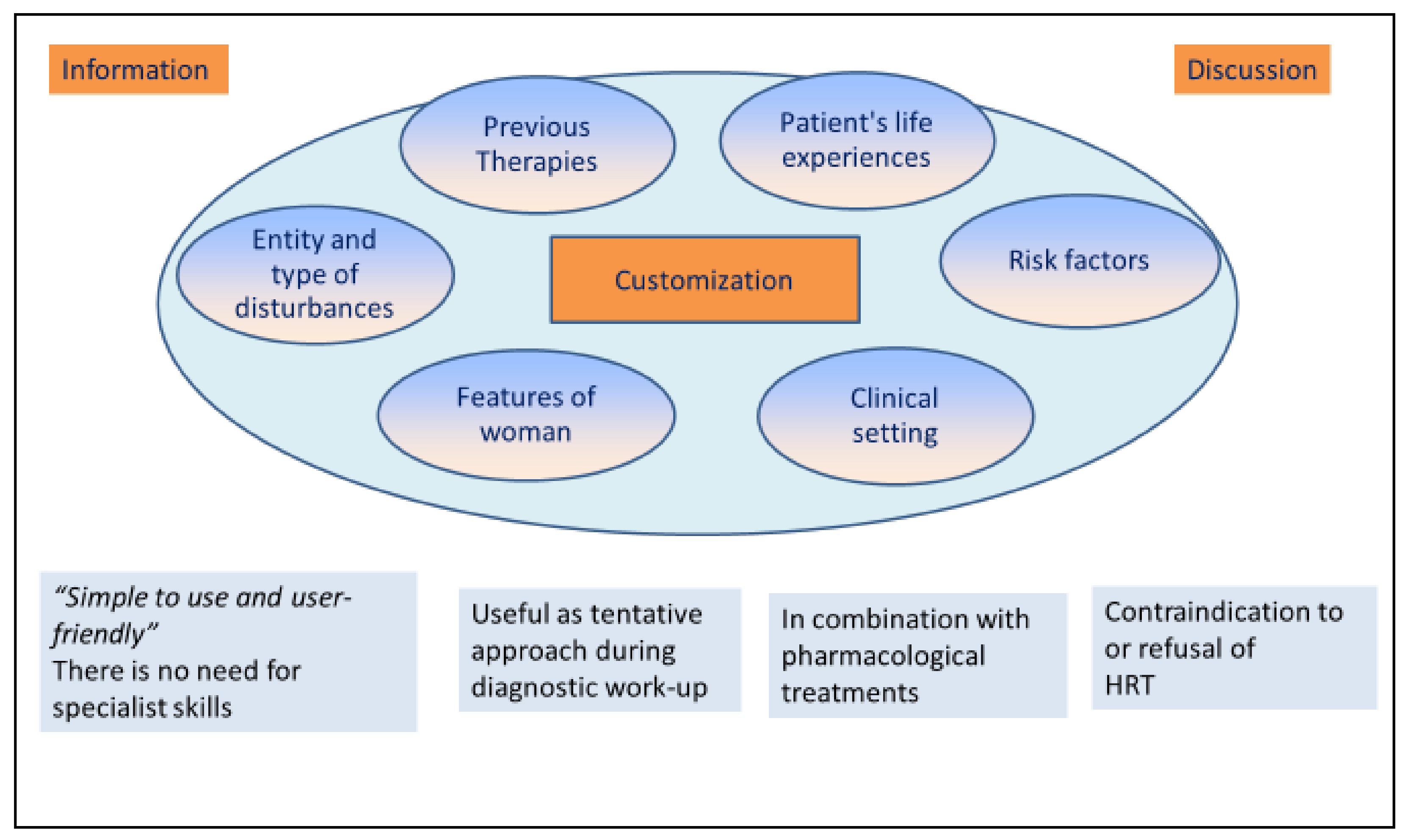
7. Discussion
8. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Soules, M.R.; Sherman, S.; Parrott, E.; Rebar, R.; Santoro, N.; Utian, W.; Woods, N. Executive summary: Stages of reproductive aging workshop (STRAW). Fertil. Steril. 2001, 76, 874–878. [Google Scholar] [CrossRef]
- Bajwa, S.; Singh, A.; Bajwa, S.J. Nutritional facts and menopausal symptomatology: The role of nutraceuticals. J. Med. Nutr. Nutraceuticals 2012, 1, 42–49. [Google Scholar] [CrossRef]
- Ainsworth, A.J.; Baumgarten, S.C.; Bakkum-Gamez, J.N.; Vachon, C.M.; Weaver, A.L.; Laughlin-Tommaso, S.K. Tubal Ligation and Age at Natural Menopause. Obstet. Gynecol. 2019, 133, 1247–1254. [Google Scholar] [CrossRef] [PubMed]
- Li, R.-L.; Shen, X.-L.; Xu, F.; Shui, X.-J.; Chen, Y.-M.; Wang, W.-H.; Zheng, J.-Y. Evaluation of ovarian function using three dimensional ultrasound in perimenopausal women. Gynecol. Endocrinol. 2019. [Google Scholar] [CrossRef] [PubMed]
- De Franciscis, P.; Cobellis, L.; Fornaro, F.; Sepe, E.; Torella, M.; Colacurci, N. Low-dose hormone therapy in the perimenopause. Int. J. Gynecol. Obstet. 2007, 98, 138–142. [Google Scholar] [CrossRef] [PubMed]
- Jutras, M.L.; Cowan, B.D. Abnormal bleeding in the climacteric. Obstet. Gynecol. Clin. N. Am. 1990, 17, 409–425. [Google Scholar]
- Gregersen, N.; Jensen, P.T.; Giraldi, A.E. Sexual dysfunction in the peri- and postmenopause. Status of incidence, pharmacological treatment and possible risks. A secondary publication. Dan. Med. Bull. 2006, 53, 349–353. [Google Scholar] [PubMed]
- Hill, D.A.; Crider, M.; Hill, S.R. Hormone Therapy and Other Treatments for Symptoms of Menopause. Am. Fam. Physician. 2016, 94, 884–889. [Google Scholar]
- Santoro, N. Perimenopause: From Research to Practice. J. Women Health 2016, 25, 332–339. [Google Scholar] [CrossRef]
- The NAMS 2017 Hormone Therapy Position Statement Advisory Panel. The 2017 hormone therapy position statement of The North American Menopause Society. Menopause 2017, 24, 728–753. [Google Scholar] [CrossRef]
- Manson, J.E.; Chlebowski, R.T.; Stefanick, M.L.; Aragaki, A.K.; Rossouw, J.E.; Prentice, R.L.; Anderson, G.; Howard, B.V.; Thomson, C.A.; LaCroix, A.Z.; et al. Menopausal hormone therapy and health outcomes during the intervention and extended poststopping phases of the Women’s Health Initiative randomized trials. JAMA 2013, 310, 1353–1368. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Ho, S.C.; Xie, Y.J.; Chen, Y.; Chen, Y.; Chen, B.; Wong, S.Y.; Chan, D.; Wong, C.K.; He, Q.; et al. Associations between dietary patterns and psychological factors: A cross-sectional study among Chinese postmenopausal women. Menopause 2016, 23, 1294–1302. [Google Scholar] [CrossRef] [PubMed]
- Marsden, J. British Menopause Society consensus statement: The risks and benefits of HRT before and after a breast cancer diagnosis. Post Reprod. Health 2019, 25, 33–37. [Google Scholar] [CrossRef] [PubMed]
- Marjoribanks, J.; Farquhar, C.; Roberts, H.; Lethaby, A.; Lee, J. Long-term hormone therapy for perimenopausal and postmenopausal women. Cochrane Database Syst. Rev. 2017, 1, CD004143. [Google Scholar] [CrossRef] [PubMed]
- Gurney, E.P.; Nachtigall, M.J.; Nachtigall, L.E.; Naftolin, F. The Women’s Health Initiative trial and related studies: 10 years later: A clinician’s view. J. Steroid Biochem. Mol. Biol. 2014, 142, 4–11. [Google Scholar] [CrossRef] [PubMed]
- Ramaa, C.S.; Shirode, A.R.; Mundada, A.S.; Kadam, V.J. Nutraceuticals—An emerging era in the treatment and prevention of cardiovascular diseases. Curr. Pharm. Biotechnol. 2006, 7, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Aronson, J.K. Defining “nutraceuticals”: Neither nutritious nor pharmaceutical. Br. J. Clin. Pharmacol. 2017, 83, 8–19. [Google Scholar] [CrossRef] [PubMed]
- Coppens, P.; Da Silva, M.F.; Pettman, S. European regulations on nutraceuticals, dietary supplements and functional foods: A framework based on safety. Toxicology 2006, 221, 59–74. [Google Scholar] [CrossRef] [PubMed]
- Watts, N.B.; Bilezikian, J.P.; Camacho, P.M.; Greenspan, S.L.; Harris, S.T.; Hodgson, S.F.; Kleerekoper, M.; Luckey, M.M.; McClung, M.R.; Pollack, R.P.; et al. American Association of Clinical Endocrinologists medical guidelines for clinical practice for the prevention and treatment of postmenopausal osteoporosis. Endocr. Pract. 2003, 9, 544–564. [Google Scholar]
- Sullivan, S.D.; Sarrel, P.M.; Nelson, L.M. Hormone replacement therapy in young women with primary ovarian insufficiency and early menopause. Fertil. Steril. 2016, 106, 1588–1599. [Google Scholar] [CrossRef]
- Lethaby, A.; Ayeleke, R.O.; Roberts, H. Local oestrogen for vaginal atrophy in postmenopausal women. Cochrane Database Syst. Rev. 2016. [Google Scholar] [CrossRef] [PubMed]
- Torgerson, D.J.; Bell-Syer, S.E. Hormone replacement therapy and prevention of nonvertebral fractures: A meta-analysis of randomized trials. JAMA 2001, 285, 2891–2897. [Google Scholar] [CrossRef] [PubMed]
- Maclennan, A.H.; Broadbent, J.L.; Lester, S.; Moore, V. Oral oestrogen and combined oestrogen/progestogen therapy versus placebo for hot flushes. Cochrane Database Syst. Rev. 2004. [Google Scholar] [CrossRef] [PubMed]
- Writing Group for the Women’s Health Initiative Investigators. Risks and Benefits of Estrogen Plus Progestin in Healthy Postmenopausal Women: Principal Results From the Women’s Health Initiative Randomized Controlled Trial. JAMA 2002, 288, 321–333. [Google Scholar] [CrossRef] [PubMed]
- Tariverdian, N.; Theoharides, T.C.; Siedentopf, F.; Gutierrez, G.; Jeschke, U.; Rabinovich, G.A.; Blois, S.M.; Arck, P.C. Neuroendocrine-immune disequilibrium and endometriosis: An interdisciplinary approach. Semin. Immunopathol. 2007, 29, 193–210. [Google Scholar] [CrossRef] [PubMed]
- Tit, D.M.; Bungau, S.; Iovan, C.; Cseppento, D.C.N.; Endres, L.; Sava, C.; Sabau, A.M.; Furau, G.; Furau, C. Effects of the Hormone Replacement Therapy and of Soy Isoflavones on Bone Resorption in Postmenopause. J. Clin. Med. 2018, 7, 297. [Google Scholar] [CrossRef] [PubMed]
- Peng, L.; Luo, Q.; Lu, H. Efficacy and safety of bazedoxifene in postmenopausal women with osteoporosis: A systematic review and meta-analysis. Medicine 2017, 96, e8659. [Google Scholar] [CrossRef]
- Conjugated oestrogens/bazedoxifene for menopause. Aust. Prescr. 2017, 40, 114–115. [CrossRef]
- LaCroix, A.Z.; Chlebowski, R.T.; Manson, J.E.; Aragaki, A.K.; Johnson, K.C.; Martin, L.; Margolis, K.L.; Stefanick, M.L.; Brzyski, R.; Curb, J.D.; et al. Health Outcomes after Stopping Conjugated Equine Estrogens Among Postmenopausal Women with Prior Hysterectomy. JAMA 2011, 305, 1305–1314. [Google Scholar] [CrossRef]
- Lobo, R.A. Hormone-replacement therapy: current thinking. Nat. Rev. Endocrinol. 2017, 13, 220–231. [Google Scholar] [CrossRef]
- De Franciscis, P.; Mainini, G.; Messalli, E.M.; Trotta, C.; Luisi, A.; Laudando, E.; Marino, G.; Della Puca, G.; Cerreto, F.V.; Torella, M. Arterial hypertension and female sexual dysfunction in postmenopausal women. Clin. Exp. Obstet. Gynecol. 2013, 40, 58–60. [Google Scholar] [PubMed]
- Johansen, N.; Liavaag, A.H.; Iversen, O.-E.; Dørum, A.; Braaten, T.; Michelsen, T.M. Use of hormone replacement therapy after risk-reducing salpingo-oophorectomy. Acta Obstet. Gynecol. Scand. 2017, 96, 547–555. [Google Scholar] [CrossRef] [PubMed]
- Gemmell, L.; Webster, K.; Kirtley, S.; Vincent, K.; Zondervan, K.; Becker, C. The management of menopause in women with a history of endometriosis: A systematic review. Hum. Reprod. Updat. 2017, 23, 481–500. [Google Scholar] [CrossRef] [PubMed]
- Campitiello, M.R.; De Franciscis, P.; Mele, D.; Izzo, G.; Sinisi, A.; DelRio, G.; Colacurci, N. Endometrial LGR7 expression during menstrual cycle. Fertil. Steril. 2011, 95, 2511–2514. [Google Scholar] [CrossRef] [PubMed]
- Siciliano, R.A.; Mazzeo, M.F.; Spada, V.; Facchiano, A.; D’Acierno, A.; Stocchero, M.; De Franciscis, P.; Colacurci, N.; Sannolo, N.; Miraglia, N. Rapid peptidomic profiling of peritoneal fluid by MALDI-TOF mass spectrometry for the identification of biomarkers of endometriosis. Gynecol. Endocrinol. 2014, 30, 872–876. [Google Scholar] [CrossRef] [PubMed]
- Donati, S.; Cotichini, R.; Mosconi, P.; Satolli, R.; Colombo, C.; Donati, S.; Cotichini, R.; Mosconi, P.; Satolli, R.; Colombo, C.; et al. Menopausa e terapia ormonale: Indagine su conoscenza, atteggiamenti e comportamenti; Istituto Superiore di Sanità: Roma, Italy, 2008; (Rapporti ISTISAN 08/28). [Google Scholar]
- Das, L.; Bhaumik, E.; Raychaudhuri, U.; Chakraborty, R. Role of nutraceuticals in human health. J. Food Sci. Technol. 2012, 49, 173–183. [Google Scholar] [CrossRef] [PubMed]
- Nonhormonal management of menopause-associated vasomotor symptoms: 2015 position statement of The North American Menopause Society. Menopause 2015, 22, 1155–1174. [CrossRef]
- Gambacciani, M.; Cagnacci, A.; Lello, S. Hormone replacement therapy and prevention of chronic conditions. Climacteric 2019, 22, 303–306. [Google Scholar] [CrossRef]
- Mosconi, P.; Donati, S.; Colombo, C.; Mele, A.; Liberati, A.; Satolli, R. Informing women about hormone replacement therapy: The consensus conference statement. BMC Women Health 2009, 9, 14. [Google Scholar] [CrossRef]
- Nicoletti, M. Nutraceuticals and botanicals: Overview and perspectives. Int. J. Food Sci. Nutr. 2012, 63, 2–6. [Google Scholar] [CrossRef]
- Santini, A.; Cammarata, S.M.; Capone, G.; Ianaro, A.; Tenore, G.C.; Pani, L.; Novellino, E. Nutraceuticals: Opening the debate for a regulatory framework. Br. J. Clin. Pharmacol. 2018, 84, 659–672. [Google Scholar] [CrossRef] [PubMed]
- Brower, V. A nutraceutical a day may keep the doctor away. EMBO Rep. 2005, 6, 708–711. [Google Scholar] [CrossRef] [PubMed]
- Donati, S.; Cotichini, R.; Mosconi, P.; Satolli, R.; Colombo, C.; Liberati, A.; Mele, E.A. Menopause: Knowledge, attitude and practice among Italian women. Maturitas 2009, 63, 246–252. [Google Scholar] [CrossRef] [PubMed]
- Laganà, A.S.; Vitale, S.G.; Stojanovska, L.; Lambrinoudaki, I.; Apostolopoulos, V.; Chiofalo, B.; Rizzo, L.; Basile, F. Preliminary results of a single-arm pilot study to assess the safety and efficacy of visnadine, prenylflavonoids and bovine colostrum in postmenopausal sexually active women affected by vulvovaginal atrophy. Maturitas 2018, 109, 78–80. [Google Scholar] [CrossRef] [PubMed]
- Pinkerton, J.V.; Santen, R.J. Managing vasomotor symptoms in women after cancer. Climacteric 2019. [Google Scholar] [CrossRef] [PubMed]
- Gulati, O.P.; Ottaway, P.B. Legislation relating to nutraceuticals in the European Union with a particular focus on botanical-sourced products. Toxicology 2006, 221, 75–87. [Google Scholar] [CrossRef] [PubMed]
- Lobstein, T.; Davies, S. Defining and labelling ‘healthy’ and ‘unhealthy’ food. Public Health Nutr. 2008, 12, 331–340. [Google Scholar] [CrossRef]
- De Felice, S. The Nutraceutical Evolution: Fueling a Powerful, New International Market. The Foundation for Innovation in Medicine: 1989. Available online: https://fimdefelice.org/library/the-nutraceutical-revolution-fueling-a-powerful-new-international-market/ (accessed on 20 June 2019).
- Takase, H.; Imanishi, K.; Miura, O.; Yumioka, E. A possible mechanism for the gastric mucosal protection by Oren-gedoku-to(OGT), a traditional herbal medicine. Jpn. J. Pharmacol. 1989, 51, 17–23. [Google Scholar] [CrossRef]
- Kobayashi, Y. Kampo Medicine in the New Model Core Curriculum of Pharmaceutical Education. Yakugaku Zasshi 2016, 136, 423–432. [Google Scholar] [CrossRef]
- Ushiroyama, T. The role of traditional Japanese medicine (Kampo) in the practice of psychosomatic medicine: The usefulness of Kampo in the treatment of the stress-related symptoms of women, especially those with peri-menopausal disorder. Biopsychosoc. Med. 2013, 7, 16. [Google Scholar] [CrossRef]
- Tonob, D.; Melby, M.K. Broadening our perspectives on complementary and alternative medicine for menopause: A narrative review. Maturitas 2017, 99, 79–85. [Google Scholar] [CrossRef]
- Kargozar, R.; Azizi, H.; Salari, R. A review of effective herbal medicines in controlling menopausal symptoms. Electron. Physician 2017, 9, 5826–5833. [Google Scholar] [CrossRef] [PubMed]
- Yu, Q. Traditional Chinese medicine: Perspectives on and treatment of menopausal symptoms. Climacteric 2018, 21, 93–95. [Google Scholar] [CrossRef] [PubMed]
- Taylor-Swanson, L.; Thomas, A.; Ismail, R.; Schnall, J.G.; Cray, L.; Mitchell, E.S.; Woods, N.F. Effects of traditional Chinese medicine on symptom clusters during the menopausal transition. Climacteric 2015, 18, 142–156. [Google Scholar] [CrossRef] [PubMed]
- Furukawa, M.; Sakashita, H.; Kamide, M.; Umeda, R. Inhibitory Effects of Kampo Medicine on Epstein-Barr Virus Antigen Induction by Tumor Promoter. Auris Nasus Larynx 1990, 17, 49–54. [Google Scholar] [CrossRef]
- Elkind-Hirsch, K. Effect of dietary phytoestrogens on hot flushes: Can soy-based proteins substitute for traditional estrogen replacement therapy? Menopause 2001, 8, 154–156. [Google Scholar] [CrossRef]
- Jampilek, J.; Kos, J.; Kralova, K. Potential of Nanomaterial Applications in Dietary Supplements and Foods for Special Medical Purposes. Nanomaterials 2019, 9, 296. [Google Scholar] [CrossRef]
- Simonelli, A.; Guadagni, R.; De Franciscis, P.; Colacurci, N.; Pieri, M.; Basilicata, P.; Pedata, P.; Lamberti, M.; Sannolo, N.; Miraglia, N. Environmental and occupational exposure to bisphenol A and endometriosis: Urinary and peritoneal fluid concentration levels. Int. Arch. Occup. Environ. Health 2017, 90, 49–61. [Google Scholar] [CrossRef]
- Newton, K.M.; Reed, S.D.; Lacroix, A.Z.; Grothaus, L.C.; Ehrlich, K.; Guiltinan, J. Treatment of Vasomotor Symptoms of Menopause with Black Cohosh, Multibotanicals, Soy, Hormone Therapy, or Placebo. Ann. Intern. Med. 2006, 145, 869. [Google Scholar] [CrossRef]
- Fait, T. Menopause hormone therapy: Latest developments and clinical practice. Drugs Context 2019, 8, 1–9. [Google Scholar] [CrossRef]
- Thomas, A.J.; Ismail, R.; Taylor-Swanson, L.; Cray, L.; Schnall, J.G.; Mitchell, E.S.; Woods, N.F. Effects of isoflavones and amino acid therapies for hot flashes and co-occurring symptoms during the menopausal transition and early postmenopause: A systematic review. Maturitas 2014, 78, 263–276. [Google Scholar] [CrossRef] [PubMed]
- Roberts, H.; Lethaby, A. Phytoestrogens for menopausal vasomotor symptoms: A Cochrane review summary. Maturitas 2014, 78, 79–81. [Google Scholar] [CrossRef] [PubMed]
- Nettleton, J.A.; Greany, K.A.; Thomas, W.; Wangen, K.E.; Adlercreutz, H.; Kurzer, M.S. The effect of soy consumption on the urinary 2:16-hydroxyestrone ratio in postmenopausal women depends on equol production status but is not influenced by probiotic consumption. J. Nutr. 2005, 135, 603–608. [Google Scholar] [CrossRef] [PubMed]
- Torella, M.; Del Deo, F.; Grimaldi, A.; Iervolino, S.; Pezzella, M.; Tammaro, C.; Gallo, P.; Rappa, C.; De Franciscis, P.; Colacurci, N. Efficacy of an orally administered combination of hyaluronic acid, chondroitin sulfate, curcumin and quercetin for the prevention of recurrent urinary tract infections in postmenopausal women. Eur. J. Obstet. Gynecol. Reprod. Biol. 2016, 207, 125–128. [Google Scholar] [CrossRef] [PubMed]
- Chien, H.-L.; Huang, H.-Y.; Chou, C.-C. Transformation of isoflavone phytoestrogens during the fermentation of soymilk with lactic acid bacteria and bifidobacteria. Food Microbiol. 2006, 23, 772–778. [Google Scholar] [CrossRef] [PubMed]
- Ding, W.; Shah, N. Enhancing the Biotransformation of Isoflavones in Soymilk Supplemented with Lactose Using Probiotic Bacteria during Extended Fermentation. J. Food Sci. 2010, 75, M140–M149. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, A.E.; De Moraes, A.V.G.; Costa-Paiva, L.H.; Pedro, A.O.; Monteiro, N.E.S. Can the use of probiotics in association with isoflavone improve the symptoms of genitourinary syndrome of menopause? Results from a randomized controlled trial. Menopause 2019, 26, 643–652. [Google Scholar] [CrossRef] [PubMed]
- Roozbeh, N.; Kashef, R.; Ghazanfarpour, M.; Kargarfard, L.; Darvish, L.; Khadivzadeh, T.; Dizavandi, F.R.; Afiat, M. Overview of the Effect of Herbal Medicines and Isoflavones on the Treatment of Cognitive Function. J. Menopausal Med. 2018, 24, 113–118. [Google Scholar] [CrossRef]
- Dizavandi, F.R.; Ghazanfarpour, M.; Roozbeh, N.; Kargarfard, L.; Khadivzadeh, T.; Dashti, S. An overview of the phytoestrogen effect on vaginal health and dyspareunia in peri- and post-menopausal women. Post Reprod. Health 2019, 25, 11–20. [Google Scholar] [CrossRef]
- Munro, I.C.; Harwood, M.; Hlywka, J.J.; Stephen, A.M.; Doull, J.; Flamm, W.G.; Adlercreutz, H. Soy Isoflavones: A Safety Review. Nutr. Rev. 2003, 61, 1–33. [Google Scholar] [CrossRef]
- Kheirkhah, M.; Naieri, S.; Tabari, N. The effect of herbal tea capsule on menopause hot flashes. J. Fam. Med. Prim. Care 2018, 7, 1074–1078. [Google Scholar]
- De Smet, P.A. Is there any danger in using traditional remedies? J. Ethnopharmacol. 1991, 32, 43–50. [Google Scholar] [CrossRef]
- Sheehan, D.M. Herbal Medicines, Phytoestrogens and Toxicity: Risk: Benefit Considerations. Exp. Biol. Med. 1998, 217, 379–385. [Google Scholar] [CrossRef] [PubMed]
- Drewe, J.; A Bucher, K.; Zahner, C. A systematic review of non-hormonal treatments of vasomotor symptoms in climacteric and cancer patients. SpringerPlus 2015, 4, 65. [Google Scholar] [CrossRef] [PubMed]
- Xi, S.; Liske, E.; Wang, S.; Liu, J.; Zhang, Z.; Geng, L.; Hu, L.; Jiao, C.; Zheng, S.; Zepelin, H.H.; et al. Effect of Isopropanolic Cimicifuga racemosa Extract on Uterine Fibroids in Comparison with Tibolone among Patients of a Recent Randomized, Double Blind, Parallel-Controlled Study in Chinese Women with Menopausal Symptoms. Evid. Based Complement. Altern. Med. 2014, 2014, 717686. [Google Scholar] [CrossRef]
- Leach, M.J.; Moore, V. Black cohosh (Cimicifuga spp.) for menopausal symptoms. Cochrane Database Syst. Rev. 2012. [Google Scholar] [CrossRef] [PubMed]
- Chenoy, R.; Hussain, S.; Tayob, Y.; O’Brien, P.M.S.; Moss, M.Y.; Morse, P.F. Effect of oral gamolenic acid from evening primrose oil on menopausal flushing. BMJ 1994, 308, 501–503. [Google Scholar] [CrossRef]
- Farzaneh, F.; Fatehi, S.; Sohrabi, M.-R.; Alizadeh, K. The effect of oral evening primrose oil on menopausal hot flashes: A randomized clinical trial. Arch. Gynecol. Obstet. 2013, 288, 1075–1079. [Google Scholar] [CrossRef]
- Ghazanfarpour, M.; Mohammadzadeh, F.; Shokrollahi, P.; Khadivzadeh, T.; Najaf Najafi, M.; Hajirezaee, H.; Afiat, M. Effect of Foeniculum vulgare (fennel) on symptoms of depression and anxiety in postmenopausal women: A double-blind randomised controlled trial. J. Obstet. Gynaecol. 2018, 38, 121–126. [Google Scholar] [CrossRef]
- Javidnia, K.; Dastgheib, L.; Samani, S.M.; Nasiri, A. Antihirsutism activity of Fennel (fruits of Foeniculum vulgare) extract—A double-blind placebo controlled study. Phytomedicine 2003, 10, 455–458. [Google Scholar] [CrossRef]
- Yavangi, M.; Rabiee, S.; Nazari, S.; Farimani-Sanoee, M.; Amiri, I.; Bahmanzadeh, M.; Heidari-Soureshjani, S. Comparison of the Effect of Oestrogen Plus Foeniculum vulgare Seed and Oestrogen alone on Increase in Endometrial Thickness in Infertile Women. J. Clin. Diagn. Res. 2018, 12, QC01–QC04. [Google Scholar] [CrossRef]
- Elsabagh, S.; Hartley, D.E.; File, S.E. Limited cognitive benefits in Stage +2 postmenopausal women after 6 weeks of treatment with Ginkgo biloba. J. Psychopharmacol. 2005, 19, 173–181. [Google Scholar] [CrossRef] [PubMed]
- Pebdani, M.A.; Taavoni, S.; Seyedfatemi, N.; Haghani, H. Triple-blind, placebo-controlled trial of Ginkgo biloba extract on sexual desire in postmenopausal women in Tehran. Iran. J. Nurs. Midwifery Res. 2014, 19, 262–265. [Google Scholar] [PubMed]
- Menati, L.; Khaleghinezhad, K.; Tadayon, M.; Siahpoosh, A. Evaluation of Contextual and Demographic Factors on Licorice Effects on Reducing Hot Flashes in Postmenopause Women. Health Care Women Int. 2014, 35, 87–99. [Google Scholar] [CrossRef] [PubMed]
- Farese, R.V.; Biglieri, E.G.; Shackleton, C.H.L.; Irony, I.; Gomez-Fontes, R. Licorice-Induced Hypermineralocorticoidism. N. Engl. J. Med. 1991, 325, 1223–1227. [Google Scholar] [CrossRef]
- Ghazanfarpour, M.; Sadeghi, R.; Latifnejad Roudsari, R.; Khadivzadeh, T.; Khorsand, I.; Afiat, M.; Esmaeilizadeh, M. Effects of flaxseed and Hypericum perforatum on hot flash, vaginal atrophy and estrogen-dependent cancers in menopausal women: A systematic review and meta-analysis. Avicenna J. Phytomed. 2016, 6, 273–283. [Google Scholar] [PubMed]
- You, M.-K.; Kim, H.-J.; Kook, J.H.; Kim, H.-A., St. John’s Wort Regulates Proliferation and Apoptosis in MCF-7 Human Breast Cancer Cells by Inhibiting AMPK/mTOR and Activating the Mitochondrial Pathway. Int. J. Mol. Sci. 2018, 19, 966. [Google Scholar] [CrossRef]
- Laakmann, E.; Grajecki, D.; Doege, K.; Zu Eulenburg, C.; Bühling, K.J. Efficacy of Cimicifuga racemosa, Hypericum perforatum and Agnus castus in the treatment of climacteric complaints: A systematic review. Gynecol. Endocrinol. 2012, 28, 703–709. [Google Scholar] [CrossRef]
- Liu, Y.-R.; Jiang, Y.-L.; Huang, R.-Q.; Yang, J.-Y.; Xiao, B.-K.; Dong, J.-X. Hypericum perforatum L. preparations for menopause: A meta-analysis of efficacy and safety. Climacteric 2014, 17, 325–335. [Google Scholar] [CrossRef]
- Zhang, C.; Li, Z.; Zhang, C.-Y.; Li, M.; Lee, Y.; Zhang, G.-G. Extract Methods, Molecular Characteristics, and Bioactivities of Polysaccharide from Alfalfa (Medicago sativa L.). Nutrients 2019, 11, 1181. [Google Scholar] [CrossRef]
- De Leo, V.; Lanzetta, D.; Cazzavacca, R.; Morgante, G. Treatment of neurovegetative menopausal symptoms with a phytotherapeutic agent. Minerva Ginecol. 1998, 50, 207–211. [Google Scholar] [PubMed]
- Klerks, M.M.; Van Gent-Pelzer, M.; Franz, E.; Zijlstra, C.; Van Bruggen, A.H.C. Physiological and Molecular Responses of Lactuca sativa to Colonization by Salmonella enterica Serovar Dublin. Appl. Environ. Microbiol. 2007, 73, 4905–4914. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.A.; Kim, O.M.; Rhee, M.S. Changes in microbial contamination levels and prevalence of foodborne pathogens in alfalfa (Medicago sativa) and rapeseed (Brassica napus) during sprout production in manufacturing plants. Lett. Appl. Microbiol. 2013, 56, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, P. Lemon balm—Melissa officinalis; also known as lemon balm, bee balm, garden balm, Melissa, melissengeist. J. Prim. Health Care 2011, 3, 165–166. [Google Scholar] [CrossRef] [PubMed]
- Shakeri, A.; Sahebkar, A.; Javadi, B. Melissa officinalis L.—A review of its traditional uses, phytochemistry and pharmacology. J. Ethnopharmacol. 2016, 188, 204–228. [Google Scholar] [CrossRef] [PubMed]
- Nasri, H.; Rafieian-Kopaei, M. Oxidative Stress and Aging Prevention. Int. J. Prev. Med. 2013, 4, 1101–1102. [Google Scholar] [PubMed]
- Miraj, S.; Rafieian, K.; Kiani, S. Melissa officinalis L: A Review Study with an Antioxidant Prospective. J. Evid. Based Complementary Altern. Med. 2017, 22, 385–394. [Google Scholar] [CrossRef] [PubMed]
- Gurčík, Ľ.; Dúbravská, R.; Miklovičová, J. Economics of the cultivation of Salvia officinalis and Melissa officinalis. Agric. Econ. 2012, 51, 348–356. [Google Scholar] [CrossRef]
- Pérez-Sánchez, A.; Barrajón-Catalán, E.; Herranz-López, M.; Castillo, J.; Micol, V. Lemon balm extract (Melissa officinalis, L.) promotes melanogenesis and prevents UVB-induced oxidative stress and DNA damage in a skin cell model. J. Dermatol. Sci. 2016, 84, 169–177. [Google Scholar] [CrossRef]
- Shergis, J.L.; Zhang, A.L.; Zhou, W.; Xue, C.C. Panax ginseng in Randomised Controlled Trials: A Systematic Review. Phyther. Res. 2013, 27, 949–965. [Google Scholar] [CrossRef]
- Lee, K.J.; Ji, G.E. The effect of fermented red ginseng on depression is mediated by lipids. Nutr. Neurosci. 2014, 17, 7–15. [Google Scholar] [CrossRef]
- Leung, K.W.; Cheung, L.W.T.; Pon, Y.L.; Wong, R.N.S.; Mak, N.K.; Fan, T.-P.; Au, S.C.L.; Tombran-Tink, J.; Wong, A.S.T. Ginsenoside Rb1 inhibits tube-like structure formation of endothelial cells by regulating pigment epithelium-derived factor through the oestrogen β receptor. Br. J. Pharmacol. 2007, 152, 207–215. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.; Park, W.; Lee, S.; Ahn, W.; Lee, Y. Ginsenoside-Rb1 from Panax ginseng C.A. Meyer Activates Estrogen Receptor-α and -β, Independent of Ligand Binding. J. Clin. Endocrinol. Metab. 2004, 89, 3510–3515. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.W.; Choi, J.; Lee, Y.; Kil, K.-J.; Lee, M.S. Ginseng for managing menopausal woman’s health. Medicine 2016, 95, e4914. [Google Scholar] [CrossRef]
- Miroddi, M.; Calapai, G.; Navarra, M.; Minciullo, P.; Gangemi, S. Passiflora incarnata L.: Ethnopharmacology, clinical application, safety and evaluation of clinical trials. J. Ethnopharmacol. 2013, 150, 791–804. [Google Scholar] [CrossRef]
- Fahami, F.; Asali, Z.; Aslani, A.; Fathizadeh, N. A comparative study on the effects of Hypericum Perforatum and passion flower on the menopausal symptoms of women referring to Isfahan city health care centers. Iran. J. Nurs. Midwifery Res. 2010, 15, 202–207. [Google Scholar] [PubMed]
- Kim, M.; Lim, H.-S.; Lee, H.-H.; Kim, T.-H. Role Identification of Passiflora Incarnata Linnaeus: A Mini Review. J. Menopausal. Med. 2017, 23, 156–159. [Google Scholar] [CrossRef]
- Mosavat, S.H.; Jaberi, A.R.; Sobhani, Z.; Mosaffa-Jahromi, M.; Iraji, A.; Moayedfard, A. Efficacy of Anise (Pimpinella anisum L.) oil for migraine headache: A pilot randomized placebo-controlled clinical trial. J. Ethnopharmacol. 2019, 236, 155–160. [Google Scholar] [CrossRef]
- Nahidi, F.; Kariman, N.; Simbar, M.; Mojab, F. The Study on the Effects of Pimpinella anisum on Relief and Recurrence of Menopausal Hot Flashes. Iran. J. Pharm. Res. 2012, 11, 1079–1085. [Google Scholar]
- Al Mofleh, I.A. Aqueous suspension of anise “Pimpinella anisum” protects rats against chemically induced gastric ulcers. World J. Gastroenterol. 2007, 13, 1112–1118. [Google Scholar] [CrossRef]
- Pontes, V.C.B.; Rodrigues, D.P.; Caetano, A.; Gamberini, M.T.; Rodriguesa, D.P. Preclinical investigation of the cardiovascular actions induced by aqueous extract of Pimpinella anisum L. seeds in rats. J. Ethnopharmacol. 2019, 237, 74–80. [Google Scholar] [CrossRef] [PubMed]
- Tober, C.; Schoop, R. Modulation of neurological pathways by Salvia officinalis and its dependence on manufacturing process and plant parts used. BMC Complement. Altern. Med. 2019, 19, 128. [Google Scholar] [CrossRef]
- Perry, N.; Houghton, P.; Jenner, P.; Keith, A.; Perry, E. Salvia lavandulaefolia essential oil inhibits cholinesterase in vivo. Phytomedicine 2002, 9, 48–51. [Google Scholar] [CrossRef] [PubMed]
- Pereira, O.R.; Catarino, M.D.; Afonso, A.F.; Silva, A.M.S.; Cardoso, S.M. Salvia elegans, Salvia greggii and Salvia officinalis Decoctions: Antioxidant Activities and Inhibition of Carbohydrate and Lipid Metabolic Enzymes. Molecules 2018, 23, 3169. [Google Scholar] [CrossRef]
- Myers, S.; Vigar, V. Effects of a standardised extract of Trifolium pratense (Promensil) at a dosage of 80mg in the treatment of menopausal hot flushes: A systematic review and meta-analysis. Phytomedicine 2017, 24, 141–147. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.A.; Moon, S.-M.; Han, S.H.; Kim, J.-S.; Kim, D.K.; Kim, C.S. The Effect of the Prethanol Extract of Trifolium pratense Leaves on Interleukin-1β-Induced Cartilage Matrix Degradation in Primary Rat Chondrocytes. Cells Tissues Organs 2018, 206, 95–105. [Google Scholar] [CrossRef] [PubMed]
- Ghazanfarpour, M.; Sadeghi, R.; Roudsari, R.L.; Khorsand, I.; Khadivzadeh, T.; Muoio, B. Red clover for treatment of hot flashes and menopausal symptoms: A systematic review and meta-analysis. J. Obstet. Gynaecol. 2016, 36, 301–311. [Google Scholar] [CrossRef]
- Thompson Coon, J.; Pittler, M.H.; Ernst, E. Trifolium pratense isoflavones in the treatment of menopausal hot flushes: A systematic review and meta-analysis. Phytomedicine 2007, 14, 153–159. [Google Scholar] [CrossRef]
- Anjaneyulu, K.; Bhat, K.M.; Srinivasa, S.R.; Devkar, R.A.; Henry, T. Beneficial Role of Hydro-alcoholic Seed Extract of Trigonella foenum graecum on Bone Structure and Strength in Menopause Induced Osteopenia. Ethiop. J. Health Sci. 2018, 28, 787–794. [Google Scholar] [PubMed]
- Steels, E.; Steele, M.L.; Harold, M.; Coulson, S. Efficacy of a Proprietary Trigonella foenum-graecum L. De-Husked Seed Extract in Reducing Menopausal Symptoms in Otherwise Healthy Women: A Double-Blind, Randomized, Placebo-Controlled Study. Phyther. Res. 2017, 31, 1316–1322. [Google Scholar] [CrossRef] [PubMed]
- Mineo, L.; Concerto, C.; Mayorga, T.; Paula, M.; Chusid, E.; Patel, D.; Aguglia, E.; Battaglia, F. Valeriana officinalis Root Extract Modulates Cortical Excitatory Circuits in Humans. Neuropsychobiology 2017, 75, 46–51. [Google Scholar] [CrossRef]
- Occhiuto, F.; Pino, A.; Palumbo, D.R.; Samperi, S.; De Pasquale, R.; Sturlese, E.; Circosta, C.; Pasquale, R. Relaxing effects of Valeriana officinalis extracts on isolated human non-pregnant uterine muscle. J. Pharm. Pharmacol. 2009, 61, 251–256. [Google Scholar] [CrossRef]
- Jenabi, E.; Shobeiri, F.; Hazavehei, S.M.M.; Roshanaei, G. The effect of Valerian on the severity and frequency of hot flashes: A triple-blind randomized clinical trial. Women Health 2018, 58, 297–304. [Google Scholar] [CrossRef] [PubMed]
- Schellenberg, R. Treatment for the premenstrual syndrome with agnus castus fruit extract: Prospective, randomised, placebo controlled study. BMJ 2001, 322, 134–137. [Google Scholar] [CrossRef] [PubMed]
- Dugoua, J.-J.; Seely, D.; Perri, D.; Koren, G.; Mills, E. Safety and efficacy of chastetree (Vitex agnus-castus) during pregnancy and lactation. Can. J. Clin. Pharmacol. 2008, 15, e74–e79. [Google Scholar]
- De Franciscis, P.; Grauso, F.; Luisi, A.; Schettino, M.; Torella, M.; Colacurci, N. Adding Agnus Castus and Magnolia to Soy Isoflavones Relieves Sleep Disturbances Besides Postmenopausal Vasomotor Symptoms-Long Term Safety and Effectiveness. Nutrients 2017, 9, 129. [Google Scholar] [CrossRef] [PubMed]
- Zollman, C.; Vickers, A. ABC of complementary medicine: Complementary medicine in conventional practice. BMJ 1999, 319, 901–904. [Google Scholar] [CrossRef]
- Vashisht, A.; Domoney, C.L.; Cronje, W.; Studd, J.W.W. Prevalence of and satisfaction with complementary therapies and hormone replacement therapy in a specialist menopause clinic. Climacteric 2001, 4, 250–256. [Google Scholar] [CrossRef]
- Parazzini, F. Resveratrol, tryptophanum, glycine and vitamin E: A nutraceutical approach to sleep disturbance and irritability in peri- and post-menopause. Minerva Ginecol. 2015, 67, 1–5. [Google Scholar] [PubMed]
- Golmakani, N.; Parnan Emamverdikhan, A.; Zarifian, A.; Sajadi Tabassi, S.A.; Hassanzadeh, M. Vitamin E as alternative local treatment in genitourinary syndrome of menopause: A randomized controlled trial. Int. Urogynecol. J. 2019, 30, 831–837. [Google Scholar] [CrossRef] [PubMed]
- Laganà, A.S.; Vitale, S.G.; Ban Frangež, H.; Vrtačnik-Bokal, E.; D’Anna, R. Vitamin D in human reproduction: The more, the better? An evidence-based critical appraisal. Eur. Rev. Med. Pharmacol. Sci. 2017, 21, 4243–4251. [Google Scholar] [PubMed]
- Colacurci, N.; Caprio, F.; La Verde, E.; Trotta, C.; Ianniello, R.; Mele, D.; De Franciscis, P. Sequential protocol with urinary-FSH/recombinant-FSH versus standard protocol with recombinant-FSH in women of advanced age undergoing IVF. Gynecol. Endocrinol. 2014, 30, 730–733. [Google Scholar] [CrossRef] [PubMed]
- Paul, C.; Laganà, A.S.; Maniglio, P.; Triolo, O.; Brady, D.M. Inositol’s and other nutraceuticals’ synergistic actions counteract insulin resistance in polycystic ovarian syndrome and metabolic syndrome: State-of-the-art and future perspectives. Gynecol. Endocrinol. 2016, 32, 431–438. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, P.P.; Cangussu, L.; Bueloni-Dias, F.N.; Orsatti, C.L.; Schmitt, E.B.; Nahas-Neto, J.; Nahas, E.A.P. Vitamin D supplementation improves the metabolic syndrome risk profile in postmenopausal women. Climacteric 2019. [Google Scholar] [CrossRef] [PubMed]
- Colonese, F.; Laganà, A.S.; Colonese, E.; Sofo, V.; Salmeri, F.M.; Granese, R.; Triolo, O. The Pleiotropic Effects of Vitamin D in Gynaecological and Obstetric Diseases: An Overview on a Hot Topic. BioMed Res. Int. 2015, 2015, 986281. [Google Scholar] [CrossRef]
- Rizzo, G.; Laganà, A.; Rapisarda, A.; La Ferrera, G.; Buscema, M.; Rossetti, P.; Nigro, A.; Muscia, V.; Valenti, G.; Sapia, F.; et al. Vitamin B12 among Vegetarians: Status, Assessment and Supplementation. Nutrients 2016, 8, 767. [Google Scholar] [CrossRef] [PubMed]
- McCabe, D.; Lisy, K.; Lockwood, C.; Colbeck, M. The impact of essential fatty acid, B vitamins, vitamin C, magnesium and zinc supplementation on stress levels in women: A systematic review. JBI Database Syst. Rev. Implement. Rep. 2017, 15, 402–453. [Google Scholar]
- Sandoval-Ramírez, B.A.; Lamuela-Raventós, R.; Estruch, R.; Sasot, G.; Doménech, M.; Tresserra-Rimbau, A. Beer Polyphenols and Menopause: Effects and Mechanisms—A Review of Current Knowledge. Oxid. Med. Cell. Longev. 2017, 2017, 4749131. [Google Scholar] [CrossRef]
- Terauchi, M.; Horiguchi, N.; Kajiyama, A.; Akiyoshi, M.; Owa, Y.; Kato, K.; Kubota, T. Effects of grape seed proanthocyanidin extract on menopausal symptoms, body composition, and cardiovascular parameters in middle-aged women: A randomized, double-blind, placebo-controlled pilot study. Menopause 2014, 21, 990–996. [Google Scholar] [CrossRef]
- Corzo, L.; Rodriguez, S.; Alejo, R.; Fernandez-Novoa, L.; Aliev, G.; Cacabelos, R. E-MHK-0103 (MineraxinTM): A Novel Nutraceutical with Biological Properties in Menopausal Conditions. Curr. Drug. Metab. 2017, 18, 39–49. [Google Scholar] [CrossRef]
- Erkkola, R.; Vervarcke, S.; Vansteelandt, S.; Rompotti, P.; De Keukeleire, D.; Heyerick, A. A randomized, double-blind, placebo-controlled, cross-over pilot study on the use of a standardized hop extract to alleviate menopausal discomforts. Phytomedicine 2010, 17, 389–396. [Google Scholar] [CrossRef] [PubMed]
- Arranz, S.; Chiva-Blanch, G.; Valderas-Martínez, P.; Medina-Remón, A.; Lamuela-Raventos, R.M.; Estruch, R. Wine, Beer, Alcohol and Polyphenols on Cardiovascular Disease and Cancer. Nutrients 2012, 4, 759–781. [Google Scholar] [CrossRef] [PubMed]
- Gresele, P.; Cerletti, C.; Guglielmini, G.; Pignatelli, P.; De Gaetano, G.; Violi, F. Effects of resveratrol and other wine polyphenols on vascular function: An update. J. Nutr. Biochem. 2011, 22, 201–211. [Google Scholar] [CrossRef] [PubMed]
- Villa, P.; Amar, I.D.; Bottoni, C.; Cipolla, C.; Dinoi, G.; Moruzzi, M.C.; Scambia, G.; Lanzone, A. The impact of combined nutraceutical supplementation on quality of life and metabolic changes during the menopausal transition: A pilot randomized trial. Arch. Gynecol. Obstet. 2017, 296, 791–801. [Google Scholar] [CrossRef] [PubMed]
- Wong, R.H.; Evans, H.M.; Howe, P.R. Resveratrol supplementation reduces pain experience by postmenopausal women. Menopause 2017, 24, 916–922. [Google Scholar] [CrossRef] [PubMed]
- Giolo, J.S.; Costa, J.G.; Da Cunha-Junior, J.P.; Pajuaba, A.C.A.M.; Taketomi, E.A.; De Souza, A.V.; Caixeta, D.C.; Peixoto, L.G.; De Oliveira, E.P.; Everman, S.; et al. The Effects of Isoflavone Supplementation Plus Combined Exercise on Lipid Levels, and Inflammatory and Oxidative Stress Markers in Postmenopausal Women. Nutrients 2018, 10, 424. [Google Scholar] [CrossRef] [PubMed]
- Purdue-Smithe, A.C.; Whitcomb, B.W.; Szegda, K.L.; Boutot, M.E.; Manson, J.E.; Hankinson, S.E.; Rosner, B.A.; Troy, L.M.; Michels, K.B.; Bertone-Johnson, E.R. Vitamin D and calcium intake and risk of early menopause12. Am. J. Clin. Nutr. 2017, 105, 1493–1501. [Google Scholar]
- Mintziori, G.; Lambrinoudaki, I.; Goulis, D.G.; Ceausu, I.; Depypere, H.; Erel, C.T.; Pérez-López, F.R.; Schenck-Gustafsson, K.; Simoncini, T.; Trémollières, F.; et al. EMAS position statement: Non-hormonal management of menopausal vasomotor symptoms. Maturitas 2015, 81, 410–413. [Google Scholar] [CrossRef]
- Woyka, J. Consensus statement for non-hormonal-based treatments for menopausal symptoms. Post Reprod. Health 2017, 23, 71–75. [Google Scholar] [CrossRef]
- Nelson, H.D.; Vesco, K.K.; Haney, E.; Fu, R.; Nedrow, A.; Miller, J.; Nicolaidis, C.; Walker, M.; Humphrey, L. Nonhormonal therapies for menopausal hot flashes: Systematic review and meta-analysis. JAMA 2006, 295, 2057–2071. [Google Scholar] [CrossRef]
- Sassarini, J.; Lumsden, M.A. Non-hormonal management of vasomotor symptoms. Climacteric 2013, 16, 31–36. [Google Scholar] [CrossRef] [PubMed]
| Herbal Derivatives | ||||
|---|---|---|---|---|
| Scientific Name | Common Name | Effects | Side Effects | References |
| Actaea racemosa | Black cohosh | Treatment of menopause symptoms such as hot flash, insomnia, irritability, but also musculoskeletal pain, fever, cough. | Gastrointestinal discomfort. | [76,77] |
| Evening Primrose Oil | Oenothera biennis oil | Treatment for menopausal and premenstrual symptoms, but also for atopic dermatitis and rheumatoid arthritis. | Gastrointestinal disorders and interaction with antiepilectic drugs. | [79,80] |
| Foeniculum vulgare | Fennel | Treatment of hot flashes, anxiety, and vaginal atrophy. | No side effects reported. | [81,82,83] |
| Ginkgo biloba | Ginkgo | Treatment of attention disorders in postmenopausal women. | Gastrointestinal disorders, allergic reactions, headache, and lowering of seizure threshold. | [84,85] |
| Glycyrrhiza glabra | Licorice | Treatment of hot flash duration. | Cardiovascular disease, hypercortisolism, hypokalemia, and hypernatremia. | [86,87] |
| Hypericum perforatum | St. John’s Wort | Treatment for the vasomotor symptoms of postmenopausal women. | Gastrointestinal disease, sensitivity to light, fatigue. | [88,89,90,91] |
| Medicago sativa | Alfalfa | Effect on neurovegetative menopausal symptoms. | Possible infection with Salmonella, Escherichia coli, and Listeria. | [92,93,94,95] |
| Melissa officinalis | Lemon balm, bee balm or honey balm | Effect on anxiety. | No side effect reported. | [96,98,99,100,101] |
| Panax ginseng | Ginseng | Treatment of sleep disorders, depression, and sexual function. | Possible effect on endometrial thickness. | [102,103,104,105,106] |
| Passiflora incarnata | Passion fruit | Treatment of vasomotor symptoms, insomnia, anxiety and dysmenorrhea. | No side effect reported. | [107,108,109] |
| Pimpinella anisum | Anise | Treatment of hot flashes but it also exerts an antiulcer action. | No side effects reported. | [110,111,112,113] |
| Salvia officinalis | Sage herb | Treatment of hot flashes and sweats. | Possible interaction with diabetes and blood pressure. | [114,115,116] |
| Trifolium pretense | Red clover | Treatment of hot flashes and it also exerts a bone preventing loss. | No side effects reported. | [117,118,119,120] |
| Trigonella foenum | Fenugreek | Treatment for hot flashes and osteopenia. | No particularly side effects. | [121,122] |
| Valerian officinalis | Valerian | Useful for hot flashes, anxiety, sleep disorders and dysmenorrhea. | No side effects reported. | [123,124,125] |
| Vitex agnus-castus | Chaste tree, chasteberry or monk’s pepper | Treatment for vasomotor symptoms and sleep diseases. | Not reported. | [126,127,128] |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Franciscis, P.; Colacurci, N.; Riemma, G.; Conte, A.; Pittana, E.; Guida, M.; Schiattarella, A. A Nutraceutical Approach to Menopausal Complaints. Medicina 2019, 55, 544. https://doi.org/10.3390/medicina55090544
De Franciscis P, Colacurci N, Riemma G, Conte A, Pittana E, Guida M, Schiattarella A. A Nutraceutical Approach to Menopausal Complaints. Medicina. 2019; 55(9):544. https://doi.org/10.3390/medicina55090544
Chicago/Turabian StyleDe Franciscis, Pasquale, Nicola Colacurci, Gaetano Riemma, Anna Conte, Erika Pittana, Maurizio Guida, and Antonio Schiattarella. 2019. "A Nutraceutical Approach to Menopausal Complaints" Medicina 55, no. 9: 544. https://doi.org/10.3390/medicina55090544
APA StyleDe Franciscis, P., Colacurci, N., Riemma, G., Conte, A., Pittana, E., Guida, M., & Schiattarella, A. (2019). A Nutraceutical Approach to Menopausal Complaints. Medicina, 55(9), 544. https://doi.org/10.3390/medicina55090544







