The Validity and Reliability of a New Simple Instrument for the Measurement of First Ray Mobility
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Sample Size Calculation
2.3. Study Design
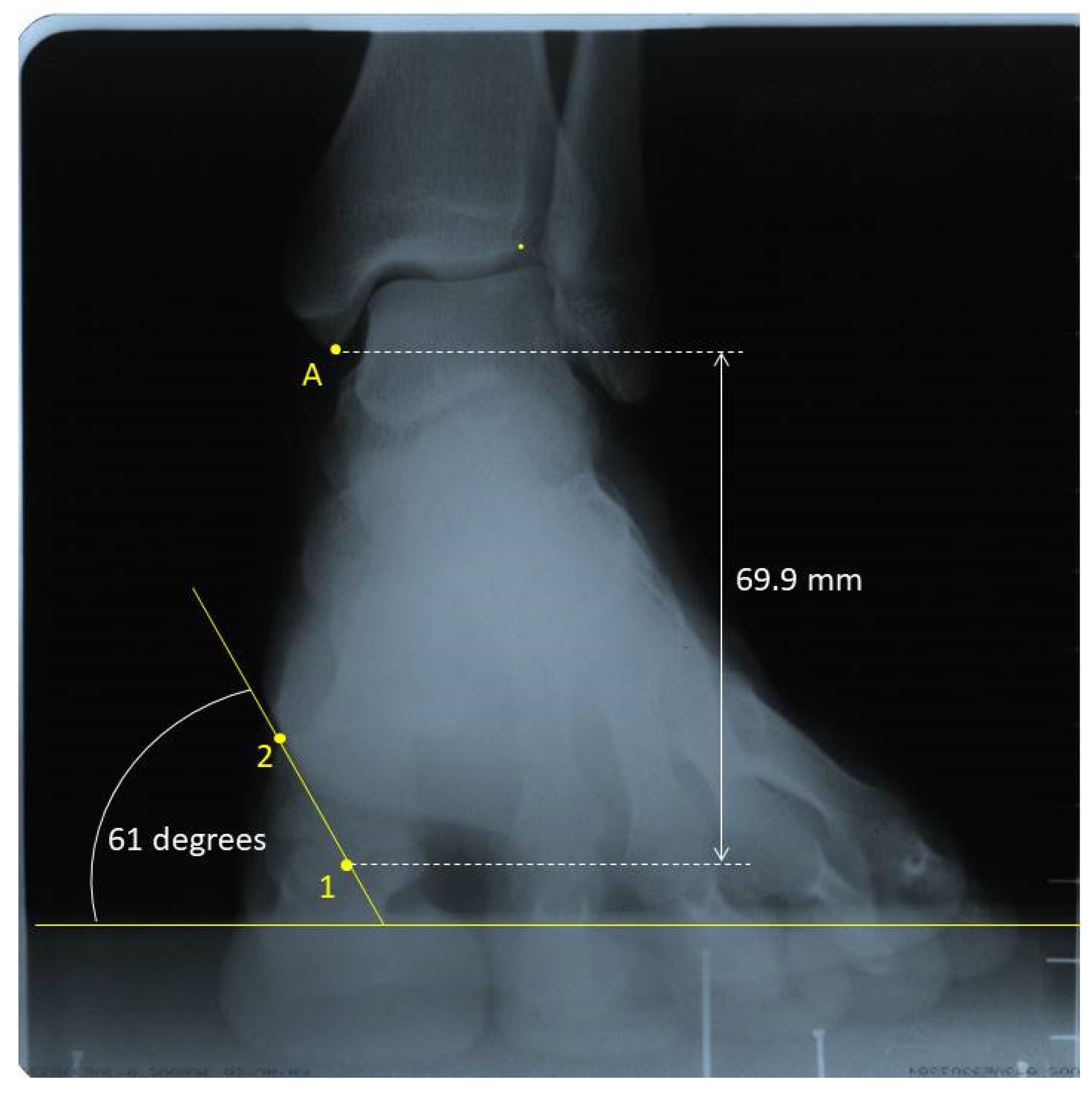
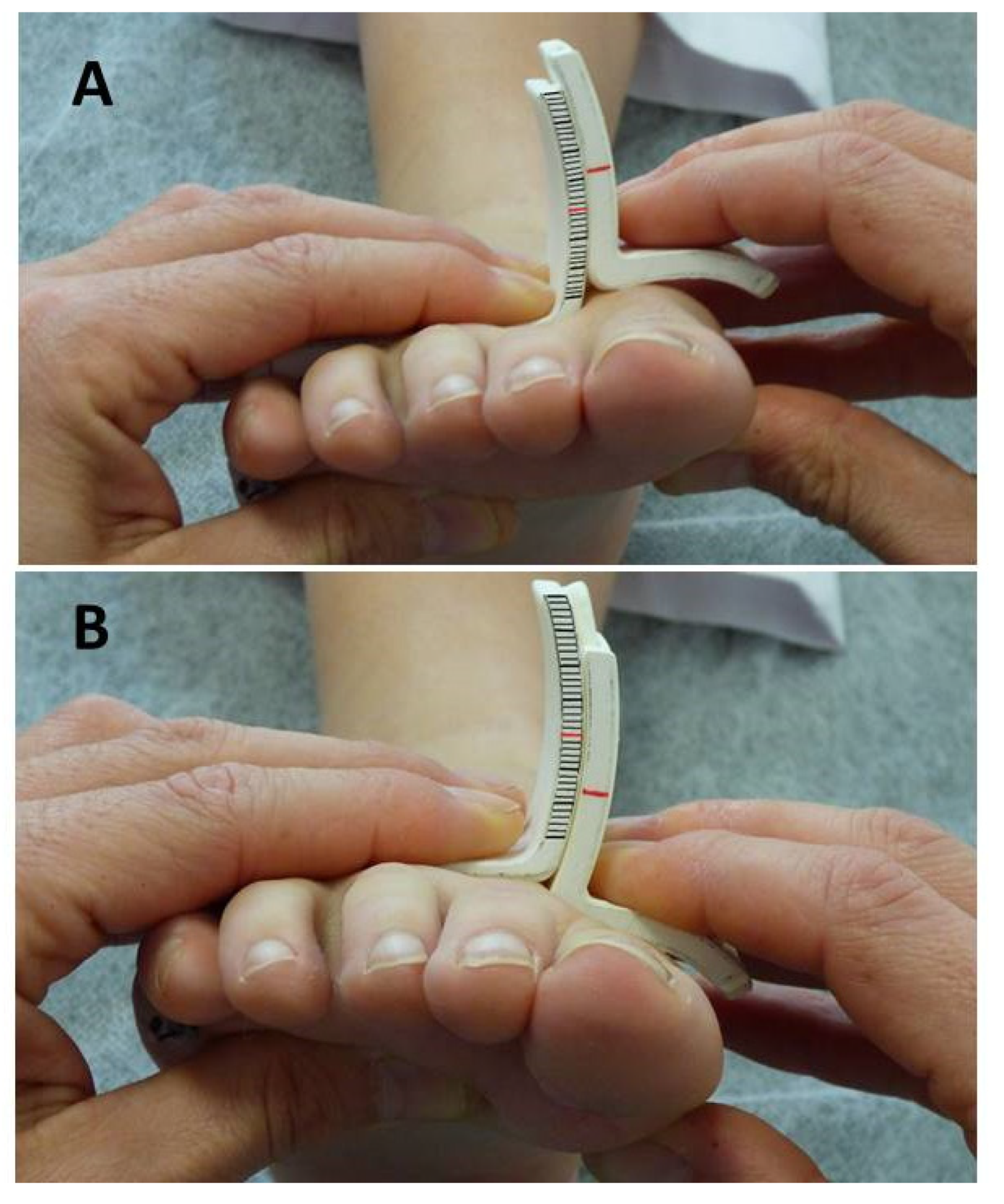
2.4. Measurements
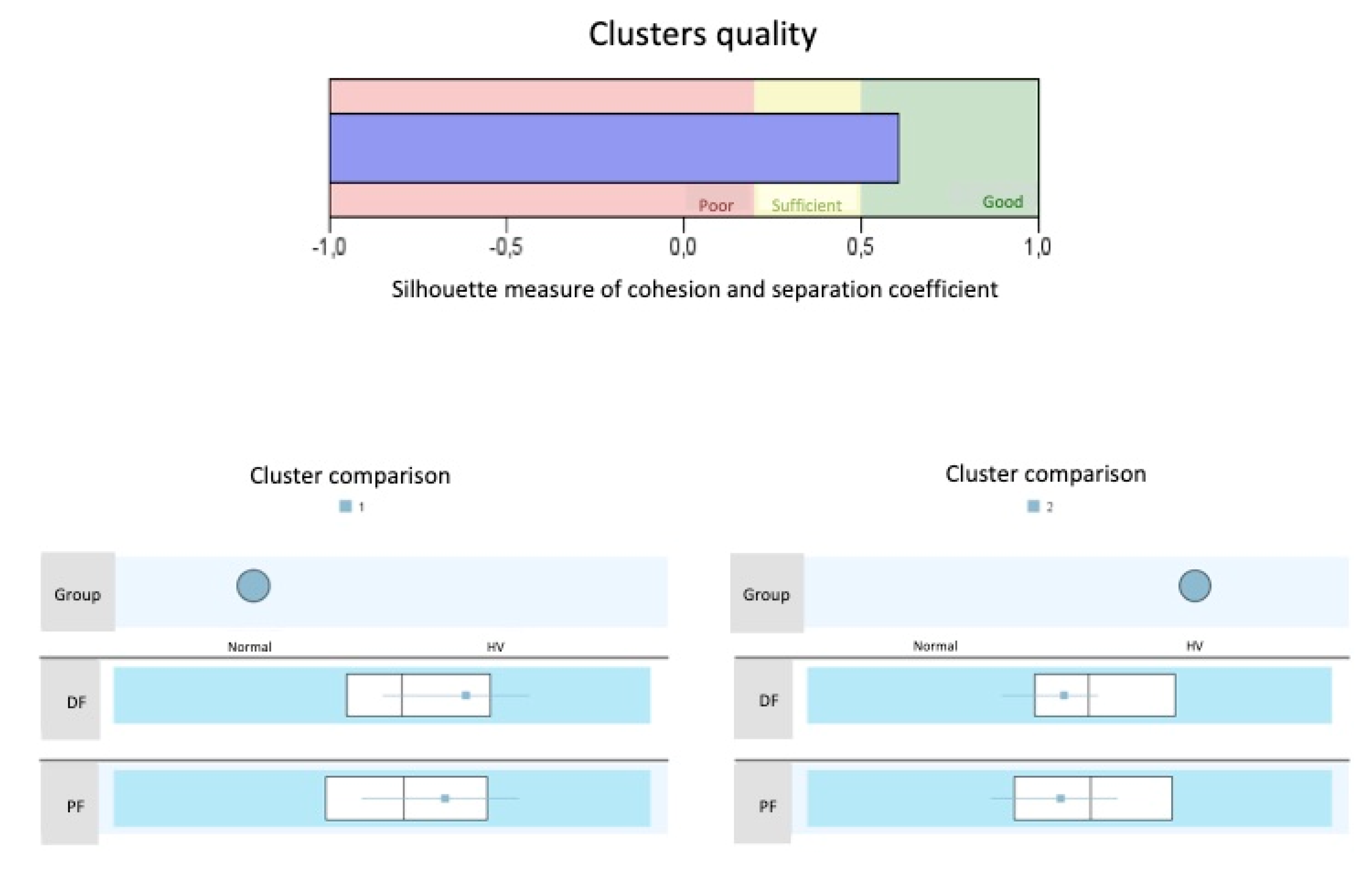
2.5. Data Analysis
3. Results
3.1. Participants’ Characteristics
3.2. Group Differences
3.3. Reliability
3.4. Validity
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Birke, J.A.; Franks, B.D.; Foto, J.G. First ray joint limitation, pressure, and ulceration of the first metatarsal head in diabetes mellitus. Foot Ankle Int. 1995, 16, 277–284. [Google Scholar] [CrossRef]
- Glasoe, W.M.; Jensen, D.D.; Kampa, B.B.; Karg, L.K.; Krych, A.R.; Pena, F.A.; Ludewig, P.M. First ray kinematics in women with rheumatoid arthritis and bunion deformity: A gait simulation imaging study. Arthritis Care Res. 2014, 66, 837–843. [Google Scholar] [CrossRef] [PubMed]
- Shibuya, N.; Roukis, T.; Jupiter, D. Mobility of the first ray in patients with or without hallux valgus deformity: Systematic review and meta-analysis. J. Foot Ankle Surg. 2017, 56, 1070–1075. [Google Scholar] [CrossRef] [PubMed]
- Kimura, T.; Kubota, M.; Taguchi, T.; Suzuki, N.; Hattori, A.; Marumo, K. Evaluation of first-ray mobility in patients with hallux valgus using weight-bearing CT and a 3-D analysis system a comparison with normal feet. J. Bone Joint. Surg. Am. Vol. 2017, 99, 247–255. [Google Scholar] [CrossRef] [PubMed]
- Morton, D. Hypermobility of the first metatarsal bone: The interlinking factor between metatarsalgia and longitudinal arch strains. J. Bone Joint. Surg. 1928, 10, 187–196. [Google Scholar]
- Morton, D. The Human Foot and Its Evolution; Columbia University Press: New York, NY, USA, 1935. [Google Scholar]
- Root, M.; Orien, W.; Weed, J. Normal and Abnormal Function of the Foot; Clinical Biomechanics Corp: Los Angeles, CA, USA, 1977; Volume 2. [Google Scholar]
- Glasoe, W.M.; Michaud, T.C. Measurement of Dorsal First Ray Mobility: A Topical Historical Review and Commentary. Foot Ankle Int. 2019, 40, 603–610. [Google Scholar] [CrossRef]
- Klaue, K.; Hansen, S.T.; Masquelet, A.C. Clinical, quantitative assessment of first tarsometatarsal mobility in the sagittal plane and its relation to hallux valgus deformity. Foot Ankle Int. 1994, 15, 9–13. [Google Scholar] [CrossRef]
- Glasoe, W.M.; Yack, H.J.; Saltzman, C.L. Measuring first ray mobility with a new device. Arch. Phys. Med. Rehabil. 1999, 80, 122–124. [Google Scholar] [CrossRef]
- Singh, D.; Biz, C.; Corradin, M.; Favero, L. Comparison of dorsal and dorsomedial displacement in evaluation of first ray hypermobility in feet with and without hallux valgus. Foot Ankle Surg. 2016, 22, 120–124. [Google Scholar] [CrossRef]
- Glasoe, W.M.; Grebing, B.R.; Beck, S.; Coughlin, M.J.; Saltzman, C.L. A comparison of device measures of dorsal first ray mobility. Foot Ankle Int. 2005, 26, 957–961. [Google Scholar] [CrossRef]
- Jones, C.P.; Coughlin, M.J.; Pierce-Villadot, R.; Golano, P.; Kennedy, M.P.; Shumas, P.S.; Grebing, B.R.; Teachout, L. The validity and reliability of the Klaue device. Foot Ankle Int. 2005, 26, 951–956. [Google Scholar] [CrossRef] [PubMed]
- Grebing, B.R.; Coughlin, M.J. Evaluation of Morton’s theory of second metatarsal hypertrophy. J. Bone Joint. Surg. Ser. A 2004, 86, 1375–1386. [Google Scholar] [CrossRef] [PubMed]
- Glasoe, W.M.; Yack, H.J.; Saltzman, C.L. The reliability and validity of a first ray measurement device. Foot Ankle Int. 2000, 21, 240–246. [Google Scholar] [CrossRef] [PubMed]
- Glasoe, W.M.; Getsoian, S.; Myers, M.; Komnick, M.; Kolkebeck, D.; Oswald, W.; Liakos, P. Criterion-related validity of a clinical measure of dorsal first ray mobility. J. Orthop. Sports Phys. Ther. 2005, 35, 589–593. [Google Scholar] [CrossRef]
- Geng, X.; Wang, C.; Ma, X.; Wang, X.; Huang, J.; Zhang, C.; Xu, J.; Yang, J. Mobility of the first metatarsal-cuneiform joint in patients with and without hallux valgus: In vivo three-dimensional analysis using computerized tomography scan. J. Orthop. Surg. Res. 2015, 10, 140. [Google Scholar] [CrossRef] [PubMed]
- Wallace, W.A.; Kilmartin, T.E. Predicting hallux abducto valgus. J. Am. Podiatr. Med. Assoc. 1990, 80, 509–510. [Google Scholar] [CrossRef]
- Lee, K.T.; Young, K. Measurement of first-ray mobility in normal vs. hallux valgus patients. Foot Ankle Int. 2001, 22, 960–964. [Google Scholar] [CrossRef]
- Kim, J.-Y.; Keun Hwang, S.; Tai Lee, K.; Won Young, K.; Seon Jung, J. A simpler device for measuring the mobility of the first ray of the foot. Foot Ankle Int. 2008, 29, 213–218. [Google Scholar] [CrossRef]
- Tavara-Vidalón, S.; Monge-Vera, M.; Lafuente-Sotillos, G.; Domínguez-Maldonado, G.; Munuera-Martínez, P. Static Range of Motion of the First Metatarsal in the Sagittal and Frontal Planes. J. Clin. Med. 2018, 7, 456. [Google Scholar] [CrossRef]
- Kirby, K. Biomechanics of the normal and abnormal foot. J. Am. Podiatr. Med. Assoc. 2000, 90, 30–34. [Google Scholar] [CrossRef]
- Menz, H.B. Two feet, or one person? Problems associated with statistical analysis of paired data in foot and ankle medicine. Foot 2004, 14, 2–5. [Google Scholar] [CrossRef]
- Garrow, A.P.; Papageorgiou, A.; Silman, A.J.; Thomas, E.; Jayson, M.I.; Macfarlane, G.J. The grading of hallux valgus. The Manchester Scale. J. Am. Podiatr. Med. Assoc. 2001, 91, 74–78. [Google Scholar] [CrossRef] [PubMed]
- Menz, H.B.; Munteanu, S.E. Radiographic validation of the Manchester scale for the classification of hallux valgus deformity. Rheumatology 2005, 44, 1061–1066. [Google Scholar] [CrossRef] [PubMed]
- Fritz, G.R.; Prieskorn, D.; Fritz, G.R. Farm First metatarsocuneiform motion: A radiographic and statistical analysis. Foot Ankle Int. 1995, 16, 117–123. [Google Scholar] [CrossRef]
- Swanson, J.E.; Stoltman, M.G.; Oyen, C.R.; Mohrbacher, J.A.; Orandi, A.; Olson, J.M.; Glasoe, W.M. Comparison of 2D-3D measurements of hallux and first ray sagittal motion in patients with and without hallux valgus. Foot Ankle Int. 2016, 37, 227–232. [Google Scholar] [CrossRef]
- King, D.; Toolan, B. Associated deformities and hypermobility in hallux valgus: An investigation with weightbearing radiographs. Foot Ankle Int. 2004, 25, 251–255. [Google Scholar] [CrossRef]
- Faber, F.W.; Kleinrensink, G.J.; Verhoog, M.W.; Vijn, A.H.; Snijders, C.J.; Mulder, P.G.; Verhaar, J.A. Mobility of the first tarsometatarsal joint in relation to hallux valgus deformity: Anatomical and biomechanical aspects. Foot Ankle Int. 1999, 20, 651–656. [Google Scholar] [CrossRef]
- Glasoe, W.M.; Allen, M.K.; Saltzman, C.L. First ray dorsal mobility in relation to hallux valgus deformity and first intermetatarsal angle. Foot Ankle Int. 2001, 22, 98–101. [Google Scholar] [CrossRef]
- Glasoe, W.M.; Pena, F.A.; Phadke, V. Cardan angle rotation sequence effects on first-metatarsophalangeal joint kinematics: Implications for measuring hallux valgus deformity. J. Foot Ankle Res. 2014, 7, 29. [Google Scholar] [CrossRef]
- Hicks, J.H. The mechanics of the foot. I. The joints. J. Anat. 1953, 87, 345–357. [Google Scholar]
- Ebisui, J. The first ray axis and the first metatarsophalangeal joint: An anatomical and pathomechanical study. J. Am. Podiatr. Med. Assoc. 1968, 58, 160–168. [Google Scholar] [CrossRef] [PubMed]
- Sarrafian, S.K. Functional characteristics of the foot and plantar aponeurosis under tibiotalar loading. Foot Ankle 1987, 8, 4–18. [Google Scholar] [CrossRef] [PubMed]
- Root, M.; Orien, W.; Weed, J.; Hughes, R. Biomechanical Examination of the Foot; Clinical Biomechanics Corp: Los Angeles, CA, USA, 1971; Volume 1. [Google Scholar]
- D’Amico, J.; Schuster, R. Motion of the first ray: Clarification through investigation. J. Am. Pod. Med. Assoc. 1979, 69, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Dayton, P.; Kauwe, M.; Didomenico, L.; Feilmeier, M.; Reimer, R. Quantitative Analysis of the Degree of Frontal Rotation Required to Anatomically Align the First Metatarsal Phalangeal Joint During Modified Tarsal-Metatarsal Arthrodesis Without Capsular Balancing. J. Foot Ankle Surg. 2016, 55, 220–225. [Google Scholar] [CrossRef]
- Grode, S.; McCarthy, D. The anatomical implications of hallux abducto valgus: A cryomicrotomy study. J. Am. Podiatr. Med. Assoc. 1980, 70, 539–551. [Google Scholar] [CrossRef]
- Oldenbrook, L.; Smith, C. Metatarsal head motion secondary to rearfoot pronation and supination: An anatomical investigation. J. Am. Podiatr. Med. Assoc. 1979, 69, 24–28. [Google Scholar] [CrossRef]
- Ota, T.; Nagura, T.; Kokubo, T.; Kitashiro, M.; Ogihara, N.; Takeshima, K.; Seki, H.; Suda, Y.; Matsumoto, M.; Nakamura, M. Etiological factors in hallux valgus, a three-dimensional analysis of the first metatarsal. J. Foot Ankle Res. 2017, 10, 43. [Google Scholar] [CrossRef]
- Kelso, S.; Richie, D.; Cohen, I.; Weed, J.; Root, M. Direction and range of motion of the first ray. J. Am. Podiatr. Med. Assoc. 1982, 72, 600–605. [Google Scholar] [CrossRef]
- Wanivenhaus, A.; Pretterklieber, M. First tarsometatarsal joint: Anatomical biomechanical study. Foot Ankle 1989, 9, 153–157. [Google Scholar] [CrossRef]
- Glasoe, W.M.; Allen, M.K.; Yack, H.J. Measurement of dorsal mobility in the first ray: Elimination of fat pad compression as a variable. Foot Ankle Int. 1998, 19, 542–546. [Google Scholar] [CrossRef]
- Rogers, M.; Cavanagh, P. A Device for the Measurement of first Ray Mobility. In Proceedings of the North American Congress on Biomechanics, Montreal, QC, Canada, 25–27 August 1986; pp. 205–206. [Google Scholar]
- Samimi, R.; Green, D.; Malay, D. Evaluation of First Metatarsophalangeal Range of motion Pre and Post Bunion Surgery: A Clinical and Radiographic Correlation with Stress Lateral Dorsiflexion Views; A Retrospective Approach. Available online: http://www.podiatryinstitute.com/pdfs/Update_2009/2009_16.pdf (accessed on 10 February 2020).
- Diaz, R.; Samimi, R.; Green, D.; Green, R.; Agan, D. Metatarsophalangeal Range of Motion Pre and Post Bunion Surgery: A Clinical and Radiographic Correlation with Stress Lateral Dorsiflexion Views. Part 2. Available online: http://www.podiatryinstitute.com/pdfs/Update_2010/2010_33.pdf (accessed on 10 February 2020).
- Greisberg, J.; Prince, D.; Sperber, L. First ray mobility increase in patients with metatarsalgia. Foot Ankle Int. 2010, 31, 954–958. [Google Scholar] [CrossRef] [PubMed]
- Davitt, J.S.; Kadel, N.; Sangeorzan, B.J.; Hansen, S.T.; Holt, S.K.; Donaldson-Fletcher, E. An association between functional second metatarsal length and midfoot arthrosis. J. Bone Joint. Surg. Ser. A 2005, 87, 795–800. [Google Scholar] [CrossRef]
- Parker, N.; Greenhalgh, A.; Chockalingam, N.; Dangerfield, P.H. Positional relationship between leg rotation and lumbar spine during quiet standing. Stud. Health Technol. Inform. 2008, 140, 231–239. [Google Scholar] [PubMed]
- Tateuchi, H.; Wada, O.; Ichihashi, N. Effects of calcaneal eversion on three-dimensional kinematics of the hip, pelvis and thorax in unilateral weight bearing. Hum. Mov. Sci. 2011, 30, 566–573. [Google Scholar] [CrossRef] [PubMed]
- Khamis, S.; Yizhar, Z. Effect of feet hyperpronation on pelvic alignment in a standing position. Gait Posture 2007, 25, 127–134. [Google Scholar] [CrossRef] [PubMed]




| Variable | Control Group (Mean ± SD) | HV Group (Mean ± SD) | P-Value | Difference 95% CI |
|---|---|---|---|---|
| Dorsiflexion (mm) | 5.19 ± 2.32 | 7.03 ± 2.76 | 0.015 | −3.30–0.38 |
| Plantarflexion (mm) | 3.32 ± 2.27 | 2.80 ± 1.84 | 0.383 | −0.67−1.71 |
| Total sagittal movement (mm) | 8.51 ± 3.41 | 9.83 ± 2.81 | 0.147 | −3.12−0.48 |
| Inversion (degrees) | 2.68 ± 4.09 | 2.71 ± 3.22 | 0.979 | −2.15–2.09 |
| Eversion (degrees) | 3.16 ± 2.91 | 2.12 ± 3.98 | 0.303 | −0.96–3.03 |
| Total frontal movement (degrees) | 5.84 ± 5.20 | 4.83 ± 3.78 | 0.444 | −1.62–3.63 |
| Movement in the transverse plane during dorsalflexion * (mm) | −0.64 ± 5.86 | 1.69 ± 6.01 | 0.656 | −3.10–4.87 |
| Movement in the transverse plane during plantarflexion * (mm) | −4.11 ± 6.06 | –5.00 ± 7.74 | 0.176 | −5.74–1.08 |
| Total transverse movement (mm) † | 4.11 ± 6.06 | 6.69 ± 9.01 | 0.244 | −1.82–6.98 |
| Variable | Control Group Mean ± SD (95% CI) | HV GroupMean ± SD (95% CI) | P-Value |
|---|---|---|---|
| Sagittal plane | 77.42 ± 8.19 (74.04–80.80) | 72.69 ± 8.99 (68.90–76.49) | 0.060 |
| Frontal plane | 53.80 ± 5.67 (51.45–56.15) | 50.00 ± 4.74 (48.00–52.00) | 0.005 |
| Transverse plane | 10.64 ± 6.48 (8.10–13.18) | 9.55 ± 5.38 (7.40–11.70) | 0.525 |
| ICC (95% CI) | ||
|---|---|---|
| Rater 1 | Rater 2 | |
| Control group | ||
| Dorsiflexion | 0.883 (0.794–0.942) | 0.892 (0.810–946) |
| Plantarflexion | 0.907 (0.837–0.954) | 0.895 (0.816–0.948) |
| HV group | ||
| Dorsiflexion | 0.872 (0.691–0.963) | 0.808 (0.537–0.945) |
| Plantarflexion | 0.917 (0.799–0.976) | 0.792 (0.597–0.940) |
| INTER-RATER | |||
|---|---|---|---|
| ICC | DF | PF | |
| Rater1-Rater2 | Normal | 0.928 (0.878–0.963) | 0.940 (0.898–0.969) |
| HV | 0.919 (0.818–0.976) | 0.925 (0.832–0.978) | |
| Total | 0.932 (0.893–0.961) | 0.932 (0.893–0.961) | |
| Group | Total First Ray ROM (mm) |
|---|---|
| Normal feet | 10.5 to 11.6 |
| Interval of uncertainty | 11.6 to 12.8 |
| HV feet | 12.8 to 14.6 |
| DF | PF | TOTAL ROM | |
|---|---|---|---|
| AUC (95% CI) | 0.656 (0.501–0.811) | 0.721 (0.577–0.865) | 0.704 (0.558–0.851) |
| Cut-off point (mm) | 6.75 | 5.08 | 12.25 |
| Sensitivity (%) | 66.7 | 75.0 | 70.8 |
| Specificity (%) | 56.0 | 52.0 | 60.0 |
| PPV (%) | 59.3 | 60.0 | 63.0 |
| NPV (%) | 63.6 | 68.4 | 68.2 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Munuera-Martínez, P.V.; Távara-Vidalón, P.; Monge-Vera, M.A.; Sáez-Díaz, A.; Lafuente-Sotillos, G. The Validity and Reliability of a New Simple Instrument for the Measurement of First Ray Mobility. Sensors 2020, 20, 2207. https://doi.org/10.3390/s20082207
Munuera-Martínez PV, Távara-Vidalón P, Monge-Vera MA, Sáez-Díaz A, Lafuente-Sotillos G. The Validity and Reliability of a New Simple Instrument for the Measurement of First Ray Mobility. Sensors. 2020; 20(8):2207. https://doi.org/10.3390/s20082207
Chicago/Turabian StyleMunuera-Martínez, Pedro V., Priscila Távara-Vidalón, Manuel A. Monge-Vera, Antonia Sáez-Díaz, and Guillermo Lafuente-Sotillos. 2020. "The Validity and Reliability of a New Simple Instrument for the Measurement of First Ray Mobility" Sensors 20, no. 8: 2207. https://doi.org/10.3390/s20082207
APA StyleMunuera-Martínez, P. V., Távara-Vidalón, P., Monge-Vera, M. A., Sáez-Díaz, A., & Lafuente-Sotillos, G. (2020). The Validity and Reliability of a New Simple Instrument for the Measurement of First Ray Mobility. Sensors, 20(8), 2207. https://doi.org/10.3390/s20082207






