Numerical Study on Death of Squamous Cell Carcinoma Based on Various Shapes of Gold Nanoparticles Using Photothermal Therapy
Abstract
:1. Introduction
2. Materials and Methods
2.1. Discrete Dipole Approximation (DDA) Method
2.2. Heat Transfer Model and Optical Properties
2.3. Apoptotic Variables
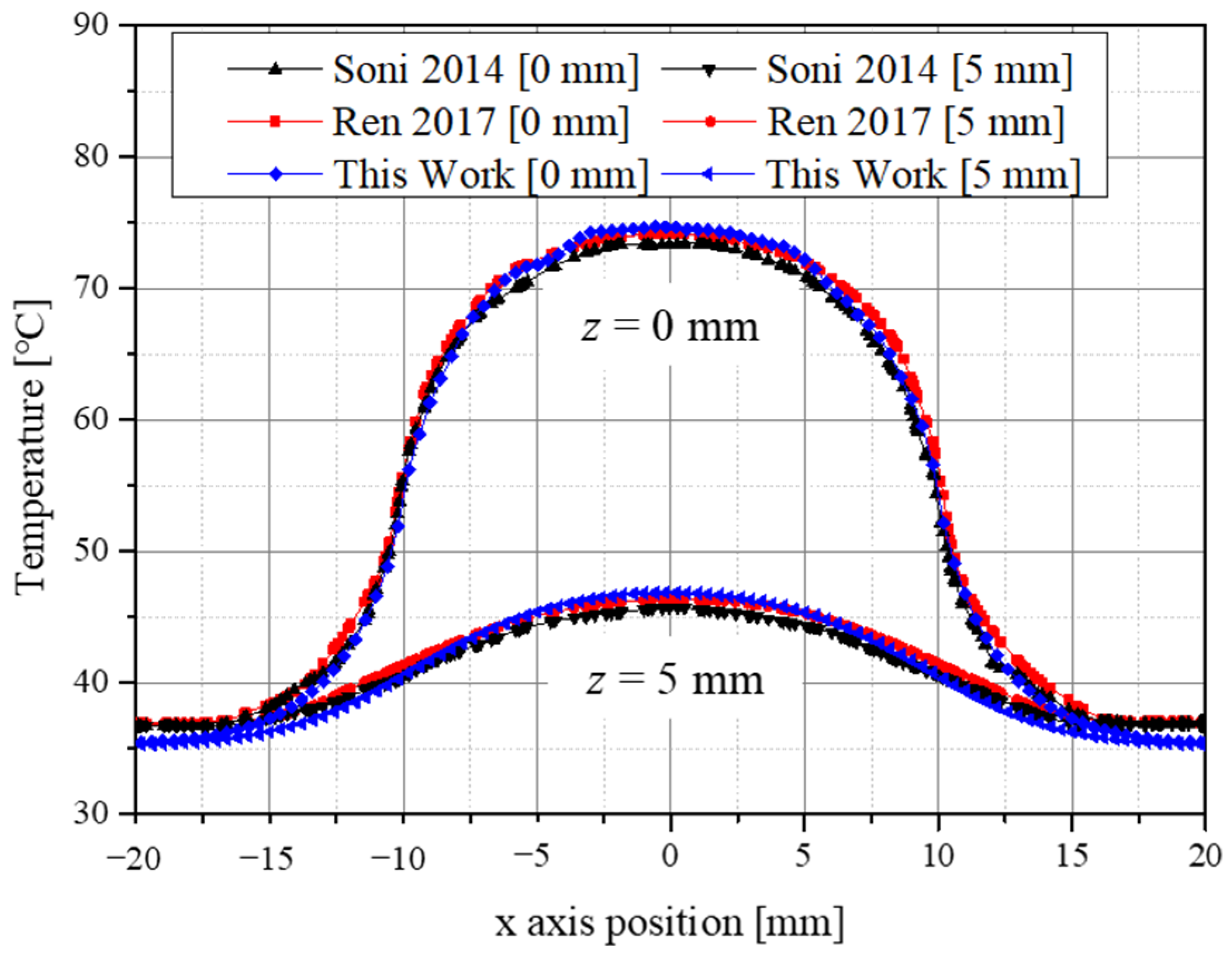
2.4. Validation of Numerical Model
2.5. Numerical Investigation
3. Results
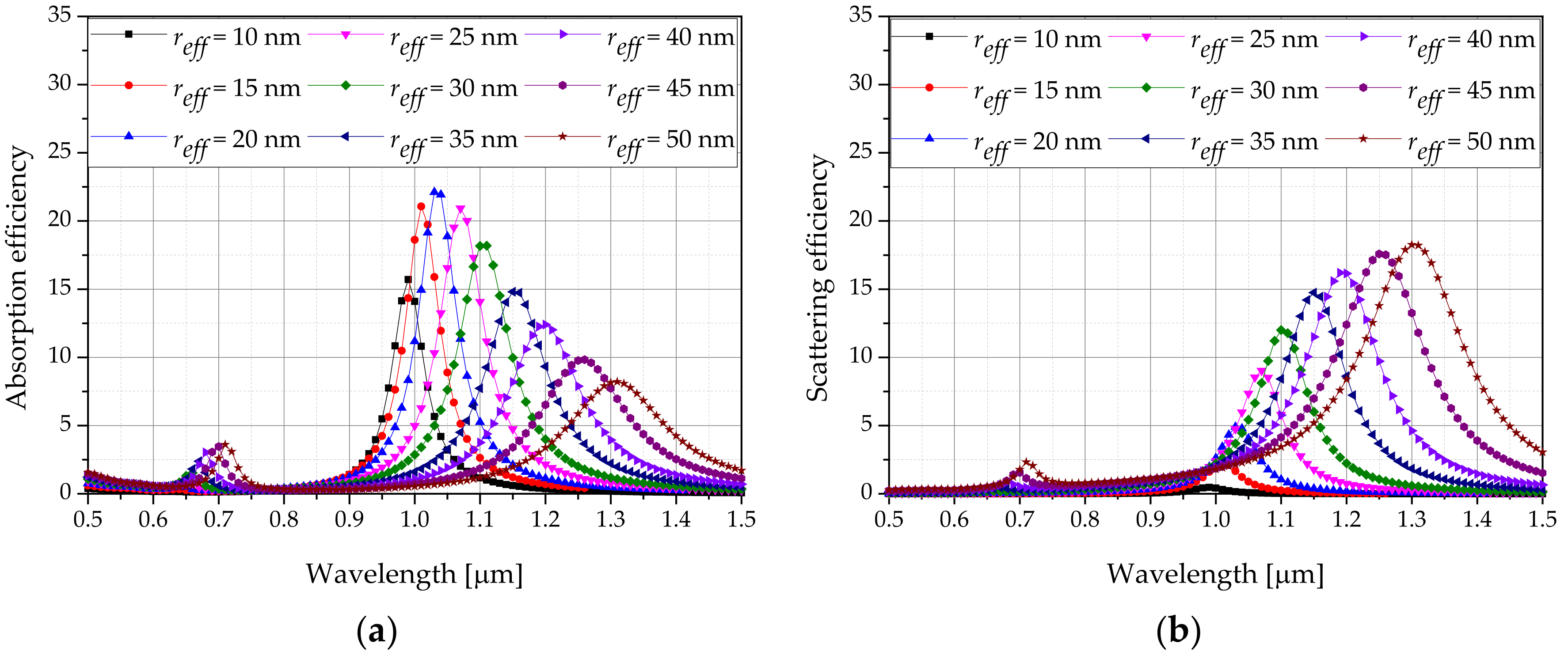
3.1. Derivation of Optical Properties for Various AuNP Types
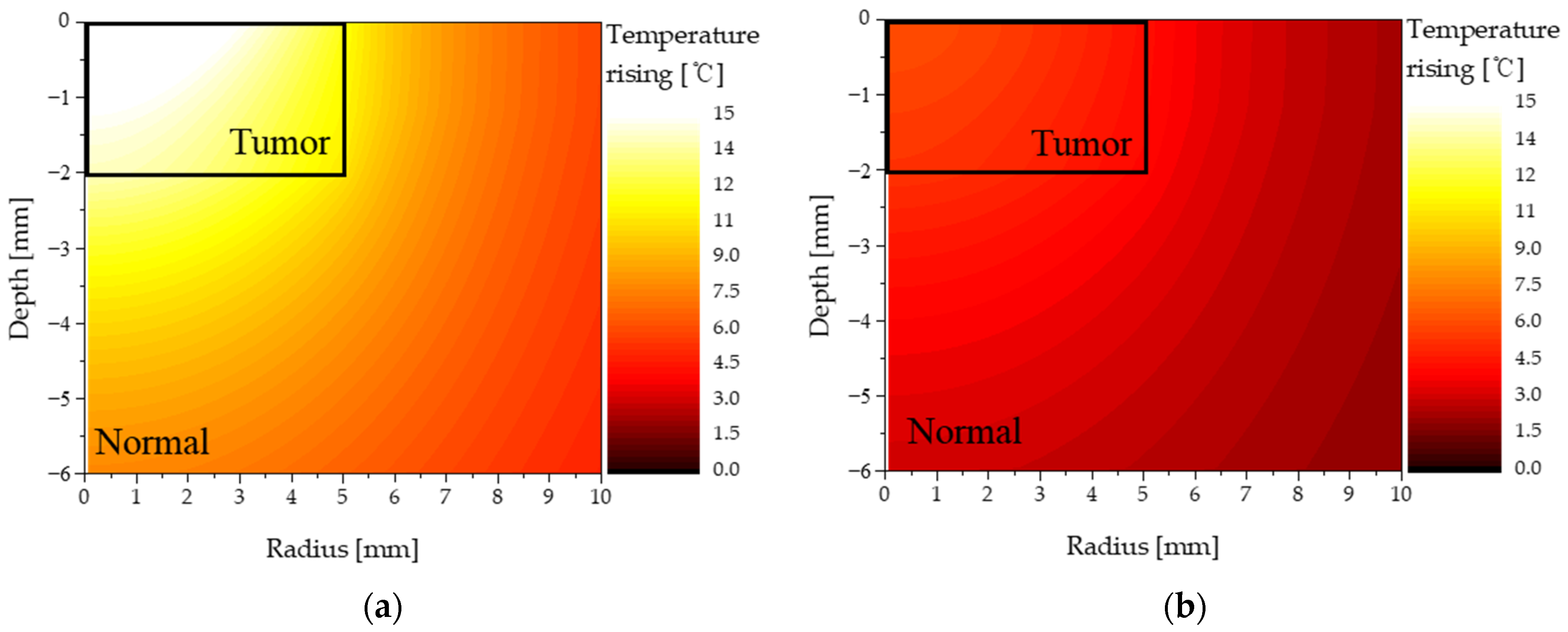
3.2. Temperature of Tumor and Normal Tissues for Various Conditions
3.3. Apoptosis Ratio
3.4. Thermal Hazard Value
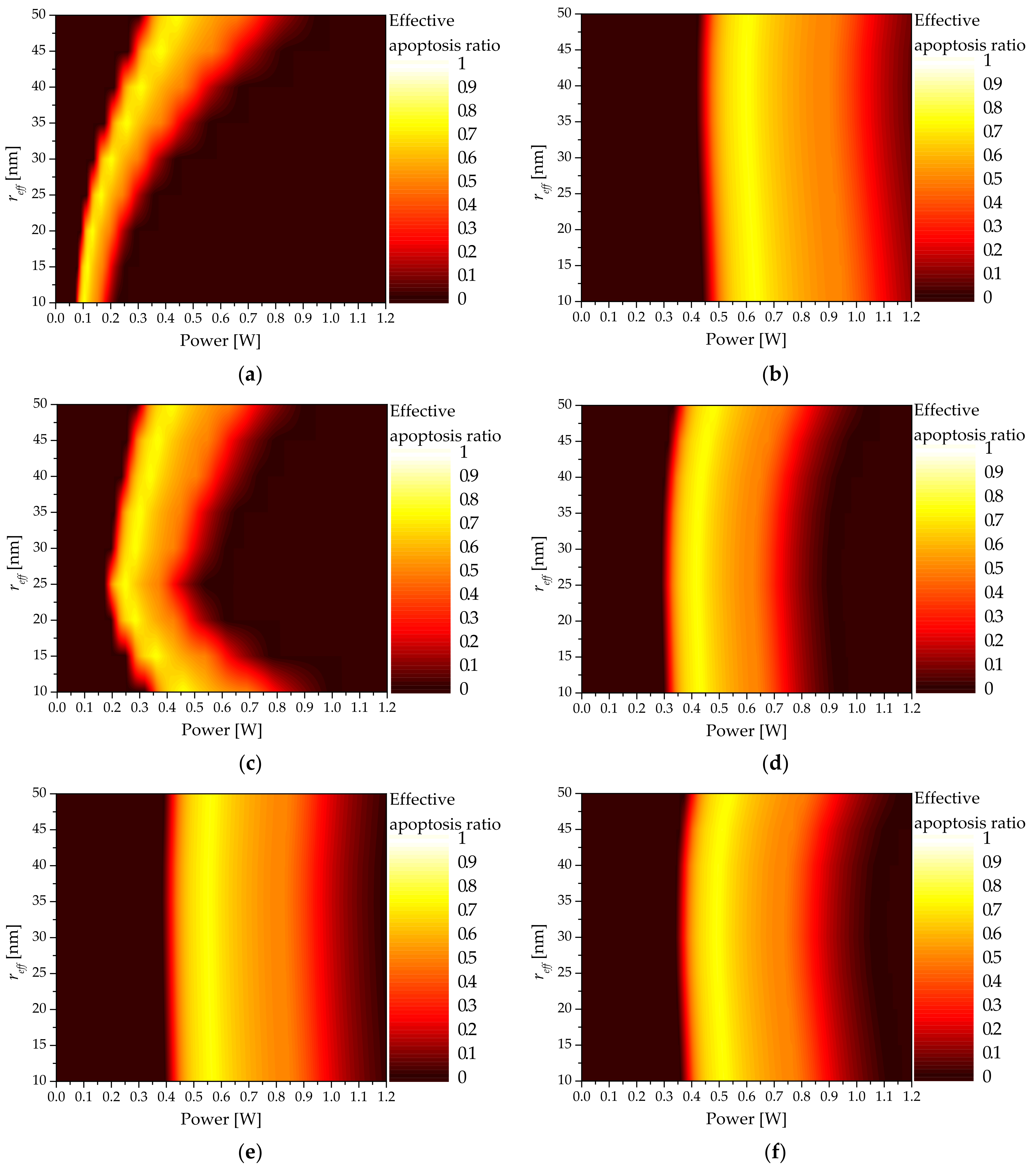
3.5. Effective Apoptosis Ratio
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| C | Cross-section area () |
| Heat capacity () | |
| d | Thickness (m) |
| E | Electric field () |
| Volume fraction of AuNPs | |
| g | Anisotropy factor |
| k | Wavenumber of radiation () |
| Thermal conductivity () | |
| P | Polarization vector () |
| Intensity of laser (W) | |
| q | Volumetric heat source () |
| Q | Dimensionless efficiency factor |
| r | Position vector |
| Effective radius of particle (m) | |
| t | Time (s) |
| T | Temperature (K) |
| V | Volume () |
| w | Weight |
| Greek symbols | |
| Polarizability () | |
| Apoptosis ratio | |
| Thermal hazard value | |
| Effective apoptosis ratio | |
| Wavelength (m) | |
| Optical coefficient (1/m) | |
| Reduced optical coefficient (1/m) | |
| Density () | |
| Subscripts | |
| abs | Absorption |
| b | Blood |
| ext | Extinction |
| l | Laser |
| m | Medium |
| max | Maximum |
| met | Metabolic |
| n | Nano particle |
| sca | Scattering |
| tot | Total |
| x, y, z | Notation of direction |
| Superscripts | |
| * | Complex conjugate |
References
- Skaggs, R.; Coldiron, B. Skin biopsy and skin cancer treatment use in the Medicare population, 1993 to 2016. J. Am. Acad. Dermatol. 2021, 84, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Wei, L.; Christensen, S.R.; Fitzgerald, M.E.; Graham, J.; Hutson, N.D.; Zhang, C.; Huang, Z.; Hu, Q.; Zhan, F.; Xie, J. Ultradeep sequencing differentiates patterns of skin clonal mutations associated with sun-exposure status and skin cancer burden. Sci. Adv. 2021, 7, eabd7703. [Google Scholar] [CrossRef] [PubMed]
- Donati, D.; Brown, S.; Eu, K.; Ho, Y.; Seow-Choen, F. Comparison between midline incision and limited right skin crease incision for right-sided colonic cancers. Tech. Coloproctology 2002, 6, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Holt, P. Cryotherapy for skin cancer: Results over a 5-year period using liquid nitrogen spray cryosurgery. Br. J. Dermatol. 1988, 119, 231–240. [Google Scholar] [CrossRef] [PubMed]
- Kirby, J.S.; Miller, C.J. Intralesional chemotherapy for nonmelanoma skin cancer: A practical review. J. Am. Acad. Dermatol. 2010, 63, 689–702. [Google Scholar] [CrossRef]
- Di Franco, R.; Sammarco, E.; Calvanese, M.G.; De Natale, F.; Falivene, S.; DiLecce, A.; Giugliano, F.M.; Murino, P.; Manzo, R.; Cappabianca, S. Preventing the acute skin side effects in patients treated with radiotherapy for breast cancer: The use of corneometry in order to evaluate the protective effect of moisturizing creams. Radiat. Oncol. 2013, 8, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Kwikkel, H.; Helmerhorst, T.J.; Bezemer, P.; Quaak, M.; Stolk, J. Laser or cryotherapy for cervical intraepithelial neoplasia: A randomized study to compare efficacy and side effects. Gynecol. Oncol. 1985, 22, 23–31. [Google Scholar] [CrossRef]
- Pearce, A.; Haas, M.; Viney, R.; Pearson, S.-A.; Haywood, P.; Brown, C.; Ward, R. Incidence and severity of self-reported chemotherapy side effects in routine care: A prospective cohort study. PLoS ONE 2017, 12, e0184360. [Google Scholar] [CrossRef]
- Johnson, C.; Serpell, J. Wound infection after abdominal incision with scalpel or diathermy. Scalpel 1990, 130, 18–95. [Google Scholar] [CrossRef]
- Lerner, S.F. Small incision trabeculectomy avoiding Tenon’s capsule: A new procedure for glaucoma surgery. Ophthalmology 1997, 104, 1237–1241. [Google Scholar] [CrossRef]
- Huang, X.; El-Sayed, M.A. Plasmonic photo-thermal therapy (PPTT). Alex. J. Med. 2011, 47, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Robinson, J.T.; Tabakman, S.M.; Liang, Y.; Wang, H.; Sanchez Casalongue, H.; Vinh, D.; Dai, H. Ultrasmall reduced graphene oxide with high near-infrared absorbance for photothermal therapy. J. Am. Chem. Soc. 2011, 133, 6825–6831. [Google Scholar] [CrossRef] [PubMed]
- Gurevich, Y.; Logvinov, G.; Lashkevich, I. Effective thermal conductivity: Application to photothermal experiments for the case of bulk light absorption. Phys. Status Solidi (B) 2004, 241, 1286–1298. [Google Scholar] [CrossRef]
- Aamodt, L.; Murphy, J. Thermal effects in photothermal spectroscopy and photothermal imaging. J. Appl. Phys. 1983, 54, 581–591. [Google Scholar] [CrossRef]
- Espinosa, A.; Di Corato, R.; Kolosnjaj-Tabi, J.; Flaud, P.; Pellegrino, T.; Wilhelm, C. Duality of iron oxide nanoparticles in cancer therapy: Amplification of heating efficiency by magnetic hyperthermia and photothermal bimodal treatment. ACS Nano 2016, 10, 2436–2446. [Google Scholar] [CrossRef]
- Abbas, M.; Zou, Q.; Li, S.; Yan, X. Self-assembled peptide-and protein-based nanomaterials for antitumor photodynamic and photothermal therapy. Adv. Mater. 2017, 29, 1605021. [Google Scholar] [CrossRef]
- Huang, X.; El-Sayed, M.A. Gold nanoparticles: Optical properties and implementations in cancer diagnosis and photothermal therapy. J. Adv. Res. 2010, 1, 13–28. [Google Scholar] [CrossRef] [Green Version]
- Salcman, M.; Samaras, G.M. Interstitial microwave hyperthermia for brain tumors. J. Neuro-Oncol. 1983, 1, 225–236. [Google Scholar] [CrossRef]
- Meglinski, I.V.; Matcher, S.J. Quantitative assessment of skin layers absorption and skin reflectance spectra simulation in the visible and near-infrared spectral regions. Physiol. Meas. 2002, 23, 741. [Google Scholar] [CrossRef]
- Khlebtsov, B.; Zharov, V.; Melnikov, A.; Tuchin, V.; Khlebtsov, N. Optical amplification of photothermal therapy with gold nanoparticles and nanoclusters. Nanotechnology 2006, 17, 5167. [Google Scholar] [CrossRef]
- Hwang, S.; Nam, J.; Jung, S.; Song, J.; Doh, H.; Kim, S. Gold nanoparticle-mediated photothermal therapy: Current status and future perspective. Nanomedicine 2014, 9, 2003–2022. [Google Scholar] [CrossRef] [PubMed]
- Li, J.-L.; Gu, M. Gold-nanoparticle-enhanced cancer photothermal therapy. IEEE J. Sel. Top. Quantum Electron. 2009, 16, 989–996. [Google Scholar]
- El-Sayed, I.H.; Huang, X.; El-Sayed, M.A. Selective laser photo-thermal therapy of epithelial carcinoma using anti-EGFR antibody conjugated gold nanoparticles. Cancer Lett. 2006, 239, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Singh, M.; Harris-Birtill, D.C.; Markar, S.R.; Hanna, G.B.; Elson, D.S. Application of gold nanoparticles for gastrointestinal cancer theranostics: A systematic review. Nanomed. Nanotechnol. Biol. Med. 2015, 11, 2083–2098. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- D’Acunto, M.; Cioni, P.; Gabellieri, E.; Presciuttini, G. Exploiting gold nanoparticles for diagnosis and cancer treatments. Nanotechnology 2021, 32, 192001. [Google Scholar] [CrossRef]
- Bucharskaya, A.B.; Maslyakova, G.; Dikht, N.; Navolokin, N.; Terentyuk, G.; Bashkatov, A.; Genina, E.; Khlebtsov, B.; Khlebtsov, N.; Tuchin, V. Plasmonic photothermal therapy of transplanted tumors in rats at multiple intravenous injection of gold nanorods. BioNanoScience 2017, 7, 216–221. [Google Scholar] [CrossRef]
- Wyllie, A.H. Cell death. Cytol. Cell Physiol. 1987, 755–785. [Google Scholar] [CrossRef]
- Song, A.S.; Najjar, A.M.; Diller, K.R. Thermally induced apoptosis, necrosis, and heat shock protein expression in three-dimensional culture. J. Biomech. Eng. 2014, 136, 071006. [Google Scholar] [CrossRef]
- Zhu, X.; Feng, W.; Chang, J.; Tan, Y.-W.; Li, J.; Chen, M.; Sun, Y.; Li, F. Temperature-feedback upconversion nanocomposite for accurate photothermal therapy at facile temperature. Nat. Commun. 2016, 7, 1–10. [Google Scholar] [CrossRef]
- Nam, J.; Son, S.; Ochyl, L.J.; Kuai, R.; Schwendeman, A.; Moon, J.J. Chemo-photothermal therapy combination elicits anti-tumor immunity against advanced metastatic cancer. Nat. Commun. 2018, 9, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Mackey, M.A.; Ali, M.R.; Austin, L.A.; Near, R.D.; El-Sayed, M.A. The most effective gold nanorod size for plasmonic photothermal therapy: Theory and in vitro experiments. J. Phys. Chem. B 2014, 118, 1319–1326. [Google Scholar] [CrossRef] [PubMed]
- Van de Broek, B.; Devoogdt, N.; D’Hollander, A.; Gijs, H.-L.; Jans, K.; Lagae, L.; Muyldermans, S.; Maes, G.; Borghs, G. Specific cell targeting with nanobody conjugated branched gold nanoparticles for photothermal therapy. ACS Nano 2011, 5, 4319–4328. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xi, D.; Xiao, M.; Cao, J.; Zhao, L.; Xu, N.; Long, S.; Fan, J.; Shao, K.; Sun, W.; Yan, X. NIR light-driving barrier-free group rotation in nanoparticles with an 88.3% photothermal conversion efficiency for photothermal therapy. Adv. Mater. 2020, 32, 1907855. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.; Kim, G.; Kim, D.; Yoo, J.; Kim, D.-K.; Kim, H. Numerical study on effective conditions for the induction of apoptotic temperatures for various tumor aspect ratios using a single continuous-wave laser in photothermal therapy using gold nanorods. Cancers 2019, 11, 764. [Google Scholar] [CrossRef] [Green Version]
- Draine, B.T.; Flatau, P.J. Discrete-dipole approximation for periodic targets: Theory and tests. Josa A 2008, 25, 2693–2703. [Google Scholar] [CrossRef] [Green Version]
- Draine, B.T.; Flatau, P.J. Discrete-dipole approximation for scattering calculations. Josa A 1994, 11, 1491–1499. [Google Scholar] [CrossRef]
- Mie, G. Beiträge zur Optik trüber Medien, speziell kolloidaler Metallösungen. Ann. Phys. 1908, 330, 377–445. [Google Scholar] [CrossRef]
- Mie, G. Contributions to the optics of turbid media, particularly of colloidal metal solutions. Contrib. Opt. Turbid Media 1976, 25, 377–445. [Google Scholar]
- Yurkin, M.A.; Hoekstra, A.G.; Brock, R.S.; Lu, J.Q. Systematic comparison of the discrete dipole approximation and the finite difference time domain method for large dielectric scatterers. Opt. Express 2007, 15, 17902–17911. [Google Scholar] [CrossRef] [Green Version]
- Pennes, H.H. Analysis of tissue and arterial blood temperatures in the resting human forearm. J. Appl. Physiol. 1948, 1, 93–122. [Google Scholar] [CrossRef]
- Chang, W.-S.; Na, S.-J. A study on heat source equations for the prediction of weld shape and thermal deformation in laser microwelding. Metall. Mater. Trans. B 2002, 33, 757–764. [Google Scholar] [CrossRef]
- Dombrovsky, L.A.; Timchenko, V.; Jackson, M.; Yeoh, G.H. A combined transient thermal model for laser hyperthermia of tumors with embedded gold nanoshells. Int. J. Heat Mass Transf. 2011, 54, 5459–5469. [Google Scholar] [CrossRef]
- Vera, J.; Bayazitoglu, Y. Gold nanoshell density variation with laser power for induced hyperthermia. Int. J. Heat Mass Transf. 2009, 52, 564–573. [Google Scholar] [CrossRef]
- Kim, D.; Kang, S.; Kim, H. Numerical Study on Factors Affecting the Induction of Apoptotic Temperatures of Tumor in the Multi-Layer Skin Structure Using Monte Carlo Method. Appl. Sci. 2021, 11, 1103. [Google Scholar] [CrossRef]
- Jawad, M.M.; Qader, S.T.A.; Zaidan, A.; Zaidan, B.; Naji, A.; Qader, I.T.A. An overview of laser principle, laser-tissue interaction mechanisms and laser safety precautions for medical laser users. Int. J. Pharmacol. 2011, 7, 149–160. [Google Scholar] [CrossRef]
- Soni, S.; Tyagi, H.; Taylor, R.A.; Kumar, A. Investigation on nanoparticle distribution for thermal ablation of a tumour subjected to nanoparticle assisted thermal therapy. J. Therm. Biol. 2014, 43, 70–80. [Google Scholar] [CrossRef]
- Ren, Y.; Qi, H.; Chen, Q.; Ruan, L. Thermal dosage investigation for optimal temperature distribution in gold nanoparticle enhanced photothermal therapy. Int. J. Heat Mass Transf. 2017, 106, 212–221. [Google Scholar] [CrossRef]
- Salomatina, E.V.; Jiang, B.; Novak, J.; Yaroslavsky, A.N. Optical properties of normal and cancerous human skin in the visible and near-infrared spectral range. J. Biomed. Opt. 2006, 11, 064026. [Google Scholar] [CrossRef]
- Çetingül, M.P.; Herman, C. A heat transfer model of skin tissue for the detection of lesions: Sensitivity analysis. Phys. Med. Biol. 2010, 55, 5933. [Google Scholar] [CrossRef]
- Çetingül, M.P.; Herman, C. Quantification of the thermal signature of a melanoma lesion. Int. J. Therm. Sci. 2011, 50, 421–431. [Google Scholar] [CrossRef]
- Jiang, S.; Ma, N.; Li, H.; Zhang, X. Effects of thermal properties and geometrical dimensions on skin burn injuries. Burns 2002, 28, 713–717. [Google Scholar] [CrossRef]
- Torvi, D.; Dale, J. A finite element model of skin subjected to a flash fire. J. Biomech. Eng. 1994, 116, 250–255. [Google Scholar] [CrossRef] [PubMed]
- Wilson, S.B.; Spence, V.A. A tissue heat transfer model for relating dynamic skin temperature changes to physiological parameters. Phys. Med. Biol. 1988, 33, 895. [Google Scholar] [CrossRef] [PubMed]
- Prasad, B.; Kim, S.; Cho, W.; Kim, S.; Kim, J.K. Effect of tumor properties on energy absorption, temperature mapping, and thermal dose in 13.56-MHz radiofrequency hyperthermia. J. Therm. Biol. 2018, 74, 281–289. [Google Scholar] [CrossRef] [PubMed]






| Temperature Range (°C) | Biological Effect | |
|---|---|---|
| 37 | Normal | 1 |
| Biostimulation | 1 | |
| Hyperthermia | 2 | |
| Reduction in enzyme activity | 2 | |
| Protein denaturation (coagulation) | 3 | |
| Welding | 4 | |
| Permeabilization of cell membranes | 5 | |
| Vaporization | 6 |
| Tumor Tissue & AuNPs | Normal Tissue | |
|---|---|---|
| Absorption coefficient (cm−1) | 121 | 0.02 |
| Reduced scattering coefficient (cm−1) | 0.5 | 6.5 |
| Density (kg/m3) | 1100 | 1000 |
| Specific heat (J/kgK) | 4200 | 4200 |
| Thermal conductivity (W/mK) | 0.55 | 0.5 |
| (mm) | (kg/m3) | (W/mK) | ||
|---|---|---|---|---|
| Epidermis | 0.08 | 1200 | 3589 | 0.235 |
| Papillary dermis | 0.5 | 1200 | 3300 | 0.445 |
| Reticular dermis | 0.6 | 1200 | 3300 | 0.445 |
| Subcutaneous fat | 4.82 | 1000 | 2500 | 0.19 |
| Tumor tissue | 2 | 1070 | 3421 | 0.495 |
| Numerical Parameter | Case | Number | Remarks |
|---|---|---|---|
| ) | 0 to 1.2 W | 601 | Interval: 0.002 W |
| Type of AuNP | Rod, sphere, shell, pyramid, prism, cube | 6 | |
| ) | 10 to 50 nm | 9 | Interval: 5 nm |
| ) | 10−3 to 10−6 | 4 | Interval: 10−1 |
| AuNP Type | ||||
|---|---|---|---|---|
| Rod | 10.01 | 990 | 15.7160 | 0.4703 |
| 15.58 | 1010 | 21.0660 | 2.2822 | |
| 20.02 | 1030 | 22.1100 | 4.9106 | |
| 25.58 | 1070 | 20.9410 | 9.0330 | |
| 30.02 | 1110 | 18.1880 | 11.7830 | |
| 35.59 | 1150 | 14.8070 | 14.7490 | |
| 40.03 | 1200 | 12.4000 | 16.1530 | |
| 45.60 | 1260 | 9.8333 | 17.5270 | |
| 50.04 | 1310 | 8.2106 | 18.2100 | |
| Sphere | 10 | 510 | 0.4589 | 0.0016 |
| 15 | 510 | 0.7113 | 0.0082 | |
| 20 | 510 | 0.9880 | 0.0266 | |
| 25 | 510 | 1.2914 | 0.0669 | |
| 30 | 510 | 1.6168 | 0.1424 | |
| 35 | 510 | 1.9491 | 0.2676 | |
| 40 | 510 | 2.2594 | 0.4531 | |
| 45 | 520 | 2.5419 | 0.8789 | |
| 50 | 520 | 2.7331 | 1.2601 | |
| Shell | 9.96 | 530 | 1.1211 | 0.0040 |
| 15.16 | 560 | 2.8056 | 0.0476 | |
| 20.11 | 590 | 5.6807 | 0.2735 | |
| 24.97 | 630 | 8.9640 | 1.0629 | |
| 30.03 | 650 | 8.6687 | 1.5817 | |
| 35.09 | 630 | 9.3365 | 2.5683 | |
| 39.99 | 860 | 8.4822 | 1.6203 | |
| 44.95 | 720 | 8.2782 | 1.7524 | |
| 49.98 | 720 | 7.1150 | 1.3602 | |
| Pyramid | 10.04 | 590 | 1.3073 | 0.0044 |
| 15.06 | 590 | 2.0064 | 0.0228 | |
| 20.07 | 600 | 2.7377 | 0.0804 | |
| 24.94 | 600 | 3.4829 | 0.1943 | |
| 29.96 | 610 | 4.1738 | 0.4310 | |
| 34.98 | 620 | 4.7951 | 0.8355 | |
| 40.15 | 630 | 5.2890 | 1.4857 | |
| 45.01 | 640 | 5.4828 | 2.3042 | |
| 49.88 | 650 | 5.3941 | 3.2793 | |
| Prism | 10.02 | 530 | 0.6632 | 0.0017 |
| 15.02 | 530 | 1.0137 | 0.0086 | |
| 20.03 | 530 | 1.3802 | 0.0268 | |
| 25.04 | 530 | 1.7562 | 0.0639 | |
| 30.05 | 540 | 2.1391 | 0.1424 | |
| 35.06 | 540 | 2.5227 | 0.2510 | |
| 40.06 | 540 | 2.8719 | 0.3962 | |
| 45.07 | 550 | 3.1703 | 0.6303 | |
| 50.08 | 550 | 3.4553 | 0.8469 | |
| Cube | 9.93 | 530 | 0.8433 | 0.0031 |
| 14.89 | 530 | 1.3110 | 0.0163 | |
| 19.85 | 530 | 1.8217 | 0.0532 | |
| 25.12 | 530 | 2.4007 | 0.1401 | |
| 30.09 | 530 | 2.9437 | 0.2905 | |
| 35.05 | 530 | 3.4159 | 0.5221 | |
| 40.01 | 540 | 3.8570 | 1.0409 | |
| 44.98 | 540 | 4.0785 | 1.5180 | |
| 49.94 | 540 | 4.0361 | 1.9763 |
| AuNP Type | Effective Apoptosis Ratio | ||||
|---|---|---|---|---|---|
| Rod | 10.01 | 990 | 10−6 | 0.104 | 0.74876 |
| 15.58 | 1010 | 10−6 | 0.116 | 0.74978 | |
| 20.02 | 1030 | 10−6 | 0.134 | 0.75035 | |
| 25.58 | 1070 | 10−6 | 0.166 | 0.75046 | |
| 30.02 | 1110 | 10−6 | 0.202 | 0.75010 | |
| 35.59 | 1150 | 10−6 | 0.260 | 0.75058 | |
| 40.03 | 1200 | 10−6 | 0.310 | 0.75020 | |
| 45.60 | 1260 | 10−6 | 0.384 | 0.75054 | |
| 50.04 | 1310 | 10−6 | 0.442 | 0.75092 | |
| Sphere | 10 | 510 | 10−6 | 0.630 | 0.75143 |
| 15 | 510 | 10−6 | 0.626 | 0.75164 | |
| 20 | 510 | 10−6 | 0.620 | 0.75119 | |
| 25 | 510 | 10−6 | 0.612 | 0.75208 | |
| 30 | 510 | 10−6 | 0.606 | 0.75178 | |
| 35 | 510 | 10−6 | 0.598 | 0.75136 | |
| 40 | 510 | 10−6 | 0.598 | 0.75189 | |
| 45 | 520 | 10−6 | 0.600 | 0.75189 | |
| 50 | 520 | 10−6 | 0.606 | 0.75107 | |
| Shell | 9.96 | 530 | 10−6 | 0.458 | 0.75111 |
| 15.16 | 560 | 10−6 | 0.360 | 0.75065 | |
| 20.11 | 590 | 10−6 | 0.284 | 0.75089 | |
| 24.97 | 630 | 10−6 | 0.248 | 0.74977 | |
| 30.03 | 650 | 10−6 | 0.284 | 0.75083 | |
| 35.09 | 630 | 10−6 | 0.302 | 0.75042 | |
| 39.99 | 860 | 10−6 | 0.338 | 0.75095 | |
| 44.95 | 720 | 10−6 | 0.466 | 0.75094 | |
| 49.98 | 720 | 10−6 | 0.416 | 0.75081 | |
| Pyramid | 10.04 | 590 | 10−6 | 0.430 | 0.75065 |
| 15.06 | 590 | 10−6 | 0.426 | 0.75119 | |
| 20.07 | 600 | 10−6 | 0.420 | 0.75090 | |
| 24.94 | 600 | 10−6 | 0.418 | 0.75056 | |
| 29.96 | 610 | 10−6 | 0.418 | 0.75072 | |
| 34.98 | 620 | 10−6 | 0.424 | 0.75143 | |
| 40.15 | 630 | 10−6 | 0.434 | 0.75101 | |
| 45.01 | 640 | 10−6 | 0.454 | 0.75066 | |
| 49.88 | 650 | 10−6 | 0.480 | 0.75088 | |
| Prism | 10.02 | 530 | 10−6 | 0.564 | 0.75141 |
| 15.02 | 530 | 10−6 | 0.562 | 0.75164 | |
| 20.03 | 530 | 10−6 | 0.558 | 0.75132 | |
| 25.04 | 530 | 10−6 | 0.556 | 0.75146 | |
| 30.05 | 540 | 10−6 | 0.554 | 0.75149 | |
| 35.06 | 540 | 10−6 | 0.552 | 0.75140 | |
| 40.06 | 540 | 10−6 | 0.554 | 0.75114 | |
| 45.07 | 550 | 10−6 | 0.558 | 0.75140 | |
| 50.08 | 550 | 10−6 | 0.560 | 0.75141 | |
| Cube | 9.93 | 530 | 10−6 | 0.518 | 0.75119 |
| 14.89 | 530 | 10−6 | 0.510 | 0.75101 | |
| 19.85 | 530 | 10−6 | 0.502 | 0.75101 | |
| 25.12 | 530 | 10−6 | 0.494 | 0.75104 | |
| 30.09 | 530 | 10−6 | 0.490 | 0.75104 | |
| 35.05 | 530 | 10−6 | 0.492 | 0.75148 | |
| 40.01 | 540 | 10−6 | 0.496 | 0.75088 | |
| 44.98 | 540 | 10−6 | 0.512 | 0.75102 | |
| 49.94 | 540 | 10−6 | 0.534 | 0.75131 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, D.; Kim, H. Numerical Study on Death of Squamous Cell Carcinoma Based on Various Shapes of Gold Nanoparticles Using Photothermal Therapy. Sensors 2022, 22, 1671. https://doi.org/10.3390/s22041671
Kim D, Kim H. Numerical Study on Death of Squamous Cell Carcinoma Based on Various Shapes of Gold Nanoparticles Using Photothermal Therapy. Sensors. 2022; 22(4):1671. https://doi.org/10.3390/s22041671
Chicago/Turabian StyleKim, Donghyuk, and Hyunjung Kim. 2022. "Numerical Study on Death of Squamous Cell Carcinoma Based on Various Shapes of Gold Nanoparticles Using Photothermal Therapy" Sensors 22, no. 4: 1671. https://doi.org/10.3390/s22041671
APA StyleKim, D., & Kim, H. (2022). Numerical Study on Death of Squamous Cell Carcinoma Based on Various Shapes of Gold Nanoparticles Using Photothermal Therapy. Sensors, 22(4), 1671. https://doi.org/10.3390/s22041671






